Tissue Banking Overview: Washington University Medical Center
Tissue Banking Overview: Washington University Medical Center
Tissue Banking Overview: Washington University Medical Center
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
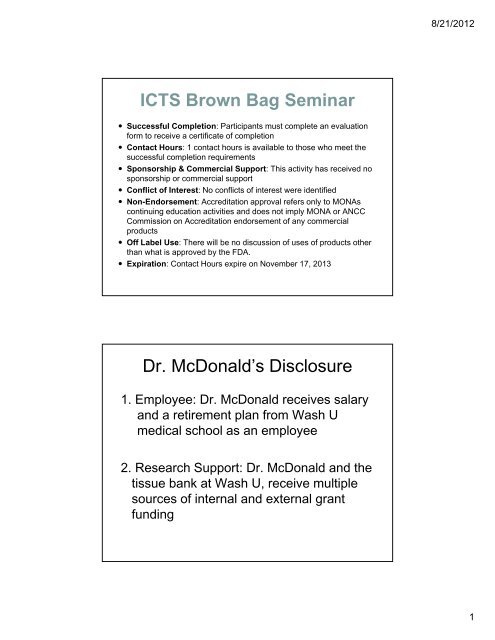
8/21/2012<br />
ICTS Brown Bag Seminar<br />
• Successful Completion: Participants must complete an evaluation<br />
form to receive a certificate of completion<br />
• Contact Hours: 1 contact hours is available to those who meet the<br />
successful completion requirements<br />
• Sponsorship & Commercial Support: This activity has received no<br />
sponsorship or commercial support<br />
• Conflict of Interest: No conflicts of interest were identified<br />
• Non-Endorsement: Accreditation approval refers only to MONAs<br />
continuing education activities and does not imply MONA or ANCC<br />
Commission on Accreditation endorsement of any commercial<br />
products<br />
• Off Label Use: There will be no discussion of uses of products other<br />
than what is approved by the FDA.<br />
• Expiration: Contact Hours expire on November 17, 2013<br />
Dr. McDonald’s Disclosure<br />
1. Employee: Dr. McDonald receives salary<br />
and a retirement plan from Wash U<br />
medical school as an employee<br />
2. Research Support: Dr. McDonald and the<br />
tissue bank at Wash U, receive multiple<br />
sources of internal and external grant<br />
funding<br />
1
8/21/2012<br />
<strong>Tissue</strong> Procurement Facility background:<br />
<strong>Washington</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong><br />
Sandra A. McDonald, MD<br />
Department of Pathology and Immunology,<br />
<strong>Washington</strong> <strong>University</strong> School of Medicine, St. Louis, Missouri<br />
Brown Bag Lunch<br />
Seminar Series<br />
August 30, 2012<br />
Summary<br />
• Biobanking science overview<br />
• Resources, mission, offered procedures of<br />
biorepository, and key contacts/ URLs<br />
• General principles of specimen ordering,<br />
procurement, evaluation, processing, and QA<br />
• Precautions for specimen banking<br />
• Pathologist roles in banking<br />
• Specimen procurement<br />
• Digital pathology<br />
2
8/21/2012<br />
<strong>Washington</strong> <strong>University</strong><br />
<strong>Medical</strong> <strong>Center</strong><br />
Biorepository<br />
• A centralized resource for biospecimens and laboratory<br />
procedures, started in 1997 as effort with Siteman Cancer Ctr.<br />
• Laboratory for Translational Pathology /<strong>Tissue</strong> Procurement<br />
Core) , 14 FTEs<br />
• ~500,000 samples (tissues and biofluids) derived from a<br />
variety of internal and external collection protocols (~70 open<br />
currently) and clinical trials; traditional focus is neoplasia<br />
• Collection, storage, quality assurance and scientific<br />
utilization/impact of biospecimens, to better understand the<br />
molecular / genomic basis of cancer and translations to pt. care<br />
• Fee-for-service mechanism, usage on a request-driven basis<br />
• Resource limited currently<br />
Wash U Biorepository Workflow<br />
Incoming<br />
tissue,<br />
blood ,<br />
and other<br />
biofluids<br />
SAMPLE ACCESSION,<br />
PREP & PROCESSING<br />
Some samples<br />
Most samples<br />
Some samples<br />
Investigator<br />
requests<br />
(samples<br />
pulled from<br />
storage in<br />
response)<br />
STORAGE<br />
(mainly frozen<br />
biospecimens, few<br />
paraffin blocks)<br />
HISTOLOGY<br />
Some samples<br />
Sections and/or<br />
fresh-frozen<br />
tissues<br />
disbursed to<br />
investigators<br />
Samples disbursed to<br />
investigators; however, for<br />
most samples, histology<br />
or molecular workup is<br />
needed first (black arrows)<br />
MOLECULAR<br />
Make RNA & DNA<br />
Sample flow within repository<br />
Sample Entry Points<br />
Sample Exit Points<br />
Key component of repository<br />
Molecular samples disbursed to<br />
investigators (following isolation<br />
and QA)<br />
3
8/21/2012<br />
<strong>Washington</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong> Biorepository<br />
WU Laboratory for Translational Pathology<br />
Watson<br />
(legacy director)<br />
McDonald<br />
(director)<br />
Brink<br />
(processing)<br />
Holtschlag<br />
(manager)<br />
Fox<br />
(regulatory)<br />
Mulvihill<br />
(informatics)<br />
Granderson<br />
(processing)<br />
Henson<br />
(processing)<br />
DeSchryver<br />
(pathology)<br />
Zhang<br />
(molecular)<br />
Gaudin<br />
(molecular)<br />
Reagan<br />
(processing)<br />
Archer<br />
(processing)<br />
Cruise<br />
(histology)<br />
Rozycki<br />
(molecular)<br />
Oertwig<br />
(processing)<br />
