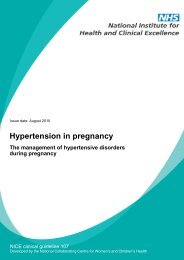
Herpes Vulvitis
Herpes Vulvitis
Herpes Vulvitis
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
22/02/53<br />
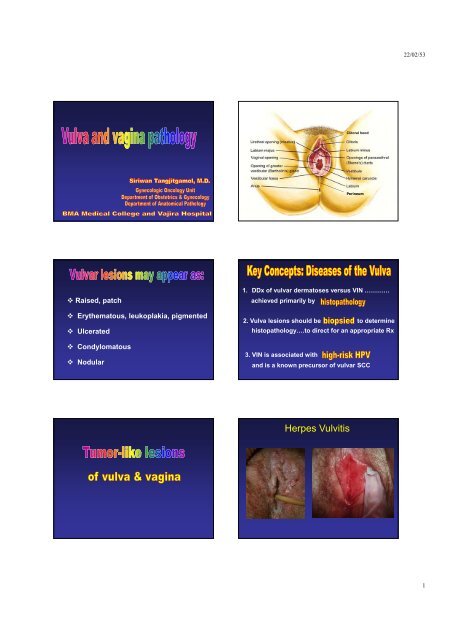
Clitoral hood<br />
Perineum<br />
Raised, patch<br />
Erythematous, leukoplakia, pigmented<br />
Ulcerated<br />
Condylomatous<br />
Nodular<br />
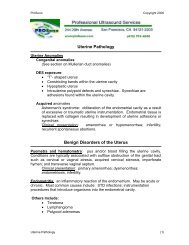
1. DDx of vulvar dermatoses versus VIN …………<br />
achieved primarily by<br />
2. Vulva lesions should be to determine<br />
histopathology….to direct for an appropriate Rx<br />
3. VIN is associated with<br />
and is a known precursor of vulvar SCC<br />
<strong>Herpes</strong> <strong>Vulvitis</strong><br />
1
22/02/53<br />
Bartholin Duct Cyst<br />
Bartholin's Abscess<br />
Vaginal Wall Cyst<br />
(Gartner’s duct cyst)<br />
Epidermal inclusion cyst<br />
cyst of hair follicle (follicular cyst)<br />
Skene duct cyst<br />
Cyst of vulva<br />
lining<br />
wall<br />
Bartholin duct<br />
cyst<br />
Sq, transition,<br />
mucinous<br />
Bartholin gl.<br />
Mucinous vestibule<br />
cyst<br />
Mucinous , sq<br />
metaplasia<br />
No smooth<br />
musle<br />
Mesonephric<br />
like cyst<br />
Low cuboid,<br />
col. No ciliated<br />
Sm muscle<br />
beneath BM<br />
2<br />
prgmea.com
22/02/53<br />
may express in 3 forms<br />
1. Fully expressed….as c. acuminata<br />
2. Minimally expressed….as koilocytes<br />
3. Latent….no morphological changes<br />
(detected only by molecular technique)<br />
Moist-- appear white<br />
frequently occur at multiple sites<br />
Parakeratosis<br />
papillomatosis<br />
hyperkeratosis<br />
Gross: Dry– appear brown<br />
Verrucous appearance<br />
Condyloma acuminata<br />
May be solitary, but more of multiple and coalesce<br />
May involve perineal, vulvar, perianal, vagina, and cervix<br />
Acanthosis<br />
Parakeratosis<br />
Basal cell hyperplasia<br />
koilocytes (perinuclear “halo”)<br />
freq seen in upper layer of epidermis<br />
koilocytosis (perinuclear “halo”)<br />
3<br />
prgmea.com
22/02/53<br />
Fibrovascular core, covered by sq epith.<br />
Paillomatosis<br />
Lack koilocytosis!<br />
Squamous papilloma<br />
Lichen sclerosus et atrophicus<br />
Clinical:<br />
• Whitened thinned epithelium<br />
• Symmetrical distribution<br />
• Labia minora shrinkage and agglutination in late stages.<br />
• Narrowed introitus or perianal stenosis (in children)<br />
• Occur in all ages grps, but common in postmenopause...<br />
• Unclear pathogenesis<br />
(genetic, autoimmunity, hormonal factors)<br />
• Insidious and progressive<br />
• Causes discomfort & predisposes to infection<br />
• Generally, not a precancerous condition<br />
BUT….a small proportion (about 1% to 4%) have been<br />
observed to develop carcinoma.<br />
1. Epithelial thinning/ hyperkeratosis<br />
2. Flattening rete ridges<br />
3. dermal edema and fibrosis<br />
Epithelial thinning with hyperkeratosis<br />
Hypertrophic vulvar dystrophy<br />
4. inflammatory cells<br />
Flattening of rete ridges<br />
Subepithelial or dermal edema and<br />
collagenous fibrous tissue change<br />
Chronic inflammatory cells in the areas<br />
4<br />
prgmea.com
22/02/53<br />
hyperkeratosis...<br />
thickened keratin layer<br />
(secondary lichenification)<br />
expanded papillary dermis.<br />
**Biopsy is indicated in all lesions……<br />
thickened epithelium, increased mitotic activity in both basal & prickle cell layers<br />
