July 2005 - The Hong Kong College of Anaesthesiologists
July 2005 - The Hong Kong College of Anaesthesiologists
July 2005 - The Hong Kong College of Anaesthesiologists
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
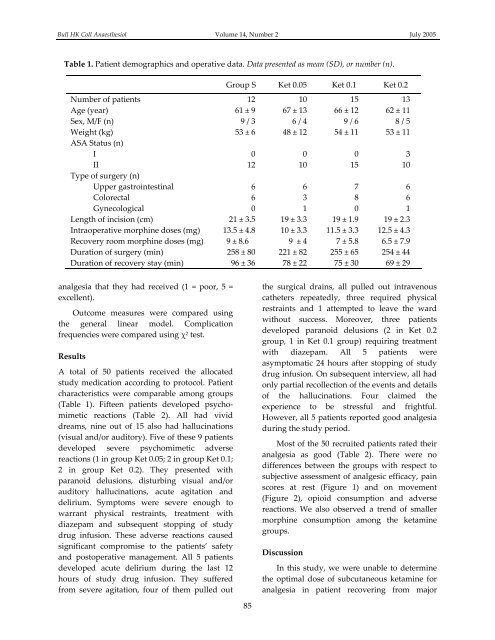
Bull HK Coll Anaesthesiol Volume 14, Number 2 <strong>July</strong> <strong>2005</strong>Table 1. Patient demographics and operative data. Data presented as mean (SD), or number (n).Group S Ket 0.05 Ket 0.1 Ket 0.2Number <strong>of</strong> patients 12 10 15 13Age (year) 61 ± 9 67 ± 13 66 ± 12 62 ± 11Sex, M/F (n) 9 / 3 6 / 4 9 / 6 8 / 5Weight (kg) 53 ± 6 48 ± 12 54 ± 11 53 ± 11ASA Status (n)I 0 0 0 3II 12 10 15 10Type <strong>of</strong> surgery (n)Upper gastrointestinal 6 6 7 6Colorectal 6 3 8 6Gynecological 0 1 0 1Length <strong>of</strong> incision (cm) 21 ± 3.5 19 ± 3.3 19 ± 1.9 19 ± 2.3Intraoperative morphine doses (mg) 13.5 ± 4.8 10 ± 3.3 11.5 ± 3.3 12.5 ± 4.3Recovery room morphine doses (mg) 9 ± 8.6 9 ± 4 7 ± 5.8 6.5 ± 7.9Duration <strong>of</strong> surgery (min) 258 ± 80 221 ± 82 255 ± 65 254 ± 44Duration <strong>of</strong> recovery stay (min) 96 ± 36 78 ± 22 75 ± 30 69 ± 29analgesia that they had received (1 = poor, 5 =excellent).Outcome measures were compared usingthe general linear model. Complicationfrequencies were compared using χ 2 test.ResultsA total <strong>of</strong> 50 patients received the allocatedstudy medication according to protocol. Patientcharacteristics were comparable among groups(Table 1). Fifteen patients developed psychomimeticreactions (Table 2). All had vividdreams, nine out <strong>of</strong> 15 also had hallucinations(visual and/or auditory). Five <strong>of</strong> these 9 patientsdeveloped severe psychomimetic adversereactions (1 in group Ket 0.05; 2 in group Ket 0.1;2 in group Ket 0.2). <strong>The</strong>y presented withparanoid delusions, disturbing visual and/orauditory hallucinations, acute agitation anddelirium. Symptoms were severe enough towarrant physical restraints, treatment withdiazepam and subsequent stopping <strong>of</strong> studydrug infusion. <strong>The</strong>se adverse reactions causedsignificant compromise to the patients’ safetyand postoperative management. All 5 patientsdeveloped acute delirium during the last 12hours <strong>of</strong> study drug infusion. <strong>The</strong>y sufferedfrom severe agitation, four <strong>of</strong> them pulled outthe surgical drains, all pulled out intravenouscatheters repeatedly, three required physicalrestraints and 1 attempted to leave the wardwithout success. Moreover, three patientsdeveloped paranoid delusions (2 in Ket 0.2group, 1 in Ket 0.1 group) requiring treatmentwith diazepam. All 5 patients wereasymptomatic 24 hours after stopping <strong>of</strong> studydrug infusion. On subsequent interview, all hadonly partial recollection <strong>of</strong> the events and details<strong>of</strong> the hallucinations. Four claimed theexperience to be stressful and frightful.However, all 5 patients reported good analgesiaduring the study period.Most <strong>of</strong> the 50 recruited patients rated theiranalgesia as good (Table 2). <strong>The</strong>re were nodifferences between the groups with respect tosubjective assessment <strong>of</strong> analgesic efficacy, painscores at rest (Figure 1) and on movement(Figure 2), opioid consumption and adversereactions. We also observed a trend <strong>of</strong> smallermorphine consumption among the ketaminegroups.DiscussionIn this study, we were unable to determinethe optimal dose <strong>of</strong> subcutaneous ketamine foranalgesia in patient recovering from major85