Processing Histology Molecular<br />
accessioning<br />
storage<br />
protocols and kits<br />
general tumor<br />
bank archive<br />
tissue processing<br />
tissue sectioning<br />
laser<br />
microdissection<br />
DNA and RNA<br />
preparation and<br />
quality and<br />
quantity<br />
determinations<br />
4
8/21/2012<br />
BJCIH<br />
Laboratory for Translational Pathology/<br />
<strong>Tissue</strong> Procurement Core<br />
Phone: 454-7605 /454-7615<br />
Email: tbank@pathology.wustl.edu<br />
Location: Room 2454 Kingshighway Bldg<br />
<strong>Washington</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong> Biorepository<br />
‣ Prospective procurement for research protocols<br />
‣ Archival specimen bank<br />
‣ Specimen processing<br />
‣ Laser capture microdissection<br />
‣ RNA and DNA prep and QA analysis<br />
‣ Biospecimen informatics<br />
‣ Pathology interpretation/ slide review<br />
‣ Scientific consultation<br />
‣ Consultation on informed consent, IRB<br />
procedures<br />
5
8/21/2012<br />
Why Use a Core Facility ?<br />
• More efficient use of personnel, space, and resources<br />
• Use of uniform processes and policies across all<br />
biospecimen-related activities, including those required by<br />
regulatory or advisory bodies<br />
• Creates a neutral entity that can oversee the distribution and<br />
utilization of resources in a coordinated fashion, while<br />
appropriately protecting patient privacy<br />
• Preserves biospecimens and associated data beyond the<br />
tenure or legacy of individual investigators or studies<br />
Why Bank Specimens ?<br />
• Molecular analysis of animal models and cell lines have<br />
limitations with regard to clinical relevance.<br />
• Infrequent disease presentations must be collected over time.<br />
• Aged specimens with clinical follow-up are more useful for<br />
clinical correlative studies.<br />
• Rare and valuable specimens should be stored and distributed<br />
judiciously.<br />
• Specimens and data must be quality-controlled.<br />
• Resources are needed to initiate funded research projects.<br />
• Basic research findings can be translated into clinical<br />
(diagnostic) tools.<br />
6
8/21/2012<br />
Classification of banked specimens for billing purposes<br />
Public - is a discard from surgical pathology. Consent is either waived or, if feasible, is<br />
obtained retroactively from the patient (i.e. at some time point following surgery) by the<br />
research nursing coordinator for the <strong>Tissue</strong> Procurement Core. SCC supports the total<br />
cost of procurement, deposit & storage. The investigator/study protocol requesting<br />
withdrawal of public samples assumes the cost of withdrawal procedures.<br />
Semi‐Public ‐ Collected per an approved research protocol. The scientist supports<br />
the cost of protocol approval and sample procurement. The SCC supports the cost of<br />
sample processing for deposit and storage costs. Semi‐public samples are considered<br />
owned by both SCC and the principal investigator (PI) of the consent form. The<br />
investigator/protocol requesting withdrawal of semi‐public sample assumes the cost of<br />
withdrawal procedures. Sample usage not restricted to a certain investigator or group.<br />
Private ‐ collected per an approved protocol. The PI supports the cost of protocol<br />
approval as well as the cost of sample procurement, storage & withdrawal. A private<br />
sample may not be withdrawn by another investigator unless the original protocol PI<br />
agrees.<br />
<strong>Tissue</strong> Utilization Committee<br />
• Has been established for the <strong>Tissue</strong> Procurement Core, and<br />
implementation is awaiting final refinements of informatics<br />
• Committee provides an independent assessment of resource usage vs.<br />
benefit/impact<br />
• Need driven by Siteman Cancer <strong>Center</strong> and CAP directives<br />
• Committee: 1 chair, 2 statisticians (ad hoc), and 9 members<br />
drawn from Siteman Cancer <strong>Center</strong> community<br />
• Initially, role of this committee will be to review public bank<br />
samples; once efficient flow is established, role will expand to<br />
semi-public and even private samples<br />
• Committee can also help assess the appropriateness of sample disposal,<br />
and storage demands for new protocols<br />
7
8/21/2012<br />
Fee for service schedule<br />
• In an effort to better meet its operational expenses, the <strong>Tissue</strong><br />
Procurement Core has initiated a fee-for-service schedule<br />
• Labor, reagents/consumables, and/or infrastructure components<br />
underlie the charges<br />
• Fee-for-service schedule is shared with investigators when they<br />