even those that are not so suspicious<br />
variable leukocytic infiltration of the dermis...<br />
squamous hyperplasia<br />
(previously called hyperplastic dystrophy)<br />
Lymphocytic inflammatory reaction<br />
Sclerotic or edematous change of<br />
dermoepidermal junction<br />
may present as:<br />
ulcer<br />
nodule<br />
macule<br />
pedunculated mass<br />
discharge<br />
bleed<br />
pain<br />
5<br />
prgmea.com
22/02/53<br />
Vulvar Intraepithelial Neoplasia<br />
(VIN)<br />
An intraepithelial squamous neoplasm of the vulva.<br />
If multiple abnormal areas , then ……..<br />
multiple biopsies are required……..<br />
to "map" all potential sites of vulvar pathology.<br />
Usually associated with high risk HPV infection,<br />
especially ill types 16 or 18.<br />
peak kincidence id ~ 20-35 yrs<br />
1/5 were assocd with SCC<br />
May follow, or be associated with cervical or vaginal<br />
neoplasia.<br />
A known precursor of vulvar squamous cell CA<br />
~ 3% of genital malignancies in women<br />
VIN: LESION COLOR (N=73)<br />
1. VIN and associated HPV infection (usually HPV type 16).<br />
2. The simplex (differentiated) type of VIN, not associated<br />
with HPV infection<br />
3. Lichen sclerosus with associated squamous hyperplasia<br />
4. Chronic granulomatous vulvar disease such as<br />
granuloma inguinale (rare in developed countries)<br />
Color Patients # %<br />
White 41 56.2<br />
Red 13 17.8<br />
Pigmented 12 16.4<br />
Unavailable 7 9.6<br />
Wilkinson EJ, World Health Organization, 2004<br />
Wilkinson EJ<br />
6
22/02/53<br />
VIN: type of lesion (N=73)<br />
Presentation Patients # %<br />
Multifocal l 57 78.1<br />
Unifocal 15 20.5<br />
Confluent 1 1.4<br />
VIN type SCC Type HPV Related<br />
Warty Condylomatous (Warty) Yes<br />
carcinoma<br />
Basaloid Basaloid carcinoma Yes<br />
Differentiated Keratinizing carcinoma No<br />
(Simplex type)<br />
Wilkinson EJ<br />
VIN 1 Mild dysplasia<br />
VIN 2<br />
Moderate dysplasia<br />
VIN 3 Severe dysplasia (8077/2)<br />
VIN 3 Carcinoma in situ (8072/2)<br />
* ICD-O, International Classification of Disease for Oncology<br />
Wilkinson EJ et al. Histological Typing of Female Genital Tract Tumors, in World Health Organization International Histological Classification of Tumours<br />
third Ed., 2004<br />
*<br />
VIN 1: abnormal epithelial cell involve lower 1/3 of the<br />
epithelium (maturation in the upper 2/3 of epithelium)<br />
VIN 2: abnormal epithelial cell involve lower 1/2 of the<br />
epithelium (maturation in the upper 1/2 of epithelium)<br />
VIN 3: abnormal epithelial cell involve most or all of the<br />
epithelium ( maturation present in the upper 1/3 of epithelium)<br />
Wilkinson EJ, World Health Organization, 2004<br />
VIN I<br />
Key points:<br />
Proliferation of basal layer<br />
Koilocytotic atypia<br />
* Enlarged pleomorphic nuclei<br />
* vacuolated cytoplasm<br />
-Disordered maturation<br />
* loss of polarity<br />
-Nuclear atypia<br />
* pleomorphism<br />
* coarse chromatin<br />
* irregular nuclear<br />
membrane<br />
* atypical MF<br />
VIN II<br />
• More proliferation<br />
• cytologic atypia in<br />
basal/parabasal<br />
layers<br />
• involving lower 1/2<br />
epithelium<br />
7
22/02/53<br />
Full thickness epith.<br />
replaced by abnormal<br />
basal and parabasal<br />
cells.<br />
VIN 3<br />
Oval nuclei with axis perpendicular to BM, except<br />
