The Differentiation of Frontotemporal Dementia ... - McLean Hospital
The Differentiation of Frontotemporal Dementia ... - McLean Hospital
The Differentiation of Frontotemporal Dementia ... - McLean Hospital
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
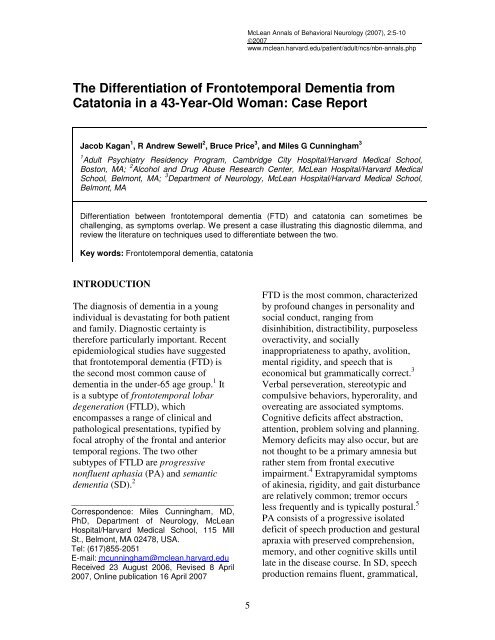
<strong>McLean</strong> Annals <strong>of</strong> Behavioral Neurology (2007), 2:5-10<br />
©2007<br />
www.mclean.harvard.edu/patient/adult/ncs/nbn-annals.php<br />
<strong>The</strong> <strong>Differentiation</strong> <strong>of</strong> <strong>Frontotemporal</strong> <strong>Dementia</strong> from<br />
Catatonia in a 43-Year-Old Woman: Case Report<br />
Jacob Kagan 1 , R Andrew Sewell 2 , Bruce Price 3 , and Miles G Cunningham 3<br />
1 Adult Psychiatry Residency Program, Cambridge City <strong>Hospital</strong>/Harvard Medical School,<br />
Boston, MA; 2 Alcohol and Drug Abuse Research Center, <strong>McLean</strong> <strong>Hospital</strong>/Harvard Medical<br />
School, Belmont, MA; 3 Department <strong>of</strong> Neurology, <strong>McLean</strong> <strong>Hospital</strong>/Harvard Medical School,<br />
Belmont, MA<br />
<strong>Differentiation</strong> between frontotemporal dementia (FTD) and catatonia can sometimes be<br />
challenging, as symptoms overlap. We present a case illustrating this diagnostic dilemma, and<br />
review the literature on techniques used to differentiate between the two.<br />
Key words: <strong>Frontotemporal</strong> dementia, catatonia<br />
INTRODUCTION<br />
<strong>The</strong> diagnosis <strong>of</strong> dementia in a young<br />
individual is devastating for both patient<br />
and family. Diagnostic certainty is<br />
therefore particularly important. Recent<br />
epidemiological studies have suggested<br />
that frontotemporal dementia (FTD) is<br />
the second most common cause <strong>of</strong><br />
dementia in the under-65 age group. 1 It<br />
is a subtype <strong>of</strong> frontotemporal lobar<br />
degeneration (FTLD), which<br />
encompasses a range <strong>of</strong> clinical and<br />
pathological presentations, typified by<br />
focal atrophy <strong>of</strong> the frontal and anterior<br />
temporal regions. <strong>The</strong> two other<br />
subtypes <strong>of</strong> FTLD are progressive<br />
nonfluent aphasia (PA) and semantic<br />
dementia (SD). 2<br />
________________________________________<br />
Correspondence: Miles Cunningham, MD,<br />
PhD, Department <strong>of</strong> Neurology, <strong>McLean</strong><br />
<strong>Hospital</strong>/Harvard Medical School, 115 Mill<br />
St., Belmont, MA 02478, USA.<br />
Tel: (617)855-2051<br />
E-mail: mcunningham@mclean.harvard.edu<br />
Received 23 August 2006, Revised 8 April<br />
2007, Online publication 16 April 2007<br />
FTD is the most common, characterized<br />
by pr<strong>of</strong>ound changes in personality and<br />
social conduct, ranging from<br />
disinhibition, distractibility, purposeless<br />
overactivity, and socially<br />
inappropriateness to apathy, avolition,<br />
mental rigidity, and speech that is<br />
economical but grammatically correct. 3<br />
Verbal perseveration, stereotypic and<br />
compulsive behaviors, hyperorality, and<br />
overeating are associated symptoms.<br />
Cognitive deficits affect abstraction,<br />
attention, problem solving and planning.<br />
Memory deficits may also occur, but are<br />
not thought to be a primary amnesia but<br />
rather stem from frontal executive<br />
impairment. 4 Extrapyramidal symptoms<br />
<strong>of</strong> akinesia, rigidity, and gait disturbance<br />
are relatively common; tremor occurs<br />
less frequently and is typically postural. 5<br />
PA consists <strong>of</strong> a progressive isolated<br />
deficit <strong>of</strong> speech production and gestural<br />
apraxia with preserved comprehension,<br />
