Psoriasiform Eruption Associated With Graft-Versus-Host ... - Cutis
Psoriasiform Eruption Associated With Graft-Versus-Host ... - Cutis
Psoriasiform Eruption Associated With Graft-Versus-Host ... - Cutis
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Psoriasiform</strong> <strong>Eruption</strong> <strong>Associated</strong> <strong>With</strong><br />
<strong>Graft</strong>-<strong>Versus</strong>-<strong>Host</strong> Disease<br />
Shijima Taguchi, MD; Yasuhiro Kawachi, MD; Yasuhiro Fujisawa, MD; Yasuhiro Nakamura, MD;<br />
Junichi Furuta, MD; Fujio Otsuka, MD<br />
Practice Points<br />
Typical cutaneous manifestations of acute graft-versus-host disease (GVHD) are maculopapular eruptions<br />
and perifollicular papules.<br />
<strong>Psoriasiform</strong> eruption can occur as a rare manifestation of acute GVHD.<br />
<strong>Graft</strong>-versus-host disease (GVHD) is a frequent<br />
complication of bone marrow transplantation<br />
(BMT) that can be classified as acute or<br />
chronic. Characteristic cutaneous manifestations<br />
of acute GVHD, which generally occurs within<br />
3 months following BMT, include maculopapular<br />
exanthema and perifollicular papular lesions. <strong>Psoriasiform</strong><br />
skin eruption as a manifestation of acute<br />
GVHD is rare. We report the case of a 4-year-old<br />
boy who developed a generalized psoriasiform<br />
eruption shortly after undergoing an allogeneic<br />
BMT. Histologic features of both psoriasis and<br />
acute GVHD were present.<br />
<strong>Cutis</strong>. 2013;92:151-153.<br />
<strong>Graft</strong>-versus-host disease (GVHD) is a frequent<br />
complication of bone marrow transplantation<br />
(BMT) that can be classified as<br />
acute or chronic. 1 Characteristic cutaneous manifestations<br />
of acute GVHD, which generally occur<br />
within 3 months following BMT, include maculopapular<br />
exanthema and perifollicular papular lesions.<br />
Chronic GVHD, which usually occurs more than<br />
3 months after BMT, typically presents as lichen planus<br />
or scleroderma. 1 We report a rare case of acute<br />
cutaneous GVHD mimicking psoriasis vulgaris in a<br />
4-year-old boy following allogeneic BMT.<br />
Do Not<br />
Case Report<br />
Copy<br />
A 4-year-old boy was diagnosed with acute lymphocytic<br />
leukemia (pro-B acute lymphoblastic leukemia,<br />
biphenotypic type). The patient had no history of<br />
rash or arthropathy, and his parents had no symptoms<br />
or history of psoriasis. He underwent allogeneic<br />
From the Department of Dermatology, Faculty of Medicine, University<br />
of Tsukuba, Japan.<br />
The authors report no conflict of interest.<br />
Correspondence: Yasuhiro Kawachi, MD, Department of<br />
Dermatology, Faculty of Medicine, University of Tsukuba, 1-1-1,<br />
Tennodai, Tsukuba 305-8575, Japan (kyasuhir@md.tsukuba.ac.jp).<br />
CUTIS<br />
BMT from an unrelated HLA antigen–matched<br />
female donor with no documented history of psoriasis.<br />
The patient received prophylactic treatment<br />
against GVHD, which included oral tacrolimus<br />
(average dose, 0.2 mg/kg daily) starting 1 day before<br />
BMT. On day 60 following BMT, the dosage of tacrolimus<br />
was tapered to 0.06 mg/kg daily. The patient<br />
developed patchy erythema on the face, trunk,<br />
and extremities with no other general symptoms<br />
(Figure 1). The eruptions consisted of keratotic erythematous<br />
papules and plaques with whitish scales<br />
and clinical features that were similar to psoriasis.<br />
Histopathology of a sample lesion from the abdomen<br />
indicated acanthosis with elongation of rete ridges,<br />
confluent parakeratosis with Munro microabscess,<br />
and dilatation of blood vessels with perivascular<br />
infiltration of lymphocytes in the upper dermis<br />
(Figures 2A and 2B). Focal satellite cell necrosis<br />
in the epidermis also was observed (Figure 2C).<br />
Immunohistochemical studies indicated infiltration<br />
of CD8 lymphocytes in the upper dermis and predominant<br />
CD8 exocytotic cells in the epidermis.<br />
WWW.CUTIS.COM<br />
VOLUME 92, SEPTEMBER 2013 151<br />
Copyright <strong>Cutis</strong> 2013. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher.