superficial layer where they are horizontal<br />
Bowenoid type<br />
VIN 3<br />
Basaloid type<br />
VIN 3<br />
VIN of differentiated<br />
(simplex) type<br />
Atypia is confined to basal<br />
& parabasal layers<br />
Squamous cell with maturation<br />
on epithelial-stromal junction<br />
suggestive of impending<br />
invasion<br />
8
22/02/53<br />
Cases should be classified as CA vulva when<br />
1 o site of the growth is in the vulva.<br />
Exclude 2 O tumor growth from other genital or<br />
extra- genital site<br />
Vulva CA VS CA vagina<br />
Malignant melanoma should be reported<br />
separately.<br />
A. Squamous cell carcinoma<br />
B. Adenocarcinoma<br />
C. Adenoid cystic carcinoma<br />
D. Adenosquamous carcinoma<br />
E. Transitional cell carcinoma<br />
F. Undifferentiated<br />
A. Embryonal rhabdomyosarcoma<br />
(sarcoma botryoides)<br />
B. Leiomyosarcoma<br />
C. Malignant fibrous histiocytoma<br />
D. Epithelioid sarcoma<br />
E. Aggressive angiomyxoma<br />
F. Dermatofibrosarcoma<br />
protuberans<br />
G. Epithelioid sarcoma<br />
H. Malignant rhabdoid tumor<br />
I. Malignant nerve sheath<br />
tumor<br />
J. Angiosarcoma<br />
K. Kaposi sarcoma<br />
L. Hemangiopericytoma<br />
M. Liposarcoma<br />
N. Alveolar soft part sarcoma<br />
O. Other sarcomas(Enzinger<br />
& Weiss or WHO)<br />
9
22/02/53<br />
A. Malignant melanoma<br />
B. Endodermal sinus tumor (yolk sac tumour)<br />
C. Neuroectodermal tumours (Merkel cell)<br />
D. Lymphomas<br />
E. Others<br />
Most epithelial malignant tumours (carcinomas)<br />
are fr. skin, mucosa or rarely bartholin gld.,<br />
~ 3% of all female genital CA<br />
90% are SCC, the remainder are melanoma,<br />
basal cell carcinomas, or adenocarcinoma<br />
A. Invasive Squamous cell carcinoma<br />
1. Keratinizing<br />
2. Non-keratinizing<br />
3. Basaloid carcinoma<br />
HPV related 4. Verrucous Carcinoma<br />
5. Warty carcinoma [condylomatous]<br />
B. Basal cell carcinoma<br />
C. Adenocarcinoma<br />
S<br />
q<br />
u<br />
a<br />
m<br />
o<br />
u<br />
s<br />
c<br />
e<br />
ll<br />
C<br />
A<br />
10
22/02/53<br />
• Uncommon variant of SCC, low malignant behavior<br />
• Very slow growing, although can grow very large,<br />
still carry an excellent prognosis.<br />
• Gross: may resemble condyloma acuminatum and<br />
present as a large fungating or cauliflower tumor<br />
mass.<br />
Exo- and endophytic<br />
tumor growth<br />
Papillomatosis (lack connective tissue core as seen in c.acuminata)<br />
hyperkeratosis<br />
undulating surface,<br />
pushing border,<br />
Tumor with pushing border, with acanthotic rete ridges extending<br />
deep into underlying tissue<br />
well differentiated SCC<br />
minimal cytologic atypia<br />
For recurrence:<br />
1. Stage, advanced<br />
2. Size > 2.5 cm<br />
3. Multifocal<br />
4. LVSI<br />
5. Assocd. VIN 2-3<br />
6. Margin involvement<br />
For survival:<br />
7. LN involvement<br />
8. Mode of treatmentt t<br />
9. Spray or finger-like pattern<br />
11
22/02/53<br />
Tumor nests& cords<br />
basal cell, showing<br />
peripheral palisading<br />
Malignant skin tumor, cells of basal layer of epidermis & adnexal structures.<br />
The College of American Pathologists (CAP)<br />
Small foci of<br />
sq.differentiation<br />
1. Depth of tumor invasion.<br />
2. Tumor thickness.<br />
3. Method of measurement…..depth th of invasion<br />
i<br />
& tumor thickness.<br />
4. Presence vascular space involvement<br />
