guidelines on collection and transport of specimens for suspected ...
guidelines on collection and transport of specimens for suspected ...
guidelines on collection and transport of specimens for suspected ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Research Institute <strong>for</strong> Tropical Medicine<br />
LABORATORY RESEARCH DIVISION<br />
MICROBIOLOGY DEPARTMENT<br />
Document:<br />
Introducti<strong>on</strong>:<br />
Guidelines <strong>for</strong> Collecti<strong>on</strong> <strong>and</strong> Transport <strong>of</strong> Specimen <strong>for</strong> Laboratory<br />
Diagnosis <strong>of</strong> Pathogenic Leptospira spp.<br />
Leptospirosis is an acute bacterial infecti<strong>on</strong> caused by organism bel<strong>on</strong>ging to<br />
the genus Leptospira. They are zo<strong>on</strong>otic organisms <strong>of</strong>ten affecting animals<br />
but can be transmitted directly or indirectly from animals to humans.<br />
Leptospirosis is a biphasic disease. The first phase, acute phase or phase <strong>of</strong><br />
leptospiremia occurs from the start <strong>of</strong> the disease <strong>and</strong> may last <strong>for</strong> 4-7 days.<br />
During this phase leptospires multiply in the blood <strong>and</strong> spread to different<br />
organs. Recovery rate <strong>of</strong> leptospires from blood or other tissues or body<br />
fluids is usually high during this stage. It is also during the acute phase<br />
wherein seroc<strong>on</strong>versi<strong>on</strong> starts but may <strong>on</strong>ly be detectable after 4-7 days<br />
after <strong>on</strong>set <strong>of</strong> illness.<br />
The sec<strong>on</strong>d phase, c<strong>on</strong>valescent phase, immune phase or leptospirurea<br />
phase occurs 3-5 days after the acute phase <strong>and</strong> may last up to 30 days after<br />
the <strong>on</strong>set <strong>of</strong> illness. During this phase leptospires are being excreted in the<br />
urine <strong>and</strong> may <strong>on</strong>ly persist in the blood at very low c<strong>on</strong>centrati<strong>on</strong>. During<br />
the c<strong>on</strong>valescent phase seroc<strong>on</strong>versi<strong>on</strong> reaches its peak <strong>and</strong> antibodies are<br />
at their highest detectable level after which they slowly decline <strong>and</strong> may last<br />
<strong>for</strong> years at very low levels.<br />
Available Tests:<br />
Real-Time PCR (qPCR)<br />
- Molecular detecti<strong>on</strong> <strong>of</strong> pathogenic Leptospira spp. DNA from blood, CSF<br />
<strong>and</strong> urine.<br />
Microscopic Agglutinati<strong>on</strong> Test (MAT)<br />
- Serological test <strong>for</strong> the detecti<strong>on</strong> <strong>of</strong> leptospire specific antibodies present<br />
in the serum.<br />
Culture<br />
- Identificati<strong>on</strong> <strong>of</strong> live leptospires from blood, CSF <strong>and</strong> urine.<br />
Rates: Samples with PIDSR <strong>for</strong>m Free <strong>of</strong> charge<br />
Samples without PIDSR <strong>for</strong>m<br />
Real-Time PCR (qPCR) 2,800.00<br />
Microscopic Agglutinati<strong>on</strong> Test 1,120.00<br />
Culture (no sensitivity test) 2,800.00<br />
Turn-around Time: Real-Time PCR (qPCR) 2-3 days<br />
(working days) Microscopic Agglutinati<strong>on</strong> Test 7 days<br />
Culture (no sensitivity test)<br />
