Vitamin C supplementation to prevent premature rupture of the ...
Vitamin C supplementation to prevent premature rupture of the ...
Vitamin C supplementation to prevent premature rupture of the ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Vitamin</strong> C <strong>supplementation</strong> <strong>to</strong> <strong>prevent</strong> <strong>premature</strong> <strong>rupture</strong> <strong>of</strong> <strong>the</strong><br />
chorioamniotic membranes: a randomized trial 1–3<br />
Es<strong>the</strong>r Casanueva, Carmina Ripoll, Maricruz Tolentino, Rosa Maria Morales, Frania Pfeffer, Pablo Vilchis, and<br />
Felipe Vadillo-Ortega<br />
ABSTRACT<br />
Background: <strong>Vitamin</strong> C is involved in <strong>the</strong> syn<strong>the</strong>sis and degradation<br />
<strong>of</strong> collagen and is important for maintenance <strong>of</strong> <strong>the</strong> chorioamniotic<br />
membranes. Inadequate availability <strong>of</strong> ascorbic acid during<br />
pregnancy has been proposed as a risk fac<strong>to</strong>r for <strong>premature</strong> <strong>rupture</strong><br />
<strong>of</strong> <strong>the</strong> chorioamniotic membranes (PROM).<br />
Objective: The objective <strong>of</strong> <strong>the</strong> study was <strong>to</strong> evaluate <strong>the</strong> effectiveness<br />
<strong>of</strong> 100 mg vitamin C/d in <strong>prevent</strong>ing PROM.<br />
Design: A controlled double-blind trial was performed. Pregnant<br />
women (n 126) in <strong>the</strong>ir 20th wk <strong>of</strong> gestation were invited; 120<br />
accepted and were randomly assigned <strong>to</strong> 2 groups (100 mg vitamin<br />
C/d or placebo). Every 4 wk, plasma and leukocyte vitamin C concentrations<br />
were measured, and each subject was evaluated for cervicovaginal<br />
infection. The incidence <strong>of</strong> PROM was recorded for<br />
each group as an indica<strong>to</strong>r <strong>of</strong> <strong>the</strong> protective effect <strong>of</strong> vitamin C<br />
<strong>supplementation</strong>.<br />
Results: One hundred nine patients finished <strong>the</strong> study. Mean plasma<br />
vitamin C concentrations decreased significantly throughout <strong>the</strong><br />
pregnancy in both groups (P 0.001), and <strong>the</strong>re were no significant<br />
differences between groups. Between weeks 20 and 36, mean leukocyte<br />
vitamin C concentrations decreased from 17.5 <strong>to</strong> 15.23 g/<br />
10 8 cells in <strong>the</strong> placebo group and increased from 17.26 <strong>to</strong> 22.17<br />
g/10 8 cells in <strong>the</strong> supplemented group (within- and between-group<br />
differences: P 0.001). The incidence <strong>of</strong> PROM was 14 per 57<br />
pregnancies (24.5%) in <strong>the</strong> placebo group and 4 per 52 pregnancies<br />
(7.69%) in <strong>the</strong> supplemented group (relative risk: 0.26; 95% CI:<br />
0.078, 0.837).<br />
Conclusion: Daily <strong>supplementation</strong> with 100 mg vitamin C after 20<br />
wk <strong>of</strong> gestation effectively lessens <strong>the</strong> incidence <strong>of</strong> PROM. Am<br />
J Clin Nutr 2005;81:859–63.<br />
KEY WORDS <strong>Vitamin</strong> C, ascorbic acid, pregnancy, <strong>premature</strong><br />
<strong>rupture</strong> <strong>of</strong> <strong>the</strong> chorioamniotic membranes, preterm labor, dietary<br />
reference intakes, DRIs, Mexico<br />
INTRODUCTION<br />
Premature <strong>rupture</strong> <strong>of</strong> <strong>the</strong> chorioamniotic membranes (PROM)<br />
is a complication affecting 10–20% <strong>of</strong> all pregnancies. PROM is<br />
<strong>the</strong> main known cause <strong>of</strong> preterm delivery and is associated<br />
worldwide with increased rates <strong>of</strong> neonatal and maternal morbidity<br />
and mortality (1). Thus, it is important <strong>to</strong> develop public<br />
health strategies <strong>to</strong> <strong>prevent</strong> PROM. It has been proposed that<br />
maintaining adequate vitamin C status, ascertained on <strong>the</strong> basis<br />
<strong>of</strong> <strong>the</strong> vitamin C concentrations in leukocytes, could help reduce<br />
<strong>the</strong> incidence <strong>of</strong> PROM (2, 3). In a previous report, we (3) showed<br />
that PROM could be used as a functional test <strong>of</strong> vitamin C status<br />
throughout pregnancy. Our findings derived from <strong>the</strong> role <strong>of</strong><br />
vitamin C in collagen metabolism and that <strong>of</strong> collagen in maintaining<br />
<strong>the</strong> mechanical strength <strong>of</strong> <strong>the</strong> chorioamniotic membranes<br />
throughout gestation (4, 5). <strong>Vitamin</strong> C is recognized as a<br />
c<strong>of</strong>ac<strong>to</strong>r for collagen posttranscriptional modifications (6) and as<br />
a down-regula<strong>to</strong>r <strong>of</strong> <strong>the</strong> gene transcription <strong>of</strong> <strong>the</strong> 72-kDa type IV<br />
collagenase, matrix metalloproteinase (MMP-2), in amnion cells<br />
(7); it also controls <strong>the</strong> catabolism <strong>of</strong> collagen.<br />
The current recommended dietary allowance for vitamin C<br />
does not adequately take in<strong>to</strong> account <strong>the</strong> metabolic adjustments<br />
that occur during pregnancy. Altered patterns <strong>of</strong> collagen syn<strong>the</strong>sis<br />