5. Diameter of tumor, including the clinically<br />
measured diameter if available.<br />
Wilkinson EJ. Arch Path Lab Med 2000;124:51-6,<br />
A: Depth of invasion<br />
epithelium-stromal junction of<br />
Methods of<br />
the most superficial dermal<br />
papillae to the deepest<br />
invasion<br />
A<br />
B<br />
C<br />
B: measurement<br />
Tumor thickness<br />
Surface of the lesion to the<br />
deepest invasion<br />
of superficial<br />
C: Tumor thickness<br />
Paget disease<br />
Melanoma<br />
(when suface is keratinized)<br />
granular layer to the deepest<br />
invasion invasive CA<br />
ISSVD: Wilkinson EJ, Lynch PJ, Kneale B. J Reprod Med 31:973-4, 1986<br />
12
22/02/53<br />
* 1 st described in 1888, Crocker reported Paget<br />
disease of scrotum and penis, 2 o to bladder CA<br />
* Most commonly involves external genitalia, less<br />
common over perianus<br />
* Also reported in other areas of axilla, umbilicus,<br />
groins, eyelids, external ear canal.<br />
* Age: 45-91 yrs (median 67 yrs)<br />
* Associated carcinoma: 4-20%<br />
* Surgery: radical vulvectomy, partial vulvectomy,<br />
wide local l excision<br />
i<br />
* Recurrence rate 30-69% after surgery<br />
* Free margin : F.S., fluorescein-aided visualization<br />
(Controversy on significance of surgical margin)<br />
Wilkinson EJ & Brown HB, Human Pathology. 2003<br />
Brummer et al. Gynecol Oncol 2004;95:336-40.<br />
Molinie etal. Ann Dermatol Venereol 1993;120:522-7<br />
Lu et al. Zhonghua Fu Chan Ke Za Zhi 1999;34:156-8<br />
Misas et al. Obstet Gynecol 1991;77:156-9.<br />
Primary Paget disease:<br />
* as a 1 o intraepithelial neoplasm.<br />
* as an intraepithelial neoplasm with invasion.<br />
* as a manifestation of an underlying cutaneous, or vulvar ACA<br />
Secondary Paget disease:<br />
* 2 o to adjacent non-cutaneous ACA (e.g. anal or rectal ACA)<br />
* of urothelial origin (PUIN) (pagetoid urothelial intraepithelial neoplasia)<br />
PUIN as a manifestation of intraepithelial urothelial neoplasia (CIS)<br />
or invasive urothelial CA<br />
* of other origins<br />
Wilkinson EJ and Brown HB, Human Pathology. 2003<br />
1 o lesion (more common)<br />
* arise within epidermis & extend into<br />
contiguous epithelium of skin<br />
* arise from skin appendages (usually<br />
apocrine glands) & extend to overlying<br />
epidermis by epidermotropism.<br />
2 o lesion<br />
* non-cutaneous CA--- involves skin by direct<br />
extension or epidermotropic metastasis<br />
Wilkinson EJ and Brown HB, Human Pathology. 2003<br />
Paget disease in<br />
vulvectomy specimen<br />
Paget disease of vulva<br />
13
22/02/53<br />
Clinical:<br />
* Pruritic red, crusted, sharply demarcated, maplike area,<br />
* Occurring usually on the labia majora.<br />
* Possible palpable submucosal thickening or tumor<br />
BUT….tumor cells often extend into skin appendages and<br />
may extend beyond the confines of the grossly visible<br />
lesion----- prone to recurrence.<br />
Prognosis is poor if associated with<br />
invasive cancer!!<br />
Paget disease as an intraepidermal lesion, may persist for<br />
many years without invasion.<br />
Clear halo, containing mucopolysaccharide<br />
(+ PAS, alcian blue, or mucicarmine stains)<br />
finely granular cytoplasm<br />
Single or small nests of large tumor cells in epidermis<br />
Ultrastructure: Paget cells display apocrine, eccrine, &<br />
keratinocyte differentiation<br />