memory, and other cognitive skills until<br />
late in the disease course. In SD, speech<br />
production remains fluent, grammatical,<br />
5
<strong>The</strong> <strong>Differentiation</strong> <strong>of</strong> Catatonia from <strong>Frontotemporal</strong><br />
<strong>Dementia</strong> in a 43-Year-Old Woman<br />
J Kagan et al.<br />
and free <strong>of</strong> paraphrasias but<br />
comprehension deteriorates, face<br />
recognition disappears, and patients also<br />
exhibit difficulty in recognizing the<br />
significance <strong>of</strong> objects.<br />
Although catatonia is historically<br />
considered a symptom <strong>of</strong> schizophrenia,<br />
it actually occurs more frequently during<br />
the course <strong>of</strong> a mood disorder, 6 and the<br />
DSM-IV-TR reflects this newer thinking<br />
about catatonia by adding catatonia as a<br />
specifier in mood disorders and as a<br />
separate syndrome occurring secondary<br />
to a general medical disorder. 7 Catatonia<br />
shares a number <strong>of</strong> characteristics with<br />
FTD (see Table 1)—paucity <strong>of</strong> speech,<br />
stereotyped or repetitive behaviors,<br />
purposeless and excessive motor<br />
activity, and echolalia. <strong>Differentiation</strong><br />
between catatonia and FTD may<br />
therefore be challenging. <strong>The</strong> following<br />
case illustrates this clinical overlap and<br />
underscores the critical importance <strong>of</strong><br />
diagnostic certainty for accurate<br />
prognosis and delineation <strong>of</strong> patient and<br />
caregiver psychosocial burden.<br />
CASE REPORT<br />
A 43-year-old married white woman<br />
presented with what her family noted to<br />
be a two-year history <strong>of</strong> progressive<br />
behavioral changes, including flattened<br />
affect, social withdrawal, compulsions,<br />
increased appetite, decreased speech,<br />
depression, and complaints <strong>of</strong> memory<br />
loss. A year prior to admission, a<br />
psychiatric nurse practitioner had noted<br />
that the patient had complained <strong>of</strong><br />
depressed mood, had a significantly<br />
flattened affect, and spoke largely using<br />
“yes” and “no” answers. She had also<br />
become increasingly socially withdrawn,<br />
had recently been fired from her position<br />
as a kindergarten teachers’ aide, and had<br />
begun compulsively showering and<br />
using the dishwasher and clothes washer.<br />
She gained over 50 pounds, frequently<br />
binging on carbohydrate-rich foods. She<br />
had grown increasingly less able to care<br />
for herself and maintain safety within the<br />
house. A few months prior to admission,<br />
the patient accidentally lit a blanket on<br />
fire on the stove and in her confusion,<br />
did not know what to do with the<br />
burning blanket. Shortly thereafter, the<br />
patient’s 23-year-old son moved back<br />
home in order to help care for his mother<br />
while her husband was traveling.<br />
Because <strong>of</strong> her bizarre behavior and<br />
apparent depressed mood and<br />
neurovegetative symptoms, she was<br />
Criterion A. Any <strong>of</strong>: (two required in diagnosis <strong>of</strong> catatonic schizophrenia)<br />
Motoric immobility as evidenced by cataplexy or stupor<br />
Excessive motor activity (apparently purposeless)<br />
Mutism or extreme negativism (motiveless resistance to instructions or maintenance<br />
<strong>of</strong> rigid posture)<br />
Peculiarities <strong>of</strong> voluntary movement (inappropriate or bizarre postures, stereotyped<br />
movements, prominent mannerisms, or prominent grimacing)<br />
Echolalia or echopraxia<br />
Criterion B: Symptoms are the direct result <strong>of</strong> a general medical condition<br />