and diminished concentrations <strong>of</strong> vitamin C at week 28 <strong>of</strong><br />
gestation have been associated with subsequent occurrence <strong>of</strong><br />
PROM (3, 4). It has been postulated that low concentrations<br />
<strong>of</strong> plasma and leukocyte ascorbic acid may result from a dilution<br />
effect caused by hemodynamic adjustments <strong>of</strong> blood volume<br />
during <strong>the</strong> third trimester <strong>of</strong> pregnancy (3). Leukocytes may act<br />
as a s<strong>to</strong>re <strong>of</strong> vitamin C and can provide a more reliable indica<strong>to</strong>r<br />
<strong>of</strong> vitamin C nutritional status (8) than can <strong>the</strong> ascorbic acid<br />
concentration in plasma or serum, which more specifically reflects<br />
<strong>the</strong> recent consumption <strong>of</strong> vitamin C. We recently conducted<br />
a clinical trial measuring <strong>the</strong> saturation dose <strong>of</strong> vitamin C<br />
in pregnant Mexican women (9) and found that 100 mg vitamin<br />
C/d added <strong>to</strong> <strong>the</strong> usual diet is sufficient <strong>to</strong> maintain a leukocyte<br />
ascorbate concentration 18 g (102 nmol)/10 8 cells, and this<br />
concentration protects against PROM (3).<br />
O<strong>the</strong>r conditions commonly present during pregnancy, such as<br />
cervicovaginal or intrauterine infections (which are <strong>the</strong>mselves<br />
risk fac<strong>to</strong>rs for PROM), may also affect <strong>the</strong> nutritional status <strong>of</strong><br />
vitamin C (10). Induction <strong>of</strong> <strong>the</strong> inflamma<strong>to</strong>ry response, which<br />
involves <strong>the</strong> respira<strong>to</strong>ry burst in leukocytes, causes <strong>the</strong> consumption<br />
<strong>of</strong> antioxidants such as vitamin C (11). The incidence <strong>of</strong><br />
1 From <strong>the</strong> Public Health Research Branch (EC, CR, MT, RMM, and FP),<br />
<strong>the</strong> Department <strong>of</strong> Obstetrics and Gynecology (PV), and <strong>the</strong> Direction <strong>of</strong><br />
Research (FV-O), National Institute <strong>of</strong> Perina<strong>to</strong>logy, Mexico City, Mexico.<br />
2 Supported by grant no. 783-P from <strong>the</strong> Consejo Nacional de Ciencia y<br />
Tecnologia, Mexico.<br />
3 Address reprint requests <strong>to</strong> E Casanueva, Public Health Research<br />
Branch, Institu<strong>to</strong> Nacional de Perina<strong>to</strong>logia, Torre de Investigacion, 2o Piso,<br />
Montes Urales 800, Lomas de Virreyes, DF 11000 Mexico. E-mail:<br />
casanuev@servidor.unam.mx.<br />
Received June 9, 2004.<br />
Accepted for publication December 6, 2004.<br />
Downloaded from www.ajcn.org by guest on January 5, 2012<br />
Am J Clin Nutr 2005;81:859–63. Printed in USA. © 2005 American Society for Clinical Nutrition<br />
859
860 CASANUEVA ET AL<br />
PROM may also reflect <strong>the</strong> potentiation <strong>of</strong> chronic or iterative<br />
infections or <strong>the</strong>ir synergistic effects during pregnancy and <strong>the</strong><br />
presence <strong>of</strong> low s<strong>to</strong>res <strong>of</strong> vitamin C (12). The aim <strong>of</strong> this study<br />
was <strong>to</strong> evaluate <strong>the</strong> effectiveness <strong>of</strong> 100 mg vitamin C/d in <strong>prevent</strong>ing<br />
PROM.<br />
SUBJECTS AND METHODS<br />
This double-blind study was performed from September 2002<br />
<strong>to</strong> August 2003 at <strong>the</strong> Institu<strong>to</strong> Nacional de Perina<strong>to</strong>logia (INPer)<br />
in Mexico City. One hundred twenty-six women attending <strong>the</strong><br />
prenatal clinic were identified as eligible participants. Inclusion<br />
criteria were defined as follows: pregnant women with no acute<br />
or chronic diseases, 20 wk <strong>of</strong> gestation, single<strong>to</strong>n pregnancy,<br />
no consumption <strong>of</strong> vitamin supplements, and provision <strong>of</strong> written<br />
informed consent. Exclusion criteria were <strong>the</strong> need for uterine<br />
cerclage or <strong>the</strong> presence <strong>of</strong> an obstetric indication for cesarean<br />
delivery.<br />
Women were allocated <strong>to</strong> 1 <strong>of</strong> 2 groups by a random-number<br />
table; one group received 100 mg vitamin C/d, and <strong>the</strong> o<strong>the</strong>r<br />
group received a placebo <strong>of</strong> <strong>the</strong> same size and shape (both<br />
provided by Roche Pharmaceuticals, Mexico City). The principal<br />
investiga<strong>to</strong>r generated <strong>the</strong> random table, prepared all<br />
tablets, and ensured that staff members were blinded as <strong>to</strong> <strong>the</strong><br />
grouping codes. <strong>Vitamin</strong> C or placebo was shipped <strong>to</strong> each<br />
participant directly from <strong>the</strong> research pharmacy, which concealed<br />
<strong>the</strong> treatment assignment from <strong>the</strong> investiga<strong>to</strong>rs. The<br />
women were instructed <strong>to</strong> ingest one tablet with water before<br />
breakfast each day.<br />
The sample size was calculated from <strong>the</strong> overall incidence <strong>of</strong><br />
PROM at <strong>the</strong> INPer (18.5%), regardless <strong>of</strong> gestational age, and<br />
