5 - Complaints, Grievances & Appeals
5 - Complaints, Grievances & Appeals
5 - Complaints, Grievances & Appeals
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
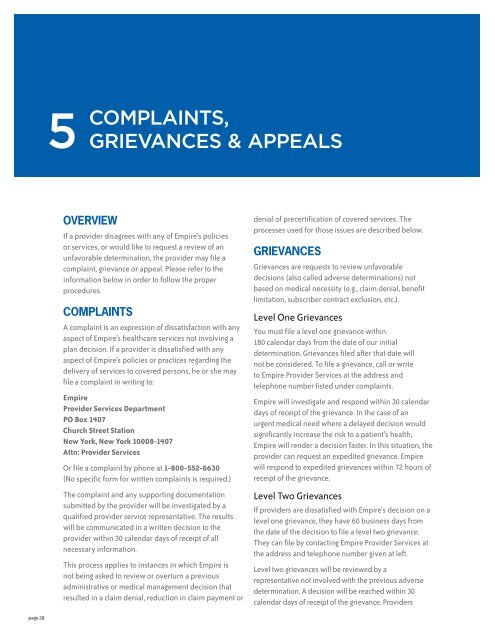
5<br />
COMPLAINTS,<br />
GRIEVANCES & APPEALS<br />
OVERVIEW<br />
If a provider disagrees with any of Empire’s policies<br />
or services, or would like to request a review of an<br />
unfavorable determination, the provider may file a<br />
complaint, grievance or appeal. Please refer to the<br />
information below in order to follow the proper<br />
procedures.<br />
COMPLAINTS<br />
A complaint is an expression of dissatisfaction with any<br />
aspect of Empire’s healthcare services not involving a<br />
plan decision. If a provider is dissatisfied with any<br />
aspect of Empire’s policies or practices regarding the<br />
delivery of services to covered persons, he or she may<br />
file a complaint in writing to:<br />
Empire<br />
Provider Services Department<br />
PO Box 1407<br />
Church Street Station<br />
New York, New York 10008-1407<br />
Attn: Provider Services<br />
Or file a complaint by phone at 1-800-552-6630<br />
(No specific form for written complaints is required.)<br />
The complaint and any supporting documentation<br />
submitted by the provider will be investigated by a<br />
qualified provider service representative. The results<br />
will be communicated in a written decision to the<br />
provider within 30 calendar days of receipt of all<br />
necessary information.<br />
This process applies to instances in which Empire is<br />
not being asked to review or overturn a previous<br />
administrative or medical management decision that<br />
resulted in a claim denial, reduction in claim payment or<br />
denial of precertification of covered services. The<br />
processes used for those issues are described below.<br />
GRIEVANCES<br />
<strong>Grievances</strong> are requests to review unfavorable<br />
decisions (also called adverse determinations) not<br />
based on medical necessity (e.g., claim denial, benefit<br />
limitation, subscriber contract exclusion, etc.).<br />
Level One <strong>Grievances</strong><br />
You must file a level one grievance within<br />
180 calendar days from the date of our initial<br />
determination. <strong>Grievances</strong> filed after that date will<br />
not be considered. To file a grievance, call or write<br />
to Empire Provider Services at the address and<br />
telephone number listed under complaints.<br />
Empire will investigate and respond within 30 calendar<br />
days of receipt of the grievance. In the case of an<br />
urgent medical need where a delayed decision would<br />
significantly increase the risk to a patient’s health,<br />
Empire will render a decision faster. In this situation, the<br />
provider can request an expedited grievance. Empire<br />
will respond to expedited grievances within 72 hours of<br />
receipt of the grievance.<br />
Level Two <strong>Grievances</strong><br />
If providers are dissatisfied with Empire’s decision on a<br />
level one grievance, they have 60 business days from<br />
the date of the decision to file a level two grievance.<br />
They can file by contacting Empire Provider Services at<br />
the address and telephone number given at left.<br />
Level two grievances will be reviewed by a<br />
representative not involved with the previous adverse<br />
determination. A decision will be reached within 30<br />
calendar days of receipt of the grievance. Providers<br />
page 28
may also file expedited level two grievances. Empire<br />
will respond to them within 72 hours of receipt of the<br />
grievance.<br />
Below are time frames for Empire’s response to<br />
grievances.<br />
Standard<br />
Expedited<br />
Level One<br />
Within 30 calendar<br />
days from our<br />
receipt of the<br />
grievance.<br />
Within 72 hours<br />
from our receipt of<br />
the grievance<br />
RECONSIDERATIONS<br />
AND APPEALS<br />
If the Medical Management Department determines<br />
that an admission, extension of the hospital stay, or<br />
some other healthcare service is not medically<br />
necessary, you may request reconsideration (through<br />
the attending physician) or appeal the decision in the<br />
ways described in the following sections.<br />
Reconsiderations<br />
A request for reconsideration can be made by calling<br />
or writing to the Medical Management Department,<br />
the specific contact information for which will be<br />
listed on the denial letter. The hospital or the<br />
physician who recommended the admission, the<br />
extension of a stay, or other healthcare services can<br />
make the request for reconsideration. In addition,<br />
the request can be made only:<br />
If we deny service prior to or during a member’s<br />
medical service, and<br />
If the denial is based on issues of medical<br />
necessity, and<br />
If the decision occurred without our Medical Director<br />
discussing the hospitalization or other services with<br />
