5 - Complaints, Grievances & Appeals
5 - Complaints, Grievances & Appeals
5 - Complaints, Grievances & Appeals
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
may also file expedited level two grievances. Empire<br />
will respond to them within 72 hours of receipt of the<br />
grievance.<br />
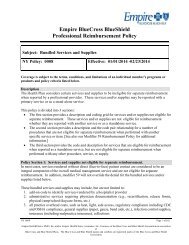
Below are time frames for Empire’s response to<br />
grievances.<br />
Standard<br />
Expedited<br />
Level One<br />
Within 30 calendar<br />
days from our<br />
receipt of the<br />
grievance.<br />
Within 72 hours<br />
from our receipt of<br />
the grievance<br />
RECONSIDERATIONS<br />
AND APPEALS<br />
If the Medical Management Department determines<br />
that an admission, extension of the hospital stay, or<br />
some other healthcare service is not medically<br />
necessary, you may request reconsideration (through<br />
the attending physician) or appeal the decision in the<br />
ways described in the following sections.<br />
Reconsiderations<br />
A request for reconsideration can be made by calling<br />
or writing to the Medical Management Department,<br />
the specific contact information for which will be<br />
listed on the denial letter. The hospital or the<br />
physician who recommended the admission, the<br />
extension of a stay, or other healthcare services can<br />
make the request for reconsideration. In addition,<br />
the request can be made only:<br />
If we deny service prior to or during a member’s<br />
medical service, and<br />
If the denial is based on issues of medical<br />
necessity, and<br />
If the decision occurred without our Medical Director<br />
discussing the hospitalization or other services with<br />
the physician who recommended them.<br />
Services that have already been provided<br />
are not subject to reconsideration.<br />
Level Two<br />
Within 30 calendar<br />
days from our<br />
receipt of the<br />
grievance.<br />
Within 72 hours<br />
from our receipt of<br />
the grievance<br />
A reconsideration may be filed within seven<br />
calendar days of our initial pre-service (prospective)<br />
determination by contacting the Case Management<br />
Department which rendered the initial denial of<br />
service.<br />
All reconsideration requests that are received<br />
beyond seven calendar days of the initial pre-service<br />
denial should be addressed to the <strong>Appeals</strong> Unit and<br />
will be processed as appeals.<br />
A request for reconsideration will be reviewed within<br />
one business day by the Medical Director who made the<br />
initial decision to deny the precertification or the<br />
extension of service. The review will include any<br />
additional information provided. If the Medical Director<br />
who made the initial decision is not available, another<br />
Medical Director may act in his or her place.<br />
If we uphold our prior decision, written notification will<br />
be provided. This notification will include the following:<br />
The reasons for the decision, including the clinical<br />
rationale<br />
Information on how to obtain a copy of the clinical<br />
review criteria used in making the decision<br />
Instructions on how to initiate an appeal<br />
What additional information, if any, must be<br />
provided to or obtained by us in order to make a<br />
decision on appeal<br />
<strong>Appeals</strong><br />
<strong>Appeals</strong> are requests to review and change unfavorable<br />
clinical decisions (also called adverse determinations)<br />
such as when an admission, the extension of a stay or<br />
some other healthcare service is determined not to be<br />
medically necessary.<br />
Expedited <strong>Appeals</strong><br />
A provider, a patient, a patient’s family or representative,<br />
or a hospital may request an urgent/expedited appeal<br />
when the denial of coverage involves:<br />
Cases involving continued or extended healthcare<br />
services<br />
Requests for additional services for a patient<br />
undergoing a continuing course of treatment<br />
Cases in which the member’s physician or healthcare<br />
provider believes an immediate appeal is warranted<br />
An expedited appeal must be filed within 180 calendar<br />
days of the initial unfavorable decision. <strong>Appeals</strong> filed<br />
after that date will not be considered, and you will<br />
receive a letter stating that the opportunity to file an<br />
appeal has been exhausted.<br />
Expedited appeals will be responded to within 72 hours<br />
of Empire’s receipt of the necessary information.<br />
page 29