on <strong>the</strong> basis <strong>of</strong> our hypo<strong>the</strong>sis that intervention with vitamin C<br />
would reduce <strong>the</strong> incidence <strong>of</strong> PROM by 20%. This would ensure<br />
an overall type I error <strong>of</strong> 5% and an 80% power-<strong>to</strong>-test reduction<br />
in <strong>the</strong> incidence <strong>of</strong> PROM. According <strong>to</strong> <strong>the</strong>se estimations and in<br />
<strong>the</strong> anticipation <strong>of</strong> losses <strong>of</strong> 10% during <strong>the</strong> study, we needed <strong>to</strong><br />
study 60 cases per group.<br />
Written informed consent was obtained from all subjects. If<br />
<strong>the</strong> pregnant woman was 18 y old, <strong>the</strong> written informed consent<br />
<strong>of</strong> a parent or legal guardian was obtained. The pro<strong>to</strong>col was<br />
reviewed and approved by <strong>the</strong> Research and Ethics Board <strong>of</strong> <strong>the</strong><br />
institution (pro<strong>to</strong>col registration no. 212250–49311).<br />
Study pro<strong>to</strong>col<br />
During <strong>the</strong> study, women were evaluated according <strong>to</strong> standardized<br />
procedures by trained nutritionists and faculty members<br />
<strong>of</strong> <strong>the</strong> Obstetrics and Gynecology Department. At <strong>the</strong> first evaluation,<br />
each woman’s general data, gynecologic and obstetric<br />
his<strong>to</strong>ry, and anthropometric data, including self-reported<br />
prepregnancy weight, were recorded. Information on socioeconomic<br />
status according <strong>to</strong> <strong>the</strong> scale <strong>of</strong> <strong>the</strong> Asociación Mexicana<br />
de Agencias de Estudios de Mercado (Mexican Association <strong>of</strong><br />
Marketing and Opinion Research) was also included; this scale<br />
measures purchasing power and contains 6 categories ranging<br />
from <strong>the</strong> highest <strong>to</strong> <strong>the</strong> lowest purchasing power (13). Each<br />
subject completed a food-frequency questionnaire, which considered<br />
<strong>the</strong> habitual intake <strong>of</strong> <strong>the</strong> previous year and which was<br />
previously validated in Mexican women (14). To obtain information<br />
on <strong>the</strong> habitual intake <strong>of</strong> vitamin C, intakes were corrected<br />
for cooking losses by a fac<strong>to</strong>r <strong>of</strong> 50% for boiled or fried<br />
food and by a fac<strong>to</strong>r <strong>of</strong> 25% for steamed food (15).<br />
From weeks 20 <strong>to</strong> 36, women were evaluated every 4 wk. At<br />
each evaluation, a vaginal explora<strong>to</strong>ry examination was performed,<br />
and a vaginal swab was taken for Gram staining and<br />
microbiologic study. The microorganisms <strong>of</strong> interest included<br />
Gardnerella vaginalis, Candida albicans, Group B strep<strong>to</strong>coccus,<br />
Escherichia coli, Neisseria gonorrhoeae, and Ureaplasma<br />
urealyticum. Cervicovaginal infection was diagnosed by clinical<br />
manifestations and positive results <strong>of</strong> <strong>the</strong> Gram stain and culture.<br />
If infection was diagnosed, <strong>the</strong> woman received treatment with<br />
antibiotics in accordance with established clinical pro<strong>to</strong>cols.<br />
Asymp<strong>to</strong>matic subjects with a positive culture did not receive<br />
treatment (16). To evaluate <strong>the</strong> adherence <strong>to</strong> treatment, <strong>the</strong><br />
women were instructed <strong>to</strong> maintain a personal record <strong>to</strong> register<br />
<strong>the</strong> daily consumption <strong>of</strong> tablets; <strong>the</strong> remaining tablets were<br />
counted by research staff at each visit.<br />
At <strong>the</strong> end <strong>of</strong> pregnancy, <strong>the</strong> incidence <strong>of</strong> PROM was registered<br />
as <strong>the</strong> primary outcome. PROM was defined in accordance<br />
with <strong>the</strong> American College <strong>of</strong> Obstetricians and Gynecologists as<br />
<strong>the</strong> leakage <strong>of</strong> amniotic fluid through <strong>rupture</strong>d chorioamniotic<br />
membranes that occurs 2 h before <strong>the</strong> onset <strong>of</strong> labor and after<br />
week 20 <strong>of</strong> pregnancy (17). The diagnosis <strong>of</strong> leakage <strong>of</strong> amniotic<br />
fluid was established clinically by physical examination that<br />
identified <strong>the</strong> leakage <strong>of</strong> amniotic fluid through <strong>the</strong> cervix and<br />
confirmed by crystallization and <strong>the</strong> nitrazine test. A clinical<br />
evaluation was performed at delivery by using <strong>the</strong> method <strong>of</strong><br />
Capurro et al (18) <strong>to</strong> verify <strong>the</strong> gestational age as estimated from<br />
<strong>the</strong> last menstrual period reported by <strong>the</strong> subject. A difference <strong>of</strong><br />
1 wk between <strong>the</strong> 2 evaluations was accepted; when <strong>the</strong> difference<br />
was 1 wk, <strong>the</strong> case was excluded from <strong>the</strong> study.<br />
Preterm labor was established when <strong>the</strong> delivery occurred before<br />
37 wk <strong>of</strong> gestation.<br />