Criterion C: Symptoms are not better accounted for by another mental disorder<br />
Criterion D: Symptoms do not occur exclusively during the course <strong>of</strong> a delirium<br />
Table 1: DSM-IV-TR criteria for Catatonic Disorder due to a General Medical<br />
Condition 16.<br />
_________________________________<br />
<strong>McLean</strong> Annals <strong>of</strong> Behavioral Neurology<br />
6
<strong>The</strong> <strong>Differentiation</strong> <strong>of</strong> Catatonia from <strong>Frontotemporal</strong><br />
<strong>Dementia</strong> in a 43-Year-Old Woman<br />
J Kagan et al.<br />
diagnosed with depression with<br />
psychotic features, and given<br />
unsuccessful trials <strong>of</strong> citalopram,<br />
venlafaxine, bupropion, nortriptyline,<br />
methylphenidate, and risperidone. She<br />
then underwent 20 sessions <strong>of</strong> bilateral<br />
electroconvulsive therapy (ECT), also<br />
without response. One week following<br />
her course <strong>of</strong> ECT, the patient was<br />
hospitalized for suicidal ideation,<br />
stabilized, and discharged two weeks<br />
later, but soon after discharge again<br />
endorsed thoughts <strong>of</strong> cutting her wrists,<br />
so was brought into our acute psychiatric<br />
care center for evaluation.<br />
<strong>The</strong> patient was a high school graduate<br />
who had completed some college-level<br />
coursework before dropping out to begin<br />
working full time. She had worked as an<br />
aide in an elder care facility and in a<br />
kindergarten class. <strong>The</strong>re was no history<br />
<strong>of</strong> dementia in the family, although the<br />
patient’s mother had a history <strong>of</strong><br />
depression and the patient’s father had<br />
died at age 45 <strong>of</strong> lung cancer.<br />
On examination, she had a severely<br />
flattened affect, echolalia, poverty <strong>of</strong><br />
speech with almost exclusive use <strong>of</strong> the<br />
words “yes” and “no”, and mild<br />
psychomotor agitation. On cognitive<br />
testing she was inattentive and had<br />
impaired recall, abstraction, and a<br />
relative anomia, but preserved<br />
visuospatial functioning. Neurological<br />
exam showed a fine postural tremor in<br />
the patient’s left great toe and foot, but<br />
no rigidity, gait abnormalities, or<br />
primitive reflexes. Basic blood count,<br />
chemistries, liver function tests, and<br />
urinalysis were normal with the<br />
exception <strong>of</strong> a mild normocytic anemia.<br />
Serum vitamin B 12 , folate, erythrocyte<br />
sedimentation rate (ESR),<br />
ceruloplasmin, serum lyme titers, and<br />
autoimmune panel were negative. Rapid<br />
plasma reagin (RPR) was non-reactive.<br />
A lumbar puncture revealed a mildly<br />
elevated opening pressure (24 mm H 2 O),<br />
but normal glucose, protein, and cell<br />
counts, non-reactive CSF syphilis<br />
serology, and no cryptococcal antigens.<br />
An electroencephalogram (EEG)<br />
disclosed low-voltage beta activity,<br />
intermittent low-voltage 9 Hz alpha<br />
activity and low-voltage slowing with<br />
drowsiness, but no epileptiform activity.<br />
MRI revealed minimally increased extracerebral<br />
space, suggesting mild early<br />
involutional changes.<br />
Neuropsychological evaluation that had<br />
been performed four months prior to<br />
admission had demonstrated impaired<br />
attention and concentration, impaired<br />
verbal and narrative memory, and<br />
significant perseveration in her<br />
responses to the <strong>The</strong>matic Apperception<br />
Test and Rorschach Test.<br />
Visuoperceptual and organizational<br />
functions were also below average in<br />
unstructured situations (Rey figure<br />
memory), but normal when structure was<br />
applied (Hooper Test).<br />