contact the bank for protocol initiation or sample withdrawal<br />
• Examples of charges:<br />
Service Unit Actual Cost<br />
Ficoll Processing<br />
10 ml peripheral blood or 2 ml BM or<br />
10^7 cells $76.80<br />
Ficoll Processing (large scale)<br />
60 ml peripheral blood or 12 ml BM or<br />
10^8 cells $101.78<br />
CPT Tube Processing and Cell Freezing per tube $31.97<br />
Cell Cryoperservation per 10^7 cells $4.28<br />
Cell Processing and Cryopreservation<br />
10‐20ml peripheral blood or 2‐5ml of<br />
BM $31.67<br />
Laser capture microscope tech time per hour $59.95<br />
Laser capture microscope use per hour $29.95<br />
DNA prep and QA from cell pellet per sample $17.29<br />
<strong>Tissue</strong> Fixation and Embedding $15.91<br />
Storage under liquid N2 vapor per stored aliquot per year $0.21<br />
<strong>Tissue</strong> banking and clinical trials<br />
• Is important for tissue banking, especially for<br />
pharmacogenomics and correlative biomarker studies<br />
Objectives:<br />
• relate biomarkers to onset, course, and outcome of disease<br />
and the level of response to various treatments<br />
• predict who will respond to therapy<br />
• modification of expression of targets/other biomarkers in<br />
response to therapy<br />
• future use of tissues for hypotheses not known at present<br />
(depending on consent scope-of-use)<br />
8
8/21/2012<br />
Specimen Collection<br />
• Diseased <strong>Tissue</strong><br />
Genetic, biochemical, or histological analysis of<br />
disease process<br />
Sampling Site<br />
Fixed vs. Frozen (Dictates storage needs<br />
and future utilization)<br />
Fixation Type<br />
Embedding Medium<br />
• Serum /<br />
Plasma<br />
Biochemical<br />
studies<br />
Aliquot and<br />
freeze<br />
• Peripheral Leukocytes/Bone Marrow<br />
Genomic (germ line) analysis; Occult<br />
tumor cell detection<br />
Whole blood<br />
Enriched nucleated cell fraction<br />
Density gradient centrifugation<br />
Cryopreservation / Immortalization<br />
• CSF and<br />
other fluids<br />
Cytospin<br />
Freeze<br />
Terminology for collected/ banked samples<br />
Identified – Labeled with personal identifiers such as name or SSN<br />
Coded – Labeled with a clinical trial subject number, investigator has<br />
access to the code<br />
De-identified – Labeled with a unique second number; link between this<br />
second number and the clinical trial subject number is maintained in a<br />
highly secure database, and generally unavailable to investigators and<br />
patients<br />
Anonymized – Link described above is irreversibly removed, so that<br />
specimens cannot be traced back to patient identities by anyone<br />
Anonymous – Samples without personal identifiers, and whose identity<br />
is unknown. An increasingly nebulous concept these days, with the<br />
advent of whole exome and genome sequencing, where the data is<br />
increasingly viewed as essentially the patient’s identity<br />
9
8/21/2012<br />
Informed consent for general tissue<br />
banking collection<br />
• Specimens collected as part of routine care<br />
• Specimens not needed for clinical management<br />
• Bank representative may access clinical data<br />
• May elect to be contacted for future studies<br />
• Investigator never provided with patient identity<br />
Online ordering system<br />
http://pathology.wustl.edu/research/cores/ltp/request.php<br />
• Wash U biorepository (2/2011) established a web-based specimen ordering<br />
system<br />
• Efficiency and tracking advantages<br />
• Not part of ca<strong>Tissue</strong> Suite program<br />
• Successful design needed consideration of lab workflow and customer needs<br />
• “Front end” – user-initiated, password-protected ordering request form<br />
• “Back end” – request tracking system accessible only to lab<br />
• User enters profile, project, and request details, and then request is assigned<br />
a number as it moves through the system<br />
• Path of a request depends on the three major categories of provided services:<br />
• Submit investigator's own samples for lab procedures<br />
• Request specific sample IDs distributed directly from the repository<br />
• Request general tissue/organ types or diseases<br />
10
8/21/2012<br />
Advantages of<br />
online system<br />
• Accessibility to research community – as a link on<br />
departmental website<br />
• Automatic capture of required information<br />
• Reliable documentation (what was requested, and who)<br />
• Tracking of stage within laboratory<br />
• Easier compliation of metrics related to requests<br />
• Possibility of additional levels of monitoring/ review if<br />
needed<br />
• Status communications to requestors – through the “back<br />