Labora<strong>to</strong>ry tests<br />
During <strong>the</strong> evaluation visits, a 15-mL sample <strong>of</strong> blood was<br />
collected in<strong>to</strong> EDTA-coated tubes <strong>to</strong> measure plasma and leukocyte<br />
vitamin C concentrations. On <strong>the</strong> day <strong>of</strong> blood sampling,<br />
<strong>the</strong> women had fasted for 10–12 h and had not consumed <strong>the</strong><br />
supplement or placebo tablet. Within 30 min after obtaining <strong>the</strong><br />
blood sample, <strong>the</strong> plasma was separated by centrifugation at<br />
1800 g for 10 min, and leukocytes were isolated by using<br />
Dextran T500 (Sigma, St Louis, MO) (19). Leukocytes were<br />
counted with an au<strong>to</strong>matic cell counter (Coulter Counter T890,<br />
version 3D; Beckman Coulter, Miami, FL). After <strong>the</strong> addition <strong>of</strong><br />
methaphosphoric acid (Sigma) <strong>to</strong> <strong>prevent</strong> vitamin C oxidation,<br />
<strong>the</strong> plasma and leukocyte pellets were frozen at 70 °C. All<br />
samples were assayed in duplicate by using HPLC with an electrochemical<br />
detec<strong>to</strong>r (Perkin Elmer Life and Analytic Sciences,<br />
Shel<strong>to</strong>n, CT; 20). Interassay and intraassay CVs were 5% for<br />
all procedures. Labora<strong>to</strong>ry personnel were blind as <strong>to</strong> patient<br />
group allocation.<br />
Data analysis<br />
We used a repeated-measures analysis <strong>of</strong> variance with orthogonal<br />
polynomial contrasts, adjusted for multiple comparisons,<br />
in <strong>the</strong> general linear models (GLM) program on SPSS<br />
s<strong>of</strong>tware (version 11.0; SPSS Inc, Chicago IL) with Tukey’s<br />
correction <strong>to</strong> evaluate changes in vitamin C concentration in<br />
plasma and leukocytes at <strong>the</strong> return visits. Comparison <strong>of</strong> <strong>the</strong><br />
maternal characteristics, infections, and <strong>the</strong> incidence <strong>of</strong> PROM<br />
in <strong>the</strong> 2 groups was performed by chi-square test. Relative risks<br />
(RRs) with 95% CIs were calculated.<br />
Downloaded from www.ajcn.org by guest on January 5, 2012<br />
prgmea.com
PREVENTION OF PREMATURE RUPTURE OF MEMBRANES 861<br />
RESULTS<br />
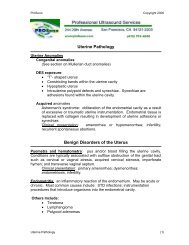
Of 126 participating women, 109 (91%) finished <strong>the</strong> study: 52<br />
women in <strong>the</strong> vitamin C–supplemented group and 57 in <strong>the</strong><br />
placebo group (Figure 1). The groups did not differ in any<br />
baseline variable such as age, number <strong>of</strong> gestations, or nutritional<br />
status. None <strong>of</strong> <strong>the</strong> women reported smoking cigarettes during<br />
pregnancy. According <strong>to</strong> <strong>the</strong> socioeconomic status scale, <strong>the</strong><br />
participants belonged <strong>to</strong> <strong>the</strong> lower middle-class, and <strong>the</strong> 2 groups<br />
did not differ significantly in socioeconomic status. A his<strong>to</strong>ry <strong>of</strong><br />
PROM was reported by 10.6%. The general and outcome variables<br />
<strong>of</strong> <strong>the</strong> 2 groups are presented in Table 1.<br />
A cervicovaginal infection at <strong>the</strong> first evaluation at 20 wk <strong>of</strong><br />
pregnancy was present in 32 (29%) <strong>of</strong> <strong>the</strong> 109 patients; 14 (25%)<br />
<strong>of</strong> <strong>the</strong> 57 women in <strong>the</strong> placebo group and 18 (35%) <strong>of</strong> <strong>the</strong> 52<br />
women in <strong>the</strong> vitamin C group (P 0.5). At week 28, only 10<br />
(18%) <strong>of</strong> 57 and 7 (14%) <strong>of</strong> 52 women had a cervicovaginal<br />
infection (P 0.05). At week 36, only 10 women had infection<br />
(6 in <strong>the</strong> placebo group and 4 in <strong>the</strong> vitamin C group; P 0.05).<br />
There were no differences between groups in <strong>the</strong> incidence <strong>of</strong><br />
infection, and only one woman had a recurrent infection. The<br />
microorganisms most frequently isolated were C. albicans<br />
(10.5% <strong>of</strong> <strong>the</strong> cases) and G. vaginalis (5.3% <strong>of</strong> <strong>the</strong> cases).<br />
According <strong>to</strong> <strong>the</strong> food-frequency questionnaire, <strong>the</strong> mean<br />
daily vitamin C intake was 63 and 68 mg in <strong>the</strong> placebo and<br />
vitamin C groups, respectively. In <strong>the</strong> placebo group, <strong>the</strong> 25th<br />
and 75 th percentile intakes were 38 and 135 mg/d, respectively;<br />
corresponding values for <strong>the</strong> vitamin C group were 45 and 118<br />
mg/d. There were no differences in dietary vitamin C intake<br />
between groups. Citrus fruit, <strong>to</strong>ma<strong>to</strong>es, and chilies (hot peppers)<br />
were <strong>the</strong> most important dietary sources <strong>of</strong> vitamin C. According<br />
<strong>to</strong> <strong>the</strong> personal records kept by <strong>the</strong> subjects, 80% reported<br />
adherence <strong>to</strong> <strong>the</strong> <strong>supplementation</strong> pro<strong>to</strong>col (83% in placebo<br />
group and 85% in <strong>the</strong> vitamin C group).<br />
The overall mean plasma vitamin C concentration at week 20<br />
