Iowa Medicaid Enterprise UB-04 Claim Form Health Insurance ...
Iowa Medicaid Enterprise UB-04 Claim Form Health Insurance ...
Iowa Medicaid Enterprise UB-04 Claim Form Health Insurance ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
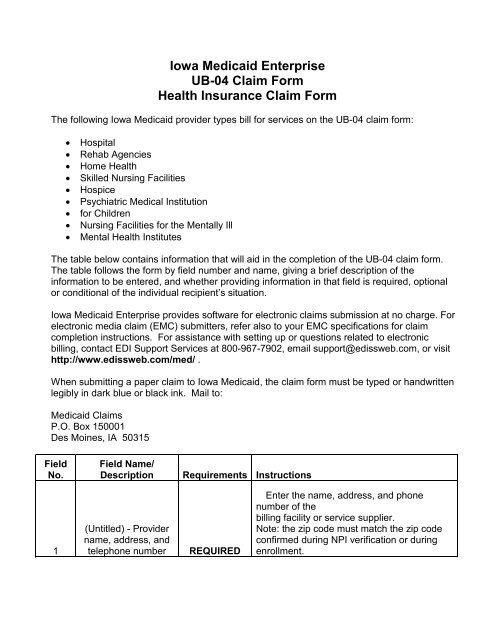
<strong>Iowa</strong> <strong>Medicaid</strong> <strong>Enterprise</strong><strong>UB</strong>-<strong>04</strong> <strong>Claim</strong> <strong>Form</strong><strong>Health</strong> <strong>Insurance</strong> <strong>Claim</strong> <strong>Form</strong>The following <strong>Iowa</strong> <strong>Medicaid</strong> provider types bill for services on the <strong>UB</strong>-<strong>04</strong> claim form:• Hospital• Rehab Agencies• Home <strong>Health</strong>• Skilled Nursing Facilities• Hospice• Psychiatric Medical Institution• for Children• Nursing Facilities for the Mentally Ill• Mental <strong>Health</strong> InstitutesThe table below contains information that will aid in the completion of the <strong>UB</strong>-<strong>04</strong> claim form.The table follows the form by field number and name, giving a brief description of theinformation to be entered, and whether providing information in that field is required, optionalor conditional of the individual recipient’s situation.<strong>Iowa</strong> <strong>Medicaid</strong> <strong>Enterprise</strong> provides software for electronic claims submission at no charge. Forelectronic media claim (EMC) submitters, refer also to your EMC specifications for claimcompletion instructions. For assistance with setting up or questions related to electronicbilling, contact EDI Support Services at 800-967-7902, email support@edissweb.com, or visithttp://www.edissweb.com/med/ .When submitting a paper claim to <strong>Iowa</strong> <strong>Medicaid</strong>, the claim form must be typed or handwrittenlegibly in dark blue or black ink. Mail to:<strong>Medicaid</strong> <strong>Claim</strong>sP.O. Box 150001Des Moines, IA 50315FieldNo.Field Name/DescriptionRequirements Instructions1(Untitled) - Providername, address, andtelephone numberREQUIREDEnter the name, address, and phonenumber of thebilling facility or service supplier.Note: the zip code must match the zip codeconfirmed during NPI verification or duringenrollment.
2(Untitled) - Pay-toname, address, andSecondaryIdentification FieldsSITUATIONALREQUIRED if Pay-to name and addressinformation is different than Billing Providerinformation in field 1.3aPatient ControlNumberOPTIONALEnter the account number assigned to thepatient by the provider of service. This field islimited to 20 alpha/numeric characters andwill be reflected on the remittance advicestatement as “Medical Record Number.”3bMedical RecordNumberOPTIONALEnter the number assigned to the patient’smedical/health record by the provider. Thisfield is limited to 20 alpha/numeric charactersand will be reflected on the remittance advicestatement as “Medical Record Number” onlyif the field 3a is blank.Enter a three-digit number consisting ofone digit from each of the followingcategories in this sequence:First digit Type of facilitySecond digit Bill classificationThird digit FrequencyType of Facility1 Hospital or psychiatric medical institutionforchildren (PMIC)2 Skilled nursing facility3 Home health agency7 Rehabilitation agency8 Hospice4 Type of Bill REQUIREDBill Classification1 Inpatient hospital, inpatient SNF orhospice
(non-hospital based)2 Hospice (hospital based)3 Outpatient hospital, outpatient SNF orhospice(hospital based)4 Hospital referenced laboratory services,home health agency, rehabilitation agencyFrequency1 Admit through discharge claim2 Interim – first claim3 Interim – continuing claim4 Interim – last claim5 Federal Tax Number OPTIONALNo entry required. NOTE: Changes to theTax ID must be reported through IMEProvider Services Unit at 1-800-338-7909 or515-256-4609 (in Des Moines).6Statement CoversPeriod(From-Through)REQUIRED7* Untitled - Not Used OPTIONALEnter the month, day, and year (MMDDYYformat) under both the From and Throughcategories for the period.No entry requiredNOTE: Covered and non-covered days arereported using value codes in fields 39a-41d.PATIENT NAME8a Last Name REQUIRED Enter the Last name of the patient8b First Name REQUIREDPATIENT ADDRESSEnter the first name and middle initial of thepatient9a Street Address OPTIONAL Enter the street address of the patient9b City OPTIONAL Enter the city for the patient’s address.9c State OPTIONAL Enter the state for the patient’s address.9d Zip Code OPTIONAL Enter the zip code for the patient’s address.9e OPTIONAL No entry required.10 Patient's Birth Date OPTIONALEnter the member's birth date as month, day,and year.
