Congenital Cystic Adenomatoid Malformation - SSM Cardinal ...
Congenital Cystic Adenomatoid Malformation - SSM Cardinal ...
Congenital Cystic Adenomatoid Malformation - SSM Cardinal ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
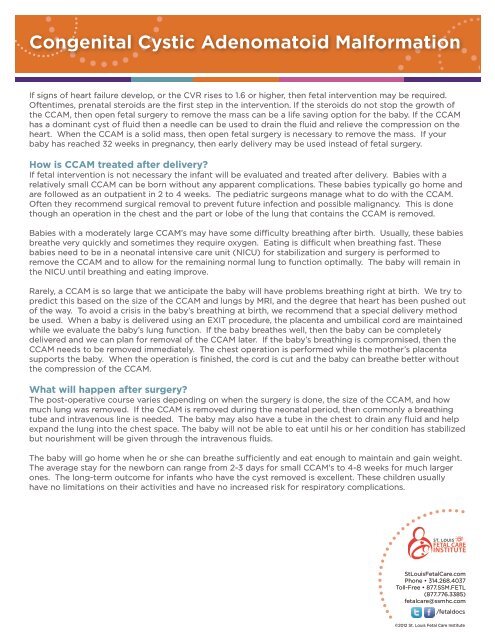
<strong>Congenital</strong> <strong>Cystic</strong> <strong>Adenomatoid</strong> <strong>Malformation</strong><br />
If signs of heart failure develop, or the CVR rises to 1.6 or higher, then fetal intervention may be required.<br />
Oftentimes, prenatal steroids are the first step in the intervention. If the steroids do not stop the growth of<br />
the CCAM, then open fetal surgery to remove the mass can be a life saving option for the baby. If the CCAM<br />
has a dominant cyst of fluid then a needle can be used to drain the fluid and relieve the compression on the<br />
heart. When the CCAM is a solid mass, then open fetal surgery is necessary to remove the mass. If your<br />
baby has reached 32 weeks in pregnancy, then early delivery may be used instead of fetal surgery.<br />
How is CCAM treated after delivery<br />
If fetal intervention is not necessary the infant will be evaluated and treated after delivery. Babies with a<br />
relatively small CCAM can be born without any apparent complications. These babies typically go home and<br />
are followed as an outpatient in 2 to 4 weeks. The pediatric surgeons manage what to do with the CCAM.<br />
Often they recommend surgical removal to prevent future infection and possible malignancy. This is done<br />
though an operation in the chest and the part or lobe of the lung that contains the CCAM is removed.<br />
Babies with a moderately large CCAM’s may have some difficulty breathing after birth. Usually, these babies<br />
breathe very quickly and sometimes they require oxygen. Eating is difficult when breathing fast. These<br />
babies need to be in a neonatal intensive care unit (NICU) for stabilization and surgery is performed to<br />
remove the CCAM and to allow for the remaining normal lung to function optimally. The baby will remain in<br />
the NICU until breathing and eating improve.<br />
Rarely, a CCAM is so large that we anticipate the baby will have problems breathing right at birth. We try to<br />
predict this based on the size of the CCAM and lungs by MRI, and the degree that heart has been pushed out<br />
of the way. To avoid a crisis in the baby’s breathing at birth, we recommend that a special delivery method<br />
be used. When a baby is delivered using an EXIT procedure, the placenta and umbilical cord are maintained<br />
while we evaluate the baby’s lung function. If the baby breathes well, then the baby can be completely<br />
delivered and we can plan for removal of the CCAM later. If the baby’s breathing is compromised, then the<br />
CCAM needs to be removed immediately. The chest operation is performed while the mother’s placenta<br />
supports the baby. When the operation is finished, the cord is cut and the baby can breathe better without<br />
the compression of the CCAM.<br />
What will happen after surgery<br />
The post-operative course varies depending on when the surgery is done, the size of the CCAM, and how<br />
much lung was removed. If the CCAM is removed during the neonatal period, then commonly a breathing<br />
tube and intravenous line is needed. The baby may also have a tube in the chest to drain any fluid and help<br />
expand the lung into the chest space. The baby will not be able to eat until his or her condition has stabilized<br />
but nourishment will be given through the intravenous fluids.<br />
The baby will go home when he or she can breathe sufficiently and eat enough to maintain and gain weight.<br />
The average stay for the newborn can range from 2-3 days for small CCAM’s to 4-8 weeks for much larger<br />
ones. The long-term outcome for infants who have the cyst removed is excellent. These children usually<br />
have no limitations on their activities and have no increased risk for respiratory complications.<br />
StLouisFetalCare.com<br />
Phone • 314.268.4037<br />
Toll-Free • 877.<strong>SSM</strong>.FETL<br />
(877.776.3385)<br />
fetalcare@ssmhc.com<br />
/fetaldocs<br />
©2012 St. Louis Fetal Care Institute