On admission, the patient was taking<br />
methylphenidate, venlafaxine, and<br />
risperidone. Lorazepam was added and<br />
titrated to 8 mg a day in the first week <strong>of</strong><br />
admission, but the patient’s presentation<br />
varied little for the remainder <strong>of</strong><br />
hospitalization. She remained minimally<br />
communicative, perseverative, and<br />
echolalic, with flattened affect, persistent<br />
purposeless activity and compulsive<br />
grooming behaviors. Three weeks later,<br />
she was discharged with a presumptive<br />
diagnosis <strong>of</strong> FTD, with plans to followup<br />
in a partial hospitalization/day<br />
program. Venlafaxine was discontinued<br />
with plans to initiate treatment with a<br />
SSRI.<br />
_________________________________<br />
<strong>McLean</strong> Annals <strong>of</strong> Behavioral Neurology<br />
7
<strong>The</strong> <strong>Differentiation</strong> <strong>of</strong> Catatonia from <strong>Frontotemporal</strong><br />
<strong>Dementia</strong> in a 43-Year-Old Woman<br />
J Kagan et al.<br />
DISCUSSION<br />
While an age <strong>of</strong> onset younger than 45 is<br />
unusual in FTD, it can not be used as an<br />
exclusion criterion, as FTD has been<br />
documented in the fourth and even third<br />
decade <strong>of</strong> life. 1, 8 Similarly, while current<br />
hallucinations or delusions are not<br />
typical <strong>of</strong> FTD, they may also be absent<br />
in schizophrenia with predominantly<br />
negative symptoms or a catatonia from a<br />
mood disorder. 8 Delusions and<br />
hallucinations may likewise occur in a<br />
small percentage <strong>of</strong> FTD patients,<br />
although they occur less frequently than<br />
other behavioral symptoms. 9<br />
Multiple imaging modalities have been<br />
used to examine FTD and catatonia,<br />
although none have compared the two<br />
directly. MRI <strong>of</strong> patients with FTD<br />
typically reveals severe frontal, anterior<br />
temporal, and anterior parietal atrophy<br />
with a characteristic asymmetric pattern<br />
<strong>of</strong> atrophy. 10, 11 Specific patterns include<br />
disinhibition associated with<br />
predominant atrophy <strong>of</strong> the orbitomedial<br />
frontal and anterior temporal regions,<br />
apathy associated with extensive frontal<br />
lobe and dorsolateral frontal lobe<br />
atrophy, and semantic impairment<br />
associated with volume loss throughout<br />
the left anterior temporal lobe, right<br />
12, 13<br />
temporal pole and subcallosal gyrus.<br />
While there is some evidence to suggest<br />
prefrontal volume loss in schizophrenic<br />
patients, the evidence is inconclusive, 14<br />
and no studies have reported<br />
morphological abnormalities specific to<br />
catatonia. Single photon emission<br />
computed tomography (SPECT) imaging<br />
has revealed severe reductions in frontal<br />
rCBF in FTD patients, 10 but similar<br />
reductions in rCBF have been found in<br />
catatonic patients in the right lower and<br />
middle prefrontal regions and parietal<br />
cortical regions. 15 Positron emission<br />
tomography (PET) imaging <strong>of</strong> FTD has<br />
revealed glucose hypometabolism<br />
predominantly in the frontal and anterior<br />
temporal lobes and abnormalities in the<br />
cingulate gyri, uncus, insula, and<br />
subcortical structures including basal<br />
17, 18<br />
ganglia and medial thalamic regions.<br />
PET studies in catatonic patients have<br />
been more limited, however, one<br />
examination <strong>of</strong> three patients with<br />
speech-sluggish catatonia revealed<br />
bitemporal and bifrontal glucose<br />
hypometabolism and bi-thalamic<br />
hypermetabolism. 19 To date, multiple<br />
imaging modalities therefore show<br />