11 Sex REQUIRED12 Admission Date REQUIRED13 Admission Hour SITUATIONALEnter the patient’s sex: “M” for male or “F” forfemale.Enter in MMDDYY formatInpatient, PMIC, and SNF – Enter the date ofadmission for inpatient services.Outpatient – Enter the dates of service.Home <strong>Health</strong> Agency and Hospice – Enterthe date of admission for care.Rehabilitation Agency – No entry required.REQUIRED FOR INPATIENT/PMIC/SNF –Thefollowing chart consists of possible admissiontimes and a corresponding code. Enter thecodethat corresponds to the hour the patient wasadmitted for inpatient care.Code Time – AM Code Time - PM00 12:00 - 12:59 12 12:00 – 12:59NoonMidnight01 1:00 - 1:59 13 1:00 – 1:5902 2:00 - 2:59 14 2:00 – 2:5903 3:00 - 3:59 15 3:00 – 3:59<strong>04</strong> 4:00 - 4:59 16 4:00 – 4:5905 5:00 - 5:59 17 5:00 – 5:5906 6:00 - 6:59 18 6:00 – 6:5907 7:00 - 7:59 19 7:00 – 7:5908 8:00 - 8:59 20 8:00 – 8:5909 9:00 - 9:59 21 9:00 – 9:5910 10:00 - 10:59 22 10:00 – 10:5911 11:00 - 11:59 23 11:00 – 11:5999 Hour unknown
14Type ofAdmission/VisitSITUATIONALREQUIRED FOR INPATIENT/PMIC/SNF –Enter thecode corresponding to the priority level of thisinpatient admission.1 Emergency2 Urgent3 Elective4 Newborn9 Information unavailable15SRC (Source ofAdmission)SITUATIONALREQUIRED FOR INPATIENT/PMIC/SNF –Enter thecode that corresponds to the source of thisadmission.1 Non-health care facility point of origin2 Clinic or physician’s office4 Transfer from a hospital5 Born inside the Hospital6 Born outside of this hospital8 Court/law enforcement9 Information unavailableThe following chart consists of possibledischarge times and a corresponding code.Enter the code that corresponds to the hourpatient was discharged from inpatient care.16DHR (DischargeHour)SITUATIONALSee Field 13, Admission Hour, for instructionsfor accepted discharge hour codes.REQUIRED FOR INPATIENT/PMIC/SNF –Enter the code that corresponds to the statusof the patient at the end of service.01 Discharged to home or self care (routinedischarge)02 Discharged/transferred to other short-termgeneral hospital for inpatient care03 Discharged/transferred to a skilled nursingfacility (SNF)17STAT(Patient Status)SITUATIONAL<strong>04</strong> Discharged/transferred to an intermediatecare facility (ICF)
05 Discharged/transferred to another type ofinstitution for inpatient care or outpatientservices06 Discharged/transferred to home with careoforganized home health services07 Left care against medical advice orotherwisediscontinued own care08 Discharged/transferred to home with careofhome IV provider10 Discharged/transferred to mental healthcare11 Discharged/transferred to <strong>Medicaid</strong>certifiedrehabilitation unit12 Discharged/transferred to <strong>Medicaid</strong>certifiedsubstance abuse unit13 Discharged/transferred to <strong>Medicaid</strong>certifiedpsychiatric unit20 Expired30 Remains a patient or is expected to returnforoutpatient services (valid only for non-DRGclaims)40 Hospice patient died at home41 Hospice Patient died at hosp42 Hospice patient died unknown43 Discharge/transferred to Fed <strong>Health</strong>50 Hospice Home51 Hospice Medical Facility61 Transferred to Swingbed62 Transferred to Rehab Facility64 Transferred to Nursing Facility65 Disc Tran Psychiatric Hosp71 Trans for another Outpat Fac
72 Trans for Outpatient ServiceEnter corresponding codes to indicatewhether ornot treatment billed on this claim is related toanycondition listed below.Up to seven codes may be used to describetheconditions surrounding a patient’s treatment.General01 Military service related02 Condition is employment related here<strong>04</strong> HMO enrollee05 Lien has been filedInpatient Only80 Neonatal level II or III unit81 Physical rehabilitation unit82 Substance abuse unit83 Psychiatric unitX3 IFMC approved lower level of care, ICFX4 IFMC approved lower level of care, SNF91 Respite careOutpatient Only84 Cardiac rehabilitation program85 Eating disorder program86 Mental health program87 Substance abuse program88 Pain management program89 Diabetic education program90 Pulmonary rehabilitation program98 Pregnancy indicator – outpatient orrehabilitation agency18-28 Condition Codes SITUATIONALSpecial Program IndicatorA1 EPSDTA2 Physically handicapped children’sprogramA3 Special federal funding
