ILIF Interlaminar Lumbar Instrumented Fusion
ILIF Interlaminar Lumbar Instrumented Fusion
ILIF Interlaminar Lumbar Instrumented Fusion
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
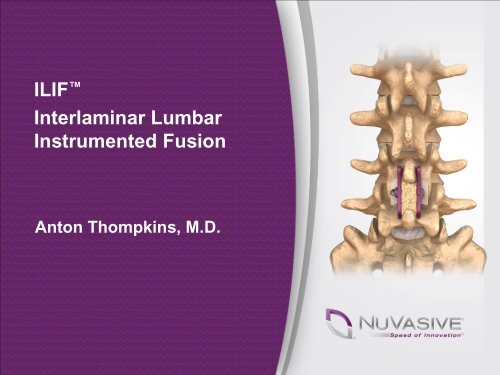
<strong>ILIF</strong> <strong>Interlaminar</strong> <strong>Lumbar</strong><strong>Instrumented</strong> <strong>Fusion</strong>Anton Thompkins, M.D.
Anton Thompkins, M.D.EDUCATION:BS, Biology, DePauw University, Greencastle, INMD, University of Cincinnati College ofMedicineRESIDENCY: Orthopedic Surgery, IndianaUniversity Medical Center, Indianapolis, INFELLOWSHIP: Spine, Panorama Orthopedics,Denver, COBOARD CERTIFICATION: American Board ofOrthopedic SurgeryMEMBERSHIPS: American Academy of OrthopedicSurgeons, J. Robert Gladden, Orthopedic Society,Indiana State Medical Association, Indiana OrthopedicSociety, Porter County Medical Society, SOLAS member,NASS member
Will <strong>ILIF</strong> Replace Pedicle ScrewInstrumentation/Procedures?
WHY REPLACE TRADITIONAL PROCEDURESWITH MAXIMUM ACCESS SURGERY?
Traditional Posterior <strong>Instrumented</strong> <strong>Fusion</strong>Bilateral pedicle screwsWide dissection totransverse processesSignificant bone removalPotential for increasedcomplicationsOften paired withinterbody implantsPedicle Screws
Potential <strong>Instrumented</strong> <strong>Fusion</strong>ComplicationsPotential destabilizationWide exposure may cause severeatrophy of paraspinal musclesIncreased OR time, blood loss, infections,dural tear, malpositioned implants,pseudarthrosis, reoperationAdjacent segment degenerationOlder patient population with likelycomorbiditiesCardiovascular diseaseLow respiratory reserveExercise intoleranceDiabetesOsteoporosis, etc.Pedicle Screws
Potential Improvements for<strong>Instrumented</strong> <strong>Fusion</strong>sSurgeons determined to:Reduce patient morbidityMinimize dissection and boney removalMinimize operative timeReduce complications with geriatric or comorbid patientsLimit surgery to midline if possible
Historical PerspectiveThe PastThe PresentThe FutureDr. Hibbs first spinalfusion in 1912; corticaltibial wedge betweenthe spinous processesCervical Gallie fusion withsublaminar wiring
<strong>ILIF</strong> Construct<strong>ILIF</strong> (<strong>Interlaminar</strong> <strong>Lumbar</strong> <strong>Instrumented</strong> <strong>Fusion</strong>)1. Improved DirectDecompression2. Posterior <strong>Fusion</strong>3. Posterior Fixation4. Biologics
WHO: IDEAL <strong>ILIF</strong> PATIENTIdeal <strong>ILIF</strong> Patient: Older Patient Suffering from <strong>Lumbar</strong>Spinal Stenosis with Mild to Moderate InstabilityThe total population over 60years-old worldwide will rise from605M in 2000 to 1.2B in 2025.<strong>Lumbar</strong> spinal stenosis (LSS) is themost common reason for backsurgery in patients over 50.“Spinal stenosis is the most common surgical indication for the geriatric patient.”SOURCE: Katz JN : <strong>Lumbar</strong> spinal fusion. Surgical rates, costs, and complications. Spine: 20; 78S-83S, 1995
WHERE TO USE <strong>ILIF</strong> ?• Elderly, low demand patient• Central, lateral recess, andforaminal stenosis• Instability is present, buttrying to avoid pedicle screws• Co-morbidities are present<strong>ILIF</strong> Midline IncisionTraditional Approach
WHEN NOT TO USE <strong>ILIF</strong>“If you’re a hammer, not every indication is a nail.”Severe osteoporosisIsthmic spondylolisthesis (pars defect)Spondylolisthesis with gross instability (>Grade 1)Previous laminectomy at operative level
WHY THE <strong>ILIF</strong> PROCEDUREAllow safe access to neural elements fordecompressionMinimal disruption to the soft tissueMaintain sagittal balance<strong>Fusion</strong> surface equal or better than currentstandardRobust fixation without burning any bridgesTime saving
<strong>ILIF</strong>/Affix in the Continuum of CareAffix® as an adjunct to interbody fusion: XLIF, TLIF, ALIFXLIF® + XLP® + AFFIX IIXLIF + <strong>ILIF</strong>Cortical Screws + <strong>ILIF</strong>TLIF + UNILATERAL DBR® II+ AFFIX IIALIF + Halo® Plate+ AFFIX II<strong>ILIF</strong> at L5-S1
Case StudiesPedicle Screw Replacement
Case Presentation # 1The 90% Patient Profile•Sex: Female•Age: 89 YO•Physical Complaints: Back and Leg Pain•Diagnosis: Stenosis - central, lateral recess, foraminal• Surgical Plan: <strong>ILIF</strong> L4-5 with decompression
Case Presentation # 1• Fixation: 35mm Affix® II• Spacer: 12mm Magnitude• EBL: 125cc
Case Presentation # 2The 5-10% Patient Profile• 58 y/o male• 2-year history of LBP• Bilateral anterior thigh pain andintermittent inguinal discomfort;LBP becoming more disabling• L2-3 spondylolisthesis withstenosis• Central, lateral recess• Comorbidities: exam non-focal• TREATMENT: L2-3 XLIF® with<strong>ILIF</strong>
The L5-S1 Patient Profile• Patient: 53 y/o male withan acute onset of left legand severe LBP. Pt s/pmicro 3 years prior• PE: Weakness with PF4/5, Achilles Reflex absentand 10/10 painCase Presentation # 3
Case Presentation # 3• Patient underwent an L5/S1 <strong>ILIF</strong> with the bladed plate• Leg pain had immediate resolution• Incision equal or smaller than previous microdiscectomy
Dr. Thompkins <strong>ILIF</strong> + TLIF Technique250+ cases with <strong>ILIF</strong>/TLIF approachAverage blood loss: 120ccAverage length of surgery: 1:25Average length of stay: 2.5 daysPreliminary VASRadicular – 75% reductionLBP – 60% reduction
Dr. Thompkins TLIF + <strong>ILIF</strong> TechniqueAdvantages-Increased fusion surface-Anterior columnsupport- Possible increasedfusion rates andconstruct rigidity-Possible decreasediscogenic back painDisadvantages-Increased operativetime-Increased cost-Minor increase bloodloss
Will/Should <strong>ILIF</strong> ReplacePedicle ScrewInstrumentation/Procedures?Yes- Augmentation foranterior support- Pt with significantcomorbitiesNO- Deformity case- Isthmic spondylolisthesis- Gross instability- Stenosis with mild tomoderate instability
In Summary . . . MINIMALLY INVASIVE IS : Less operative time Less blood loss Less postoperative pain Less post op medications Less hospital stay Rapid return to normalactivity Improved Quality of Life
TheEnd