significant overlap in findings between<br />
catatonia and FTD—perhaps related to<br />
common frontal neurocircuitry—but<br />
there are no studies directly comparing<br />
the two groups.<br />
CONCLUSION<br />
We describe a patient with the early<br />
onset <strong>of</strong> a number <strong>of</strong> disabling,<br />
progressive symptoms including<br />
prominently flattened affect, paucity <strong>of</strong><br />
speech with maintained grammatical<br />
structure, verbal and physical<br />
perseveration, purposeless motor<br />
activity, and deficits in attention,<br />
concentration, abstraction, and memory.<br />
Laboratory investigations for infectious,<br />
metabolic and inflammatory processes<br />
were unrevealing and MRI suggested<br />
early frontal lobe atrophy. While the<br />
differential diagnosis <strong>of</strong> an early onset<br />
dementing process is large, this patient’s<br />
presentation was highly suggestive <strong>of</strong> a<br />
mood-disorder-associated catatonia or<br />
FTD. We are unaware <strong>of</strong> prior case<br />
reports describing this diagnostic<br />
challenge. <strong>The</strong> importance <strong>of</strong> correct<br />
diagnosis <strong>of</strong> FTD in a young, formerly<br />
_________________________________<br />
<strong>McLean</strong> Annals <strong>of</strong> Behavioral Neurology<br />
8
<strong>The</strong> <strong>Differentiation</strong> <strong>of</strong> Catatonia from <strong>Frontotemporal</strong><br />
<strong>Dementia</strong> in a 43-Year-Old Woman<br />
J Kagan et al.<br />
high-functioning individual can not be<br />
overestimated, given the rapid<br />
progression and limited life expectancy<br />
in this disorder. 20 Age <strong>of</strong> onset, clinical<br />
presentation, and neuroimaging are not<br />
helpful in differentiating catatonia from<br />
FTD, but our patient’s non-response to<br />
both ECT trials and lorazepam challenge<br />
proved diagnostic in this case, as<br />
catatonia has been shown to be<br />
remarkably responsive to both treatment<br />
modalities. 7, 21, 22 Future research directly<br />
comparing catatonia and FTD might<br />
further delineate the diagnostic utility <strong>of</strong><br />
MRI, PET, SPECT and fMRI, but until<br />
then, clinical judgment and judicious<br />
trials <strong>of</strong> lorazepam and ECT are the most<br />
appropriate tools available to clarify this<br />
difficult diagnostic challenge.<br />
REFERENCES<br />
1. Ratnavalli E, Brayne C, Dawson<br />
K, Hodges JR. <strong>The</strong> prevalence <strong>of</strong><br />
frontotemporal dementia.<br />
Neurology. Jun 11<br />
2002;58(11):1615-1621.<br />
2. Neary D, Snowden JS, Gustafson<br />
L, et al. <strong>Frontotemporal</strong> lobar<br />
degeneration: a consensus on<br />
clinical diagnostic criteria.<br />
Neurology. Dec<br />
1998;51(6):1546-1554.<br />
3. Johnson JK, Diehl J, Mendez<br />
MF, et al. <strong>Frontotemporal</strong> lobar<br />
degeneration: demographic<br />
characteristics <strong>of</strong> 353 patients.<br />
Arch Neurol. Jun<br />
2005;62(6):925-930.<br />
4. Tolnay M, Probst A.<br />
<strong>Frontotemporal</strong> lobar<br />
degeneration. An update on<br />
clinical, pathological and genetic<br />
findings. Gerontology. Jan-Feb<br />
2001;47(1):1-8.<br />
5. Rinne JO, Laine M, Kaasinen V,<br />
Norvasuo-Heila MK, Nagren K,<br />
Helenius H. Striatal dopamine<br />
transporter and extrapyramidal<br />
symptoms in frontotemporal<br />
dementia. Neurology. May 28<br />
2002;58(10):1489-1493.<br />
6. Taylor MA, Fink M. Catatonia in<br />
psychiatric classification: a home<br />
<strong>of</strong> its own. Am J Psychiatry. Jul<br />
2003;160(7):1233-1241.<br />
7. Fink M, Taylor M. Catatonia: a<br />
separate category for DSM-IV<br />
Integrative Psychiatry.<br />
1991(7):2-10.<br />