A4 Family planningA5 DisabilityA6 Vaccine/Medicare 100% paymentA7 Induced abortion – danger to lifeA8 Induced abortion – victim rape/incestA9 Second opinion surgeryHome <strong>Health</strong> Agency (Medicare notapplicable)XA Condition stableXB Not homeboundXC Maintenance careXD No skilled service29 Accident State OPTIONAL No entry required30 Untitled OPTIONAL No entry required31-34 Occurrence Codesand DatesREQUIRED if any of the occurrences listedbelow are applicable to this claim, enter thecorresponding code and the month, day, andyear of that occurrence.Accident Related01 Auto accident02 No fault insurance involved, including autoaccident/other03 Accident/tort liability<strong>04</strong> Accident/employment related05 Other accident06 Crime victimSITUATIONAL<strong>Insurance</strong> Related17 Date outpatient occupational planestablishedor reviewed24 Date insurance denied25 Date benefits terminated by primary payer27 Date home health plan was established orlastreviewedA3 Medicare benefits exhausted
Other11 Date of onset35-36 Occurrence SpanCode and Dates OPTIONAL No entry required37 Untitled OPTIONAL No entry required.38 Untitled (Responsibleparty name andaddress)39-41 Value Codes andAmountsOPTIONALNo entry required.REQUIRED – Enter the value code, followedby the NUMBER of covered and/or noncovereddays that are included in the billingperiod. (NOTE: there should not be a dollaramount in this field).If more than one value code is shown for abilling period, codes are shown in ascendingnumeric sequence.42 Revenue CodeREQUIRED80 Covered days81 Non-Covered daysEnter the revenue code that corresponds toeach item or service billed.A list of valid revenue codes can be found atthe end of these <strong>UB</strong>-<strong>04</strong> claim forminstructions.REQUIREDNote:Not all listed revenue codes are payable by<strong>Medicaid</strong>.
43 Revenue Description43 Page ___ of ___Line2344 HCPCS/Rates/HIPPSRate CodesSITUATIONALSITUATIONALSITUATIONAL – Required if the providerenters a HCPCs “J-code” for a drug that hasbeen administered. Enter the National DrugCode (NDC) that corresponds to the J-codeentered in Field 44. The NDC must bepreceded with a “N4” qualifier. NDC shouldbe entered in NNNNN-NNNN-NN format. NOOTHER ENTRIES SHOULD BE MADE INTHIS FIELD.REQUIRED if claim is more than one page.Enter the page number and the total numberof pages for the claim.NOTE: The “PAGE ___ OF ___” andCREATION DATE on line 23 should bereported on all pages of the <strong>UB</strong>-<strong>04</strong>REQUIRED for Outpatient Hospital, InpatientSNF, and Home <strong>Health</strong> Agencies.Outpatient Hospital – Enter the HCPCS/CPTcode for each service billed, assigning aprocedure, ancillary or medical APG.Inpatient SNF – Enter the HCPCS codeW0511 for ventilator dependent patients,otherwise leave blank.Home <strong>Health</strong> Agencies – Enter theappropriate HCPCS code from the priorauthorization when billing for EPSDT relatedservices.All Others – Leave blank.DO NOT enter rates in this field.* When applicable, a procedure code modifiershould be displayed after the procedure code.SITUATIONAL45 Service Dates SITUATIONAL REQUIRED for Outpatient claims.
46 Service UnitsSITUATIONALOutpatient - Enter the service date foroutpatient service referenced in Field 42 orField 44. Note that one entry is required foreach date in which the service wasperformed.REQUIRED for Inpatient, Outpatient andHome <strong>Health</strong> Agencies.Inpatient – Enter the appropriate units ofservice for accommodation days.Outpatient – Enter the appropriate units ofservice provided per CPT/revenue code.(Batch-bill APGs require one unit = 15minutes of service time.)Home <strong>Health</strong> Agencies – Enter theappropriate units for each service billed. Aunit of service = a visit. Prior authorizationprivate-duty nursing/personal care –one unit = an hour.ALL units should be entered using wholenumbers only (1). Do not indicate partialunits (1.5) or anything after the decimal (1.0).47 Total ChargesEnter the total charges for each line billed.The total must include both dollars andREQUIRED cents.47 TotalsEnter the sum of the total charges for all linesbilled (all of 47).Line23 This field should be completed on the lastpage of the claim only.48 Non-CoveredCharges48 TotalsLine23REQUIREDREQUIREDREQUIREDThe total must include both dollars andcents.Enter the non-covered charges for eachapplicable line.***The total must include both dollars andcents.Enter the sum of the total non-coveredcharges for all lines billed (all of 48).
