pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
the medical records must clearly document the E/M reported. Both procedure codes should be shown as<br />
separate line items on the claim. These services can also be performed separately on separate <strong>of</strong>fice visits.<br />
Repeat Obtaining Screening Pap Smear Due To Inadequate Specimen<br />
Related Change Request (CR) #: 3659 Medlearn Matters Number: MM3659 Related CR Transmittal #:<br />
440 Implementation Date: July 5, 2005<br />
When a Pap smear specimen is not sufficient for the laboratory to interpret the results <strong>and</strong> another<br />
specimen is needed report Q0091 <strong>and</strong> append the -76 modifier to indicate it is a repeat specimen. The<br />
Carrier will pay for the collection <strong>of</strong> the specimen. Physicians should not report the screening pelvic<br />
examination again as the entire service is not medically necessary. It is also inappropriate to report an<br />
E/M code unless the patient has another problem needing a medically necessary evaluation on the same<br />
date <strong>of</strong> service.<br />
CMS Incident To Clarification<br />
CMS Region V clarified that screening pelvic examination with clinical breast exam (G0101) <strong>and</strong><br />
obtaining screening Pap smear (Q0091) cannot be billed “incident to” the physician’s services. The<br />
physician or nonphysician practitioner who PERFORMS the service(s) must report these screening<br />
services. This clarification applies to all screening services.<br />
Covered Diagnoses For Reporting Screening Pelvic Examination Or The Obtaining Of A Screening<br />
Pap Smear<br />
Medicare Claims Processing Manual Chapter 18 §30.6 (Rev. 1, 10-01-03) AB-03-054 (CR 2637) (Rev.<br />
440, Issued: 01-21-05, Effective: 07-01-05, Implementation: 07-05-05)<br />
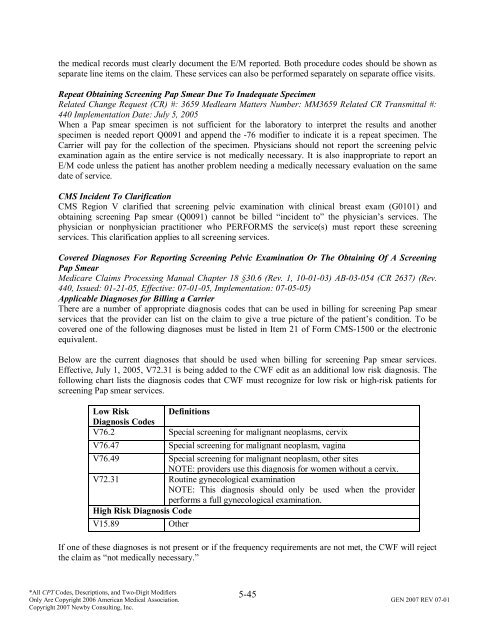
Applicable Diagnoses for Billing a Carrier<br />
There are a number <strong>of</strong> appropriate diagnosis codes that can be used in billing for screening Pap smear<br />
services that the provider can list on the claim to give a true picture <strong>of</strong> the patient’s condition. To be<br />
covered one <strong>of</strong> the following diagnoses must be listed in Item 21 <strong>of</strong> Form CMS-1500 or the electronic<br />
equivalent.<br />
Below are the current diagnoses that should be used when billing for screening Pap smear services.<br />
Effective, July 1, 2005, V72.31 is being added to the CWF edit as an additional low risk diagnosis. The<br />
following chart lists the diagnosis codes that CWF must recognize for low risk or high-risk patients for<br />
screening Pap smear services.<br />
Low Risk Definitions<br />
Diagnosis Codes<br />
V76.2 Special screening for malignant neoplasms, cervix<br />
V76.47 Special screening for malignant neoplasm, vagina<br />
V76.49 Special screening for malignant neoplasm, other sites<br />
NOTE: providers use this diagnosis for women without a cervix.<br />
V72.31 Routine gynecological examination<br />
NOTE: This diagnosis should only be used when the provider<br />
performs a full gynecological examination.<br />
High Risk Diagnosis Code<br />
V15.89 Other<br />
If one <strong>of</strong> these diagnoses is not present or if the frequency requirements are not met, the CWF will reject<br />
the claim as “not medically necessary.”<br />
5-45<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.