Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
various scans, including a single-photon emission CT (SPECT), positron emission<br />
tomography (PET), CT and MRI. Paugh <strong>the</strong>n merges <strong>the</strong>se scans to develop a<br />
detailed brain map, giving <strong>the</strong> surgical team a view of every angle of <strong>the</strong> brain.<br />
Unlike 2-D imagery, this 3-D model provides more precise location of <strong>the</strong> abnormal<br />
brain tissue that’s causing seizures.<br />
This technology can reduce <strong>the</strong> amount of electrodes used during surgery, allow<br />
doctors to see a more precise location of eloquent brain function (i.e., speech or<br />
motor function) and ultimately lead to more successful operations. The 3-D image<br />
pinpointed <strong>the</strong> area of seizure origin in Micheal’s brain and showed <strong>the</strong> region of <strong>the</strong><br />
brain responsible for speech.<br />
For Micheal and his family, <strong>the</strong> technology gave <strong>the</strong>m hope of ending 10 long<br />
years of anguish and fear that included three different stints in a mental hospital.<br />
Micheal was a unique case. Years of uncontrolled seizures had made both of<br />
his temporal lobes abnormal. The best surgical candidates have only one area of<br />
abnormality; Micheal had two. The odds of becoming seizure free decrease when<br />
multiple regions are involved.<br />
“With all <strong>the</strong> history of behavior problems and evidence of bilateral temporal<br />
lobe abnormalities, Micheal was not <strong>the</strong> best surgical candidate,” Dr. Perry said.<br />
“Removal of one bad temporal lobe does not guarantee that <strong>the</strong> o<strong>the</strong>r damaged<br />
temporal lobe will not cause seizures. With 3-D imaging, we were able to show that<br />
<strong>the</strong> left side was <strong>the</strong> worst side and <strong>the</strong> true area of seizures onset. We never found<br />
a seizure that came from <strong>the</strong> right side. We also knew <strong>the</strong> left side of his brain was<br />
his dominant hemisphere and where language function resides. After we placed<br />
<strong>the</strong> electrodes on his temporal lobe, I was able to map out where his language was<br />
located. We were able to do a detailed surgery that removed <strong>the</strong> tissue that caused<br />
seizures, but stopped short of involving an area responsible for speech.”<br />
Without surgery and with <strong>the</strong> temporal lobe on <strong>the</strong> left side of Micheal’s brain<br />
already bad, Dr. Perry believes that eventually <strong>the</strong> right temporal lobe would have<br />
worsened. Without surgery, Micheal would have had a hard time maintaining a job<br />
and probably would not finish school because of missed days due to his psychiatric<br />
problems and seizures. His parents feared that Micheal would spend <strong>the</strong> rest of his<br />
life in some type of facility.<br />
Weighing <strong>the</strong>ir options, including that Micheal’s behavior could become worse, <strong>the</strong><br />
Driggars family did not hesitate. They felt <strong>the</strong> risk was worth <strong>the</strong> possible reward and<br />
Micheal made <strong>the</strong> final decision. “I want <strong>the</strong> old Micheal back,” he told his parents.<br />
With <strong>the</strong> detailed information from <strong>the</strong> 3-D image in hand, neurosurgeon David<br />
Donahue, M.D., was able to remove <strong>the</strong> left temporal lobe without harming Micheal’s<br />
ability to speak.<br />
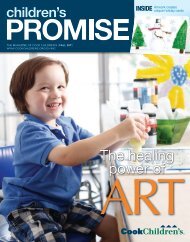
Since <strong>the</strong> operation, <strong>the</strong> old Micheal has returned. He has not had a seizure since<br />
<strong>the</strong> operation and his depression and angry outbursts are gone.<br />
“It was like a weight had been lifted off of us,” Brandy said. “For 10 years, Micheal<br />
was miserable. All he ever wanted was to be normal. He said, ‘I want to be able to<br />
drive one day. I want to do all those things that o<strong>the</strong>r kids do. What I thought was<br />
amazing was that after our first visit with Dr. Perry, we were in <strong>the</strong> car on <strong>the</strong> way<br />
home and Micheal said, ‘Mom, I think God sent us to Dr. Perry.’”<br />
Nowadays, Micheal shows an interest in art, music and working out. At a recent<br />
visit to <strong>Cook</strong> Children’s, Micheal flexed his bicep, and showed off his recent weight<br />
loss. He has a new focus on appearance that he shares with most 15-year-old boys.<br />
After receiving deserved compliments for his muscles, Micheal flashed a big grin.<br />
Behind Micheal’s smile <strong>the</strong>re’s an experienced and dedicated team of<br />
neurologists, neurosurgeons, neuroradiologists, neuropsychologists, nurses and a<br />
software bio-engineer which make up <strong>the</strong> <strong>Cook</strong> Children’s Comprehensive Epilepsy<br />
Program.<br />
“For so long he did not smile - he had one emotion, only anger,” Brandy Driggars<br />
said of her son. “Now he has <strong>the</strong> huge smile on his face, and he laughs a lot.”<br />
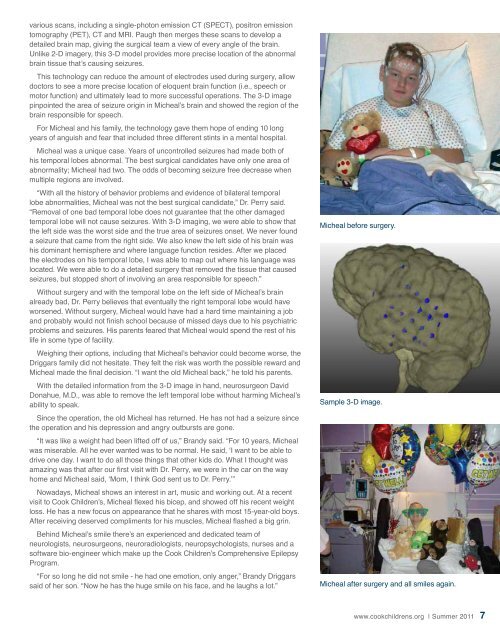
Micheal before surgery.<br />
Sample 3-D image.<br />
Micheal after surgery and all smiles again.<br />
www.cookchildrens.org | Summer 2011 7