LEICESTER, LEICESTERSHIRE AND RUTLAND PCT ... - NHS
LEICESTER, LEICESTERSHIRE AND RUTLAND PCT ... - NHS
LEICESTER, LEICESTERSHIRE AND RUTLAND PCT ... - NHS
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Paper PLLR <strong>PCT</strong> Cluster Integrated Board meeting8 September 2011<strong>LEICESTER</strong>, <strong>LEICESTER</strong>SHIRE <strong>AND</strong> RUTL<strong>AND</strong> <strong>PCT</strong> CLUSTERINTEGRATED BOARD MEETINGFront SheetTitle of the report:Report to:Section:QIPP Progress ReportLeicester, Leicestershire and Rutland <strong>PCT</strong> ClusterIntegrated Board MeetingPublicDate of the meeting: 8 September 2011Report by:Sponsoring Director:Presented by:Ket Chudasama, Associate Director, Planning andDeliverySue Bishop, Director of FinanceSue Bishop, Director of FinanceReport supports the following corporate objective(s) 2011 – 2012:Handing over a good legacy √ Deliver the six identified transitionalstrands of workManage Providers’ performance againstupdated health goals and identifiedhealth inequalitiesDeliver agreed performance targetsagainst the six identified transformationwork streamsEXECUTIVE SUMMARY:Develop and maintain an energeticstakeholder engagement programmethroughout the transition1. The paper outlines the progress made on the five QIPP priority workstreamsRECOMMENDATIONS:The Trust Board is requested to:NOTE the progress made for the five QIPP priority work streams to date.1
Paper PLLR <strong>PCT</strong> Cluster Integrated Board Meeting8 September 2011<strong>NHS</strong> <strong>LEICESTER</strong>, <strong>LEICESTER</strong>SHIRE COUNTY & RUTL<strong>AND</strong> CLUSTERINTEGRATED BOARD MEETING8 SEPTEMBER 2011QUALITY INNOVATION PRODUCTIVITY & PREVENTION PROGRAMME 2011/12PROGRESS REPORTIntroduction1 The purpose of this paper is to provide an update on the progress of the fiveQIPP priority work streams against agreed plans following the last report tothe Trust Board in May 2011. Where known financial implications and savingspotential/avoided costs of the work streams have been included.Governance2 The benefit delivery of the five key work streams is reported to the Trust Boardon a quarterly basis.3 Progress of all QIPP schemes is monitored on a monthly basis by the DeliveryGroup. The scope of the Delivery Group also includes: productivity andsavings schemes, Transformation fund proposals, contract performance,workforce and SOP developments. The Delivery Group is chaired by theDirector of Finance and reports to the Performance Transition ManagementTeam.4 The Delivery Group will co-ordinate the 2012/13 QIPP plans throughengagement with the CCG’s.LLR Formulary and Prescribing Incentive Schemes5 The budgetary responsibility for prescribing has been devolved to the CCG’sand the LLR Formulary project has been combined with Prescribing IncentiveSchemes (PIS) to encourage practices to concentrate their actions upon theactivities that will deliver the greatest savings and improvements in quality.6 £5.306m has been removed from CCG prescribing operational budgets andperformance against this position is £649.3k under spent as at month 4 asshown in the table below.Consortium and PracticePrescribingYTD as at M4Budget (£) Spend (£) Variance (£)City 17,318,586 17,318,586 0ELR 15,383,537 14,965,137 (418,400)West 17,567,596 17,336,676 (230,920)Total 50,269,719 49,620,399 (649,320)1
Paper PLLR <strong>PCT</strong> Cluster Integrated Board Meeting8 September 20117 LLR Formulary adherence is included as a CQUIN for UHL and is reportedquarterly at the Clinical Quality Review Group and CCG performance isreported monthly at the Delivery Group.8 Delivery of LLR Formulary adherence savings will be further supported by theimplementation of the successful Transformation Fund proposals, which aimto embed the formulary into GP clinical systems at the point of prescribing andprovide real time prescribing information.9 All CCG Boards have agreed to implement an incentive scheme and practicesare implementing their individual practice plans with support from the CCGmedicines management teams. A performance monitoring framework is beingdeveloped to monitor the impact of individual schemes.10 Although the reduced medicines management team resource will placegreater reliance upon practices to deliver savings, CCG’s are to commissionsome additional support.11 The planned savings for this work stream are £5.306m and confidence ofachievement is high.Maternity12 This work stream relates to the pricing and coding of non-elective obstetricadmissions unrelated to birth.13 A contractual price adjustment has been agreed with UHL, the preliminarywork on best practice from other areas has been undertaken and aretrospective coding exercise has been started to code the last six monthsactivity in line with new HRG codes.14 The