pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
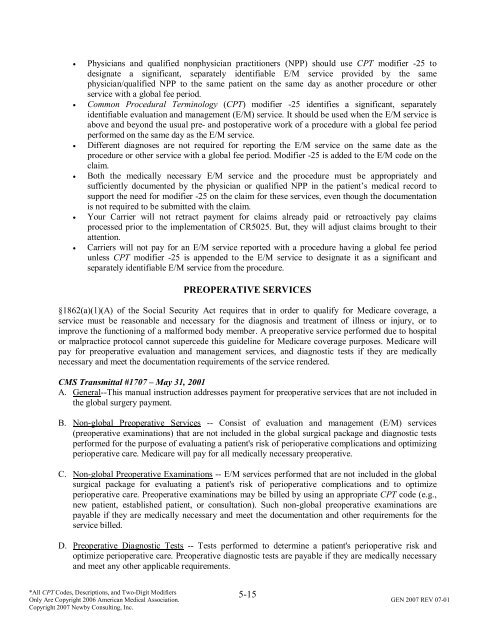
• Physicians <strong>and</strong> qualified nonphysician practitioners (NPP) should use CPT modifier -25 to<br />
designate a significant, separately identifiable E/M service provided by the same<br />
physician/qualified NPP to the same patient on the same day as another procedure or other<br />
service with a global fee period.<br />
• Common Procedural Terminology (CPT) modifier -25 identifies a significant, separately<br />
identifiable evaluation <strong>and</strong> management (E/M) service. It should be used when the E/M service is<br />
above <strong>and</strong> beyond the usual pre- <strong>and</strong> postoperative work <strong>of</strong> a procedure with a global fee period<br />
performed on the same day as the E/M service.<br />
• Different diagnoses are not required for <strong>reporting</strong> the E/M service on the same date as the<br />
procedure or other service with a global fee period. Modifier -25 is added to the E/M code on the<br />
claim.<br />
• Both the medically necessary E/M service <strong>and</strong> the procedure must be appropriately <strong>and</strong><br />
sufficiently documented by the physician or qualified NPP in the patient’s medical record to<br />
support the need for modifier -25 on the claim for these services, even though the documentation<br />
is not required to be submitted with the claim.<br />
• Your Carrier will not retract payment for claims already paid or retroactively pay claims<br />
processed prior to the implementation <strong>of</strong> CR5025. But, they will adjust claims brought to their<br />
attention.<br />
• Carriers will not pay for an E/M service reported with a procedure having a global fee period<br />
unless CPT modifier -25 is appended to the E/M service to designate it as a significant <strong>and</strong><br />
separately identifiable E/M service from the procedure.<br />
PREOPERATIVE SERVICES<br />
§1862(a)(1)(A) <strong>of</strong> the Social Security Act requires that in order to qualify for Medicare coverage, a<br />
service must be reasonable <strong>and</strong> necessary for the diagnosis <strong>and</strong> treatment <strong>of</strong> illness or injury, or to<br />
improve the functioning <strong>of</strong> a malformed body member. A preoperative service performed due to hospital<br />
or malpractice protocol cannot supercede this guideline for Medicare coverage purposes. Medicare will<br />
pay for preoperative evaluation <strong>and</strong> management services, <strong>and</strong> diagnostic tests if they are medically<br />
necessary <strong>and</strong> meet the documentation requirements <strong>of</strong> the service rendered.<br />
CMS Transmittal #1707 – May 31, 2001<br />
A. General--This manual instruction addresses payment for preoperative services that are not included in<br />
the global surgery payment.<br />
B. Non-global Preoperative Services -- Consist <strong>of</strong> evaluation <strong>and</strong> management (E/M) services<br />
(preoperative examinations) that are not included in the global surgical package <strong>and</strong> diagnostic tests<br />
performed for the purpose <strong>of</strong> evaluating a patient's risk <strong>of</strong> perioperative complications <strong>and</strong> optimizing<br />
perioperative care. Medicare will pay for all medically necessary preoperative.<br />
C. Non-global Preoperative Examinations -- E/M services performed that are not included in the global<br />
surgical package for evaluating a patient's risk <strong>of</strong> perioperative complications <strong>and</strong> to optimize<br />
perioperative care. Preoperative examinations may be billed by using an appropriate CPT code (e.g.,<br />
new patient, established patient, or consultation). Such non-global preoperative examinations are<br />
payable if they are medically necessary <strong>and</strong> meet the documentation <strong>and</strong> other requirements for the<br />
service billed.<br />
D. Preoperative Diagnostic Tests -- Tests performed to determine a patient's perioperative risk <strong>and</strong><br />
optimize perioperative care. Preoperative diagnostic tests are payable if they are medically necessary<br />
<strong>and</strong> meet any other applicable requirements.<br />
5-15<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.