<strong>of</strong> gestation was 0.76 0.28 mg/dL (43.15 15.9 mol/L).<br />
Plasma vitamin C concentrations decreased similarly throughout<br />
pregnancy in both groups (between-subjects differences: P <br />
FIGURE 1. Flow chart for a randomized vitamin C trial.<br />
0.001), and <strong>the</strong>y followed a significant (P 0.001) linear trend<br />
with time (Table 2).<br />
The mean leukocyte vitamin C concentration in <strong>the</strong> groups<br />
diverged as gestation progressed (between-subjects differences:<br />
P 0.001). The concentration increased significantly between<br />
weeks 20 and 36 in <strong>the</strong> vitamin C–supplemented group, but it<br />
decreased over <strong>the</strong> same period in <strong>the</strong> placebo group (betweensubjects<br />
differences: P 0.001; Table 2).<br />
The incidence <strong>of</strong> PROM was 4 (8%) <strong>of</strong> 52 women in <strong>the</strong><br />
vitamin C–supplemented group and 14 (25%) <strong>of</strong> 57 women in <strong>the</strong><br />
TABLE 1<br />
Characteristics and outcome variables 1<br />
Placebo<br />
group<br />
(n 57)<br />
<strong>Vitamin</strong> C<br />
group<br />
(n 52)<br />
Characteristics <strong>of</strong> <strong>the</strong> mo<strong>the</strong>rs<br />
Age (y) 27.4 7.7 2 27.5 7.4<br />
Number <strong>of</strong> gestations (n) 2.3 1.2 2.4 1.2<br />
Height (cm) 155.4 6.7 155.0 6.9<br />
Pregestational BMI (kg/m 2 ) 23.8 3.86 24.2 4.2<br />
Schooling (y) 11.0 3.1 10.3 2.7<br />
Married [n (%)] 35 (61) 33 (63)<br />
Characteristics <strong>of</strong> <strong>the</strong> fetuses<br />
Percentage <strong>of</strong> weight expected for 109 24 104 12<br />
height and gestational age at week<br />
20 (%)<br />
Gestational age at prenatal care (wk) 20 3 20 5<br />
Outcome results<br />
Birth weight (g) 3015 629 3015 513<br />
Gestational age at birth (wk) 38.0 3.1 38.5 2.0<br />
Premature births [n (%)] 14 (24) 7 (13.4)<br />
PROM [n (%)] 14 (24) 4 (7.6) 3<br />
1 PROM, <strong>premature</strong> <strong>rupture</strong> <strong>of</strong> <strong>the</strong> chorioamniotic membrane.<br />
2 x SD (all such values).<br />
3 Significantly different from placebo group, P 0.018 (chi-square<br />
test).<br />
Downloaded from www.ajcn.org by guest on January 5, 2012<br />
prgmea.com
862 CASANUEVA ET AL<br />
TABLE 2<br />
Concentration <strong>of</strong> vitamin C in plasma and leukocytes 1<br />
Weeks <strong>of</strong> gestation<br />
Placebo<br />
group<br />
(n 57)<br />
<strong>Vitamin</strong> C<br />
group<br />
(n 52) P 2<br />
Plasma (g/dL) 3<br />
20 0.78 0.28 0.74 0.28<br />
24 0.73 0.27 0.74 0.25<br />
28 0.72 0.26 0.72 0.29<br />
32 0.63 0.24 0.68 0.26<br />
36 0.55 0.25 0.58 0.21<br />
Leukocytes (g/10 8 cells) 4<br />
20 17.50 6.15 17.26 6.05 0.835<br />
24 17.28 5.79 18.98 6.30 0.145<br />
28 17.23 6.50 21.29 8.22 0.005<br />
32 15.79 6.47 21.56 7.47 0.001<br />
36 15.23 6.12 22.17 8.73 0.001<br />
1 All values are x SD.<br />
2 Comparison between groups for each week <strong>of</strong> pregnancy.<br />
3 1 g/dL 56.8 mol/L. Plasma vitamin C concentration: withinsubject<br />
difference (time), P 0.001; between-subject difference, P 0.760;<br />
<strong>the</strong>re was no significant time treatment interaction.<br />
4 1 g/10 8 cells 5.7 nmol/10 8 cells. Leukocyte vitamin C concentration:<br />
within-subject difference, P 0.01; between-subject difference, P <br />
0.001. P for interaction 0.001; P for time 0.001; for P for treatment <br />
0.001. Two-fac<strong>to</strong>r ANOVA with Tukey’s correction for repeated measure<br />
(gestational weeks 20–36).<br />
placebo group (P 0.018). <strong>Vitamin</strong> C <strong>supplementation</strong> appeared<br />
<strong>to</strong> have a protective effect <strong>of</strong> 74% and an RR <strong>of</strong> 0.26 (95%<br />
CI: 0.078, 0.837).<br />
The overall incidence <strong>of</strong> preterm labor was 21 (19%) in 109,<br />
but <strong>the</strong>re was no significant difference between groups (24% in<br />
<strong>the</strong> placebo group and 13% in <strong>the</strong> vitamin C group; P 0.142).<br />
Preterm labor occurred in 9 <strong>of</strong> 18 pregnancies complicated with<br />
PROM and in 12 <strong>of</strong> 91 pregnancies not complicated with PROM<br />
(RR: 6.58; 95% CI: 2.17, 19.89).<br />
DISCUSSION<br />
Although <strong>premature</strong> <strong>rupture</strong> <strong>of</strong> <strong>the</strong> membranes can have multiple<br />
causes, <strong>the</strong> mechanism that triggers <strong>the</strong> final damage affects<br />
<strong>the</strong> integrity <strong>of</strong> <strong>the</strong> amniochorion connective tissue by decreasing<br />
<strong>the</strong> tissular content <strong>of</strong> collagen and causing <strong>the</strong> sudden loss <strong>of</strong><br />
mechanical strength (1, 4). We hypo<strong>the</strong>sized that vitamin C <strong>supplementation</strong><br />
during pregnancy could <strong>prevent</strong> PROM by modulating<br />
collagen metabolism and favoring its deposit in fetal tissues,<br />
including <strong>the</strong> amniochorion membranes.<br />
Many fac<strong>to</strong>rs can alter <strong>the</strong> availability <strong>of</strong> vitamin C during<br />
pregnancy, and, under some circumstances, it might be necessary<br />
<strong>to</strong> adjust <strong>the</strong> current recommended daily dietary allowance. We<br />
assessed vitamin C status by measuring its concentration in<br />