6-8 weeks<br />
Ver. 1.5 2012 EMS<br />
Page 1 <strong>of</strong> 5
Research Institute <strong>for</strong> Tropical Medicine<br />
LABORATORY RESEARCH DIVISION<br />
MICROBIOLOGY DEPARTMENT<br />
Recommended Specimen: (Collecti<strong>on</strong> <strong>and</strong> Transport)<br />
<br />
For Real-Time PCR (qPCR)<br />
1. BLOOD (1 to 10 days after <strong>on</strong>set <strong>of</strong> symptoms)<br />
a. Serum is the preferred sample. Obtain 0.5 to 2 ml <strong>of</strong> serum <strong>and</strong> transfer it into a<br />
sterile 2ml screw capped tube. Freeze sample (-10±5°C)<br />
b. Venous blood in EDTA tube (do not use citrate <strong>and</strong> heparin anticoagulants)<br />
2. CSF (5 to 10 days after <strong>on</strong>set <strong>of</strong> symptoms)<br />
a. Aseptically collect CSF (0.5-1ml)<strong>and</strong> store in a sterile leak-pro<strong>of</strong> c<strong>on</strong>tainer.<br />
Preferably a sterile 2 ml screw cap tube. Freeze sample (-10±5°C)<br />
3. URINE (2 nd week <strong>of</strong> illness up to 30 days after <strong>on</strong>set <strong>of</strong> symptoms)<br />
a. Collect sample <strong>of</strong> midstream urine (10-20ml) in a leak pro<strong>of</strong> c<strong>on</strong>tainer. Freeze<br />
sample (-10±5°C)<br />
<br />
For MAT (Serum <strong>on</strong>ly)<br />
1. Preferably, paired sera must be submitted. Obtain 0.5 to 1 ml <strong>of</strong> serum <strong>and</strong> transfer it<br />
into a sterile 2ml screw capped tube. (Label tubes if acute or c<strong>on</strong>valescent phase sample.<br />
Freeze sample (-10±5°C)<br />
a. Acute phase sample (collected 5-10 days after <strong>on</strong>set <strong>of</strong> symptoms)<br />
b. C<strong>on</strong>valescent phase sample (collected 3-20 days after acute phase)<br />
2. If <strong>on</strong>ly <strong>on</strong>e serum is submitted. Obtain 0.5 to 1 ml <strong>of</strong> serum <strong>and</strong> transfer it into a sterile<br />
2ml screw capped tube. Freeze sample (-10±5°C)<br />
<br />
For Culture<br />
1. BLOOD (1 to 10 days after <strong>on</strong>set <strong>of</strong> symptoms)<br />
a. Bedside collecti<strong>on</strong> <strong>and</strong> inoculati<strong>on</strong> <strong>on</strong>ly. Obtain 2 EMJH or Fletcher’s media from<br />
the clinical laboratory be<strong>for</strong>e collecti<strong>on</strong>. Label tubes A <strong>and</strong> B. Aseptically extract<br />
1-2 ml <strong>of</strong> venous <strong>and</strong> aseptically add 2 drops <strong>of</strong> blood to tube A <strong>and</strong> 4 drops <strong>of</strong><br />
blood to tube B. Wrap tubes with opaque material <strong>and</strong> store in room<br />
temperature away from light. Store at room temperature (30±2°C)<br />
2. CSF (5 to 10 days after <strong>on</strong>set <strong>of</strong> symptoms)<br />
a. Bedside collecti<strong>on</strong> <strong>and</strong> inoculati<strong>on</strong> <strong>on</strong>ly. Obtain 2 EMJH or Fletcher’s media from<br />
the clinical laboratory be<strong>for</strong>e collecti<strong>on</strong>. Add 0.5 ml <strong>of</strong> CSF per tube. Wrap tubes<br />
with opaque material <strong>and</strong> store in room temperature away from light. Store at<br />
room temperature (30±2°C)<br />
b. If quantity is not sufficient, inoculate into <strong>on</strong>e tube <strong>on</strong>ly.<br />
Ver. 1.5 2012 EMS<br />
Page 2 <strong>of</strong> 5