end” updating the “front end”<br />
ca<strong>Tissue</strong> Suite v1.2<br />
• Web-based application for biospecimen information management<br />
• Professional approach to software design<br />
• Open source / Open access (Free)<br />
• Iterative development cycle (Always improving)<br />
• Flexible to meet the needs of varying biobank environments<br />
• Multiple sources of electronic and human support<br />
11
8/21/2012<br />
Anatomic pathology correlation, including gross<br />
and microscopic evaluation, is critical to the<br />
success of research tissue banks.<br />
Such correlation facilitates<br />
• optimal sample procurement from gross<br />
specimens, especially surgical pathology<br />
• optimal selection and use of banked tissue<br />
samples to meet research objectives.<br />
McDonald SA. Principles of research tissue banking and specimen evaluation from<br />
the pathologist's perspective. Biopreservation and Biobanking, 8: 197-201, 2010.<br />
<strong>Tissue</strong> processing<br />
12
8/21/2012<br />
Specimen QA<br />
• Specimen identity<br />
• Important using whole genome technologies<br />
• Histological review of tissue specimens<br />
• <strong>Tissue</strong> viability, cellularity, disease representation<br />
• Conflicts in diagnosis<br />
• Molecular review of specimens<br />
• A260/A280 and A260/A230 ratios<br />
• Gel electrophoresis results<br />
• Feedback to biospecimen source / collectors<br />
Principles of specimen collection<br />
‣Specific, reproducible criteria are the most<br />
important, which are standardized as much as<br />
possible across the collection sites<br />
‣Clear, practical procedures are needed, with<br />
good communication essential<br />
‣<strong>Tissue</strong> bank users should understand<br />
collection practices and how they might<br />
impact their studies<br />
13
8/21/2012<br />
Specimen Collection<br />
• Dedicated personnel on call to collect biospecimens from<br />
BJH OR, surgical pathology suite, and clinics.<br />
• Self-contained biospecimen procurement kits and<br />
procurement tutorials to collect off-site.<br />
• Collection of surgically resected tissue, peripheral blood,<br />
bone marrow, needle biopsies, and lavage fluid.<br />
Specimen Preservation<br />
• Snap Freezing<br />
Difficult / Requires resources<br />
Poor histology<br />
Expensive storage<br />
Best molecular yield<br />
• Ethanol Fixation / LMPE<br />
Difficult / Requires resources<br />
Stability issues<br />
Good histology<br />
Cheap storage<br />
Good molecular yield<br />
• “RNALater”<br />
Still need to freeze / embed<br />
Poor histology<br />
Convenient<br />
Good nucleic acid yield<br />
• Formalin Fixation / PE<br />
Poor molecular yield<br />
Standardized<br />
Stable<br />
Excellent histology<br />
14
8/21/2012<br />
Specimen Storage<br />
• Ultralow mechanical freezers (-80°C)<br />
Cheaper (Long Term)<br />
Error Prone<br />
Less Stable<br />
• Liquid nitrogen (-130°C)<br />
More Stable<br />
Less Error Prone<br />
More Expensive<br />
• Vacuum sealed (4°C)<br />
Paraffin Blocks / Slides<br />
No Data<br />
Gross procurement of tissues for research banking<br />
‣ Academic hospitals with research tissue repositories<br />
often derive many internal specimen acquisitions from<br />
their site's surgical pathology service<br />
‣ Typically, such acquisitions come from appropriately<br />
consented tissue discards sampled from surgical<br />
resections<br />
‣<strong>Tissue</strong>, if not banked, would otherwise be thrown<br />
away since it is not needed for clinical diagnosis<br />
‣ Surgical pathology has patient care as its primary<br />
mission, so competing needs for tissue inevitable arise:<br />
preserving adequate tissue for clinical diagnosis is key<br />
‣ Involvement of trained pathology personnel is<br />
important<br />
McDonald SA, Chernock RD, Leach TA, Kahn AA, Yip JH, Rossi J, Pfeifer JD. Procurement of<br />
human tissues for research banking in the surgical pathology laboratory: prioritization practices at<br />
<strong>Washington</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong>. In press, Biopreservation and Biobanking, 2011.<br />
15
8/21/2012<br />
Sample for<br />
diagnostic<br />
surgical<br />
pathology<br />
Yes, more tissue needed<br />
for microscopic<br />
diagnosis<br />
In effect, every region<br />
of every specimen is<br />
subjected to a threeway<br />
decision in the<br />
gross room!<br />
Option #1<br />
Option #2<br />
Sample for<br />
tissue banking<br />
(general or<br />
specific<br />
protocol)<br />
More for<br />
banking<br />
(rare, since<br />
tissue is fixed<br />
at this point)<br />
Is more<br />
tissue now<br />
needed for<br />
diagnosis?<br />
No<br />