plasma and leukocytes in 2 groups <strong>of</strong> pregnant women; one group<br />
ingested 100 mg vitamin C/d and <strong>the</strong> o<strong>the</strong>r ingested placebo. The<br />
plasma concentration <strong>of</strong> vitamin C did not differ significantly<br />
between groups. A possible explanation for this fact is that <strong>the</strong><br />
range <strong>of</strong> dietary vitamin C intakes is very small (40–230 mg<br />
vitamin C/d), and <strong>the</strong> authors who documented a direct and<br />
significant relation between vitamin C intake and its plasma<br />
concentration explored vitamin C intake ranges from 0 <strong>to</strong> 2500<br />
mg/d (8, 21, 22) In contrast, leukocyte concentrations increased<br />
in <strong>the</strong> vitamin C group but decreased in <strong>the</strong> placebo group, and<br />
leukocyte concentration is considered an indica<strong>to</strong>r <strong>of</strong> <strong>the</strong> s<strong>to</strong>red<br />
amount <strong>of</strong> vitamin (13, 23). We measured plasma vitamin C<br />
concentration in fasted subjects because its concentration in<br />
plasma is coregulated with blood glucose by insulin (24).<br />
Plasma vitamin C concentration decreased progressively during<br />
gestation regardless <strong>of</strong> <strong>supplementation</strong>. This decrease most<br />
likely reflects <strong>the</strong> effects <strong>of</strong> hemodilution (3, 25) and <strong>of</strong> active<br />
transport <strong>of</strong> vitamin C <strong>to</strong> <strong>the</strong> fetus, which increases throughout<br />
pregnancy (26). Leukocyte vitamin C concentration differed significantly<br />
between groups. Because <strong>the</strong> 2 groups did not differ in<br />
<strong>the</strong>ir dietary intake <strong>of</strong> vitamin C, <strong>the</strong>se changes most likely reflect<br />
<strong>the</strong> effect <strong>of</strong> <strong>supplementation</strong>, which suggests that <strong>the</strong> extra vitamin<br />
C was taken up by <strong>the</strong> leukocyte compartment. Thus,<br />
leukocyte vitamin C concentration might serve as a direct marker<br />
<strong>of</strong> compliance.<br />
The amount <strong>of</strong> vitamin C contained in <strong>the</strong> supplement tablet<br />
(100 mg/d) is less than <strong>the</strong> highest intake limit <strong>of</strong> 2000 mg/d<br />
established by <strong>the</strong> Institute <strong>of</strong> Medicine (27); this explains <strong>the</strong><br />
lack <strong>of</strong> adverse effects <strong>of</strong> <strong>supplementation</strong> in our study. A daily<br />
dose <strong>of</strong> 100 mg ascorbate in combination with <strong>the</strong> average dietary<br />
intake <strong>of</strong> 65 mg vitamin C appears <strong>to</strong> be sufficient <strong>to</strong> maintain<br />
leukocyte an ascorbic acid concentration <strong>of</strong> 18 g (102 nmol)/<br />
10 8 cells, which has been shown <strong>to</strong> <strong>prevent</strong> PROM (3). In our<br />
study, <strong>the</strong> incidence <strong>of</strong> PROM in <strong>the</strong> placebo group was 3 times<br />
that in <strong>the</strong> supplemented group, which represents a 76% protective<br />
effect <strong>of</strong> vitamin C <strong>supplementation</strong>. To our knowledge, this<br />
is <strong>the</strong> first example <strong>of</strong> a beneficial effect <strong>of</strong> vitamin C in lowering<br />
<strong>the</strong> incidence <strong>of</strong> PROM.<br />
Our data are consistent with a previous study <strong>of</strong> 2000 women<br />
that found an inverse relation between vitamin C intake and <strong>the</strong><br />
incidence <strong>of</strong> PROM (28), although only diet and clinical cervicovaginal<br />
infection were evaluated. Ano<strong>the</strong>r recent trial <strong>of</strong> vitamin<br />
C <strong>supplementation</strong> during pregnancy failed <strong>to</strong> show any<br />
beneficial effect on <strong>the</strong> incidence <strong>of</strong> preterm labor (29). However,<br />
<strong>the</strong> latter study used preterm labor as <strong>the</strong> primary outcome<br />
and did not evaluate <strong>the</strong> effect <strong>of</strong> <strong>supplementation</strong> on <strong>the</strong> incidence<br />
<strong>of</strong> PROM. Moreover, <strong>the</strong> dose <strong>of</strong> vitamin C was much<br />
higher (500 mg/d) than that in our study, and <strong>the</strong> method <strong>of</strong><br />
evaluating vitamin C concentration was colorimetric assay.<br />
Large doses <strong>of</strong> vitamin C can cause adverse reactions, such as<br />
those associated with oxidative stress (30). Reactive oxygen<br />
species can enhance collagen degradation in chorioamniotic<br />
membranes (31), which can interfere with <strong>the</strong> protective effect on<br />
<strong>the</strong> gene expression <strong>of</strong> metalloproteinases (eg, MMP-2) and can<br />
lead <strong>to</strong> increased collagen degradation, a condition thought <strong>to</strong> be<br />
an important mechanism in <strong>the</strong> genesis <strong>of</strong> PROM (32–34). This<br />
potential, undesirable effect must be taken in<strong>to</strong> account when<br />
establishing <strong>the</strong> supplement dose <strong>of</strong> vitamin C. We propose that<br />
vitamin C status could be used as a functional indica<strong>to</strong>r <strong>of</strong> <strong>the</strong> risk<br />