contractual agreement has ensured that the cost pressure of £4.6m inrespect of vanilla tariff payment for non-elective obstetric admissions has beenavoided in full.Paediatrics (Non elective care pathway)15 A local price for Children’s Assessment Unit (CAU) and the Short StayPaediatric Assessment Unit (SSPAU) has been contractually embedded withinthe UHL contract. Assuming activity levels remain the same this will achieve a£2.5m price productivity gain, or in essence cost avoidance.16 An integrated rapid assessment and follow up outreach service will beimplemented with non recurrent funding of £642, 707 approved throughTransformation Funds. This will fund additional consultants and nursepractitioners at the single front door access point and will ensure earlier seniorclinical decision making, thereby reducing unnecessary admissions to theSSPAU.Frail Older People (FOP)17 A Frail Older People (FOP) Implementation Board has been established andwill meet in September and will be chaired by GP lead, Dr Nitin Joshi.2
Paper PLLR <strong>PCT</strong> Cluster Integrated Board Meeting8 September 201118 The FOP Project Initiation Document (PID) has received widespread supportand final amendments are being made following further GP engagement.19 Implementation of the Geriatric outreach clinics and assessments hascommenced in county community hospitals20 An interim project manager has been brought in to work across a whole rangeof stakeholders involved in re-ablement, including acute trusts, LPT, localauthority, voluntary sector; in order to agree options and preferences forinvestment of ring fenced re-ablement monies. This exercise is estimated tobe completed by mid Sep 2011.21 In terms of Intermediate Care (a now identified related programme) targetsand work streams have been set for County re: integrated health and socialcare vision, including shared re-ablement plans; communication of city bedavailability to GPs; re-ablement data analysed and priorities agreed for all 3Local Authority areas; specification for Intermediate Care bed requirementsconsulted on and confirmed; project plan for procurement of IC beds outlinedand approved by Competition and Procurement Committee.22 Transformation funds that impact upon the FOP programme have beenapproved by the Cluster Board in July 2011 for Interface Geriatrics (£1.014m),Liaison Psychiatry (£356k) and Integration of the single point of access(£207k). Confirmation of delivery plans and evidence of early implementationagainst key milestones has been requested by 27 August 2011 and paymentof 33% of the transformation funds will be made subject to Delivery Groupapproval in September 2011.Right Care23 The Right Care Programme consists of four key areas of work. These aretreatments of limited value, reduction in follow-up ratios, undertaking surgicalprocedures in the lowest cost setting and reductions in clinical variation.24 The first three streams totalling £2.091m has been approved at the JointConfidential section of the Board in March 2011 and the methodology forreductions in clinical variation totalling £2.0m has been initially discussed atthe Commissioning Collaborative Board in May 2011 and activity targets havesubsequently been agreed with CCG’s.25 The Right Care Steering Group has been established as a sub group of theUHL Contract Performance Meeting (UHL CPM). The UHL CPM will monitorprogress and hold the provider to account for delivery and for release ofagreed transformational funding to support the change.26 Referral thresholds have been implemented from 1 June 2011 and are beingoverseen on a monthly basis by the Right Care Steering Group. The tablebelow displays the performance to date but it is important to note that therewill be a time lag for implementation to become apparent and activity reported(apr –jun) will be for those already booked in the system before the projectwent ‘live’.3
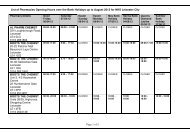
Right Care ProceduresYTDActualsYTDTargetFOTActualPaper PLLR <strong>PCT</strong> Cluster Integrated Board Meeting8 September 2011AnnualTargetYear toDate RunRateClinical Commissioning GroupYTD TargetTargetthe YearLeicester, Leicestershire and Rutland 2,847 2,586 262 11,388 10,342 10.1% 949 833Leicester City 828 783 45 3,312 3,131 5.8% 276 256Crescent 897 865 32 3,588 3,460 3.7% 299 285West Leicestershire 1,122 938 184 4,488 3,751 19.6% 374 292Right Care ProceduresYTDActualsYTDTargetPositionagainstPositionagainstFOTActualAnnualTargetPositionagainstAnnualPositionagainstAnnualYear toDate RunRateRequired RunRate ForRemainder ofRequired RunRate ForRemainder ofClusterYTD TargetTargetthe YearLeicester, Leicestershire and Rutland 2,847 2,586 262 11,388 10,342 10.1% 949 833Hernia Surgery 436 313 124 1,744 1,250 39.5% 145 90Septoplasty 77 72 5 308 287 7.3% 26 23Tonsillectomy 