Option #3<br />
Do neither<br />
Specimen goes into<br />
formalin; kept for a<br />
short time following<br />
diagnostic signout<br />
Surgical biospecimens are often inadequate for<br />
molecular diagnostics<br />
• Many diseases and cases are not subject to surgical<br />
therapy<br />
• Many diseases and cases are not treatment naïve at the<br />
time of surgical therapy<br />
• Surgical therapy often occurs at only one time point in<br />
a patient’s clinical course<br />
• Surgical specimens experience tremendous preanalytical<br />
processing variability<br />
• Competing needs for traditional histopathology<br />
assessment<br />
• Requirement for minimally invasive, repeated sampling<br />
16
8/21/2012<br />
<strong>Tissue</strong> banking<br />
principles<br />
‣ Changes made recently to surgical tissue collection/<br />
transport practices which result in delivery of more<br />
tissue in “real time” (
8/21/2012<br />
Laser capture microscopy<br />
Before LCM After LCM Cap picture<br />
Adenocarcinom<br />
a<br />
Digital<br />
pathology<br />
‣ Biorepository has access to an Aperio XT<br />
120-slide digital slide scanner within pathology<br />
department<br />
‣ Useful for slide review and sharing,<br />
documentation, teaching<br />
‣ Image analysis programs hold promise for the<br />
quantitative assessment of cases, especially<br />
tumor % cellularity<br />
18
8/21/2012<br />
Acknowledgments<br />
• Siteman Cancer <strong>Center</strong> (Grant #P30 CA91842)<br />
• Institute for Clinical and Translational Science<br />
(Grant #UL1RR024992)<br />
at <strong>Washington</strong> <strong>University</strong> <strong>Medical</strong> <strong>Center</strong>,<br />
which have partially funded the biorepository at<br />
<strong>Washington</strong> <strong>University</strong> School of Medicine.<br />
• Mark Watson (co-director, LTP)<br />
• Vicky Holtschlag (lab manager, LTP)<br />
• Benjamin Ryan (IT)<br />
• All my LTP colleagues!<br />
Backup slides<br />
19
8/21/2012<br />
Suitability of Needle Aspirates for Molecular<br />
Diagnosis of Lung Cancer<br />
• Lung adenocarcinoma is often<br />
non-operable<br />
• Diagnosis is limited to FNA or<br />
Needle Core biopsy<br />
• Sampling quality depends on<br />
modality<br />
• Sampling quality is operator<br />
dependent<br />
• Requires QA for overall sample<br />
quality and representation<br />
Sample Set<br />
• 17 resected tumors > 17 RNA<br />
• 17 resected normal > 17 RNA<br />
• 17 (matched)ex-vivo FNA > 10 RNA<br />
• 29 in-vivo FNA > 8 RNA<br />
• 4 image-guided<br />
• 4 endoscopy<br />
92 gene<br />
predictor<br />
Lim, Clin. Ca. Res.<br />
9;5980 (2003)<br />
Building a WU Repository Network<br />
20
8/21/2012<br />
WUMC Biobanking 2011<br />
Regulatory Requirements<br />
• For biospecimen procurement, risks are mainly breach of confidentiality.<br />
• HIPAA: (45 CFR Parts 160 and 164) Conditions under which PHI may be<br />
used or disclosed by Covered Entities for research purposes:<br />
• “Safe Harbor” method: Lists 18 specific types of data elements that<br />
must be removed; de-identified data does not constitute PHI and<br />
therefore can be freely disclosed.<br />
• Statistical method.<br />
• The “limited data set”: Requires removal of 16 elements and an<br />
agreement to be executed limiting the use of the data<br />
• Requirements of individual institutions / IRBs<br />
• FDA Rule for Human Subjects Research (21 CFR Part 50)<br />
• State law<br />
• Intellectual Property / Materials Transfer / Legal Requirements<br />
21
8/21/2012<br />
22
8/21/2012<br />
Contraindications to tissue banking<br />
‣ small tumors and other cases where most<br />
lesional tissue is needed for diagnosis<br />
‣ surgical margins of resection<br />
‣ specimens where tumor and benign areas<br />
cannot be clearly delineated grossly<br />
‣ grossly visible areas of primarily necrosis,<br />
hemorrhage, or fat<br />
‣ specimens which are known to have been<br />
delayed significantly more than 30<br />
minutes past their procurement time in the<br />
OR<br />
‣ tissue previously freeze-thawed, or frozen<br />
slowly (e.g. in the cryostat or -80 freezer)<br />
Contraindications to tissue banking<br />
‣ areas of deepest invasion, tumor/normal<br />
interface, tumor/capsule interface,<br />
extranodal extension of tumor, and<br />
other key landmarks for surgical<br />
pathology evaluation and tumor staging<br />
‣ chemotherapy- or radiation-treated<br />
tumors with no gross residual tumor<br />
mass<br />
‣ diagnostic biopsies where most or all<br />
tissue must be submitted for pathology<br />
evaluation…most lymph node, GI,<br />
bone marrow, and liver biopsies<br />
fall in this category<br />