Research Institute <strong>for</strong> Tropical Medicine<br />
LABORATORY RESEARCH DIVISION<br />
MICROBIOLOGY DEPARTMENT<br />
3. URINE (2 nd week <strong>of</strong> illness up to 30 days after <strong>on</strong>set <strong>of</strong> symptoms)<br />
a. Collect sample <strong>of</strong> midstream urine (10-20ml) in a leak pro<strong>of</strong> c<strong>on</strong>tainer <strong>and</strong><br />
<strong>transport</strong> immediately to RITM within 2 hours. Refrigerate sample (6±2°C)<br />
Transport <strong>of</strong> specimen:<br />
<br />
All sample c<strong>on</strong>tainers must have tight-sealing caps or lids <strong>and</strong> secure with paper tape<br />
(micropore) or parafilm whenever available be<strong>for</strong>e packing <strong>for</strong> <strong>transport</strong>.<br />
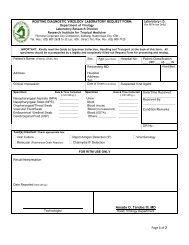
1. Check the following:<br />
a. The request <strong>for</strong>m which should c<strong>on</strong>tain at least:<br />
i. Patient’s complete name (with middle initial)<br />
ii. Date <strong>of</strong> birth<br />
iii. Age <strong>and</strong> Sex<br />
iv. Date <strong>of</strong> <strong>on</strong>set <strong>of</strong> illness<br />
v. Referring Instituti<strong>on</strong><br />
vi. Test requested<br />
b. All samples should be labeled <strong>on</strong> the c<strong>on</strong>tainer body with the:<br />
i. Patient’s complete name<br />
ii. Age<br />
iii. Sex<br />
iv. Date <strong>of</strong> specimen collecti<strong>on</strong><br />
2. Packaging should follow the triple-packing system wherein:<br />
a. Primary c<strong>on</strong>tainer - sample c<strong>on</strong>tainer (ex. screw cap tube, red top tube.)<br />
b. Sec<strong>on</strong>dary c<strong>on</strong>tainer - plastic bag <strong>for</strong> samples <strong>and</strong> can be sealed (ziplock)<br />
c. Tertiary c<strong>on</strong>tainer - sample packaging (ex. <strong>transport</strong> box, ice chest, styro box)<br />
3. Pack sample c<strong>on</strong>tainers in an upright positi<strong>on</strong> inside the “Ziplock” bag <strong>and</strong> add enough<br />
absorbent material (ex. tissue paper, paper towel) inside <strong>and</strong> seal the “Ziplock” bag with<br />
tape ensuring that samples will stay upright.<br />
4. Place the “Ziplock” bag inside the tertiary c<strong>on</strong>tainer <strong>and</strong> tape the bag to the wall <strong>of</strong> the<br />
tertiary c<strong>on</strong>tainer or positi<strong>on</strong> the sample in the center <strong>and</strong> secure in positi<strong>on</strong> with filling<br />
material.<br />
5. Place 2 ice packs/cool dogs beside or <strong>on</strong> top <strong>of</strong> the sample. If travel time is expected to<br />
exceed 1 day, add 2 ice packs/cold dogs per additi<strong>on</strong>al day <strong>of</strong> <strong>transport</strong>. Add filling material<br />
to secure all c<strong>on</strong>tents inside from moving during <strong>transport</strong>.<br />
Ver. 1.5 2012 EMS<br />
Page 3 <strong>of</strong> 5
Research Institute <strong>for</strong> Tropical Medicine<br />
LABORATORY RESEARCH DIVISION<br />
MICROBIOLOGY DEPARTMENT<br />
6. Seal box with packing tape <strong>and</strong> indicate outside the following:<br />
a. Sender’s name<br />
b. Sender’s address<br />
c. Sender’s c<strong>on</strong>tact in<strong>for</strong>mati<strong>on</strong><br />