<strong>of</strong> PROM and that a leukocyte vitamin C concentration 18 g<br />
(102 nmol)/10 8 cells is an indica<strong>to</strong>r <strong>of</strong> adequate bioavailability <strong>of</strong><br />
<strong>the</strong> vitamin (35).<br />
We found no relation between infection and PROM, although<br />
38% <strong>of</strong> <strong>the</strong> women had cervicovaginal infections by week 20 <strong>of</strong><br />
gestation. We treated <strong>the</strong>se infections and found no infection<br />
relapses in <strong>the</strong> women.<br />
In conclusion, our data support <strong>the</strong> concept that vitamin C<br />
at dietary doses (100 mg/d) can <strong>prevent</strong> PROM. Because<br />
PROM may trigger 40% <strong>of</strong> all preterm labor, <strong>supplementation</strong><br />
could be a valuable <strong>to</strong>ol in sustaining pregnancy <strong>to</strong> term.<br />
Downloaded from www.ajcn.org by guest on January 5, 2012<br />
prgmea.com
PREVENTION OF PREMATURE RUPTURE OF MEMBRANES 863<br />
The next challenge is <strong>to</strong> design educational programs <strong>to</strong> promote<br />
adequate intakes <strong>of</strong> vitamin C through <strong>the</strong> consumption<br />
<strong>of</strong> fruit and vegetables and not through <strong>the</strong> taking <strong>of</strong> supplements<br />
during pregnancy.<br />
We thank <strong>the</strong> volunteer women for <strong>the</strong>ir valuable participation.<br />
EC assisted with <strong>the</strong> development <strong>of</strong> <strong>the</strong> research study pro<strong>to</strong>col, coordinated<br />
<strong>the</strong> study, performed <strong>the</strong> statistical analyses, interpreted <strong>the</strong> data, and<br />
<strong>to</strong>ok <strong>the</strong> major responsibility for writing <strong>the</strong> manuscript. CR assisted with <strong>the</strong><br />
recruitment and study <strong>of</strong> <strong>the</strong> subjects and collected data. MC and RMM<br />
performed <strong>the</strong> labora<strong>to</strong>ry experiments and collected data. FP assisted with<br />
coordination <strong>of</strong> <strong>the</strong> study and with writing <strong>the</strong> manuscript. PV assisted with<br />
<strong>the</strong> obstetric evaluations <strong>of</strong> <strong>the</strong> subjects. FVO assisted in <strong>the</strong> development <strong>of</strong><br />
<strong>the</strong> research pro<strong>to</strong>col, review <strong>of</strong> <strong>the</strong> literature, interpretation <strong>of</strong> <strong>the</strong> data, and<br />
revision <strong>of</strong> <strong>the</strong> manuscript. None <strong>of</strong> <strong>the</strong> authors had a personal or pr<strong>of</strong>essional<br />
conflict <strong>of</strong> interest.<br />
REFERENCES<br />
1. Parry S, Strauss JF. Premature <strong>rupture</strong> <strong>of</strong> <strong>the</strong> fetal membranes. N Engl<br />
J Med 1998;338:663–8.<br />
2. Woods JR Jr, Plessinger MA, Miller RK. <strong>Vitamin</strong>s C and E: missing<br />
links in <strong>prevent</strong>ing preterm <strong>premature</strong> <strong>rupture</strong> <strong>of</strong> membranes? Am J<br />
Obstet Gynecol 2001;185:5–10.<br />
3. Casanueva E, Vadillo-Ortega F, Pfeffer F, Tejero E. <strong>Vitamin</strong> C and<br />
<strong>premature</strong> <strong>rupture</strong> <strong>of</strong> chorioamniotic membranes. Nutr Res 1998;18:<br />
241–5.<br />
4. Bryant-Greenwood GD. The extracellular matrix <strong>of</strong> <strong>the</strong> human fetal<br />
membranes: structure and function. Placenta 1998;19:1–11.<br />
5. Tejero E, Perichart O, Pfeffer F, Casanueva E. Vadillo-Ortega F. Collagen<br />
syn<strong>the</strong>sis during pregnancy, vitamin C availability and risk <strong>of</strong><br />
<strong>premature</strong> <strong>rupture</strong> <strong>of</strong> fetal membranes. Int J Gynecol Obstet 2003;81:<br />
29–34.<br />
6. Levine M. New concepts in <strong>the</strong> biology and biochemistry <strong>of</strong> ascorbic<br />
acid. N Engl J Med 1986;314:892–902.<br />
7. Pfeffer F, Casanueva E, Kamar J, Guerra A, Perichart O, Vadillo-Ortega<br />
F. Modulation <strong>of</strong> 72-kilodal<strong>to</strong>n type IV collagenase (matrix<br />
metalloproteinase-2) by ascorbic acid in cultured human amnionderived<br />
cells. Biol Reprod 1998;59:326–9.<br />
8. Levine M, Wang Y, Padayatty SJ, Morrow J. A new recommended<br />
dietary allowance <strong>of</strong> vitamin C for healthy young women. Proc Natl<br />
Acad Sci USA2001;98:9842–6.<br />
9. Casanueva E, Angulo ME, Goldberg S, Pfeffer F, Meza-Camacho C,<br />
Vadillo-Ortega F. Bases para estimar las necesidades de vitamina C en<br />
la gestación. [The basis for recommendations for vitamin C in pregnancy.]<br />
Gac Med Mex (in press) (in Spanish).<br />
10. Gomez R, Romero R, Edwin SS, David C. Pathogenesis <strong>of</strong> preterm labor<br />
and preterm <strong>premature</strong> <strong>rupture</strong> <strong>of</strong> membranes associated with intraamniotic<br />
infection. Infect Dis Clin North Am 1997;11:135–76.<br />
11. Frei B. Reactive oxygen species and antioxidant vitamins: mechanisms<br />
<strong>of</strong> action. Am J Med 1994;97:5S–13S.<br />
12. Casanueva E, Reyes L, Luna A, Tejero E, Pfeffer F, Meza C. <strong>Vitamin</strong> C<br />
and cervicovaginal infections in pregnant women. Nutr Res 1998;18:<br />
