pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
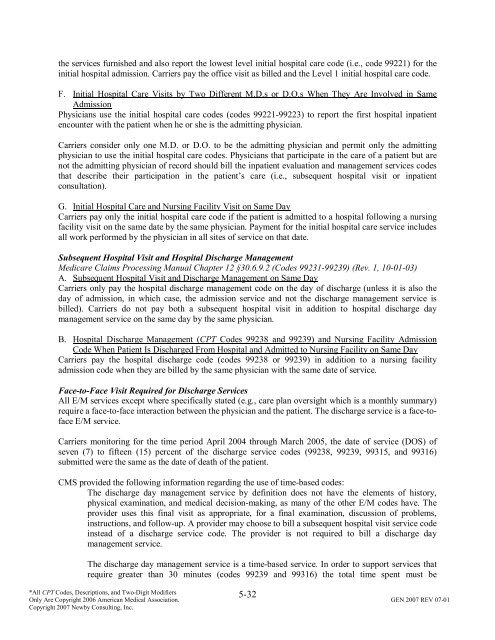
the services furnished <strong>and</strong> also report the lowest level initial hospital care code (i.e., code 99221) for the<br />
initial hospital admission. Carriers pay the <strong>of</strong>fice visit as billed <strong>and</strong> the Level 1 initial hospital care code.<br />
F. Initial Hospital Care Visits by Two Different M.D.s or D.O.s When They Are Involved in Same<br />
Admission<br />
Physicians use the initial hospital care codes (codes 99221-99223) to report the first hospital inpatient<br />
encounter with the patient when he or she is the admitting physician.<br />
Carriers consider only one M.D. or D.O. to be the admitting physician <strong>and</strong> permit only the admitting<br />
physician to use the initial hospital care codes. Physicians that participate in the care <strong>of</strong> a patient but are<br />
not the admitting physician <strong>of</strong> record should bill the inpatient evaluation <strong>and</strong> management services codes<br />
that describe their participation in the patient’s care (i.e., subsequent hospital visit or inpatient<br />
consultation).<br />
G. Initial Hospital Care <strong>and</strong> Nursing Facility Visit on Same Day<br />
Carriers pay only the initial hospital care code if the patient is admitted to a hospital following a nursing<br />
facility visit on the same date by the same physician. Payment for the initial hospital care service includes<br />
all work performed by the physician in all sites <strong>of</strong> service on that date.<br />
Subsequent Hospital Visit <strong>and</strong> Hospital Discharge Management<br />
Medicare Claims Processing Manual Chapter 12 §30.6.9.2 (Codes 99231-99239) (Rev. 1, 10-01-03)<br />
A. Subsequent Hospital Visit <strong>and</strong> Discharge Management on Same Day<br />
Carriers only pay the hospital discharge management code on the day <strong>of</strong> discharge (unless it is also the<br />
day <strong>of</strong> admission, in which case, the admission service <strong>and</strong> not the discharge management service is<br />
billed). Carriers do not pay both a subsequent hospital visit in addition to hospital discharge day<br />
management service on the same day by the same physician.<br />
B. Hospital Discharge Management (CPT Codes 99238 <strong>and</strong> 99239) <strong>and</strong> Nursing Facility Admission<br />
Code When Patient Is Discharged From Hospital <strong>and</strong> Admitted to Nursing Facility on Same Day<br />
Carriers pay the hospital discharge code (codes 99238 or 99239) in addition to a nursing facility<br />
admission code when they are billed by the same physician with the same date <strong>of</strong> service.<br />
Face-to-Face Visit Required for Discharge Services<br />
All E/M services except where specifically stated (e.g., care plan oversight which is a monthly summary)<br />
require a face-to-face interaction between the physician <strong>and</strong> the patient. The discharge service is a face-t<strong>of</strong>ace<br />
E/M service.<br />
Carriers monitoring for the time period April 2004 through March 2005, the date <strong>of</strong> service (DOS) <strong>of</strong><br />
seven (7) to fifteen (15) percent <strong>of</strong> the discharge service codes (99238, 99239, 99315, <strong>and</strong> 99316)<br />
submitted were the same as the date <strong>of</strong> death <strong>of</strong> the patient.<br />
CMS provided the following information regarding the use <strong>of</strong> time-based codes:<br />
The discharge day management service by definition does not have the elements <strong>of</strong> history,<br />
physical examination, <strong>and</strong> medical decision-making, as many <strong>of</strong> the other E/M codes have. The<br />
provider uses this final visit as appropriate, for a final examination, discussion <strong>of</strong> problems,<br />
instructions, <strong>and</strong> follow-up. A provider may choose to bill a subsequent hospital visit service code<br />
instead <strong>of</strong> a discharge service code. The provider is not required to bill a discharge day<br />
management service.<br />
The discharge day management service is a time-based service. In order to support services that<br />
require greater than 30 minutes (codes 99239 <strong>and</strong> 99316) the total time spent must be<br />
5-32<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.