Guidelines For Professional Working Standards Ultrasound Practice
Guidelines For Professional Working Standards Ultrasound Practice
Guidelines For Professional Working Standards Ultrasound Practice
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
2.3 <strong>Guidelines</strong> Relevant To Gynaecological Examinations<br />
The type of examination carried out, i.e. using vaginal (EV) and/or trans-abdominal (TA) techniques should<br />
be directed by the clinical presentation of the patient. As discussed in Section 1.5 a full explanation of<br />
the techniques should be given to the patient and appropriate consent sought. The need for a chaperone<br />
should also be considered. (Refer to Section 1.6).<br />
The sonographer should consider the following:<br />
• obtaining information regarding the patient’s previous medical and menstrual history including stage<br />
and cycle<br />
• establishing information relating to any medication e.g. oral contraceptive pill, hormone replacement<br />
therapy, Tamoxifen<br />
• that EV ultrasound is the recommended technique for detailed assessment of the endometrium<br />
(e.g. referral for post menopausal bleeding) and ovaries (e.g. referral for polycystic ovaries)<br />
• using colour flow mapping and/or power Doppler in appropriate clinical presentations<br />
e.g. the assessment of myometrial vascularity, ovarian angiogenesis, endometrial vascularity<br />
• using 3D ultrasound in the assessment of pathology and congenital malformations of the uterus<br />
and ovaries<br />
Observations<br />
The anatomical structures which the sonographer should normally examine during a gynaecological<br />
examination should be in accordance with the clinical information given and are shown in Table 3. This<br />
should include assessment of size, outline and ultrasound characteristics.<br />
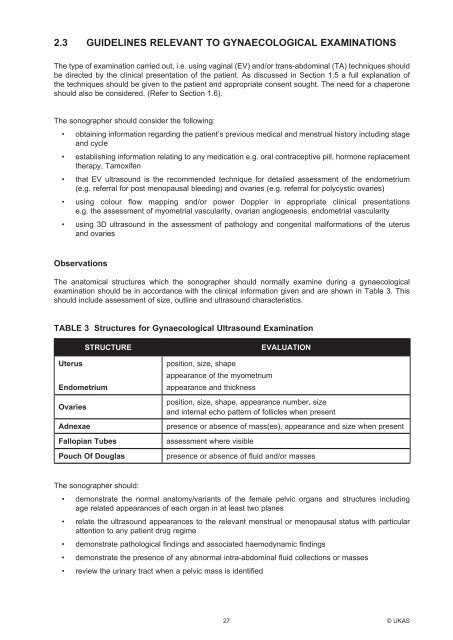
TABLE 3 Structures for Gynaecological <strong>Ultrasound</strong> Examination<br />
STRUCTURE<br />
Uterus<br />
Endometrium<br />
Ovaries<br />
Adnexae<br />
Fallopian Tubes<br />
Pouch Of Douglas<br />
position, size, shape<br />
appearance of the myometrium<br />
appearance and thickness<br />
EVALUATION<br />
position, size, shape, appearance number, size<br />
and internal echo pattern of follicles when present<br />
presence or absence of mass(es). appearance and size when present<br />
assessment where visible<br />
presence or absence of fluid and/or masses<br />
The sonographer should:<br />
• demonstrate the normal anatomy/variants of the female pelvic organs and structures including<br />
age related appearances of each organ in at least two planes<br />
• relate the ultrasound appearances to the relevant menstrual or menopausal status with particular<br />
attention to any patient drug regime<br />
• demonstrate pathological findings and associated haemodynamic findings<br />
• demonstrate the presence of any abnormal intra-abdominal fluid collections or masses<br />
• review the urinary tract when a pelvic mass is identified<br />
27 © UKAS