Model Answers Microbiology Written examinations 2007 - RCPA
Model Answers Microbiology Written examinations 2007 - RCPA
Model Answers Microbiology Written examinations 2007 - RCPA
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
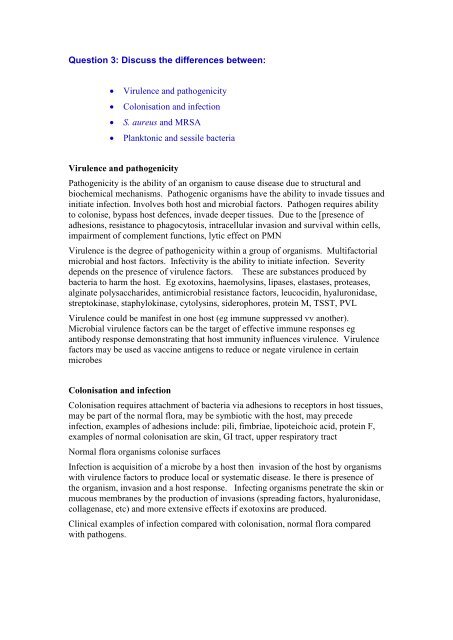
Question 3: Discuss the differences between:<br />
<br />
<br />
<br />
<br />
Virulence and pathogenicity<br />
Colonisation and infection<br />
S. aureus and MRSA<br />
Planktonic and sessile bacteria<br />
Virulence and pathogenicity<br />
Pathogenicity is the ability of an organism to cause disease due to structural and<br />
biochemical mechanisms. Pathogenic organisms have the ability to invade tissues and<br />
initiate infection. Involves both host and microbial factors. Pathogen requires ability<br />
to colonise, bypass host defences, invade deeper tissues. Due to the [presence of<br />
adhesions, resistance to phagocytosis, intracellular invasion and survival within cells,<br />
impairment of complement functions, lytic effect on PMN<br />
Virulence is the degree of pathogenicity within a group of organisms. Multifactorial<br />
microbial and host factors. Infectivity is the ability to initiate infection. Severity<br />
depends on the presence of virulence factors. These are substances produced by<br />
bacteria to harm the host. Eg exotoxins, haemolysins, lipases, elastases, proteases,<br />
alginate polysaccharides, antimicrobial resistance factors, leucocidin, hyaluronidase,<br />
streptokinase, staphylokinase, cytolysins, siderophores, protein M, TSST, PVL<br />
Virulence could be manifest in one host (eg immune suppressed vv another).<br />
Microbial virulence factors can be the target of effective immune responses eg<br />
antibody response demonstrating that host immunity influences virulence. Virulence<br />
factors may be used as vaccine antigens to reduce or negate virulence in certain<br />
microbes<br />
Colonisation and infection<br />
Colonisation requires attachment of bacteria via adhesions to receptors in host tissues,<br />
may be part of the normal flora, may be symbiotic with the host, may precede<br />
infection, examples of adhesions include: pili, fimbriae, lipoteichoic acid, protein F,<br />
examples of normal colonisation are skin, GI tract, upper respiratory tract<br />
Normal flora organisms colonise surfaces<br />
Infection is acquisition of a microbe by a host then invasion of the host by organisms<br />
with virulence factors to produce local or systematic disease. Ie there is presence of<br />
the organism, invasion and a host response. Infecting organisms penetrate the skin or<br />
mucous membranes by the production of invasions (spreading factors, hyaluronidase,<br />
collagenase, etc) and more extensive effects if exotoxins are produced.<br />
Clinical examples of infection compared with colonisation, normal flora compared<br />
with pathogens.