‣ tissue clearly marked as intended<br />
for a special study such as<br />
immunofluorescence<br />
23
8/21/2012<br />
Organ-specific contraindications: examples<br />
• Too little tissue typically available for banking, or all<br />
available tissue often needed for diagnosis<br />
– Brain tumors<br />
– Testicular tumors, especially germ cell neoplasms<br />
– Many diagnostic biopsies<br />
– Primary melanomas<br />
• Diagnoses where submission of most or all tissue is<br />
needed to substantiate a previous diagnosis or look<br />
for invasive areas<br />
– DCIS, LCIS, atypical endometrial hyperplasia<br />
Organ-specific contraindications: examples<br />
• Necessity to preserve landmarks important for<br />
surgical pathology evaluation<br />
– Capsule for thyroid masses<br />
– Surgical margins<br />
– Stalk for tubulovillous adenomas<br />
– Lymph node capsule in radical neck dissections<br />
• Gross/ microscopic correlation difficulties<br />
• Bony tumors requiring decalcification<br />
24
8/21/2012<br />
Organ-specific contraindications: examples<br />
• Necessity to preserve landmarks important for<br />
surgical pathology evaluation<br />
– Capsule for thyroid masses<br />
– Surgical margins<br />
– Stalk for tubulovillous adenomas<br />
– Lymph node capsule in radical neck dissections<br />
• Gross/ microscopic correlation difficulties<br />
• Bony tumors requiring decalcification<br />
Key issues for banked samples:<br />
our experience<br />
‣samples received from outside sources may not be<br />
of the type or disease state advertised, or may be of<br />
poor quality, i.e. necrotic<br />
‣certain cell types within a sample, such as epithelial<br />
lining or an inflammatory component, may need to<br />
be isolated specifically, rather than the whole tissue<br />
being digested in an expression assay<br />
‣pigments, inflammatory infiltrates, preservation<br />
conditions, or other features may affect the intended<br />
performance of the tissue in an expression assay.<br />
25
8/21/2012<br />
Sampling issues<br />
This sample of metastatic<br />
adenocarcinoma in the liver is largely<br />
necrotic. Therefore, this would not be<br />
an ideal specimen for most studies,<br />
especially digestion of the tissue for<br />
RNA expression studies (H&E, 200x)<br />
The endometrial glands of this uterus<br />
specimen are of primary interest, but<br />
the specimen also contains stromal and<br />
vascular cells. Thus, specific isolation<br />
of the desired cell type may be needed,<br />
for example through laser-capture<br />
microscopy, if a digestive assay is<br />
planned (H&E, 400x)<br />
Contributions of tissue banking<br />
Demonstration by IHC that a<br />
phosphorylated membrane<br />
receptor was overexpressed in<br />
human lung carcinoma (brown<br />
reaction product) helped support<br />
research interest in the receptor<br />
(200x)<br />
Identification of respiratory<br />
epithelium (top) was needed for its<br />
isolation by laser capture<br />
microscopy, to perform pilot<br />
studies for gene expression in<br />
diseased lung tissue (H&E, 400x)<br />
26
8/21/2012<br />
“Adjacent normal” tissue<br />
This case of<br />
metastatic carcinoma<br />
to the liver showed<br />
inflammatory<br />
infiltrates in portal<br />
tracts in the adjacent<br />
non-neoplastic liver<br />
tissue<br />
Discrepancies between stated and actual<br />
specimen dx: commercial samples<br />
• This specimen was<br />
billed by a commercial<br />
tissue provider as<br />
normal lung (H&E,<br />
200x)<br />
• This specimen was<br />
billed by a commercial<br />
tissue provider as<br />
normal pancreas (H&E,<br />
200x)<br />
27
8/21/2012<br />
Lessons learned<br />
When planning the use of tissue specimens<br />
in research, think like a pathologist and<br />
consider how gross, histologic, and quality<br />
factors in the tissue may impact your studies<br />
“Trust but verify” – be suspicious of any<br />
diagnosis or interpretation attached to an<br />
outside tissue, unless you have examined it<br />
histologically<br />
Pathologists and tissue microarrays (TMAs)<br />
• <strong>Tissue</strong> arrays provide rapid screening for dozens<br />
or hundreds of tissue specimens with probes for<br />
protein, RNA or DNA targets, without exhausting<br />
tissue resources.<br />
• Traditional TMA = paraffin block<br />
• TMAs adaptable to any assay routinely done on<br />
tissue sections<br />
• Multiorgan TMAs and matching tumor/normal<br />
TMAs enhance the output of information<br />
28
8/21/2012<br />
<strong>Tissue</strong> Microarrays<br />
Advantages<br />
High-throughput screening (100-500 cases per slide)<br />
Uniform processing across all cases<br />
Conservation of specimen block<br />