Presumably arise from primitive epithelial progenitor cells.<br />
pale cytoplasm<br />
(stain for mucin, PAS-D stain, CEA, EMA)<br />
1 o Paget dis. 2 o Paget dis.<br />
prominent nucleolus<br />
wide & deep surgical excision<br />
directed toward Rx of ass. CA<br />
large round to oval nuclei<br />
40X<br />
14
22/02/53<br />
DDx of vulvar intraepithelial Pagetoid cells<br />
• 1 o Paget Disease<br />
Usually requires IHC to distinguish<br />
• 2 o Paget disease<br />
• Vulva intraepithelial neoplasia<br />
• Superficial spreading melanoma<br />
• Pagetoid Spitz nevus<br />
• Sebaceous carcinoma<br />
• Merkel cell carcinoma<br />
• Clear cell papulosis (related to Toker cells)<br />
• Cutaneous T-cell lymphoma<br />
• Histiocytosis X<br />
• Langerhans’ cell microabscess<br />
• Benign mucinous metaplasia of vulva<br />
IHC findings of Paget disease<br />
Type CK-7 CK-20 GCDFP-15 CEA UP- III<br />
1 O skin + - + + (most) -<br />
1 O anorectal CA (+) + - + (>90%) -<br />
1 O urothelial CA + (+) - + (67%) + (50-60%)<br />
CK, cytokeratin; CEA, carcinoembryonic antigen; GCDFP, gross cystic disease fluid protein;<br />
UP, uroplakin<br />
Brown & Wilkinson. Hum Pathol 2002;33:545-8.<br />
Tumor of vagina<br />
• Epithelial tumor<br />
Tumor of vagina<br />
• Mesenchymal tumor<br />
• Mixed epithelial and mesenchymal tumor<br />
• Melanocytic tumor<br />
• Miscellaneous tumor<br />
Epithelial tumor<br />
• Squamous tumor :<br />
– squamous cell carcinoma : keratinizing,<br />
nonkeratinizing, basaloid, verrucous, warty<br />
– Squamous intraepithelial neoplasia : VAIN<br />
– Benign squamous lesions : Condyloma<br />
acuminata, squamous papilloma (vaginal<br />
micropapillomatosis), fibroepithelial polyp<br />
Epithelial tumor<br />
• Glandular tumor<br />
– Clear cell adenocarcinoma<br />
– Endometrioid adenocarcinoma<br />
Mucinous adenocarcinoma<br />
– Mucinous adenocarcinoma<br />
– Mesonephric adenocarcinoma<br />
– Malignant papilloma<br />
– Adenoma : tubular, tubulovillous, villous<br />
15
22/02/53<br />
Epithelial tumor<br />
• Other epithelial tumors<br />
– Adenosquamous carcinoma<br />
– Adenoid cystic carcinoma<br />
– Adenoid basal carcinoma<br />
– Carcinoid<br />
– Small cell carcinoma<br />
– Undifferentiated carcinoma<br />
Vaginal intraepithelial neoplasia (VAIN)<br />
• Premalignant lesion of the vainal squamous<br />
epithelium that can develop primary in the<br />
vagina or as an extension from the cervix<br />
• Histologically VAIN is defined in the same way<br />
as cervical intraepithelial neoplasia (CIN)<br />
Vaginal intraepithelial neoplasia (VAIN)<br />
• Much less common than CIN<br />
• Mean age is 50 years<br />
• Majority occur in prior hysterectomy or history of<br />
cervical or vulvar neoplasia<br />
• Increase incidence among young and<br />
immunosuppressed women<br />
• Associated with HPV infection (HPV type 16)<br />
Vaginal intraepithelial neoplasia (VAIN)<br />
• More commonly multifocal<br />
• Isolated lesion are mainly in the upper third of<br />
vagina and vaginal vault after hysterectomy<br />
• VAIN is asymptomatic and cannot be diagnosed<br />
by the naked eye<br />
• Detection is by mean of colposcopic biopsy<br />
Vaginal intraepithelial neoplasia (VAIN)<br />
Vaginal intraepithelial neoplasia (VAIN)<br />
• VAIN is always iodine-negative<br />
• Presence of punctuation on a sharply<br />
demarcated aceto-white area is the sinle<br />