the physician who recommended them.<br />
Services that have already been provided<br />
are not subject to reconsideration.<br />
Level Two<br />
Within 30 calendar<br />
days from our<br />
receipt of the<br />
grievance.<br />
Within 72 hours<br />
from our receipt of<br />
the grievance<br />
A reconsideration may be filed within seven<br />
calendar days of our initial pre-service (prospective)<br />
determination by contacting the Case Management<br />
Department which rendered the initial denial of<br />
service.<br />
All reconsideration requests that are received<br />
beyond seven calendar days of the initial pre-service<br />
denial should be addressed to the <strong>Appeals</strong> Unit and<br />
will be processed as appeals.<br />
A request for reconsideration will be reviewed within<br />
one business day by the Medical Director who made the<br />
initial decision to deny the precertification or the<br />
extension of service. The review will include any<br />
additional information provided. If the Medical Director<br />
who made the initial decision is not available, another<br />
Medical Director may act in his or her place.<br />
If we uphold our prior decision, written notification will<br />
be provided. This notification will include the following:<br />
The reasons for the decision, including the clinical<br />
rationale<br />
Information on how to obtain a copy of the clinical<br />
review criteria used in making the decision<br />
Instructions on how to initiate an appeal<br />
What additional information, if any, must be<br />
provided to or obtained by us in order to make a<br />
decision on appeal<br />
<strong>Appeals</strong><br />
<strong>Appeals</strong> are requests to review and change unfavorable<br />
clinical decisions (also called adverse determinations)<br />
such as when an admission, the extension of a stay or<br />
some other healthcare service is determined not to be<br />
medically necessary.<br />
Expedited <strong>Appeals</strong><br />
A provider, a patient, a patient’s family or representative,<br />
or a hospital may request an urgent/expedited appeal<br />
when the denial of coverage involves:<br />
Cases involving continued or extended healthcare<br />
services<br />
Requests for additional services for a patient<br />
undergoing a continuing course of treatment<br />
Cases in which the member’s physician or healthcare<br />
provider believes an immediate appeal is warranted<br />
An expedited appeal must be filed within 180 calendar<br />
days of the initial unfavorable decision. <strong>Appeals</strong> filed<br />
after that date will not be considered, and you will<br />
receive a letter stating that the opportunity to file an<br />
appeal has been exhausted.<br />
Expedited appeals will be responded to within 72 hours<br />
of Empire’s receipt of the necessary information.<br />
page 29
For our Administrative Service Only (ASO) line of<br />
business, there are no further appeal options after<br />
an expedited appeal.<br />
For our fully insured lines of business, a level two<br />
pre-service or post-service appeal may be filed<br />
within 60 business days of a level one expedited<br />
denial. Any level two appeals completed after an<br />
expedited appeal will be responded to within<br />
60 calendar days.<br />
We will provide reasonable access to a Medical<br />
Director within one business day of receiving notice<br />
of the request for an expedited appeal.<br />
Pre-Service (Prospective) <strong>Appeals</strong><br />
A pre-service appeal is a request to review an<br />
unfavorable decision issued prior to or during a service.<br />
Empire offers two levels of pre-service appeals for<br />
providers:<br />
Level one pre-service appeals must be filed<br />
within 180 calendar days of the initial adverse<br />
determination. <strong>Appeals</strong> filed after that date will not<br />
be considered, and you will receive a letter stating<br />
that the opportunity to file an appeal has been<br />
exhausted. Level one pre-service appeals will be<br />
responded to within 15 calendar days of Empire’s<br />
receipt of the appeal request.<br />
Level two pre-service appeals must be filed<br />
within 60 business days of the level one appeal<br />
determination. <strong>Appeals</strong> filed after that date will<br />
not be considered, and you will receive a letter<br />
stating that the opportunity to appeal has been<br />
exhausted. Level two pre-service appeals will be<br />
responded to within 15 calendar days of Empire’s<br />
receipt of the appeal request.<br />
Post-Service (Retrospective) <strong>Appeals</strong><br />
A post-service appeal is a request to review an<br />
unfavorable decision issued after a service was<br />
rendered. Empire offers two levels of post-service<br />
appeals for providers:<br />
Level one post-service appeals must be filed<br />
within 180 calendar days of the initial adverse<br />
determination. <strong>Appeals</strong> filed after that date will not<br />