Conservation of probe (antibody)<br />
Adaptability to image analysis programs for interpretation<br />
Disadvantages<br />
Limited sampling of specimen<br />
Low-throughput interpretation<br />
Need for robust informatics<br />
<strong>Tissue</strong> microarray construction<br />
TMA work<br />
station. Cores<br />
of tissue are<br />
transferred<br />
from donor<br />
blocks to the<br />
arrayed<br />
recipient block.<br />
The arrayed<br />
slides can be<br />
stained by IHC,<br />
ISH or FISH.<br />
29
8/21/2012<br />
Pathologist roles in TMAs<br />
Selecting “donor”<br />
tissue blocks for<br />
TMA construction<br />
Selecting areas of<br />
“donor” blocks to<br />
obtain tissue core from<br />
Configuring TMA block<br />
parameters appropriately.<br />
For example, too many<br />
cores on a slide will yield<br />
smaller core areas. This<br />
raises the risk that edge<br />
artifacts from IHC staining<br />
will obscure useful<br />
information.<br />
Reviewing H&E slide<br />
for TMA blocks, for<br />
quality assurance<br />
purposes (i.e. making<br />
sure that appropriate<br />
tissues are represented in<br />
cores, and documenting<br />
if they are not)<br />
Operating Procedures for Specimen Evaluation<br />
Verify the pathology of all incoming tissues,<br />
storage of these interpretations in data files<br />
Communicate with outside tissue suppliers about our findings<br />
and any discrepancies with claimed diagnosis or tissue quality<br />
Consider the project goals and methods vs. the anatomic<br />
makeup of the tissue:<br />
What cells or component(s) of the tissue are key to the<br />
study or the choice of controls?<br />
30
8/21/2012<br />
Operating Procedures for Specimen Evaluation<br />
Supply H&E sections matching<br />
the provided tissue, with relevant<br />
areas of disease marked<br />
Oncology: areas of tumor,<br />
pre-malignant change,<br />
normal adjacent tissue,<br />
overall % tumor cellularity<br />
Atherosclerosis: areas of<br />
plaque (stable and<br />
unstable) vs. normal<br />
vessel wall<br />
Collection Limitations<br />
• Surgically Inaccessible<br />
Previous resection<br />
Brain metastasis<br />
Small cell lung cancer<br />
• Limiting Material<br />
FNA<br />
DCIS<br />
• Sampling Error<br />
Prostate cancer<br />
• Proper Collection Procedures<br />
Primary hospitals<br />
Academic centers<br />
• Insufficient Claim / Interest<br />
• Competition<br />
31
8/21/2012<br />
Solutions<br />
• Specific Protocols for Prospective Procurement<br />
Need Clinician Interest<br />
Need for Informed Consent<br />
• Use of Archived Surgical Pathology Clinical Specimens<br />
Inability to Obtain Informed Consent<br />
Technical Hurdles<br />
• Use of Smaller Specimens (FNA / Touch Prep / Histological<br />
Sections)<br />
Need Clinician Interest<br />
Technical Hurdles<br />
• Education and Support<br />
‣ Only tissue that is absolutely not needed for clinical<br />
diagnosis should be collected for the Tumor Bank. If in<br />
doubt, do NOT submit specimens for banking.<br />
‣ Once specimens have been accessioned into the Bank, they<br />
cannot be used for clinical purposes.<br />
‣ Procurement practices are a “work in progress”, i.e. can and<br />
should be changed in response to evolving needs<br />
‣ Specialized protocols exist (LCBRN, TCGA); surgical and<br />
TPC staff will assist with these<br />
‣ Questions regarding tissue banking procedures:<br />
– Sandra McDonald (7-5773)<br />
– Joan Rossi (2-0135)<br />
– Tracey Leach (7-1354)<br />
– <strong>Tissue</strong> Procurement Core (TPC) processing lab (4-7615)<br />
(Amy Brink, Vicky Holtschlag)<br />
32
8/21/2012<br />
General procedure<br />
‣ Use a <strong>Tissue</strong> Procurement Specimen Bag – these contain a white-label area with a<br />
TPC-provided number written on them. Do not use any other container or bag. If<br />
no bags are available call the TPC (4-7615) to obtain more bags.<br />
‣ Check the specimen submission sheet from the OR and verify that the specimen is<br />
acceptable for tissue banking (i.e. the specimen is not marked for special studies<br />
such as immunofluorescence requiring immersion in special fixatives).<br />
‣ Fill out the patient information on the sheet titled "Tumor Bank <strong>Tissue</strong> Collection"<br />
which is located next to the cryobath. On the left-hand side of this sheet, place the<br />
patient information. Important: include the surgical pathology number here. On<br />
the right-hand side, place the bag's number, tissue type, and "collected by" person<br />
(pathologist or PA who actually procured the banking specimen)<br />
‣ Do not label the TPC bag with any patient or clinical information; instead place<br />