223 166 57 892 663 34.5% 74 49Cataract 1,387 1,281 106 5,548 5,123 8.3% 462 415Carpal Tunnel 234 216 18 936 865 8.2% 78 70MSK Hips 214 278 -64 856 1,113 (23.1%) 71 100MSK Knees 276 260 16 1,104 1,041 6.1% 92 8527 The Right Care Plans developed by UHL to address the in year changes toachieve a reduction in new to follow up rates and the shift in care to as lowercost setting as possible were presented at a confirm and challenge session onTuesday the 16th of August led by Dr. Dave Briggs and Dr Simon Freeman.28 Assurance was sought at the meeting about several areas, including the levelof clinical sign up to the plans, the confidence within the organisation thatthese were deliverable. Further work was requested between commissionerand provider to develop the plans for addressing multiple same day outpatientattendances.29 Recommendations about specific additions to the plans in terms of identifyingappropriate clinical leads and the setting of clear milestones for delivery wererequested. On completion of this it was then recommended that the RightCare plans be approved and the first instalment of 33% of the £3.7milliontransformation funds be paid following the CPM on 23 August 2011.30 A Clinical Variation (planned care) performance monitoring schedule has beendeveloped to allow monitoring of activity reductions at CCG level. This isdiscussed at the Delivery Group and fed into the relevant contractmanagement leads.4
New OP Attendances by Practice (Activity)YTDActualsYTDTargetPaper PLLR <strong>PCT</strong> Cluster Integrated Board Meeting8 September 2011AnnualTargetYear toDate RunRateClinical Commissioning GroupYTD Target FOT ActualTargetthe YearLeicester, Leicestershire and Rutland 64,240 63,287 953 256,960 253,147 1.5% 21,413 20,990Leicester City 20,449 21,114 -665 81,796 84,457 (3.2%) 6816 7112Crescent 20,222 19,611 611 80,888 78,445 3.1% 6741 6469West Leicestershire 23,569 22,561 1,008 94,276 90,244 4.5% 7856 7408New OP Attendances by Practice (Finance £'s)YTDActualsYTDTargetPositionagainstPositionagainstAnnualTargetPositionagainstAnnualPositionagainstAnnualYear toDate RunRateRequired RunRate ForRemainder ofRequired RunRate ForRemainder ofClinical Commissioning GroupYTD Target FOT ActualTargetthe YearLeicester, Leicestershire and Rutland 9,611,214 9,643,066 -31,853 38,444,854 38,572,265 (0.3%) 3,203,738 3,217,895Leicester City 3,300,664 3,230,497 70,167 13,202,656 12,921,987 2.2% 1,100,221 1,069,036Crescent 3,038,978 3,000,530 38,448 12,155,910 12,002,119 1.3% 1,012,993 995,905West Leicestershire 3,271,572 3,412,040 -140,468 13,086,288 13,648,158 (4.1%) 1,090,524 1,152,954Emergency Care31 A Clinical Variation (emergency care) performance monitoring schedule hasbeen developed to allow monitoring of activity reductions at CCG level. This isdiscussed at the Delivery Group and fed into the relevant contractmanagement leads.Emergency Spells by PracticeYTDActualsYTDTargetAnnualTargetYear toDate RunRateClinical Commissioning GroupYTD Target FOT ActualTargetthe YearLeicester, Leicestershire and Rutland 13,467 13,160 307 53,868 52,642 2.3% 4,489 4,353Leicester City 4,696 4,494 202 18,784 17,975 4.5% 1565 1475Crescent 4,888 4,811 77 19,552 19,244 1.6% 1629 1595West Leicestershire 3,883 3,856 27 15,532 15,422 0.7% 1294 1282Emergency Spells by Practice (Finance £'s)YTDActualsYTDTargetPositionagainstPositionagainstAnnualTargetPositionagainstAnnualPositionagainstAnnualYear toDate RunRateRequired RunRate ForRemainder ofRequired RunRate ForRemainder ofClinical Commissioning GroupYTD Target FOT ActualTargetthe YearLeicester, Leicestershire and Rutland 17,755,255 15,693,357 2,061,899 71,021,022 62,773,428 13.1% 5,918,418 5,002,019Leicester City 5,182,424 4,736,517 445,907 20,729,695 18,946,068 9.4% 1,727,475 1,529,294Crescent 7,869,606 6,937,445 932,161 31,478,425 27,749,779 13.4% 2,623,202 2,208,908West Leicestershire 4,703,226 4,019,395 683,830 18,812,902 16,077,581 17.0% 1,567,742 1,263,81732 The Emergency Care work stream has a number of sub-streams each ofwhich provides a progress report to the Emergency Care Network. The currentstatus of these areas is as follows :Clinicians Delivering Change (CDC)33 The CDC has now migrated to the Clinical Interface Group (CIG) and will bemeeting on 1 September 2011. This group comprises of the 3 urgent careleads from each commissioning consortia, UHL and LPT clinicians. Partneragencies, such as EMAS, CHS and the local authority would also need to beinvolved.34 The CIG will primarily be responsible for the development and delivery ofclinical pathways in relation to:1. The principles of Right Care, Right Place, Right Time5