939–44.<br />
13. Asociación de Agencias de Estudios de Mercado y Opinión 2003 (Mexican<br />
Association <strong>of</strong> Marketing and Opinion Research). Socioeconomic<br />
status scale. Internet: www.amai.org (accessed 30 May 2003).<br />
14. Romieu I, Parra S, Hernandez JF, Madrigal H, Willet W, Hernandez M.<br />
Questionnaire assessment <strong>of</strong> antioxidants and retinal intakes in Mexican<br />
woman. Arch Med Res 1999;30:224–39.<br />
15. Sauberlich HE. Labora<strong>to</strong>ry tests for <strong>the</strong> assessment <strong>of</strong> nutritional status.<br />
2nd ed. Boca Ra<strong>to</strong>n, FL: CRC Press, 1999:11–28.<br />
16. Carey JC, Kleban<strong>of</strong>f MA. What have we learned about vaginal infections<br />
and preterm delivery? Semin Perina<strong>to</strong>l 2003;27:212–6.<br />
17. Premature <strong>rupture</strong> <strong>of</strong> membranes. Clinical management guidelines for<br />
obstetrician-gynecologists. ACOG Practice Bulletin. Int J Gynaecol Obstet<br />
1998;63:75–84.<br />
18. Capurro J, Konichezky S, Fonseca D, Caldeyro-Barcia R. A simplified<br />
method for diagnosis <strong>of</strong> gestational age in <strong>the</strong> newborn infant. J Pediatr<br />
1978;93:120–2.<br />
19. Omaye ST, Schaus EE, Kutnink MA, Hawkees WC. Measurement <strong>of</strong><br />
vitamin C in blood components by high-performance liquid chroma<strong>to</strong>graphy.<br />
Ann N Y Acad Sci 1987;498:398–402.<br />
20. Lee W, Hamernyik P, Hutchinson M, Raisuys VA, Labbe RF. Ascorbic<br />
acid in lymphocytes: cell preparation and liquid-chroma<strong>to</strong>graphic assay.<br />
Clin Chem 1982;10:2165–9.<br />
21. Bejarano L, Pfeffer F, Tejero E, Meza C, Casanueva E. Concentraciones<br />
plasmáticas y leucocitarias de vitamina C en la gestación. [<strong>Vitamin</strong> C<br />
concentrations in plasma and leukocytes during pregnancy.] Perina<strong>to</strong>l<br />
Reprod Hum 1994;8217–21 (in Spanish).<br />
22. Jacob RA. <strong>Vitamin</strong> C. In: Shills ME, Olson JA, Shike M, Ross AC, eds.<br />
Modern nutrition in health and disease. 9th ed. Philadelphia: Lippincott<br />
Williams & Wilkins, 1999:467–83.<br />
23. Rumsey SC, Kwon O, Xu GW, Burant CF, Simpson I, Levine M. Glucose<br />
transported is<strong>of</strong>orms GLUT1 and GLUT3 transport dehydroascorbic<br />
acid. J Biol Chem 1997;272:18982–9.<br />
24. Morse EH, Clark RP, Keyser DE, Merrow SB, Bee DE. Comparison <strong>of</strong><br />
<strong>the</strong> nutritional status <strong>of</strong> pregnant adolescents with adult pregnant<br />
women. I. Biochemistry findings Am J Clin Nutr 1975;28:1000–13.<br />
25. Choi JL, Rose RC. Transport and metabolism <strong>of</strong> ascorbic acid in human<br />
placenta. Am J Physiol 1989;257:110–3.<br />
26. Food and Nutrition Board, Institute <strong>of</strong> Medicine. Dietary reference intakes<br />
for vitamin C, vitamin E, selenium and carotenoids. Washing<strong>to</strong>n,<br />
DC: National Academy Press, 2000:95–185.<br />
27. Siega-Riz AM, Promislow JH, Savitz DA, Throp JM Jr, McDonald T.<br />
<strong>Vitamin</strong> C intake and <strong>the</strong> risk <strong>of</strong> preterm delivery. Am J Obstet Gynecol<br />
2003;189:519–25.<br />
28. Steyn PS, Odendaal HJ, Schoeman J, Stander C, Fanie N, Grove D. A<br />
randomised, double-blind placebo-controlled trial <strong>of</strong> ascorbic acid <strong>supplementation</strong><br />
for <strong>the</strong> <strong>prevent</strong>ion <strong>of</strong> preterm labour. J Obstet Gynaecol<br />
2003;23:150–5.<br />
29. Naidu KA. <strong>Vitamin</strong> C in human health and disease is still a mystery? An<br />
overview. Nutr J 2003;2:7–16.<br />
30. Woods JR Jr. Reactive oxygen species and preterm <strong>premature</strong> <strong>rupture</strong> <strong>of</strong><br />
membranes—a review. Placenta 2001;22:38s–44s.<br />
31. Vadillo-Ortega F, Hernández MA, González-Avila G, Bermejo L, Iwata<br />
K, Strauss J. Increased matrix metalloproteinase activity and reduced<br />
tissue inhibi<strong>to</strong>r <strong>of</strong> metalloproteinases-1 levels in amniotic fluids from<br />
pregnancies complicated by <strong>premature</strong> <strong>rupture</strong> <strong>of</strong> membranes. Am J<br />
Obstet Gynecol 1996;174:1371–6.<br />
32. Maymon E, Romero R, Pacora P, et al. Evidence for <strong>the</strong> participation <strong>of</strong><br />
interstitial collagenase (matrix metalloproteinase 1) in preterm <strong>premature</strong><br />
<strong>rupture</strong> <strong>of</strong> membranes. Am J Obstet Gynecol 2000;183:914–20.<br />
33. Fortuna<strong>to</strong> SJ, Menon R. Distinct molecular events suggest different<br />
pathways for preterm labor and <strong>premature</strong> <strong>rupture</strong> <strong>of</strong> membranes. Am J<br />
Obstet Gynecol 2001;184:1399–405.<br />
34. Casanueva E, Magaña L, Pfeffer F, Báez A. Incidence <strong>of</strong> <strong>premature</strong><br />
<strong>rupture</strong> <strong>of</strong> membranes in pregnant women with low leukocyte levels <strong>of</strong><br />
vitamin C. Eur J Clin Nutr 1991;45:401–5.<br />
35. Arroyo P. Casanueva E, Reynoso M. Peso esperado para la talla y edad<br />
gestacional. Tablas de referencia. [Weight for height and gestational age.<br />
Reference tables.] Ginecol Obstet Mex 1985;53:227–31 (in Spanish).<br />
Downloaded from www.ajcn.org by guest on January 5, 2012<br />
prgmea.com