be considered, and you will receive a letter stating<br />
that the opportunity to appeal has been exhausted.<br />
Level one post-service appeals will be responded to<br />
within 30 calendar days of Empire’s receipt of the<br />
appeal request.<br />
Level two post-service appeals must be filed<br />
within 60 business days of the level one appeal<br />
determination. <strong>Appeals</strong> filed after that date will not<br />
be considered, and you will receive a letter stating<br />
that the opportunity to appeal has been exhausted.<br />
Level two post-service appeals will be responded to<br />
within 30 calendar days of Empire’s receipt of the<br />
appeal request.<br />
Below are appeal time frames for fully insured and ASO<br />
lines of business:<br />
Standard<br />
Expedited<br />
Level One<br />
Pre-Service<br />
Within 15 calendar<br />
days from the<br />
receipt of the<br />
appeal request.<br />
Post-Service<br />
Within 30 calendar<br />
days from the<br />
receipt of the<br />
appeal request.<br />
Within 72 hours<br />
from the receipt of<br />
the appeal request.<br />
APPEAL REVIEW PROCESS<br />
Level Two<br />
Your appeal should be accompanied by a letter stating<br />
why the decision is being appealed and why you feel<br />
the decision should be overturned. Also include the<br />
information necessary to review it, such as the<br />
medical record.<br />
All appeals are reviewed by a qualified medical<br />
professional, with the same or similar specialty<br />
as the practitioner rendering the care and who<br />
was not involved with the initial determination.<br />
Pre-Service<br />
Within 15 calendar<br />
days from the<br />
receipt of the<br />
appeal request.<br />
Post-Service<br />
Within 30 calendar<br />
days from the<br />
receipt of the<br />
appeal request.<br />
N/A for ASO<br />
accounts. Within<br />
60 calendar days<br />
for fully insured<br />
accounts.<br />
If sufficient documentation to support the reasons for<br />
the appeal is not provided, Empire <strong>Appeals</strong> Department<br />
will attempt to request additional documentation or<br />
medical records.<br />
page 30
Appeal Communication<br />
If we make a decision favorable to the person filing the<br />
appeal, written notification is sent stating that the denial<br />
decision has been reversed. On the other hand, if we<br />
make a decision that is not favorable, we will provide<br />
written notification that will include the clinical<br />
rationale upon which the appeal determination is<br />
based. The letter will also contain information and rights<br />
regarding any further appeals.<br />
Expedited and pre-service appeal outcomes are also<br />
telephonically relayed to the person filing the appeal.<br />
External <strong>Appeals</strong><br />
Based on New York State Department of Insurance<br />
regulations, if services were denied based on medical<br />
necessity or a determination that they are experimental<br />
or investigational, subsequent to an appeal you may<br />
have the right to an external review. You can initiate an<br />
external review using the form Empire will send you<br />
when our final adverse determination is made. Please<br />
note: providers may request external review only when<br />
representing a member on pre-service (prospective)<br />
appeal or themselves on a post-service (retrospective)<br />
appeal.<br />
BEHAVIORAL HEALTHCARE<br />
APPEALS<br />
To request an appeal of an initial behavioral<br />
healthcare medical management decision (level one<br />
determination) rendered by Magellan, please submit<br />
your request in writing to:<br />
<strong>Appeals</strong> Department<br />
Magellan Behavioral Health<br />
199 Pomeroy Road<br />
Parsippany, NJ 07054<br />
Should a member not be satisfied with the level one<br />
determination, please follow the procedure outlined in<br />
the level-one determination letter.<br />
Send behavioral health related complaints or<br />
grievances not relating to Medical Management<br />
Department appeals to:<br />
<strong>Complaints</strong><br />
Magellan Behavioral Health<br />
199 Pomeroy Road<br />
Parsippany, NJ 07054<br />
Or call 1-800-626-3643<br />
For all other behavioral health vendors, please follow<br />
the instructions on the notice of adverse determination.<br />
For information regarding all claims, or claim disputes,<br />
call Empire Provider Services at 1-800-992-BLUE<br />
(1-800-992-2583), Monday – Friday, 8:30 a.m. – 5:00 p.m.<br />
OUR ADDITIONAL<br />
RESPONSIBILITIES<br />
In addition to the previously stated responsibilities,<br />
we will also:<br />
Protect the confidentiality of all parties involved in<br />
the complaint and appeals process<br />
Allow a member to appoint a representative to act on<br />
his/her behalf at any point during the grievance and<br />
appeals process<br />
Include information regarding the next available<br />
level of appeal into all adverse responses to appeals<br />
page 31