Paper PLLR <strong>PCT</strong> Cluster Integrated Board Meeting8 September 2011a. The physical footprint of ED and UCCb. ED-UCC interface including clinical investigations and commonIT systemsc. ED patient processingd. ED/admission unit/base wards interfacee. ED and Hospital flow to patient discharge working with separategroup looking at discharge2. Children’s Unscheduled Care3. Emergency access to mental health services4. Provision of ambulatory care - chronic disease and frequent attenders(COPD, Diabetes, CVD, etc)35 The group will:o Support the development of high quality clinical pathways byfacilitating negotiations between clinicians across both primary andsecondary care, as well as those of partner organisationso Facilitate the production of project specific plans, with clearobjectives for delivery in 2011 (giving monthly reports)e.g.• ED footprint• UCC footprint• Clinician working• Patient processing36 The footprint change to the Majors and Resuscitation areas has been agreedand has resulted in a positive increase in terms of space and capacity. Themodel will have a single front door for all ambulatory patients, a triage areaand will stream patients into Minors, Urgent Care Centre, EmergencyDecisions Unit, Elderly Frail Unit, Majors or discharge home.37 The footprint has been agreed by clinical work force across specialties and willimpact other areas but will result in overall benefits to patient flow.Transformation funding of £11.235m has been approved by the Cluster Boardin July 2011 and the work will be staged over two financial years to limitoperational risks during peak periods and to allow time for procurement rulesto be followed.38 In terms of workforce, the following substantive staff have commenced in post:• 2 x substantive ED consultants• 2 x locum ED consultants• 5 x advanced ED practitioners• 3 x physicians assistants• 6 x HCA's• Nursing increased from 19 per shift to 21 per shift• AMU 6-10pm cover mainstreamed• EFU team – 2 x Acute physicians• 2 x lean officers (MAU)6
Paper PLLR <strong>PCT</strong> Cluster Integrated Board Meeting8 September 201139 The bed bureau pilot concluded in May 2011 but the pathway will continue asresults indicate a 33% and 47% drop in admissions in the medical andsurgical pilots as well as an increase in quality of services provided. However,the negative impact on EMAS should be noted; increase in overall call cycle,far longer handover delays leading to 1 x crew off the road to man the EDambulance doors to accept handovers. Following on from this, patients are nolonger going through ED. This will ultimately be resolved as part of the EDfootprint redesign.Senior Operational Group (SOG)40 UHL have achieved the number of people discharged by 1pm following anemergency from 13% to 20% on all acute medical wards by July 2011 withfuture targets of 25% by 30 September 2011 and 30% by 30 November 2011.41 All community hospitals have signed up to discharge by midday. In theCounty, all community hospitals except two are achieving 40% of discharge bymidday.42 Part-time project resource appointed by UHL to lead on UHL components hashad the secondment extended to November 2011 to reflect commitment toembedding successful processes.Intermediate care43 The procurement process is at invitation to tender stage (ITT) and remains ontrack to deliver awarding of contract in November 2011.General Updates44 A 12 month contract extension has been approved by the Competition andProcurement Committee in July 2011 for Interim hosting arrangements of theUrgent Care Centre (UCC). This will allow essential redesign work to becompleted.45 Agreement that work regarding access to emergency mental health pathwayswill be led by LPT. Objectives and outcome measures to be defined.46 A re-launch of the ‘red phone’ system is to take place as soon as the coverageissues are resolved and costings will be discussed at ECN in September2011.47 Draft winter checklist has been submitted to the SHA and we are awaitingSHA feedback. A final version will be returned to the SHA by 30 September2011 and will include an updated winter plan, escalation plan and wintercontact details.48 The Care Homes Summit event took place in July 2011 and a further sessionis planned for end of August 2011. The Care Homes Advisory Group hasagreed an action plan and is working on a falls pathway with UHL and EMAS.Conclusions7
Paper PLLR <strong>PCT</strong> Cluster Integrated Board Meeting8 September 201149 Strong progress has been made across the work streams, particularly withregards to contractually embedding the financial terms and benefits i.e.paediatrics local pricing and Right Care activity reductions made to UHLcontract.50 Significant progress is required by the next reporting period to confirm that theimplementation of each work stream is delivering the planned savings andimprovements in quality.Recommendations51 The Trust Board is requested to:- Note the progress made for the five QIPP priority work streams todate8