most reliable feture suggestive of VAIN<br />
• Histopathology is the same as CIN<br />
16
22/02/53<br />
Vaginal intraepithelial neoplasia (VAIN)<br />
• Differential diagnosis<br />
– Atrophy<br />
– Squamous atypia<br />
– Transitional metaplasia<br />
Vaginal intraepithelial neoplasia (VAIN)<br />
• Prognosis<br />
– Low grade VAIN : 88% regress without treatment<br />
– High grade VAIN : 8% progress to invasive CA<br />
– Recurrent rate is 33%<br />
Mesenchymal tumor<br />
• Sarcoma botryoides<br />
• Leiomyosarcoma<br />
• Endometrioid stromal sarcoma, low grade<br />
• Undifferentiated vaginal sarcoma<br />
• Leiomyoma<br />
• Genital rhabdomyoma<br />
• Deep angiomyxoma<br />
• Postoperative spindle cell nodule<br />
Sarcoma botryoides<br />
• A malignant mesenchymal tuor composed<br />
of small round or oval to spindle shaped<br />
cells some of which show evidence of<br />
striated muscle differentiation<br />
• Embryonal rhabdomyosarcoma<br />
Sarcoma botryoides<br />
• Most common vaginal sarcoma<br />
• Occurs almost exclusively in children and infants<br />
< 5 years of age (mean 1.8 years)<br />
• Occuring in young adult, pregnancy,<br />
postmenopausal women were reported<br />
• Present as a vaginal mass with soft edematous<br />
polypoid nodules or grape-like nodules often<br />
protruding through the introitus<br />
Sarcoma botryoides<br />
• Most common vaginal sarcoma<br />
• Occurs almost exclusively in children and<br />
infants < 5 years of age (mean 1.8 years)<br />
• Occuring in young adult, pregnancy,<br />
postmenopausal women were reported<br />
• Present as a vaginal mass with soft<br />
edematous polypoid nodules or grape-like<br />
nodules often protruding through the<br />
introitus<br />
17
22/02/53<br />
Sarcoma botryoides<br />
Sarcoma botryoides<br />
Sarcoma botryoides<br />
Benign conditions<br />
Vaginal adenosis<br />
• Found in 1/3 asymptomatic girls or young women<br />
exposed to DES, CO2laser vaporization, tropical 5FU<br />
treatment of condyloma<br />
• Rare in postmenopausal age group<br />
• Upper 1/3 of vagina usually effect, middle 1/3 10%,<br />
lower1/3 2%<br />
• Adenosis rarely develop clear cell adenocarcinoma or<br />
vaginal intraepithelial neoplasia<br />
Adenosis<br />
Micro :<br />
• Benign type columnar<br />
epithelium replaces<br />
normal squamous<br />
epithelium or forms<br />
glands within superficial<br />
stroma<br />
• Endocervical or<br />
tuboendometrioid<br />
• Squamous metaplasia of<br />
glands may be missed<br />
diagnosis as squamous<br />
cell CA<br />
18
22/02/53<br />
Postoperative Spindle Cell Nodule(PSCN)<br />
• Reactive pseudosarcomatous spindle cell<br />
lesion<br />
• Develop shortly after operation on lower<br />
genitourinary tract<br />
• Detect in operative site 112 weeks after surgy<br />
• PSCN in upper vagina usually followed<br />
vaginal hysterectomy<br />
• PSCN in lower vagina or vulva usually<br />
followed episiotomy<br />
Postoperative Spindle Cell Nodule(PSCN)<br />
• Benign clinical<br />
• Rare recur<br />
• Soft polypoid mass
22/02/53<br />
Fibroepithelial polyp<br />
• Usually single , may be multiple<br />
• Sessile , pedunculated, botryoid appearance<br />
•
22/02/53<br />
Aggressive angiomyxoma<br />
• Differential diagnosis :<br />
– Angiomyofibroblastoma (superficial location,<br />
small size, absence of thick wall muscular<br />
vessels, ,p presence of PMNs)<br />
–Myxoma<br />
21