This field should be completed on the lastpage of the claim only.The total must include both dollars andcents.49 Untitled N/A Not Used50 A-C Payer Identification51 A-C*<strong>Health</strong> Plan ID52 A-C Release ofInformationCertification Indicator53 A-C Assignment ofBenefits CertificationIndicator54 A-C Prior PaymentsREQUIREDLEAVEBLANKOPTIONALOPTIONALEnter the designation provided by the state<strong>Medicaid</strong> agency. Enter the name of eachpayer organization from which you mightexpect some payment for the bill. Whenindicating <strong>Iowa</strong> <strong>Medicaid</strong> as a payer, enter“<strong>Medicaid</strong>”.This field must be left BLANK.Entering information in this field will cause theclaim to be returned.By submitting the claim, the provider hasagreed to all information on the back of theclaim form, including release of informationNo entry requiredREQUIRED if prior payments were made bya payer other than <strong>Medicaid</strong>. If applicable,enter the amount paid by a payer other than<strong>Medicaid</strong>.Do not enter previous <strong>Medicaid</strong> payments.The total must include both dollars andOPTIONAL cents.55 A-C Estimated AmountDue From Patient OPTIONAL No entry required56 * National Provider ID(NPI)REQUIRED57A *57B *57C *UntitledOtherProvider IDLEAVEBLANKEnter the NPI of the Billing entity.This field must be left BLANK. Enteringinformation in this field will cause the claim tobe returned.
58 Insured’s name59 Patient’s Relationshipto Insured60 A-C Insured’s unique IDREQUIREDOPTIONALEnter the last name, first name, and middleinitial of the <strong>Medicaid</strong> member on the line (A,B, or C) that corresponds to <strong>Medicaid</strong> fromField 50.No entry required.Required- Enter the member’s <strong>Medicaid</strong>identification number found on the MedicalAssistance Eligibility Card. It should consist ofseven digits followed by a letter, i.e.,1234567AEnter the <strong>Medicaid</strong> ID on the line (A, B, or C)REQUIRED that corresponds to <strong>Medicaid</strong> from Field 50.61 Group Name OPTIONAL No entry required62 A-C <strong>Insurance</strong> GroupNumber OPTIONAL No entry requiredEnter prior authorization number if applicable.63 TreatmentAuthorization CodeNOTE: This field is no longer used to reportthe MEDIPASS referral. Refer to Field 79 toenter the MEDIPASS referralSITUATIONAL Note: Lock-In moved to a Field 7864 Document ControlNumber (DCN OPTIONAL No entry required65 Employer nameOPTIONAL No entry required66 Diagnosis andProcedure codeQualifier (ICDVersion Indicator)67 Principal DiagnosisCodePresent onAdmission (POA)OPTIONALREQUIREDREQUIREDNo entry required. <strong>Medicaid</strong> only acceptsICD-9 codesEnter the ICD-9-CM code for the principaldiagnosis.POA indicator is the eighth digit of field 67 A-Q. POA indicates if a condition was presentor incubating at the time the order forinpatient admission occurs.Code Reason for CodeY Diagnosis was present at inpatientadmission.U Documentation insufficient to determine ifpresent at admission.
67 A-Q Other DiagnosisCodes68 Untitled69 Admitting Diagnosis70 A-C Patient’s Reason forVisitSITUATIONALOPTIONALSITUATIONALSITUATIONAL71 PPS (ProspectivePayment System)Code OPTIONAL No entry required.72 ECI (External Causeof Injury codesOPTIONAL No entry required.73 Untitled OPTIONAL No entry required.74 Principal ProcedureCode and Date74 A-E Other ProcedureCodes and DatesSITUATIONALSITUATIONAL75 Untitled OPTIONAL No entry required.76 *W Unable to clinically determine if present attimeof admission.(blank) Diagnosis is exempt from POAreporting.1 Invalid indicator – do not submit!REQUIRED if a diagnosis other than theprincipal is made. Enter the ICD-9-CM codesfor additional diagnosis.No entry required.REQUIRED for Inpatient hospital claims.Inpatient Hospital – The admitting diagnosisis required.REQUIRED if visit is unscheduled. Patient’sReason for Visit is required for all unscheduledoutpatient visits for outpatient bills.REQUIRED for the principal surgicalprocedure, enter the ICD-9-CM procedurecode and surgery date, when applicable.REQUIRED for additional surgicalprocedures, enter the ICD-9-CM procedurecodes and surgery dates.Attending Provider Name and IdentifiersNPIEnter the NPI of the attending physician.REQUIREDRequired when claim/encounter contains anyservices other than nonscheduledtransportation services.
77 *78 *79 *QualLastFirstLEAVEBLANKREQUIREDREQUIREDThe attending provider is the individual whohas overall responsibility for the patient’smedical care and treatment reported in thisclaim/ encounter.If not required, do not send.This field must be left BLANK. Enteringinformation in this field will cause the claim tobe returned.Enter the last name of the referring physician.Enter the first name of the referring physician.Operating Provider Name and IdentifiersNPIREQUIRED if the physician performing theprincipal procedure is different than theattending physician. Enter the NPI of theSITUATIONAL operating physician.QualThis field must be left BLANK. EnteringLEAVE information in this field will cause the claim toBLANK be returned.LastEnter the last name of the operatingSITUATIONAL physician.FirstEnter the first name of the operatingSITUATIONAL physician.Other Provider Name and IdentifiersNPIQualLastFirstSITUATIONALLEAVEBLANKSITUATIONALSITUATIONALOther Provider Name and IdentifiersREQUIRED if the patient is in the Lock-Inprogram. Enter the NPI of the member’sLock-In provider.This field must be left BLANK. Enteringinformation in this field will cause the claim tobe returned.Enter the last name of the member’s Lock-Inprovider.Enter the first name of the member’s Lock-Inprovider.
NPIQualLastFirst80 * RemarksSITUATIONALLEAVEBLANKSITUATIONALSITUATIONALREQUIRED if the patient is in the MediPASSprogram or if Non-MediPASS and claim isOutpatient- Enter the NPI of the referringphysician. This area should not be completedif the primary physician did not give thereferral.This field must be left BLANK. Enteringinformation in this field will cause the claim tobe returned.Enter the last name of the referringMediPASS physician.Enter the first name of the referringMediPASS physician.REQUIRED if a diagnosis other than theprincipal is made.SITUATIONAL When applicable enter one of the following:- “Not a Medicare Benefit”- “Resubmit” (and list the original filing date)81 * Code-Code Fields- Member is “Retro-Eligible and NOD isattached” (notice of decision).REQUIRED – Enter taxonomy codeassociated with the NPI of the billing entity(Field 56). Precede taxonomy code withqualifier “B3” (healthcare provider taxonomycode).REQUIREDNote: the taxonomy code must match thetaxonomy code confirmed during NPIverification or during enrollment.Updated 4/17/12
Revenue CodesBOX 42CODE DEFINED S<strong>UB</strong>GATEGORIES11XRoom & BoardPrivate(medical or general)12XRoom & BoardSemi-Private TwoBed(medical or general)13XRoom & BoardSemi-Private Threeand Four Beds(medical or general)14XPrivate(deluxe)15XRoom & BoardWard(medical or general)16XOther Room &BoardCharges for accommodationswith a single bed.Charges for accommodationswith two beds.Charges for accommodationswith three and four beds.Charges for accommodationswith amenities substantially inexcess of those provided toother patients.Charges for accommodationswith five or more beds.Charges for accommodationsthat cannot be included in thespecific revenue centercodes. Hospitals that are0 General classifications1 Medical/surgical/GYN2 OB3 Pediatric4 Psychiatric6 Detoxification7 Oncology8 Rehabilitation9 Other0 General classifications4 Sterile environment7 Self care9 Other0 General classifications4 Sterile environment7 Self care9 Other0 General classifications4 Sterile environment7 Self care9 Other0 General classifications4 Sterile environment7 Self care9 Other0 General classifications4 Sterile environment7 Self care
17XNursery18XLeave of Absence20XIntensive Care21XCoronary Care22XSpecial Charges23XIncremental NursingCharge Rateseparating this charge forbilling Sterile environment isto be usedCharges for nursing care fornewborn and prematureinfants in nurseries.Charges for holding aroom/bed for a patient whilethey are temporarily awayfrom the provider.Charges for medical orsurgical care provided topatients who require a moreintensive level of care than isrendered in the generalmedical or surgical unit.Charges for medical careprovided to patients withcoronary illnesses requiring amore intensive level of carethan is rendered in thegeneral medical care unit.Charges incurred during aninpatient stay or on a dailybasis for certain services.9 Other0 General classification1 Newborn2 Premature5 Neonatal ICU9 Other5 Nursing home (forhospitalization)0 General classification1 Surgical2 Medical3 Pediatric4 Psychiatric6 Post ICU7 Burn care8 Trauma9 Other intensive care0 General classification1 Myocardial infarction2 Pulmonary care3 Heart transplant4 Post CCU9 Other coronary care0 General classification1 Admission charge2 Technical support charge3 U.R. service charge4 Late discharge, medicallynecessary9 Other special charges0 General classification1 Nursery2 OB3 ICU4 CCU
24XAll InclusiveAncillary25XPharmacy26XIV Therapy27XMedical/SurgicalSupplies andDevices(also see 62X, anextension of 27X)28XOncologyA flat rate charge incurred oneither a daily or total staybasis for ancillary servicesonly.Charges for medicationproduced, manufactured,packaged, controlled,assayed, dispensed, anddistributed under direction oflicensed pharmacies.Equipment charge oradministration of intravenoussolution by specially trainedpersonnel to individualsrequiring such treatment.This code should be usedonly when a discrete serviceunit exists.Charges for supply itemsrequired for patient care.Charges for the treatment oftumors and related diseases.9 Other0 General classification9 Other inclusive ancillary0 General classification1 Generic drugs2 Nongeneric drugs3 Take home drugs4 Drugs incident to otherdiagnostic services5 Drugs incident to radiology6 Experimental drugs7 Nonprescription8 IV solutions9 Other pharmacy0 General classification1 Infusion pump2 IV therapy/pharmacy services3 IV therapy/drug/supply delivery4 IV therapy/supplies9 Other IV therapy0 General classification1 Nonsterile supply2 Sterile supply3 Take home supplies4 Prosthetic/orthotic devices5 Pacemaker6 Intraocular lens7 Oxygen – take home8 Other implants9 Other supplies/devices0 General classification9 Other oncology29X Charges for medical 0 General classification
Durable MedicalEquipment(other than renal)30XLaboratory31XLaboratoryPathological32XRadiologyDiagnostic33XRadiologyTherapeutic34XNuclear Medicineequipment that can withstandrepeated use (excluding renalequipment).Charges for the performanceof diagnostic and routineclinical laboratory tests. Foroutpatient services, be sureto indicate the code for eachlab charge in <strong>UB</strong>-<strong>04</strong> formfield number 44.Charges for diagnostic androutine laboratory tests ontissues and cultures. Foroutpatient services, indicatethe CPT code for each labcharge in <strong>UB</strong>-<strong>04</strong> form fieldnumber 44.Charges for diagnosticradiology services providedfor the examination and careof patients. Includes taking,processing, examining andinterpreting of radiographsand fluorographsCharges for therapeuticradiology services andchemotherapy required forcare and treatment ofpatients. Includes therapy byinjection or ingestion ofradioactive substances.Charges for procedures andtests performed by a1 Rental2 Purchase of new DME3 Purchase of used DME4 Supplies/drugs for DMEeffectiveness(home health agency only)9 Other equipment0 General classification1 Chemistry2 Immunology3 Renal patient (home)4 Nonroutine dialysis5 Hematology6 Bacteriology and microbiology9 Other laboratory0 General classification1 Cytology2 Histology4 Biopsy9 Other0 General classification1 Angiocardiography2 Arthrography3 Arteriography4 Chest x-ray9 Other0 General classification1 Chemotherapy – injected2 Chemotherapy – oral3 Radiation therapy5 Chemotherapy – IV9 Other0 General classification1 Diagnostic
35XCT Scan36XOperating RoomServices37XAnesthesia38XBlood39XBlood Storageand Processing40XOther ImagingServicesradioisotope laboratoryutilizing radioactive materialsas required for diagnosis andtreatment of patients.Charges for computedtomographic scans of thehead and other parts of thebody.Charges for servicesprovided to patient byspecifically trained nursingpersonnel who assistedphysicians in surgical/relatedprocedures during andimmediately followingsurgery.Charges for anesthesiaservices in the hospital.Charges for blood must beseparately identified forprivate payer purposes.Charges for the storage andprocessing of whole blood.2 Therapeutic9 Other0 General classification1 Head scan2 Body scan9 Other CT scans0 General classification1 Minor surgery2 Organ transplant – other thankidney7 Kidney transplant9 Other operating room services0 General classification1 Anesthesia incident toradiology2 Anesthesia incident to otherdiagnostic services4 Acupuncture9 Other anesthesia0 General classification1 Packed red cells2 Whole blood3 Plasma4 Platelets5 Leukocytes6 Other components7 Other derivatives(cryoprecipitates)9 Other blood0 General classification1 Blood administration9 Other blood storage andprocessing0 General classification1 Diagnostic mammography2 Ultrasound
41XRespiratoryServices42XPhysical Therapy43XOccupationalTherapy44XSpeechLanguagePathologyCharges for administration ofoxygen and certain potentdrugs through inhalation orpositive pressure and otherforms of rehabilitative therapythrough measurement ofinhaled and exhaled gasesand analysis of blood andevaluation of the patient’sability to exchange oxygenand other gases.Charges for therapeuticexercises, massage, andutilization of effectiveproperties of light, heat, cold,water, electricity, andassistive devices fordiagnosis and rehabilitationof patients who haveneuromuscular, orthopedic,and other disabilities.Charges for teaching manualskills and independence inpersonal care to stimulatemental and emotional activityon the part of patients.Charges for servicesprovided to those withimpaired functionalcommunication skills.3 Screening mammography4 Positron emission tomography9 Other imaging services0 General classification1 Inhalation services3 Hyperbaric oxygen therapy9 Other respiratory services0 General classification1 Visit charge2 Hourly charge3 Group rate4 Evaluation or reevaluation9 Other occupationaltherapy/trial occupational therapy –rehab agency0 General classification1 Visit charge2 Hourly charge3 Group rate4 Evaluation or reevaluation9 Other occupationaltherapy/trial occupational therapy –rehab agency0 General classification1 Visit charge2 Hourly charge3 Group rate4 Evaluation or reevaluation9 Other speech-languagepathology/trial speech therapy –rehab agency
45XEmergency Room46XPulmonary Function47XAudiology48XCardiology49XAmbulatorySurgical Care50XOutpatient Services51XClinic52XFree-StandingClinicCharges for emergencytreatment to ill and injuredrequiring immediateunscheduled medical/surgicalcare.Charges for tests measuringinhaled and exhaled gases,the analysis of blood and fortests evaluating the patient’sability to exchange oxygenand other gases.Charges for the detection andmanagement ofcommunication handicapscentering in whole or in parton the hearing function.Charges for cardiacprocedures rendered in aseparate unit within thehospital. Procedures include,but are not limited to: heartcatheterization, coronaryangiography, Swan-Ganzcatheterization, exercisestress tests.Charges for ambulatorysurgery not covered by othercategories.Outpatient charges forservices rendered to anoutpatient admitted as aninpatient before midnight ofthe day following the date ofservice.Clinic(nonemergency/scheduledoutpatient visit) charges forproviding diagnostic,preventive curative,rehabilitative, and educationservices on a scheduledbasis to ambulatory patients.0 General classification9 Other emergency room0 General classification9 Other pulmonary function0 General classification1 Diagnosis2 Treatment9 Other audiology0 General classification1 Cardiac cath lab2 Stress test9 Other cardiology0 General classification9 Other ambulatory surgical care0 General classification9 Other outpatient services0 General classification1 Chronic pain center2 Dental clinic3 Psychiatric clinic4 OB-GYN clinic5 Pediatric clinic9 Other clinic0 General classification1 Rural health – clinic
53XOsteopathicServices54XAmbulance55XSkilled Nursing(home health agencyonly)56XMedical SocialServices(home health agencyonly)57XHome <strong>Health</strong> AideCharges for a structuralevaluation of the cranium,entire cervical, dorsal andlumbar spine by a doctor ofosteopathy.Charges for ambulanceservice, usually on anunscheduled basis to the illand injured requiringimmediate medical attention.Ambulance is payable on the<strong>UB</strong>-<strong>04</strong> form only inconjunction with inpatientadmissions. Otherambulance charges must besubmitted on the ambulanceclaim form. Documentation ofmedical necessity must beprovided for ambulancetransport. The diagnosis/documentation must reflectthat the patient wasnonambulatory and the tripwas to the nearest adequatefacility.Charges for nursing servicesthat must be provided underthe direct supervision of alicensed nurse ensuring thesafety of the patient andachieving the medicallydesired result.Charges for servicesprovided to patients on anybasis, such as counseling,interviewing and interpretingsocial situations problems.Charges made by a homehealth agency for personnel2 Rural health – home3 Family practice9 Other free-standing clinic0 General classification1 Osteopathic therapy9 Other osteopathic services0 General classification1 Supplies2 Medical transport3 Heart mobile4 Oxygen5 Air ambulance6 Neonatal ambulance services7 Pharmacy8 Telephone transmission EKG9 Other ambulance0 General classification1 Visit charge2 Hourly charge9 Other skilled nursing0 General classification1 Visit charge2 Hourly charge9 Other medical social services0 General classification1 Visit charge
(home health agencyonly)61XMRI62XMedical/SurgicalSupplies(extension of 27X)63XDrugs RequiringSpecificIdentification64XHome IV TherapyServicesprimarily responsible for thepersonal care of the patientCharges for MagneticResonance Imaging of thebrain and other body parts.Charges for supply itemsrequired for patient care. Thecategory is an extension of27X for reporting additionalbreakdown where needed.Subcode 1 is for providersthat cannot bill supplies usedfor radiology proceduresunder radiology. Subcode 2is for providers that cannotbill supplies used for otherdiagnostic procedures.Charges for drugs andbiologicals requiring specificidentification as required bythe payer. IfHCPCS is used to describethe drug, enter theHCPCS code in <strong>UB</strong>-<strong>04</strong> formfield number 44.Charges for intravenous drugtherapy services performed inthe patient’s residence. Forhome IV providers theHCPCS code must beentered for all equipment andall types of covered therapy.2 Hourly charge9 Other home health aideservices0 General classification1 Brain (including brainstem)2 Spinal cord (including spine)9 Other MRI1 Supplies incident to radiology2 Supplies incident to otherdiagnostic services0 General classification1 Single source drug2 Multiple source drug3 Restrictive prescription4 Erythropoietin (EPO), less than10,000 units5 Erythropoietin (EPO), 10,000 ormore units6 Drugs requiring detailed coding0 General classification1 Nonroutine nursing, central line2 IV site care, central line3 IV site/change, peripheral line4 Nonroutine nursing, peripheralline
65XHospice Services(hospice only)70XCast Room71XRecovery Room72XLaborRoom/Delivery73XEKG/ECG(electro-cardiogram)74XEEGCharges for hospice careservices for a terminally illpatient they elects theseservices in lieu of otherservices for the terminalcondition.Charges for services relatedto the application,maintenance, and removal ofcasts.Charges for labor anddelivery room servicesprovided by specially trainednursing personnel to patients.This includes prenatal careduring labor, assistanceduring delivery, postnatalcare in the recovery room,and minor gynecologicprocedures if performed inthe delivery suite.Charges for the operation ofspecialized equipment torecord electromotivevariations in actions of theheart muscle on anelectrocardiography for thediagnosis of heart ailments.Charges for the operation ofspecialized equipment5 Training patient/caregiver,central line6 Training, disabled patient,central line7 Training, patient/caregiver,peripheral line8 Training, disabled patient,peripheral line9 Other IV therapy services1 Routine home care2 Continuous home care (hourly)5 Inpatient respite care6 General inpatient care8 Care in an ICF or SNF0 General classification9 Other cast room0 General classification9 Other recovery room0 General classification1 Labor2 Delivery3 Circumcision4 Birthing center9 Other labor room/delivery0 General classification1 Holter monitor2 Telemetry9 Other EKG/ECG0 General classification9 Other EEG
(electroencephalogram)75XGastro-IntestinalServices76XTreatment orObservation Room79XLithotripsy80XInpatient RenalDialysis81XOrgan Acquisition(see 89X)82XHemodialysismeasuring impulsefrequencies and differencesin electrical potential invarious brain areas to obtaindata used in diagnosing braindisorders.Procedure room charges forendoscopic procedures notperformed in the operatingroom.Charges for the use of atreatment room or the roomcharge associated withoutpatient observationservices. HCPCS codeW9220 must be used withthese codes on outpatientclaims.Charges for the use oflithotripsy in the treatment ofkidney stones.A waste removal processperformed in an inpatientsetting using an artificialkidney when the bodies ownkidneys have failed. Thewaste may be removeddirectly from the blood orindirectly from the blood byflushing a special solutionbetween the abdominalcovering and the tissue.The acquisition of a kidney,liver or heart for transplantuse. (All other human organsfall under category 89X.)A waste removal process,performed in an outpatient orhome setting, necessary0 General classification9 Other gastro-intestinal0 General classification1 Treatment room2 Observation room9 Other treatment/observationroom0 General classification9 Other lithotripsy0 General classification1 Inpatient hemodialysis2 Inpatient peritoneal(nonCAPD)3 Inpatient continuousambulatory peritoneal dialysis4 Inpatient continuous cyclingperitoneal dialysis (CCPD)9 Other inpatient dialysis0 General classification1 Living donor – kidney2 Cadaver donor – kidney3 Unknown donor – kidney4 Other kidney acquisition5 Cadaver donor – heart6 Other heart acquisition7 Donor – liver9 Other organ acquisition0 General classification1 Hemodialysis/composite orother rate
(Outpatient or home) when the body’s own kidneyshave failed. Waste isremoved directly from theblood.83XPeritoneal Dialysis(Outpatient or home)84XContinuousAmbulatoryPeritoneal Dialysis(CCPD)(Outpatient or home)85XContinuous CyclingPeritoneal Dialysis(CCPD)(Outpatient or home)88XMiscellaneousDialysis89XOther Donor Bank(extension of 81X)A waste removal process,performed in an outpatient orhome setting, necessarywhen the bodies own kidneyshave failed. Waste isremoved indirectly by flushinga special solution betweenthe abdominal covering andthe tissue.A continuous dialysis processperformed in an outpatient orhome setting using thepatient peritoneal membraneas a dialyzer.A continuous dialysis processperformed in an outpatient orhome setting using amachine to make automaticchanges at night.Charges for dialysis servicesnot identified elsewhere.Charges for the acquisition,storage, and preservation ofall human organs (excluding2 Home supplies3 Home equipment4 Maintenance/100%5 Support services9 Other outpatient hemodialysis0 General classification1 Peritoneal/composite or otherrate2 Home supplies3 Home equipment4 Maintenance/100%5 Support services9 Other outpatient peritonealdialysis0 General classification1 CAPD/composite or other rate2 Home supplies3 Home equipment4 Maintenance/100%5 Support services9 Other outpatient CAPD0 General classification1 CCPD/composite or other rate2 Home supplies3 Home equipment4 Maintenance/100%5 Support services9 Other outpatient CCPD0 General classification1 Ultrafiltration2 Home dialysis aid visit9 Miscellaneous dialysis other0 General classification1 Bone
92XOther DiagnosticServices94XOther TherapeuticServices99XPatientConvenience Itemskidneys, livers, and hearts –see 81X).Charges for other therapeuticservices not otherwisecategorized.Charges for items generallyconsidered by the third partypayers to be strictlyconvenience items, and,therefore, are not covered.2 Organ (other than kidney)3 Skin9 Other donor bank0 General classification1 Peripheral vascular lab2 Electromyelogram3 Pap smear4 Allergy test5 Pregnancy test9 Other diagnostic services0 General classification1 Recreational therapy2 Education/training3 Cardiac rehabilitation4 Drug rehabilitation5 Alcohol rehabilitation6 Complex medical equipment –routine7 Complex medical equipment –ancillary9 Other therapeutic services0 General classification1 Cafeteria/guest tray2 Private linen service3 Telephone/telegraph4 TV/radio5 Nonpatient room rentals6 Late discharge charge7 Admission kits8 Beauty shop/barber9 Other patient convenienceitems** If you have any questions about this information, please contact Provider Services at1-800-338-7909. Local in the Des Moines area at 515-256-4609.