8. Faber R. <strong>Frontotemporal</strong> lobar<br />
degeneration: a consensus on<br />
clinical diagnostic criteria.<br />
Neurology. Sep 22<br />
1999;53(5):1159.<br />
9. Mourik JC, Rosso SM,<br />
Niermeijer MF, Duivenvoorden<br />
HJ, Van Swieten JC, Tibben A.<br />
<strong>Frontotemporal</strong> dementia:<br />
behavioral symptoms and<br />
caregiver distress. Dement<br />
Geriatr Cogn Disord. 2004;18(3-<br />
4):299-306.<br />
10. Varma AR, Adams W, Lloyd JJ,<br />
et al. Diagnostic patterns <strong>of</strong><br />
regional atrophy on MRI and<br />
regional cerebral blood flow<br />
change on SPECT in young onset<br />
patients with Alzheimer's<br />
disease, frontotemporal dementia<br />
and vascular dementia. Acta<br />
Neurol Scand. Apr<br />
2002;105(4):261-269.<br />
11. Boccardi M, Laakso MP,<br />
Bresciani L, et al. <strong>The</strong> MRI<br />
pattern <strong>of</strong> frontal and temporal<br />
brain atrophy in fronto-temporal<br />
dementia. Neurobiol Aging. Jan-<br />
Feb 2003;24(1):95-103.<br />
12. Williams GB, Nestor PJ, Hodges<br />
JR. Neural correlates <strong>of</strong> semantic<br />
_________________________________<br />
<strong>McLean</strong> Annals <strong>of</strong> Behavioral Neurology<br />
9
<strong>The</strong> <strong>Differentiation</strong> <strong>of</strong> Catatonia from <strong>Frontotemporal</strong><br />
<strong>Dementia</strong> in a 43-Year-Old Woman<br />
J Kagan et al.<br />
and behavioural deficits in<br />
frontotemporal dementia.<br />
Neuroimage. Feb 15<br />
2005;24(4):1042-1051.<br />
13. Snowden JS, Neary D, Mann<br />
DM. <strong>Frontotemporal</strong> dementia.<br />
Br J Psychiatry. Feb<br />
2002;180:140-143.<br />
14. Semkovska M, Bedard MA, Stip<br />
E. [Hyp<strong>of</strong>rontality and negative<br />
symptoms in schizophrenia:<br />
synthesis <strong>of</strong> anatomic and<br />
neuropsychological knowledge<br />
and ecological perspectives].<br />
Encephale. Sep-Oct<br />
2001;27(5):405-415.<br />
15. North<strong>of</strong>f G, Steinke R, Nagel<br />
DC, et al. Right lower prefrontoparietal<br />
cortical dysfunction in<br />
akinetic catatonia: a combined<br />
study <strong>of</strong> neuropsychology and<br />
regional cerebral blood flow.<br />
Psychol Med. May<br />
2000;30(3):583-596.<br />
16. American Psychiatric<br />
Association. Diagnostic and<br />
Statistical Manual <strong>of</strong> Mental<br />
Disorders, 4th edition, Text<br />
Revision. Washington, DC:<br />
American Psychiatric<br />
Association; 2000.<br />
17. Ishii K, Sakamoto S, Sasaki M,<br />
et al. Cerebral glucose<br />
metabolism in patients with<br />
frontotemporal dementia. J Nucl<br />
Med. Nov 1998;39(11):1875-<br />
1878.<br />
18. Jeong Y, Cho SS, Park JM, et al.<br />
18F-FDG PET findings in<br />
frontotemporal dementia: an<br />
SPM analysis <strong>of</strong> 29 patients. J<br />
Nucl Med. Feb 2005;46(2):233-<br />
239.<br />
19. Lauer M, Schirrmeister H,<br />
Gerhard A, et al. Disturbed<br />
neural circuits in a subtype <strong>of</strong><br />
chronic catatonic schizophrenia<br />
demonstrated by F-18-FDG-PET<br />
and F-18-DOPA-PET. J Neural<br />
Transm. 2001;108(6):661-670.<br />
20. Hodges JR, Davies R, Xuereb J,<br />
Kril J, Halliday G. Survival in<br />
frontotemporal dementia.<br />
Neurology. Aug 12<br />
2003;61(3):349-354.<br />
21. Rohland BM, Carroll BT, Jacoby<br />
RG. ECT in the treatment <strong>of</strong> the<br />
catatonic syndrome. J Affect<br />
Disord. Dec 1993;29(4):255-261.<br />
22. Bush G, Fink M, Petrides G,<br />
Dowling F, Francis A. Catatonia.<br />
II. Treatment with lorazepam and<br />
electroconvulsive therapy. Acta<br />
Psychiatr Scand. Feb<br />
1996;93(2):137-143.<br />
_________________________________<br />
<strong>McLean</strong> Annals <strong>of</strong> Behavioral Neurology<br />
10