that on the sheet.<br />
General procedure,<br />
continued<br />
‣ Place a single tissue specimen flat in the plastic bag. A single tissue specimen's volume<br />
should be at least 0.5 cm 3 , and at most 3 – 4 cm 3 , with at least one dimension measuring<br />
< 0.5cm thick for quick freezing.<br />
‣ Collect non-malignant and malignant tissue. Non-malignant (i.e. "adjacent normal") tissue<br />
should be collected > 2 cm from the primary tumor, subject to any geometric limitations.<br />
Do not place tumor and non-malignant tissue in the same bag.<br />
‣ If feasible, collect and separately identify both: 1) primary tumor and 2) metastatic lesions to<br />
lymph nodes or other tissues.<br />
‣ 5-7mm skin punch biopsy instrument can be considered, instead of a scalpel blade, as a way<br />
to get samples fromdifficult cases<br />
‣ TPC's 2-methylbutane bath (-50C) immediately afterwards<br />
‣ Goal: bankable tissue immersed in bath
8/21/2012<br />
ca<strong>Tissue</strong>: Event / QC Tracking<br />
ca<strong>Tissue</strong>: Specimen Search<br />
34
8/21/2012<br />
ca<strong>Tissue</strong>: Search Results<br />
Tree view of results<br />
Results table view<br />
with pre-defined<br />
data elements<br />
Select specimens<br />
for request<br />
Building a WU Repository Network<br />
35
8/21/2012<br />
Clinical tissue banking:<br />
Requirements for a successful program<br />
‣ Close partnerships between pathologists, surgeons, and<br />
hospital adminstrators<br />
‣ Demonstration of solid clinical value to hospital<br />
administration<br />
‣ Pathologists’ assistants and other gross room staff with<br />
good knowledge of gross room techniques<br />
‣ Knowledgeable tissue bank pathologist(s) and staff who<br />
understand the process and the value of good communication<br />
‣ Transport personnel between operating rooms and<br />
pathology laboratory<br />
‣ Instruction/ education process for staff and stakeholders<br />
Research vs. clinical tissue banking<br />
• In the past, tissue banking was regarded as primarily a research activity<br />
• Advent of molecular technologies has made the storage of fresh-frozen<br />
tissue for diagnostic purposes desirable; i.e. tissue banking can and<br />
should become a routine part of patient care<br />
- Specimens banked now and used later at an unspecified time<br />
- Results may be correlated with past or future clinical specimens,<br />
i.e. time becomes an added dimension of banking, especially<br />
advancing knowledge/ hypotheses<br />
• Consent and IRB expectations for clinical tissue banking should evolve<br />
similarly to other clinical processes, i.e. clinicians not needing specific<br />
IRB approval for diagnostic blood draws from patients<br />
- Clinical bank specimens would remain identified<br />
• In a sense, clinical tissue banking has always existed with paraffin block<br />
archives from surgical pathology; demand for fresh-frozen specimens<br />
driven by molecular/ genomic technologies is key<br />
36
8/21/2012<br />
Comparison between umbilical cord blood banking and clinical<br />
tissue banking<br />
Issue Comparison Comments<br />
Time dimension of the<br />
biobanking process<br />
Promotion of advantages of<br />
the procedure to physicians<br />
and patients<br />
Link to patient identity<br />
Accreditation<br />
In both fields, specimens are<br />
banked now for an uncertain but<br />
potentially high-impact use in the<br />
future; can be of benefit in ways<br />
not necessarily forseen at the<br />
time of procurement<br />
Communication/education is a<br />
central component of cord blood<br />
banking to increase use of the<br />
procedure; this is also likely true<br />
of clinical tissue banking<br />
Private (though not public) cord<br />
bank specimens linked to patient<br />
identity; required for clinical<br />
tissue banking<br />
Besides FDA regulations, the<br />
American Association of Blood<br />
Banks (AABB), (CAP) and the<br />
Foundation for the Accreditation<br />
of Cellular Therapy (FACT).<br />
Accreditation program for tissue<br />
banks (CAP) released in 2011.<br />
Education of users is required,<br />
since stakeholders often tend to<br />
value only those things that offer<br />
immediate benefits<br />
Helps overcome expectation and<br />
cost barriers, and helps the<br />
practice become more widely<br />
used<br />
Consent process distinct from<br />
that that used for biospecimen<br />
repositories focused on research<br />
Certification standards and<br />
accreditation programs enhance<br />
patient care; they will also<br />
increase patient and physician<br />
confidence in the overall<br />
enterprise, as well as the<br />
individual repositories they use<br />
37