d. Destinati<strong>on</strong>’s c<strong>on</strong>tact pers<strong>on</strong><br />
e. Destinati<strong>on</strong>’s address<br />
f. Destinati<strong>on</strong>’s c<strong>on</strong>tact number<br />
7. Insert in a separate “Ziplock” bag all documents (ex. Request <strong>for</strong>m, PIDSR <strong>for</strong>m, RITM outbreak<br />
referral <strong>for</strong>m, Line list) <strong>and</strong> securely attach it preferably <strong>on</strong> top <strong>of</strong> the <strong>transport</strong> box.<br />
Criteria <strong>for</strong> Rejecti<strong>on</strong>:<br />
1. Improper sample collected <strong>for</strong> test requested<br />
(Please refer to the recommended specimen secti<strong>on</strong> <strong>of</strong> this document)<br />
2. Inadequate sample quantity.<br />
(Please refer to the recommended specimen secti<strong>on</strong> <strong>of</strong> this document)<br />
3. Samples without request <strong>for</strong>ms.<br />
4. Incomplete data <strong>on</strong> request <strong>for</strong>m.<br />
(must c<strong>on</strong>tain at least the following: complete name <strong>of</strong> patient, date <strong>of</strong> birth, age <strong>and</strong> sex,<br />
referring instituti<strong>on</strong>, <strong>and</strong> test requested)<br />
5. Improperly labeled or unlabeled sample<br />
(must indicate at least the following: complete name <strong>of</strong> patient, age <strong>and</strong> sex, <strong>and</strong> date <strong>of</strong> sample<br />
collecti<strong>on</strong>.)<br />
6. Samples with visible c<strong>on</strong>taminati<strong>on</strong>.<br />
7. Spillage or breakage in transit.<br />
C<strong>on</strong>tact Pers<strong>on</strong>s:<br />
Office hours (M<strong>on</strong>day to Friday, 8am to 5pm)<br />
Department <strong>of</strong> Microbiology: 807-2628 to 32 local 604<br />
Lydia T. Sombrero, RMT<br />
Melisa U. M<strong>on</strong>doy, RMT MPH<br />
Eds<strong>on</strong> Michael M. Sim<strong>on</strong>, RMT<br />
Weekends <strong>and</strong> Holidays<br />
Clinical Laboratory: 807-2628 to 32 local 201<br />
Ver. 1.5 2012 EMS<br />
Page 4 <strong>of</strong> 5
Research Institute <strong>for</strong> Tropical Medicine<br />
LABORATORY RESEARCH DIVISION<br />
MICROBIOLOGY DEPARTMENT<br />
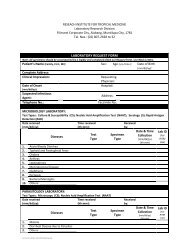
Flowchart from Specimen Submissi<strong>on</strong> to Reporting: (without PIDSR <strong>for</strong>m)<br />
STEP 1: Sample will be submitted by the Clinical Laboratory to the Microbiology<br />
Laboratory <strong>for</strong> testing.<br />
STEP 2: Microbiology Laboratory will release verified result to the Clinical Laboratory.<br />
STEP 3: CLinical Laboratory will release result afer presenting the OR.<br />
i. Flowchart from Specimen Submissi<strong>on</strong> to Reporting: (with PIDSR <strong>for</strong>m)<br />
STEP 1: Sample will be submitted or <strong>for</strong>warded by the Clinical Laboratory to the<br />
Microbiology Laboratory <strong>for</strong> testing.<br />
STEP 2: Microbiology Laboratory will <strong>for</strong>ward verified result, signed by the<br />
Microbiology Department head to the Director's Office with the cover letter to be<br />
signed by the Director.<br />
Copy furnished the Laboratory Divisi<strong>on</strong> Chief<br />
STEP 3: Director's Office will fax the result to respective CHD <strong>and</strong> to the NEC.<br />
Ver. 1.5 2012 EMS<br />
Page 5 <strong>of</strong> 5