<strong>Psoriasiform</strong> <strong>Eruption</strong> <strong>Associated</strong> <strong>With</strong> GVHD<br />
Additionally, a marked decrease in the number of<br />
CD1a Langerhans cells was noted in the psoriatic<br />
lesion in the epidermis compared to contiguous<br />
normal skin (Figure 2D). Based on these clinical and<br />
histopathologic findings, a diagnosis of psoriasiform<br />
eruption associated with acute GVHD was made.<br />
Systemic steroid therapy with oral prednisolone<br />
(3 mg/kg daily) was administered for 2 weeks and<br />
then was tapered slowly. After his skin lesions and<br />
general condition rapidly improved, the patient was<br />
discharged from the hospital 1 month later (day 118<br />
following BMT); however, the eruptions recurred<br />
when the dose of oral prednisolone was tapered to<br />
1 mg/kg daily. As the patient’s condition worsened,<br />
he returned to the hospital and was administered<br />
oral methotrexate (10 mg weekly). Because this<br />
treatment was effective, the patient left the hospital<br />
after 2 weeks and his condition remained good thereafter<br />
with the same treatment.<br />
Comment<br />
Cutaneous involvement is common in GVHD.<br />
Typical cutaneous manifestations of acute GVHD<br />
CUTIS<br />
include maculopapular eruptions and perifollicular<br />
papules. 1 <strong>Psoriasiform</strong> eruptions following BMT are<br />
rare. Several cases showing the development of<br />
psoriasis vulgaris after BMT from donors with a history<br />
of psoriasis or resolution of psoriasis after BMT<br />
from a normal donor have been reported, 2,3 suggesting<br />
an adoptive transfer of susceptibility to psoriasis<br />
Do Not<br />
from a donor<br />
Copy<br />
with a genetic background of psoriasis.<br />
Although it is possible that our case was the result of<br />
transmission via BMT from a donor with nonsymptomatic<br />
subclinical psoriasis, we treated the psoriasiform<br />
eruptions in our patient as associated with acute<br />
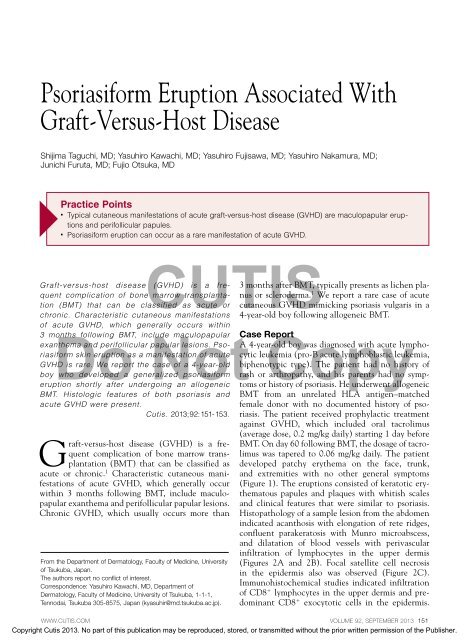
Figure 1. Widespread erythematous papules and GVHD rather than immunoadoptive psoriasis vulgaris<br />
because the donor had no documented plaques with whitish scales on the back.<br />
history<br />
Figure 2. The epidermis<br />
showed characteristic histopathologic<br />
changes of psoriasis<br />
with Munro microabscess (arrow<br />
in B)(A and B)(H&E; original<br />
magnifications 40 and 200,<br />
respectively). Focal satellite cell<br />
necrosis (arrow) of keratinocytes<br />
was seen in the epidermis<br />
(C)(H&E, original magnification<br />
200). CD1a Langerhans cells<br />
(arrows) were present in normal<br />
skin (left) and absent in the<br />
epidermis of the psoriatic lesion<br />
(right)(D)(original magnification<br />
40).<br />
A<br />
B<br />
C<br />
D<br />
152 CUTIS ®<br />
WWW.CUTIS.COM<br />
Copyright <strong>Cutis</strong> 2013. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher.
<strong>Psoriasiform</strong> <strong>Eruption</strong> <strong>Associated</strong> <strong>With</strong> GVHD<br />
of psoriasis. Histologically, satellite cell necrosis<br />
and depletion of CD1a Langerhans cells from the<br />
epidermis, which is characteristic of GVHD, 4 were<br />
observed in the psoriasiform eruptions. According to<br />
a PubMed search of articles indexed for MEDLINE<br />
using the term graft-versus-host disease psoriasis,<br />
2 other reports of psoriasiform eruptions associated<br />
with GVHD have been reported in the literature. 5,6<br />
Conclusion<br />
We present a rare case of acute cutaneous GVHD<br />
mimicking psoriasis vulgaris in a 4-year-old boy following<br />
allogeneic BMT. Our case presents histologic<br />
features of both psoriasis and acute GVHD.<br />
REFERENCES<br />
1. Aractingi S, Chosidow O. Cutaneous graft-versus-host disease.<br />
Arch Dermatol. 1998;134:602-612.<br />
2. Masszi T, Farkas A, Remenyi P, et al. Ten-year remission<br />
of psoriasis after allogeneic but not autologous<br />
bone marrow transplantation. Dermatology. 2006;212:<br />
88-89.<br />
3. Slavin S, Nagler A, Varadi G, et al. <strong>Graft</strong> vs autoimmunity<br />
following allogeneic non-myeloablative blood stem<br />
cell transplantation in a patient with chronic myelogenous<br />
leukemia and severe systemic psoriasis and psoriatic polyarthritis.<br />
Exp Hematol. 2000;28:853-857.<br />
4. Lampert IA, Janossy G, Suitters AJ, et al. Immunological<br />
analysis of the skin in graft versus host disease. Clin Exp<br />
Immunol. 1982;50:123-131.<br />
5. Kawakami Y, Oyama N, Nakamura K, et al. <strong>Psoriasiform</strong><br />
eruption associated with graft-versus-host disease. Acta<br />
Derm Venereol. 2007;87:436-438.<br />
6. Matsushita T, Hasegawa M, Shirasaki F, et al. A case of<br />
acute cutaneous graft-versus-host disease mimicking psoriasis<br />
vulgaris. Dermatology. 2008;216:64-67.<br />
CUTIS<br />
Do Not Copy<br />
WWW.CUTIS.COM<br />
VOLUME 92, SEPTEMBER 2013 153<br />
Copyright <strong>Cutis</strong> 2013. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher.