Annual report 2012-13 - West London Mental Health NHS Trust
Annual report 2012-13 - West London Mental Health NHS Trust
Annual report 2012-13 - West London Mental Health NHS Trust
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
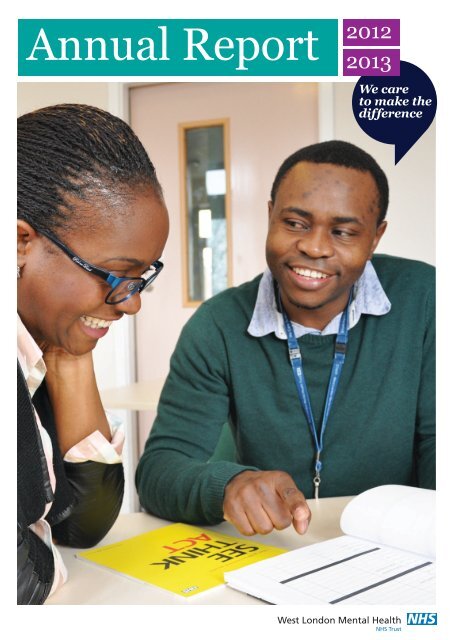
<strong>Annual</strong> Report <strong>2012</strong>20<strong>13</strong>
Message from the chairmanMessage from the chief executiveI would also like to thank everybody for their hardwork in moving forward with our application to bea foundation trust (FT).We are aiming to become an FT in 2014 and arecurrently undertaking the internal and externalassessments which will allow us to progress tothe next stage; assessment by the National <strong>Trust</strong>Development Authority (NTDA). The NTDA willwork with us to ensure our organisation is fit forpurpose and operates at the very highest levelsof effectiveness, providing excellent patient care,in line with our values and strategic aims. If ourapplication is approved we will then be referred toMonitor (the regulator) for a final assessment.There are many examples in the pages of this reviewof the work we are doing to improve services. Forexample, we’re moving our work rehabilitation servicesto the heart of the local community in Ealing. Thismeans not only a more attractive environment, but thechance for service users to participate in productivework. We are partnering with an organisation withexperience of making social enterprises a successwhich will help to ensure that the service is sustainable.Our focus on recovery, and our work as a pilot in thenational Implementing Recovery for OrganisationalChange (IMROC) programme, is ensuring that wemove towards a model of care with the patient and hisor her recovery at its heart.NigelMcCorkellI am delighted to have been reappointed this year aschairman for a further four-year term. Looking backover the last four years, there is much that we canbe proud of as we strive, in the words of our vision,to be an excellent provider of high quality services.We have agreed our core values and strategic aims,strengthened leadership at the trust, and becomea ‘flatter’ organisation with fewer layers betweenboard and service user, staff and directors, soenabling us to be a more responsive organisation.But I know that we have more work to do.We are making good progress on our plans todevelop our Broadmoor Hospital and St Bernard’ssites. You can read more about that in the pagesof this <strong>report</strong>. I want to thank everyone who hassupported this work. We are looking forward tomarking the 150th anniversary of Broadmoor inJune 20<strong>13</strong>.FT status will give us more freedom to respondto the needs of our service users and ourcommunities. The process itself is proving to bea focus for improvement and for engagementwith staff, partners and the public. Our aim overthe course of 20<strong>13</strong> is to continue recruiting ourtrust membership, which now stands at 8,000members, and prepare to hold elections for ourgoverning board, which will provide a strong voicefor service users, the public, staff and anybodyelse with an interest in helping to create the bestpossible mental health services.Nigel McCorkellSteveShrubbIt’s been nearly a year since I joined the trust. From dayone I’ve been struck by the compassion and qualityof care I’ve seen from staff across the organisation.There are many challenges for those of us workingin the <strong>NHS</strong> when the economy is difficult and thereare many changes facing both <strong>NHS</strong> services and theenvironment in which we operate. But wherever Ilook I see my colleagues working hard to improve thequality of care and service user experience while layingfirm foundations for the trust’s future.One of the main areas of focus for the trust is staffengagement. We value the work of our staff, butwe need to make sure that we show how we valuethem. They’re our key resource, they are best placedto identify the improvements that are needed and todeliver them. As you can read in this review, we areintroducing new ways to increase staff engagementand feedback.The role that each and every one of us plays indelivering safe, effective and continuously improvingcare has been brought home forcefully this year bythe Francis <strong>report</strong> into what went wrong at MidStaffordshire Hospital. We need to be mindful of itsfindings in all the decisions we make and ineverything we do.Our staff need the right infrastructure and supportto do their jobs to the best of their ability. Whethersupporting remote and mobile working, building aregister of patients interested in taking part in researchor allowing GPs direct access to our systems foreasier referrals and appointments, our IT colleagueshave been working to develop our knowledgemanagement and IT which is essential to help deliverour vision of high quality care and productivity.We don’t work in isolation. Especially at this time ofchange in the <strong>NHS</strong> and other public services. Buildingrelationships with GPs and other commissioners,stakeholders and the third sector is essential to ourtask of providing truly integrated care.I have been highly impressed and encouraged bywhat I have seen since joining the trust. There isalways more to be done, but I am confident that weare building a firm basis for the future as we strive todeliver safe and effective services providing excellentpersonalised care and treatment for everyone whouses our services.Steve Shrubb4 <strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>5
Best practice and user involvementStrategic aim: safe and effective servicesIt’s our priority to ensure that we deliver services that work in thebest interests of our service users and in this section of the <strong>report</strong>we discuss some of the areas where improvements have been made.<strong>Mental</strong> illness can be extremely distressing for service users andcarers. They need to be sure that they can access the help theyneed, when they need it, and that their voices are heard.24-hour support is just a call awayService users in our local services can now getsupport any time of the day or night, thanks to anew telephone support line we’ve launched.The line was set up with the help of theSamaritans, who worked with the trust’s learningand development team to train our contact centrestaff in how to manage the calls. The service,provided by the trust, gives access to clinicalsupport, advice for families, and informationabout mental health services 365 days a year.The line currently receives an average of 700 callsper month, around 8% of which are from peopleexperiencing an immediate mental health crisis.Service user and carer involvementThe involvement of service users and carers is vitalto ensuring that our services are the best that theycan be. We commissioned an independent reviewof the way we currently involve users and carersin our local services, carried out by Phil Hough, aconsultant and carer with experience of reviewinginvolvement services, and his brother Simon, aservice user.They ran workshops, met with involvement leadsand visited carer and user groups to find outhow involvement works in the trust. Their <strong>report</strong>,Enhancing Involvement, Embracing Experience,found that there is established involvement inthe trust, from co-producing and deliveringtraining to attending committees. However, thetrust lacks the systems needed to get and keeppeople involved.Phil explained: “It’s good that involvement happensand that lived experience is used to some degreebut it can be hit and miss. Service users and carersare not sure what they can be involved with andhow you go about getting involved.”The <strong>report</strong> makes recommendations forimprovements in four key areas: the process ofinvolvement, support structures, payments and ondeveloping a clear and simple new involvementstrategy for our local services.Chief executive Steve Shrubb welcomed the<strong>report</strong>: “We are committed to ensuring activeand positive engagement at every level of thetrust. The <strong>report</strong> will help us develop effective,well-supported involvement.”“Staff are also keen tohave a way to see at aglance where their effortsshould be focused in agiven month to maintainhigh standards of care.Dr Leigh Poyser, Darzi fellow“Hearing patients’ viewsOur new patient feedback system uses electronicquestionnaires on tablet computers and ourwebsite to find out how service users and carersrate their experiences. People can also makecomments and offer suggestions about what wecould do differently.Part of our commitment to improve the quality ofcare we deliver, the Meridian system allows usersto give their feedback anonymously. We will usethe results to help us deliver care in a way thatresponds to the needs of patients.A number of inpatient wards are also piloting highprofilepatient feedback boards, showing responsesto the Meridian patient questionnaires, as well ashow the ward is performing in key areas of qualityand safety.The feedback board pilot is being led by thetrust’s Darzi fellow, Dr Leigh Poyser, who said:“The idea has been really well received bypatients who particularly like the ‘you said…we did’ column, which shows comments andsuggestions from patients and what the ward isdoing to address any issues. Staff are also keen tohave a way to see at a glance where their effortsshould be focused in a given month to maintainhigh standards of care.”“We are committed toensuring active andpositive engagement atevery level of the trust.The <strong>report</strong> will help usdevelop effective, wellsupportedinvolvement.Steve Shrubb, chief executive“6 <strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>7
Developing national policy<strong>Trust</strong> expertise is helping to plan and developsecure and forensic services across the country.The trust’s medical director, Nick Broughton, chairsa national clinical reference group advising onsecure and forensic services.Clinical reference groups were set up by the <strong>NHS</strong>Commissioning Board (<strong>NHS</strong>CB) which oversees<strong>NHS</strong> services in England. They contribute to thestrategic planning of specialised services by bringingtogether clinical experts, patients and carers.Set up to help develop commissioning policiesand improve commissioning of services, they arethe main source of clinical advice to specialisedcommissioning for the <strong>NHS</strong>CB.The secure and forensic services group drawsmembers from across the country, includingclinicians from high, medium and low secureservices and those with knowledge and experienceof community forensic services.It also has two very active service userrepresentatives and a commissioning lead.The group’s most significant work to date hasbeen to develop national specifications for thecommissioning of high and medium/low servicesfor 20<strong>13</strong>-14.Rethinking schizophrenia careThe trust has been invited to join theDevelopment Network, created by Rethink<strong>Mental</strong> Illness to implement recommendationsof the Schizophrenia Commission’s <strong>report</strong>into the care received by people affected byschizophrenia and their families.The <strong>report</strong>, published in November <strong>2012</strong>, andthe recent National Audit of Schizophrenia,showed significant variation in care receivedacross the country.The network will be looking at ways toimplement, evaluate and support the spreadof best practice across the country. As part ofthis, the trust will identify areas of work wherekey recommendations of the <strong>report</strong> can beimplemented and studied.Rethink <strong>Mental</strong> Illness will be facilitatinglearning sets and master classes on themessuggested by network members and willcoordinate a national advisory board tosupport the programme of work.Focussing on recoveryStrategic aim: excellent personalised care and treatmentRecovery is the defining principle of everything we do. This meanswe have been moving from a model of care where we ‘look after’people to one where we work with patients to manage theirsymptoms and improve their health. We are working hard toembed this principle of recovery into everything we do.Patient-centred careThe trust was chosen two years ago as a pilot sitefor a national recovery initiative ImplementingRecovery for Organisational Change (IMROC), whichenabled us to benefit from expert advice and sharegood practice with trusts around the country. Theresult was a huge burst of energy and enthusiasmamong staff for the recovery ethos and we havebeen building on that with a range of initiativesdesigned to embed recovery into every service.Recovery conferences, such as west <strong>London</strong>forensic service’s conference in January, whichbrought together staff and service users to talkabout the importance of personal stories insupporting recovery.‘It’s Possible’, is an inspiring collection of artwork,poetry and personal accounts contributed bypeople who have used our forensic services, givento people newly admitted to the forensic service tohelp and encourage them.Broadmoor’s recovery college, where patients andstaff attend recovery learning sessions together,helping to break down barriers and give a sharedunderstanding of what recovery means.Recovery hubThe recovery hub was developed by the trust toprovide a variety of resources to staff, service usersand carers to assist them in their personal recoveryjourneys or with supporting others.The aim is to give people the tools and skills tobecome architects of their own recovery journeys.A large part of this process is encouraging andempowering people to take control of theirown lives and allowing individuals to take upopportunities that will support their recovery.All of the hub courses are jointly designed andrun by service users, carers, and staff. Theycover topics such as an introduction to recovery,disclosing mental health problems at work andbuilding confidence.“Today’s learning has given me more knowledgeand hope for my recovery journey,” said oneservice user after the course. A carer said: “It willhelp me to care for my son.”“Today’s learning has given memore knowledge and hopefor my recovery journey.Service user“8<strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>9
START projectThrough our START recovery project, teamshave been changing the way they work to helpthem become more recovery focussed. (STARTstands for system transformation aroundrecovery team.)Aurora ward, The OrchardFollowing training in the recovery approach, staffon Aurora ward in our Orchard women’s unit,have made changes to their multi-disciplinaryteam meetings – with service users now moreactively involved in discussions and decisions.“This was a new concept for many, but thebenefits have been immense, says wardmanager Lillian Hove. “We really do nowfeel like one big team. It has been a trulyempowering exercise for all involved.”Dr Hayley Dare, consultant clinical psychologistfor the ward added: “The benefits of the newways of working are significant for staff and forservice users. For example, staff sickness hasdecreased, complaints are now rare, seclusionand incidents have reduced too.”Patients also talk about positive changes they’veseen on the ward: “We’ve enjoyed working withstaff to produce pamphlets to give to new serviceusers to make them feel welcome and so theyknow about the activities and groups on offer. Thesupport from staff on this ward is tremendous andreally does help us along the way.”“The benefits of thenew ways of workingare significant for staffand for service users.For example, staffsickness has decreased,complaints are now rare,seclusion and incidentshave reduced too.Dr Hayley Dare, consultantclinical psychologist““Staff have more confidenceto engage positively withpatients whilst encouragingand supporting them totake responsibility for theirown care. Both patients andstaff on Kingfisher wardhave become one team andwe’re all striving for thesame goal, recovery.Brightmore Mukutirwa,ward manager“Kingfisher ward, LakesideBrightmore Mukutirwa, ward manager onKingfisher ward in Lakeside <strong>Mental</strong> <strong>Health</strong> Unitis a START project champion and has led histeam through a period of significant change.Kingfisher, a 20-bed women’s recovery ward,was in need of an innovative way to engageservice users and support them to take controlof their own care. “That’s where the STARTproject came in,” said Brightmore. “It gave theteam fresh ideas, new ways of working andnew ways of thinking.”“Since starting this project, the benefits havebeen vast. The average length of patient stayhas reduced from two years to less than sixmonths. Staff have more confidence to engagepositively with patients whilst encouraging andsupporting them to take responsibility for theirown care. Both patients and staff on Kingfisherward have become one team and we’re allstriving for the same goal, recovery.”Woburn ward, Broadmoor Hospital“Being part of the START project hasempowered us to be more creative and ishelping us to be more recovery focussed in ourwork,” says Janice Dickson, ward manager onWoburn ward.“The response from the team to the project hasbeen great, we’ve all welcomed the additionalsupport which has included recovery workshopsfor patients and staff.“One noticeable difference is that patients arenow contributing much more to their own careplans and we’re talking to the patients earlierabout regional secure units, which shows thatwe’re more focussed on recovery than we mayhave been in the past. We’ve also invited patientsfurther along in the recovery journey in to talk toour patients to inspire hope and confidence.“It has been great to have some time out to reallythink through what we do and to think as a groupabout what improvements we should be makingfor patients to make sure their recovery is in thefore of our minds at all times.”“One noticeable differenceis that patients arenow contributing muchmore to their own careplans and we’re talkingto the patients earlierabout regional secureunits, which shows thatwe’re more focussed onrecovery than we mayhave been in the past.Janice Dickson, ward manager“10 <strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>11
Great moves for work rehabMeaningful work can be the biggest boostto recovery and our work rehab services haveflourished on the St Bernard’s Hospital site. Nownew premises, in busy locations at the heartof the community, will enable the people withmental health problems and learning disabilitieswho use them to experience a real worksituation, dealing directly with the public.The print shop and picture framing servicehave moved to <strong>West</strong> Ealing, along with twocommunity shops. Horticulture is moving toHorsenden Hill Farm, a busy beauty spot inPerivale. We’re also looking to set up a cateringbusiness run by service users in the newArmstrong Way building when staff moveover there later this year.“This partnership means wecan continue to providesupport and direction,while helping to securethe businesses’ future,so allowing us to offergreater opportunities tomore service users ontheir way to recovery.“John Belli, deputy service managerThe new businesses are being run in partnershipwith Accession Social Enterprise, who have yearsof expertise in setting up social enterprise andmaking them work.John Belli, deputy service manager at workrehabilitation said: “This partnership means wecan continue to provide support and direction,while helping to secure the businesses’ future, soallowing us to offer greater opportunities to moreservice users on their way to recovery.”Helping from experiencePeer support workers are key to our recoveryapproach. Having experienced mental distressthemselves, they are well placed to work alongsideothers with similar stories, helping them to recoverby promoting hope and providing support basedon their common experience.Peer support workers are given training, and havetheir own personal supervisor throughout the course.Edward Dixon is the first paid peer supportworker with the early intervention team for clientsexperiencing their first episode of psychosis.“Service users are experts by experience,” he says.“We are making a move away from the patient/expert relationship. Our role is to act as coachesor mentors and enable the individual to take backcontrol of their lives and ownership of their illness.We can help to find and maintain hope until thatperson is able to maintain hope for themselves.“I feel that believing that I could do it made abig difference in my recovery. I had learned byexperience to embody my aspirations and keepmotivated, determined, and positive in order tosucceed as well as keeping the goals realistic. Thiszeal and enthusiasm is something I hope to sharewith everyone I work with.“Supporting mental healthin general hospitalsThis year we expanded our liaison psychiatry teamto provide more comprehensive services in the three<strong>London</strong> boroughs we cover. One aspect of liaisonpsychiatry services is to provide ageless (16+) specialistmental health care to patients in the general hospitalsetting, who have coinciding physical health andmental health problems. A person’s physical healthcan have a profound effect on their mental health (andvice versa), particularly for those people living with longterm physical ill-health. This year we developedinpatient liaison psychiatry pilot teams at EalingHospital and <strong>West</strong> Middlesex University Hospital, aswell as maintaining the pre-existing services we runat Charing Cross Hospital, Hammersmith and QueenCharlotte’s & Chelsea Hospital.Bruce Mamvura, team manager says: “I amenormously proud to currently manage the liaisonpsychiatry service at Ealing Hospital as I believe theseservices are in a unique position to make a positivedifference to the psychiatric care and treatment ofpatients within the general hospital setting.“This includes providing assessment and treatment topatients with long term chronic physical illnesses thatmay, for example, have also become depressed. Theteam’s work is very diverse and we are able to respondurgently to the care of any patients presenting withsignificant risks to them self or others, usually in A&E,as well as also extending support to elderly patientswith delirium and dementia. There is no greaterreward than to see patients recover quicker withimproved longer term outcomes, by receiving the rightintervention for their mental health needs, at the sametime as their physical healthcare.”In addition, this year, clinicians from our liaisonpsychiatry teams have been contributing to theintegrated care pilot in north west <strong>London</strong> (NWL). Thisinitiative aims to improve outcomes for patients withlong term conditions (such as diabetes, coronary heartdisease and chronic obstructive pulmonary disease),create access to better, more integrated care outsideof hospital, reduce unnecessary hospital admissionsand enable effective working of health and socialcare professionals across provider boundaries. In thismodel of care we see clinicians working together inmulti-disciplinary groups which include acute providers,general practice, community care, social care andmental health to provide collaborative and cohesivecare for patients with complex problems. Due tothe success of this pilot the work will continue to bedeveloped in the coming year.12<strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong><strong>13</strong>
Recognised for qualityStrategic aim: provider of choiceWe aim to be the mental health provider of choice in west <strong>London</strong>, theservice that people can turn to, knowing that they will find top-quality care.Towards foundation trust statusIn order to succeed as an independent, effectivetrust we need to become a foundation trust.Foundation trusts manage their own finances, arefree from direct government control and can takedecisions that are best placed to improve servicesfor the local community. We are aiming to achieveFT status by 2014.Building for top-quality careThe trust is about to embark on two majorredevelopment projects, one at our St Bernard’s sitein Southall and the other at Broadmoor Hospital inBerkshire. Both will create modern, fit-for-purposebuildings, each designed to support the high-qualitycare our staff provide, but with enough flexibility toadapt to the needs of our patients in the future.<strong>Trust</strong>s have much more involvement and controlby the people who know what is needed tomake a difference and improve services – ourstaff and service users. We will have a council ofgovernors, made up of staff, service users, partnerorganisations and the public, responsible forholding the board to account for the performanceof the trust and ensuring that the voice of our keystakeholders is heard.Steve Shrubb, chief executive of the trust, said:“Our ability to become a foundation trust willdepend upon the support of every staff memberand this in turn will enable us to achieve our visionof becoming a leading provider of excellent mentalhealth services.”“Our ability to become afoundation trust will dependupon the support of everystaff member and this in turnwill enable us to achieve ourvision of becoming a leadingprovider of excellent mentalhealth services.“St Bernard’sSome of the buildings that make up St Bernard’sare no longer suitable for the delivery of modernmedium secure mental health care, whilst othersrequire extensive refurbishment to make themfit for purpose for local services patients. InNovember, the board approved the business casefor a new 80-bed medium secure unit to replacethe existing John Conolly Wing.In preparation for this work and to allow us tomake better use of our estates and improvemental health services, we have been preparingthe site, renovating buildings and relocatingservices. So far, we have moved the psychiatricintensive care unit (PICU) to Hammersmith,upgraded Glynn ward (now called Jubilee ward)to accommodate older people’s services andcompleted a £3 million refurbishment of B-blockfor inpatients.The coming year will see additional moves to getthe site ready for the wider redevelopment ofSt Bernard’s later in 20<strong>13</strong>.Chief executive Steve Shrubb said: “Theredevelopment work is allowing us to makebetter use of <strong>NHS</strong> resources, while creatingmore space for clinical services.”Vickie Holcroft, programme manager said:“We are making good progress with theredevelopment of the St Bernard’s site. We areworking closely with all our stakeholders and thelocal community to provide the best solution forour service users, whilst securing local jobs andenhancing the local community.”Broadmoor HospitalBroadmoor Hospital, as one of only three highsecurehospitals in England, plays an importantrole in the mental health system. However, manyof its buildings have changed little since theywere built in 1863. The outdated layout is makingit increasingly difficult for staff to provide themodern treatments our patients need, that offerbest value for <strong>NHS</strong> funds.Built within the existing grounds, the new hospitalwill contain 234 beds, providing accommodationfor 210 male patients, and space for 24 flexible-usebeds. Alongside this new living space, there will bea new therapy building housing vocational services,Our plans for a redeveloped Broadmoor Hospital.patients’ shopping facilities, education servicesand visiting suites. The aim is to give patients moreindependence, which we know has a positiveimpact on rehabilitation, while enhancing our abilityto provide safe and secure services.Site preparation, including demolishing some of theunused buildings, creating a link road to divert trafficfrom the local town centre and safely re-housingprotected species, will continue until late 20<strong>13</strong>, whenconstruction of the new hospital can begin.Leeanne McGee, director of high secure servicessaid: “We have recently introduced a new modelof care aimed at motivating and encouragingpatients while providing them with intensivetreatment, all centred on therapeutic activities.Evidence shows that treating patients in this waycan lead to faster recovery. The new building willhelp us implement this model, and put our servicesin line with best practice models across the world.”Steve Shrubb, chief executive14<strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>15
“The system has proved verysuccessful and from an initialpilot of just eight gp’s, we arenow rolling direct bookingout across the trust.“Commissioner engagementRelationships – with patients, with our staff, and withour partner organisations – are key to the success ofthe trust. And with the changes in the <strong>NHS</strong>, we alsoneed to ensure that the new commissioners in clinicalcommissioning groups (CCGs) hear about the qualityservices we offer and see us as the provider of choicefor local patients.This is also the guiding principal of the integrationwork we’ve been doing with key stakeholdersincluding CCGs, the local authority, primary care,third sector partners, service users and carers onour new transformation board. Set up in January20<strong>13</strong>, it is co-chaired by our medical directorDr Nick Broughton and one of the CCG mentalhealth leads, GP Dr Annabel Crowe.The transformation board will allow us to build onthe work which has been started by our redesignprogramme board, but with a focus on collaboratingwith our external partners to meet the priorities forthe north west sector of <strong>London</strong> – making sure thatmental health services are provided where, whenand how local people want them.Michael Doyle,programme managerSupporting GPs to make referralsWe were the first mental health trust in Englandto use direct booking, where GPs can accessour clinical appointments system and book anassessment during a consultation. Based on thenational Choose and Book system, direct bookingprovides a more efficient service for our referrersand a better experience for patients.GPs can now link directly to the adult assessmentteam and the memory and dementia services,allowing them to see exactly what appointments areavailable. They can also look up information suchas referral investigations and treatments offered.Patients can choose the time and date of theirappointment with a mental health clinician whilethey are sitting with their GP.Evidence shows that Choose and Book offers a hostof benefits, including shorter waiting times betweenreferral and a reduction in non-attendance at firstappointments, which are high in the trust. Early datashows non-attendance figures are reducing alongwith average waiting times for first appointment.All 31 GP practices in Hammersmith & Fulham arenow able to use direct booking. Next steps includeadding the Hounslow early intervention and cognitiveimpairment and dementia teams on to the system.Michael Doyle, local services programme manager,said: “The system has proved very successful and froman initial pilot of just eight GPs, we are now rollingdirect booking out across the <strong>Trust</strong>. A number of acuteproviders have also requested our input to supporttheir own move to electronic referral and booking.”One stop shopTo supplement the support we offer GPs, we’velaunched a new area on our website, specificallyaimed at referrers.The dedicated section was created in consultationwith local GPs and brings referral advice, clinicalpathways and other guidance together in one place.Raising awareness withthe Tamil communityMany of <strong>London</strong>’s Tamil community arrivedhere as refugees from the war in Sri Lanka.The trust has been keen to raise awareness ofthe psychological effects of war trauma andencourage people to come forward and use theservices available to help them.A conference, ‘Promoting well-being in the TamilCommunity’, brought together Tamil people,clinicians and mental health organisations tohear about the effects war trauma can have onpsychological health.Clinicians who work closely with Tamil peoplehad the opportunity to take part in workshopsto improve their understanding of issues facingthe Tamil community and to help them overcomepossible obstacles to communication.The conference was organised in partnership withCentral and North <strong>West</strong> <strong>London</strong> <strong>Mental</strong> <strong>Health</strong> <strong>Trust</strong>and the Tamil Community Centre in Hounslow.Guests also enjoyed a vibrant example of Tamilculture – a display of dancing and music.<strong>Trust</strong> consultant psychologist, Dr AngelaManning said: “The event was a step towardshelping clinicians and the Tamil communityunderstand the effects of war trauma andreduce the stigma of mental ill health. We werepleased to have over 20 organisations join usat the event and were supported by Mind andthe IAPT (Improving Access to PsychologicalTherapies) service who offered advice to thecommunity. It was a great collaboration.”“The event was a steptowards helping cliniciansand the Tamil communityunderstand the effects ofwar trauma and reduce thestigma of mental ill health.Dr Angela Manning,trust consultant psychologist“16<strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>17
Setting the pace on qualityStrategic aim: continuous improvement of quality and productivityThe trust is constantly striving to improve the services we provideand promote good practice in mental health care. This meansinnovating and using all our resources, including technology andresearch. And it means engaging with other partners to contributeto and benefit from national developments in mental health care.Improving access to therapy“The therapy works as an accelerator in thehealing process. I’ve stopped worrying about thethings I cannot change and learned to acceptthem.” That was the feedback from Douglas,who uses one of the trust’s three ImprovingAccess to Psychological Therapies (IAPT) services.IAPT is a national initiative introduced in 2008 tomake psychological treatments for people withdepression and anxiety disorders more readilyavailable. There is evidence that IAPT services arecontributing to real improvements in the lives ofpeople with anxiety and depression, with recoveryrates nationally in excess of 45%.Ruth Dennis, who manages the Hammersmith& Fulham service, explains: “Service users tellus that they value the flexible way we provideour services, either in person, over the phoneand even by computer. We provide treatment attimes and in places to suit services users. Theycan refer themselves rather than going througha GP, which helps cut down on waiting timesand the need for health professionals to spendtime on referrals.”People can sign up to the online Buddy tool,a text messaging service which enables usersto keep a diary, helping them to identify whattriggers certain moods and figure out their owncoping mechanisms.The service has also joined up with employeesupport agencies to provide employment advicefor service users who need it and the serviceoffers other benefits through its relationshipwith mental health charity MIND.Harnessing technologyfor better patient careThe trust’s IT team is helping to improve clinicalinformation sharing between mental health cliniciansand GPs in Hounslow. SystemOne allows a linkbetween the clinicians and the GP’s patients system.Not only will this improve communicationsbetween professionals equally engaged inimproving a patients’ health; the system willenable them to send messages, and it will flag upany alerts.After the pilot phase, the system will be extendedto the adult community assessment and recoveryteams and to A&E.Patients receiving a service from the local servicescan get automated text reminders one week and,again, one day in advance of their appointment.This has already proved effective in reducingnon-attendance to appointments which is verycostly to us.The service allows for two-way communicationbetween the service user and the trust contactcentre so that the service user can text back aresponse to confirm, cancel, or reschedule.Clinical auditOne way we check on the quality of care isthrough the National Clinical Audit and PatientOutcomes Programme (NCAPOP). This nationalproject collects data on a particular area of carewith the aim of ensuring that all patients receivethe most effective, up-to-date and appropriatetreatment, delivered by clinicians with the rightskills and experience.The trust’s commitment to this performancemonitoring can be seen by the fact that during<strong>2012</strong>-<strong>13</strong> we participated in all the nationalclinical audits we were eligible for. We alsotook part in the <strong>2012</strong> National ConfidentialEnquiry in suicide and homicide by people withmental health illness. Like the audit, the aimis to detect areas for improvement and makerecommendations, but confidential enquiriesgo further than audit, with each case criticallyreviewed by a team of experts to see whetherclinical standards were met, and whether theright clinical decisions were made.We reviewed the <strong>report</strong>s of six national clinicalaudits in <strong>2012</strong>/<strong>13</strong>. The actions we have drawnup as a result can be seen in full on our website.Medical director, Dr Nick Broughton said: “Theseclose looks at our work help us see what weare doing well and just as important, where weneed to improve. They are an invaluable way ofhelping to make our services better.”“These close looks at ourwork help us see what weare doing well and just asimportant, where we needto improve. They are aninvaluable way of helping tomake our services better.“Dr Nick Broughton, medical director18<strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>19
Academic <strong>Health</strong> Science PartnershipThe trust is a key partner in the new Academic<strong>Health</strong> Science Partnership (AHSP) which bringstogether healthcare providers across northwest <strong>London</strong>, including metal healthcare, anduniversities to improve health and quality carefor patients.Researchers and clinicians work together tounlock new opportunities for patients, both indirect care and in research and development,sharing specialist expertise. The trust’s boardagreed to provide a share of the initial funding,enabling us to play a key role in developing thepartnership’s programme and ensuring that metalhealth is an important part of the research.Dr Craig Ritchie, the trust’s director of researchand development, said: “This is the latest stepin our five-year strategy to become a leader inresearch into mental health treatment and care.”Transforming services withpatients at the centreIn line with other providers of mental healthcare providers in <strong>London</strong>, the trust is workingwith primary care to ensure service users arecared for more routinely by GP teams in thecommunity so that service users receive moreappropriate care and scarce resources andfunds are used more efficiently.Our local services transformation board is helpingus build more joined up and integrated services,bringing together senior clinicians, serviceusers, carers, managers, clinical commissioninggroups, local authority leads and voluntaryorganisations. It provides the forum to make keydecisions in designing pathways that are simpleto understand, effective and designed with thepatient at their centre.All three CCGs are enthusiastic about thisapproach. One of the programme board’s firstpieces of work is likely to be looking at how wecan better provide mental health care in primarycare so that patients only need to receive care fromspecialist services when it is absolutely necessary.Harnessing the skills and experience of all our staffStrategic aim: an engaged workforce focussed on recoveryEngaged staff deliver better results and so it’s our aimto work with staff to improve levels of engagement.Gathering staff feedbackSome 30 staff members from across theorganisation have volunteered to lead a projectto discover how staff feel about working at thetrust. We’re running this project because weknow from the <strong>NHS</strong> staff survey that our staff donot feel valued in parts of the organisation. It’simportant that we address this because we knowfrom research that staff who feel valued by theirorganisation and involved in decision makingare more productive at work, leading to a betterservice and better outcomes for patients.Each volunteer agreed to speak to ten colleaguesabout their experiences and opinions of working atthe trust. These views will be fed back to the board.The aim is to ensure that the board hears exactlywhat staff feel needs to be done to improve theculture and ways of working at the trust.Chief executive Steve Shrubb said: “Staffengagement is fundamental to the future successof our organisation. The <strong>report</strong>er project uses theexpertise we already have – the people who workhere. They understand the issues, and can advisethe board on how best to improve the way wework together in the trust.”“This is the latest step inour five-year strategyto become a leader inresearch into mental healthtreatment and care.Dr Craig Ritchie, director ofresearch and development““Staff engagement isfundamental to thefuture success of ourorganisation.“Steve Shrubb, chief executive20<strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>21
“For their own benefit andthat of their patients, mentalhealth staff should haveaccess to regular, high quality,clinical supervision.“Steve Shrubb, chief executiveClinical supervision – supportingstaff to support their patientsClinical supervision is key to helping mentalhealth staff cope with job-related stress andwe know from research evidence that it canimprove patient care, reduce sickness absencerates and boost staff wellbeing and morale.Following a national conference on clinicalsupervision hosted by the trust in 2011, weagreed to launch a new programme, aimedat ensuring that nurses and occupationaltherapists have regular access to evidencebased,high quality clinical supervision.Creating a dialogue with staffWe know from our surveys that staff feel theydon’t know enough about our key strategicpriorities, nor about the wider <strong>NHS</strong> policies thatinfluence us. They also told us that they feeldisengaged from senior management.In response, chief executive Steve Shrubb hasincreased publication of his blog to staff, awell-read update on issues facing the trust, toonce a week. And, because we want to improvecommunications with all our stakeholders, it’savailable on the website too.“The tone is positive,” explains Steve. “But itdoesn’t shirk difficult discussions about whereimprovement is needed.”Our monthly listening events, held in differentlocations around the trust, give staff the chanceto hear directly from the chief executive what ishappening, give their views and put any questionsthey might have to the executive team.Diversity adviser joins the trustThe trust is working to strengthen the way itmeets the needs of all our service users, carersand staff through a new post of diversity adviser.Jane Gaffa, who has a background as a clinician,has initially focussed on meeting the diversityneeds of service users, while providing adviceand guidance to staff.Already the diversity unit has produced a rangeof tools to help clinicians provide care that isappropriate to the particular service user, including:• Guidance on dealing with sexuality.• A video produced in conjunction with thegender identity clinic, on caring for trans-genderservice users.• A tool-kit on the culture, customs, and religiouspractices of some of our largest communities.• Working with the trust’s spirituality & pastoralcare department and IT specialists on a spiritualassessment tool (HOPE), to help staff ask usersabout religion and spirituality.• Organised a conference in conjunction withCentral and North <strong>West</strong> <strong>London</strong> to raiseawareness of the issues faced by the Tamilcommunity in accessing mental health servicesand reduce stigma associated with mentalillness in the Tamil community.Diversity training itself has been revamped thisyear with a renewed focus on the patient.Jane said: “I have only been in post for ashort while, but I am already impressed by thefoundations which are in place. Working withinan atmosphere of positive change is very uplifting,as is the trust’s renewed commitment to progressequality for service users’ and staff.”We have also introduced the ManchesterClinical Supervision Scale to enable us tomonitor the programme in terms of benefits tostaff wellbeing and patient outcomes.The programme began with an evaluation ofclinical supervision at the trust. The informationwas used by the project team, which includesinternational experts in the field, to design anew policy to strengthen clinical supervision sothat it reflects the latest research evidence andour own findings.This year, we have added extra listening eventsspecifically for staff from black and minorityethnic (BME) communities. The aim is toimprove engagement with BME staff and helpto improve representation at senior levels withinthe trust.“For their own benefit and that of theirpatients, mental health staff should have accessto regular, high quality, clinical supervision,”said chief executive Steve Shrubb. “The aim isfor all nurses and occupational therapists tohave training in clinical supervision so that wecan embed the process throughout the trust.”22<strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>23
Aiming for equalityThe trust has agreed four equality objectivesand an action plan, to make the environmentmore inclusive for its service users and staff.We aim to:• Improve the quality and completeness ofinformation obtained from our electronicdata collection systems by 2014.• Increase the number of equality impactassessments undertaken that relate to servicechanges and improve the quality of theseassessments by 2014.• Reduce violence perpetrated by users,relatives and carers against BME staff from25% to national average of 18% by 2014.• Reduce the number of <strong>report</strong>s in the staffsurvey from people who have experienceddiscrimination from 28% to national averageof 14% by 2014.Conference for front line care staffThis year over 100 of our healthcare assistants(HCAs) and clinical support workers (CSWs) cametogether for the trust’s first annual healthcareassistant conference.Tanis Hand, national HCA advisor at the RoyalCollege of Nursing, was our keynote speakerand talked about how important it is for HCAsto have a voice not only within the organisation,but nationally too. A key focus of the day was tounderstand how we can support these key staffbetter, through training and education.Francis Thompson, head of nursing educationand standards said: “I was delighted by theattendance at our first conference which willnow be held annually to give our staff a goodopportunity to share information, learn fromothers and network.”“I was delighted by theattendance at our firstconference which willnow be held annuallyto give our staff a goodopportunity to shareinformation, learn fromothers and network.“Francis Thomson, head ofnursing education and standardsCelebrating excellenceOur Employee of the Month Award celebratespeople who have shown outstandingcommitment to their work. And once a year, ourQuality Awards recognise those individuals andteams who have delivered that extra something interms of innovation, team work and patient care.Director of organisational development andworkforce, Rachael Moench, said: “Not onlyare the awards a great way of saying thankyou to staff, they also help celebrate our valuesof togetherness, responsibility, excellence andcaring. They show the difference that enthusiastic,committed people make to our organisation.”That includes people like Emmanuel Ofori, whoset up a band with service users. At first, it washard to manage a diverse group with variousmental health problems to work as a team.Emmanueal gave up his Saturday afternoonsand Tuesday evenings to teach, provide technicaladvice and inspire the group to use their soulfulmusic as a pathway to recovery.Senior nurse Appiah Oyinka, who nominatedEmmanuel, said: “Through music he has given thegroup the needed confidence to grow, developand acquire a new sense of purpose in life in spiteof their mental health problems.”Our ambitionfor the future<strong>West</strong> <strong>London</strong> <strong>Mental</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong> is at akey point in its development as we strive tobecome a foundation trust.This annual <strong>report</strong> sets out some of the advanceswe have been making and the challenges weface in working towards our vision of being aprovider of excellent, high quality services, witha focus on recovery.However, like all <strong>NHS</strong> organisations we facechallenges in today’s health economy wherebudgets are decreasing and competition to provideservices is increasing. We are constantly challengedto find new and more efficient ways of deliveringservices which has resulted in changes to the waywe run some services as well as a reduction in thenumber of staff posts needed to deliver services.The scale and pace of change has proved difficultfor staff working in those areas. Patients and theircarers also have had to get used to care beingprovided differently.Again this year we have an ambitious programmefor our services, our staff, our buildings and, aboveall, for the experience we offer our service users.Our objectives for 20<strong>13</strong>-14 focus on:• Becoming a leading provider – were aiming tobe the leading provider in specialist areas andto be amongst the best across the full range ofservices we provide.• Person-centred care - the needs of ourservice users and their carers will remain ouroverriding priority. We will work in partnershipwith service users and carers in order to deliverperson-centred care that reflects their needs.As such these key stakeholders will be activelyinvolved in the ongoing development of thetrust. We will ensure that they are effectivelyengaged and able to meaningfully influenceour strategic decisions.• Partnerships - we will work to deliver excellentcare in collaboration with other providers,including colleagues in primary care, acute care,other mental health trusts and the not-for-profitsector. We will develop strategic partnershipsto deliver integrated care pathways for specificpatient groups, such as individuals suffering fromlong term conditions such as diabetes and COPD.• Evidence-based services - our research anddevelopment strategy will ensure that researchis a central component in how we deliverclinical care, and that the trust has a reputationfor innovation and academic excellence. Inkeeping with this we will be an active memberof Imperial College <strong>Health</strong> Partners and willwork closely with other healthcare providers todevelop and deliver integrated models of care.• Valued staff - our services need to be deliveredby well-trained, highly motivated and clinicallyengaged staff, working across a full rangeof disciplines. We will work to give our staffthe support they need to do their jobs to anexcellent standard.Key to our plans are two programmes to redevelopour two main sites, St Bernard’s in Ealing andBroadmoor Hospital. These extensive redevelopmentswill transform dated buildings into modern premisesthat can support modern, high-quality care. There’salso the important but challenging work we’re doingthrough our local services transformation boardwhich aims to bring services out of hospital and intothe community, closer to home, at the same time aswe build more joined up and integrated services withprimary care and social services. Equally we mustensure that they are financially sustainable.We are working hard to achieve foundation truststatus which will give us greater autonomy, thepower to manage our own finances and the abilityto respond with greater flexibility to the needs ofour local communities. The process we’re goingthrough is time-consuming and challenging,but with enough of a focus we’re aiming to beaccredited as a foundation trust by 2014.24<strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>25
InformationAbout the trustStructure<strong>West</strong> <strong>London</strong> <strong>Mental</strong> <strong>Health</strong> <strong>Trust</strong> is structuredaround three clinical service units.The three clinical service units are:• Local services.• High secure services (Broadmoor Hospital).• Specialist and forensic services.Each of our clinical service units is led by a directorwho is a member of the board, along with strongclinical leadership.We serve a diverse population and it’s importantthat we attract and develop staff who reflect thecommunities we serve and deliver services thatare culturally sensitive and appropriate. We have adedicated diversity advisory service which focuseson making diversity from both an employment andservice provision perspective, part of our day-todaybusiness.Employee relationsWe work very closely with the trade unions whorepresent their colleagues. We believe strongly inpartnership working and this is why we have atrust partnership forum, where union officers meetwith the trust’s directors and senior managers on aregular basis to discuss current staff issues.The trust provides information to its staff ina variety of ways including an intranet, chiefexecutive’s blog, quarterly magazine, monthlyteam brief and weekly email bulletin. Inaddition, monthly listening events are hosted bydirectors and ad hoc briefings are given on keydevelopments. The majority of staff have regularteam meetings with their line manager and havean annual performance development review.Where significant changes are proposed, formalconsultation is undertaken with all affected staff.ComplaintsOur central governance team provides us with avaluable source of feedback on the experiencesof our service users, carers and wider publicusing our services through the Patient Adviseand Liaison Service (PALS), complaints andcompliments. During <strong>2012</strong>/<strong>13</strong>, we received andregistered 307 formal complaints, <strong>13</strong>83 PALSconcerns and 34 compliments. We respondedto 89% of complaints in an agreed timeframeand shall continue to work to increase our timelyresponse rate in the coming months.The key emerging themes highlighted incomplaints were related to all ‘aspects of care andtreatment’ and ‘staff attitude’. Care and treatmentthemes cover a wide range of issues includingmedication, admission, assessments, diagnosis,detainment and discontent due to policies such asthe no smoking and room search policies. Themesrelated to staff attitudes include service userssaying they feel they are not being treated withrespect and dignity.We work to resolve such issues and, at the sametime, take action in individual cases. Such actioncould include expediting a payment to a serviceuser due to their property being lost during a wardmove or training staff. We have the mechanismsin place to learn from complaints and furtherwork is being done to make those mechanismsmore robust. At the same time, it is our priority toapologise, learn from people’s experience and doeverything we can to prevent a reoccurrence.We set targets around response times which isagreed with the complainant and learning fromcomplaints is closely monitored by the board,providing assurance that we will improve practiceand, in turn, the patient experience.CQC registrationAll <strong>West</strong> <strong>London</strong> <strong>Mental</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong> servicesare registered with the Care Quality Commission(CQC) ‘ without conditions’. This means that therehave been no formal concerns raised on the qualityof the services by the CQC.The Care Quality Commission has not taken anyenforcement action against <strong>West</strong> <strong>London</strong> <strong>Mental</strong><strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong> during <strong>2012</strong>/<strong>13</strong>.<strong>West</strong> <strong>London</strong> <strong>Mental</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong> has notparticipated in any special reviews or investigationsby the CQC during <strong>2012</strong>/<strong>13</strong>. However, as partof their routine schedule of visits we receivedtwo <strong>report</strong>s from the CQC that assessed ourcompliance against the ‘Essential Standards ofQuality and Safety’.Following the visits they concluded that the trustwas not meeting the outcomes below:Outcome 07: safeguarding peoplewho use services from abuseThe CQC judged that the Limes was not meetingthis standard and that this has a moderate impacton service users using this service. CQC felt thatservice users using this service were not fullyprotected from risk of abuse because trust staffwere not always able to take reasonable steps toensure staff always responded appropriately toany allegation of abuse.The actions taken to address this issue were:• Immediate internal alert disseminated acrossthe trust to ensure all staff knew the process forhighlighting safeguarding concerns.• Focus groups were held to establish theunderlying cause of this concern.• Bespoke training was implemented withimmediate effect.• All incidents/ concerns discussed at service areaweekly meetings.• Policy reviewed, updated and staff consultationcompleted.Outcome 14: supporting workersCQC judged that people are supported bystaff who receive training to deliver care to anappropriate standard. However, staff themselvesdid not feel appropriately supported in relation totheir responsibilities, which they felt had an impacton the care people received, and could put peoplewho use the service at risk.The actions taken to address this issue were:• The development and implementation of astaff engagement programme, where feedbackis received from a wide selection of staff andcomments directly <strong>report</strong>ed to the trust board.• The board agreed the implementation ofthe trustwide workforce and organisationaldevelopment strategy.• The whistleblowing policy was immediatelyreviewed, updated and reissued across the trust.These outcomes are due to be re-assessed byCQC in June 20<strong>13</strong> to ensure full compliance hasbeen achieved.26 <strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>27
Statement of the chief executive’sresponsibilities as the accountable officer of the trustCapitalThe trust fixed assets have increased to £364 million in <strong>2012</strong>/<strong>13</strong> (£350 million in 2011/12). The £14 millionincrease in the value of fixed assets is due to capital expenditure in year, offset by depreciation and a reductionin the value of land and buildings following a full revaluation by the district valuer.The trust invested £32.3 million in the capital programme in <strong>2012</strong>/<strong>13</strong>. The Broadmoor Hospitalredevelopment continues to receive public funds from the Department of <strong>Health</strong> to fund part of theredevelopment work.The trust has two major capital projects Broadmoor redevelopment and the medium secure unit reprovsion.Future financial performanceThe trust continues to faces a number of challenges in the next few years.These are summarised as:External environment - Continued impact of the economic downturn on publicly funded services,changes in commissioning and the reality of increased competition. This will increase as a tariff fundedapproach to mental health services is introduced.Internal - The increasingly challenging requirement for cost improvements while maintaining andraising quality. The need to continue to shift cost improvements from essentially transactional approachto a transformational one brings both risks and opportunities The trust is fundamentally changing itsmodel of local services to a stronger community focus with less dependence on inpatient beds. This hassignificant impact of staff. The implementation of mental health payment for activity and the currentabove average reference cost position for those services first in line for tariff approach leads to an addedpressure for cost reduction. As finances get tighter only services that meet cost and quality requirementswill be commissioned.The chief executive of the <strong>NHS</strong> has designated that the chief executive should be the accountable officerto the trust. The relevant responsibilities of accountable officers are set out in the accountable officersmemorandum issued by the Department of <strong>Health</strong>. These include ensuring that:• there are effective management systems in place to safeguard public funds and assets and assist in theimplementation of corporate governance;• value for money is achieved from the resources available to the trust;• the expenditure and income of the trust has been applied to the purposes intended by parliament andconform to the authorities which govern them;• effective and sound financial management systems are in place; and• annual statutory accounts are prepared in a format directed by the secretary of state with the approvalof the treasury to give a true and fair view of the state of affairs as at the end of the financial year andthe income and expenditure, recognised gains and losses and cash flows for the year.To the best of my knowledge and belief, I have properly discharged the responsibilities set out in my letterof appointment as an accountable officer.Capital – The funding and delivery of two major capital redevelopments will continue to be asignificant challenge.SignedDate29/05/20<strong>13</strong>Steve Shrubb Chief executiveSignedDate29/05/20<strong>13</strong>Barbara Byrne Director of finance & information / deputy chief executive32<strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>33
Statement of financial position as at 31 March 20<strong>13</strong>31 March 20<strong>13</strong> (£) 31 March <strong>2012</strong> (£)Non-current assets:Property, plant and equipment 363,629 349,937Intangible assets 3 6Total non-current assets 363,632 349,943Current assets:Inventories 385 311Trade and other receivables 7,301 8,349Cash and cash equivalents 27,798 24,293Total current assets 35,484 32,953Non-current assets held for sale 500 848Total current assets 35,984 33,801Total assets 399,616 383,744Current liabilitiesTrade and other payables (24,317) (20,449)Provisions (2,056) (1,908)Total current liabilities (26,373) (22,357)Non-current assets plus/less net current assets/liabilities 373,243 361,387Non-current liabilitiesTrade and other payables (123) (<strong>13</strong>2)Provisions (2,633) (2,547)Total non-current liabilities (2,756) (2,679)Total assets employed: 370,487 358,708Statement of changes in taxpayers’ equity for the year ended 31 March 20<strong>13</strong>Changes in taxpayers’ equity for <strong>2012</strong>-<strong>13</strong>Public Dividend Retained Revaluation Other Totalcapital earnings reserve reserves reservesBalance at 1 April <strong>2012</strong> 270,562 (<strong>13</strong>,321) 101,931 (464) 358,708Retained surplus/(deficit) for the year 0 (25,998) 0 0 (25,998)Net gain / (loss) on revaluationof property, plant, equipment 0 0 54,505 0 54,505Net gain / (loss) on revaluationof assets held for sale 0 0 924 0 924Impairments and reversals 0 0 (32,763) 0 (32,763)Transfers between reserves 0 924 (1,388) 464 0New PDC Received 15,111 0 0 0 15,111Balance at 31 March 20<strong>13</strong> 285,673 (38,395) 123,209 0 370,487Changes in taxpayers’ equity for 2011-12Balance at 1 April 2011 257,362 (16,188) 99,321 (464) 340,031Retained surplus/(deficit) for the year 0 1,675 0 0 1,675Net gain / (loss) on revaluationof property, plant, equipment 0 0 6,655 0 6,655Net gain / (loss) on revaluationof assets held for sale 0 0 (<strong>13</strong>) 0 (<strong>13</strong>)Impairments and reversals 0 0 (2,840) 0 (2,840)Transfers between reserves 0 1,192 (1,192) 0 0New PDC Received <strong>13</strong>,200 0 0 0 <strong>13</strong>,200Balance at 31 March <strong>2012</strong> 270,562 (<strong>13</strong>,321) 101,931 (464) 358,708Financed by: taxpayers’ equityPDC 285,673 270,562Retained earnings (38,395) (<strong>13</strong>,321)Revaluation reserve 123,209 101,931Other reserves 0 (464)Total Taxpayers’ Equity: 370,487 358,70836<strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>37
Statement of cash flows for the year ended 31 March 20<strong>13</strong>31 March 20<strong>13</strong> (£) 31 March <strong>2012</strong> (£)Cash flows from operating activitiesOperating surplus/deficit (14,232) <strong>13</strong>,245Depreciation and amortisation 10,493 10,929Impairments and reversals 31,282 3,206Donated assets received credited to revenue but non-cash (1,450) 0Dividend paid (11,544) (11,918)(Increase)/decrease in inventories (74) 4(Increase)/decrease in trade and other receivables 1,048 (1,769)Increase in trade and other payables 2,941 1,976Provisions utilised (2,056) (1,199)Increase in provisions 2,247 1,980Net cash inflow from operating activities 18,655 16,454Cash flows from investing activitiesInterest received 69 54(Payments) for property, plant and equipment (30,330) (15,839)Net cash outflow from investing activities (30,261) (15,785)Net cash inflow/(outflow) before financing (11,606) 669Cash flows from financing activitiesPublic dividend capital received 15,111 <strong>13</strong>,200Net cash inflow from financing activities 15,111 <strong>13</strong>,200Net increase in cash and cash equivalents 3,505 <strong>13</strong>,869Cash and Cash Equivalents at Beginning of the Period 24,293 10,424Cash and Cash Equivalents at year end 27,798 24,293DIRECTORS’ REMUNERATIONSalary and pension entitlements of senior managers<strong>2012</strong>/<strong>13</strong> 2011/12Salary Other Performance Benefits Salary Other Performance Benefitsremuneration related remuneration relatedbonusesbonuses(bands of (bands of (bands of rounded (bands of (bands of (bands of roundedName and Title £5,000) £5,000) £5,000) to £100 £5,000) £5,000) £5,000) to £100Peter Cubbon, chiefexecutive, until 30/04/12 20-25 - - - 175-180 - - -Steve Shrubb, chiefexecutive, from 25/06/12 160-165 - - - 0 - - -Barbara Byrne, director offinance & information /deputy chief executive <strong>13</strong>0-<strong>13</strong>5 - - - 120-125 - - -Steve Trenchard, directorof nursing and patientexperience, until 31/01/<strong>13</strong> 100-105 - - - 120-125 - - -Anne Aiyegbusi, interimdirector of nursing and patientexperience, from 03/12/<strong>2012</strong> 30-35 - - - 0 - - -Leanne McGee, director ofhigh secure services 115-120 - - - 115-120 - - -Dr Nick Broughton,medical director 145-150 - 15-20 - 145-150 - 15-20 -Nigel Leonard, director ofplanning and corporateaffairs, until 19/10/12 55-60 - - - 90-95 - - -Jean George, director oflocal services 110-115 - - - 110-115 - - -Andy Weir, director offorensic services 110-115 - - - 105-110 - - -Charles Allen, interim directorof organisational developmentand workforce, until 31/12/12 90-95 - - - 5-10 - - -Rachael Moench, director oforganisational developmentand workforce, from 17/12/12 30-35 - - - 0 - - -Nigel McCorkell, chairman 20-25 - - - 20-25 - - -Barbara Kerin,non-executive director 5-10 - - - 5-10 - - -Lynne Weedall,non-executive director 5-10 - - - 0-5 - - -Christine Higgins,non-executive director 5-10 - - - 5-10 - - -Dame Sally Powell,non-executive director,until 30/09/12 0-5 - - - 10-15 - - -Prof Lefkos Middleton,non-executive director 5-10 - - - 5-10 - - -Neville Manuel,non-executive director 5-10 - - - 5-10 - - -Geoff Rose,non-executive director 5-10 - - - 5-10 - - -Carolyn Gray,non-executive director,from 18/03/20<strong>13</strong> 0-5 - - - 0 - - -38<strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>39
Pay multiples commentaryDIRECTORS’ REMUNERATIONDirectors pension benefitsReal increase Total accrued Cash equivalent Cash equivalent Real increasein pension & pension & transfer transfer in cashrelated lump related lump value at 31 value at 31 equivalentsum at age 60 sum at age 60 March 20<strong>13</strong> March <strong>2012</strong> transfer(bands of (bands of (£) (£) (£)£2,500) £2,500)Peter Cubbon, chief executive,until 30/04/12 0 305-310 0 1593 N/ASteve Shrubb, chief executive,from 25/06/12 22.5-25 355-360 1860 1125 519Barbara Byrne, director of finance &information / deputy chief executive 5-7.5 205-210 1182 955 177Steve Trenchard, director ofnursing and patient experience 0-2.5 5-10 64 46 <strong>13</strong>Anne Aiyegbusi, interim directorof nursing and patient experience,from 03/12/12 0-2.5 155-160 759 628 32Leanne McGee, director ofhigh secure services - - - - -Dr Nick Broughton,medical director 0-2.5 <strong>13</strong>5-140 531 490 15Nigel Leonard, director ofplanning and corporate affairs,until 19/10/12 0 20-25 96 411 (186)Jean George, director oflocal services 0-2.5 100-105 494 453 17Andy Weir, director offorensic Services 22.5-25 70-75 348 306 26Charles Allen, interim directorof organisational developmentand workforce, until 31/12/12 0-2.5 175-180 0 877 N/ARachael Moench, director oforganisational developmentand workforce, from 17/12/12 0-2.5 95-100 387 275 28Reporting bodies are required to disclose the relationship between the remuneration of the highest-paiddirector in their organisation and the median remuneration of the organisation’s workforce.The banded remuneration of the highest paid director at <strong>West</strong> <strong>London</strong> <strong>Mental</strong> <strong>Health</strong> <strong>Trust</strong> in thefinancial year <strong>2012</strong>-<strong>13</strong> was £242,500 (2011-12, £202,500). This was 7.5 times (2011-12, 6.4) themedian remuneration of the workforce, which was £32,282 (2011-12, £31,618).In <strong>2012</strong>-<strong>13</strong>, no employees received remuneration in excess of the highest-paid director (2011-12, 0).Remuneration ranged from £6,100 to £191,100 (2011-12, £6,100 to £202,100).Total remuneration includes salary, non-consolidated performance-related pay, benefits-in-kind as well asseverance payments. It does not include employer pension contributions and the cash equivalent transfervalue of pensions.During the financial year <strong>2012</strong>-<strong>13</strong> there has been a decrease to the trust’s workforce due in part to the closureof the dangerous & severe personality disorders unit (DSPD) at Broadmoor Hospital and the family serviceat The Cassel at the end of the 2011-12 financial year. Achieving trust cost improvement targets has alsoresulted in a reduction in the employee numbers. The reduction in the workforce has affected staff across allpay bands and has therefore not had a material impact on the pay multiple ratio comparison, year-on-year.Exit packages agreed<strong>2012</strong>-<strong>13</strong>Number of Number of other Total number ofExit package cost band compulsory departures exit packages(including any special payment element) redundancies agreed by cost bandLess than £10,000 1 0 1£10,001-£25,000 11 0 11£25,001-£50,000 4 0 4£50,001-£100,000 5 0 5£100,001 - £150,000 4 0 4£150,001 - £200,000 0 0 0>£200,000 0 0 0Total number of exit packages by type 25 0 25Total resource cost (£) 1,284 0 1,284SignedSteve Shrubb Chief Executive, Accountable OfficerDate 29/05/20<strong>13</strong>40<strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>41
2011-12Number of Number of other Total number ofExit package cost band compulsory departures exit packages(including any special payment element) redundancies agreed by cost bandLess than £10,000 2 7 9£10,001-£25,000 10 8 18£25,001-£50,000 6 34 40£50,001-£100,000 4 14 18£100,001 - £150,000 2 5 7£150,001 - £200,000 0 2 2>£200,000 2 0 2Total number of exit packages by type 26 70 96Total resource cost (£) 1,581 3,377 4,958Better payment practice codeBetter payment practice code <strong>2012</strong>-<strong>13</strong> <strong>2012</strong>-<strong>13</strong> 2011-12 2011-12Measure of compliance (number) (£) (number) (£)Non-<strong>NHS</strong> payablesTotal non-<strong>NHS</strong> trade invoices paid in the year 29,375 64,873 29,023 46,818Total non-<strong>NHS</strong> trade invoices paid within target 27,205 61,641 27,628 44,852Percentage of non-<strong>NHS</strong> trade invoices paidwithin target 93% 95% 95% 96%<strong>NHS</strong> payablesTotal <strong>NHS</strong> trade invoices paid in the year 621 4,201 612 3,990Total <strong>NHS</strong> trade Invoices paid within target 579 4,142 576 3,926Percentage of <strong>NHS</strong> trade invoices paidwithin target 93% 99% 94% 98%Staff sickness absenceOff payroll engagementsOff-payroll engagements at a cost of over £58,200 per annum that were in place as of 31 January <strong>2012</strong>.No. in place on 31 January <strong>2012</strong> 17Of which:<strong>2012</strong>-<strong>13</strong> 2011-12TotalTotalnumbernumberTotal days lost 36,356 36,982Total staff years 3,367 3,650Average working days lost 10.8 10.1No. that have since come onto the organisation’s payroll 0No. that have since been re-negotiated/re-engaged to include to include contractualclauses allowing the (department) to seek assurance as to their tax obligations 0No. that have not been successfully re-negotiated, and therefore continue withoutcontractual clauses allowing the (department) to seek assurance as to their tax obligations 6No that have come to an end 11Total 30The six engagements <strong>report</strong>ed above all relate to individuals contracted to work for the trust viaemployment agencies. In each instance the individuals remuneration is paid net of taxation which theagency pays directly to HMRC.The Department of <strong>Health</strong> also requires <strong>NHS</strong> bodies to <strong>report</strong> any new off-payroll engagementscommencing between 23 August <strong>2012</strong> and 31 March 20<strong>13</strong>, for more than £220 per day and for longerthan 6 months. During this period there were no new off-payroll engagements that fulfills this criteria.The Late Payment of Commercial Debts (Interest) Act 1998The trust did not incur any expenditure in relation to this Act during <strong>2012</strong>/<strong>13</strong> or 2011/12.42<strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>43
Governance statement <strong>2012</strong>/<strong>13</strong>from the chief executive1. Scope of responsibilityAs accountable officer, and chief executive ofthis board, I have responsibility for maintaining asound system of internal control that supports theachievement of the organisation’s policies, aims andobjectives whilst safeguarding the public funds andthe organisation’s assets for which I am personallyresponsible, in accordance with the requirements setout in the accountable officer memorandum.I am accountable to the chairman of <strong>West</strong> <strong>London</strong><strong>Mental</strong> <strong>Health</strong> <strong>Trust</strong> for my performance. I am alsoaccountable to <strong>NHS</strong> <strong>London</strong> for the performanceof the trust. I work in partnership with PCTs /CCGs, local authorities and the police, throughlocal partnership boards and agreements, todeliver objectives that cut across organisationalboundaries. There are also separate performancereviews with <strong>NHS</strong> <strong>London</strong> for the services providedby the high secure hospital, Broadmoor.As chief executive, I have overall responsibility forhaving effective risk management arrangementsin place. As accountable officer I have delegatedthe following lead responsibilities to otherexecutive directors:• Director of nursing & patient experience -responsibility for infection control, liaison withthe Care Quality Commission, patient safety,patient experience, risk management and theboard assurance framework.• Medical director - overall responsibility forclinical effectiveness, medicines managementand safeguarding.• Director of finance / deputy chief executive -responsibility for financial and business risk.• Clinical service unit (CSU) directors areresponsible for ensuring significant risks areidentified, assessed, and effectively controlledwithin their area of responsibility.2. Governance frameworkThe trust’s governance framework is designed tomanage and mitigate risk to a reasonable levelrather than to eliminate all risk of failure to achievepolicies, aims and objectives; it can therefore onlyprovide reasonable and not absolute assurance ofeffectiveness. Governance and internal control ofthe organisation is an ongoing process designed to:• identify and prioritise the risks to the achievementof the organisation’s policies, aims and objectives,• evaluate the likelihood of those risks being realisedand their impact, should they be realised, and• manage and mitigate risk efficiently, effectivelyand economically.The system of internal control has been in place in<strong>West</strong> <strong>London</strong> <strong>Mental</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong> throughoutthe year ended 31 March 20<strong>13</strong> and up to the dateof approval of the annual <strong>report</strong> and accounts.The board is compliant with the corporategovernance code and continues to make goodprogress with its application to become a foundationtrust. Further reviews of the governance frameworkhave taken place especially in relation to qualitygovernance and this was reviewed by externalassessors (Ernst & Young) and an action plandeveloped to address the issues raised, whichincluded strengthening our quality strategy bymaking objectives more measurable, improving andstreamlining the performance and quality metrics<strong>report</strong>ed to the board and ensuring consistent qualitygovernance arrangements across the trust’s CSUs.Other areas of governance have also been subjectedto external review including financial governanceand the effectiveness of the board. The board hasnow instigated a process of continuous improvementin relation to governance arrangements taking intoaccount the lessons learnt from other applicant trustsand external experts. The board is supported in itsjourney by a comprehensive board developmentprogramme which is informed both by individualand collective appraisals of board members and thefeedback from the various experts. The trust, thestrategic health authority and the Department of<strong>Health</strong> have a tripartite formal agreement, settingout key milestones to be achieved on the FT journey,against which they formally monitor our progress.From 1 April 20<strong>13</strong>, the trust’s progress with bemonitored by the <strong>NHS</strong> <strong>Trust</strong> Development Authority.Supporting committee structureTo support the board in carrying out its dutieseffectively, sub-committees <strong>report</strong>ing to it havebeen formally established. Their remits and termsof reference were reviewed during the year toensure robust governance and assurance. Eachreceives a set of regular <strong>report</strong>s as outlined in itsterms of reference and provides summary <strong>report</strong>sto the trust board after each meeting.The main sub-committees are as follows:Audit committee - reviews the establishment andmaintenance of an effective system of integratedgovernance, risk management and internal controlacross the whole of the trust’s activities. Gainsassurance that effective systems of internal controlare in place and monitors the integrity of the trust’sfinancial information.Quality committee - discusses evidence of clinicalgovernance and risk management within the trust.It provides strategic leadership for the developmentof continuous quality improvement, based on userexperience and feedback from stakeholders. Itscrutinises the risk register, approves and monitorsthe risk management processes and providesassurance on these processes to the audit committee.It approves and monitors the implementation ofclinical governance delivery plans.Finance & investment committee - ensuresthat processes governing strategic investments arebeing followed, and makes recommendations tothe board. This includes major capital or revenueexpenditure, the purchase, sale or alteration ofproperty (above an agreed threshold) and serviceexpansion or major service change, in addition toinformation governance.Attendance at board & sub committees <strong>2012</strong>/<strong>13</strong>During the year all board and sub committeemeetings have been quorate, except the trustboard meeting in December <strong>2012</strong>, where businesswas conducted with due regard to that fact.CommitteeAverage attendanceof members<strong>Trust</strong> board 82%Audit committee 75%Quality committee 67%Finance & investmentcommittee 80%The quality committee attendance figures wereimpacted in year by the long term absence, due toill health, of one member.In addition to the above, key, sub-committees forgovernance and assurance, the board is supportedby the:• Remuneration & nominations committee• Charitable funds committee• <strong>Mental</strong> health act managers’ committee• Service users’ & carers’ forumAlso, three programme boards, the staffengagement forum and the trust managementteam <strong>report</strong> into the trust board.44 <strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>45
3. Risk assessment and managementThe trust’s risk assessment and managementarrangements are described in detail in the trust’srisk management policy, which complementsthe trust’s risk management strategy. These riskmanagement arrangements enable risks to beidentified, assessed, and controlled consistentlyand effectively.The board is aware of the risks in the organisationthrough the use and review of the risk register and isresponsible for ensuring action plans are in place tomanage those risks. Risks are managed in differentways including risk transfer and developing systemsto mitigate risks. All staff within the organisationhave a responsibility for risk management and thetrust has in place a programme of training andeducation for staff which includes risk managementand clinical risk training.Risks that cannot be managed within the highsecure services, specialist & forensic services orlocal services clinical service units or corporatedepartments, are escalated to the trust-wide (level1) risk register. There may be some residual riskthat cannot reasonably be eliminated that theboard will choose to accept where this is necessaryto deliver its objectives.Level 1 risks and the board assurance frameworkare reviewed bi-monthly by the board and regularlyby the audit committee, quality committee,finance & investment committee and the trustmanagement team.The trust has a comprehensive and effectiveclinical audit system in place which is closelyaligned to the board’s assurance framework andreflects clinical risks identified through the incident<strong>report</strong>ing system. The clinical audit programme isoverseen by the trust’s quality committee and themedical director is the executive director with theresponsibility for clinical audit.During <strong>2012</strong>/<strong>13</strong> the trust’s clinical governancearrangements have been externally assessedby Ernst & Young on two occasions against therequirements of the Monitor quality governanceframework. These assessments have demonstrateda progressive improvement. Work is ongoingto further improve the monitoring of clinicalperformance and to ensure the implementation ofthe trust’s recently revised quality strategy.Highest risksThe current highest-rated risks to the trustconcern: (i) potential failure to deliver savings inlocal services; (ii) potential failure to achieve thecost improvement plan (CIP) efficiencies requiredby the current five year trust integrated businessplan; (iii) the impact of failure to redevelop theSt Bernard’s Hospital site; and (iv) the consistentassessment and management of clinical risk.New risks <strong>2012</strong>/<strong>13</strong>In the past year, several new significant trust-widerisks were identified and continue to appear on thetrust-wide risk register. These are:• Lack of an effective quality strategy and metricsleading to inconsistent quality of care resultingin poor patient experience and commissionerdissatisfaction.• Failure to deliver savings in local services inline with commissioners’ intentions 20<strong>13</strong>/14,resulting in service restrictions and/or closures.In addition, several closely related risks werecombined and are now represented by a singleclinical risk:• Failure to assess and manage clinical riskeffectively, resulting in harm.4. The risk and control frameworkThe risk management strategy, complemented bythe risk management policy, details the lines ofaccountability and the responsibilities of all staff,including accountability arrangements with keystakeholders. It describes the trust committeestructure established to ensure effective riskmanagement and the arrangements in placeto ensure the board receives timely, accurateinformation on the principal risks to achievementof the trust’s strategic aims i.e. the boardassurance frameworkThe board assurance framework details thesignificant risks to the achievement of the trust’sstrategic aims, the key controls in place tomanage those risks, the assurances regarding theeffectiveness of those controls, any gaps in controlor assurance and the actions that are being takento secure more effective control over that risk.Therefore, the board is kept aware of thosesignificant risks to the trust’s achievement ofits strategic aims through its monthly review ofthe trust-wide (level 1) risk register, the <strong>report</strong>sit receives from the chairs of the board’s subcommitteesand its bi-monthly review of the boardassurance framework.Significant trust-wide risks are reviewed regularlyby the trust management team, and assurances,regarding the effective management of risk, aregiven by other board sub-committees, which arechaired by non-executive directors. Those subcommitteesroutinely scrutinise the risks and, inthe process, receive from the risk owner detailedinformation about the nature, severity andmanagement of the risk.The audit committee provides the board with furtherassurance regarding the trust’s risk managementarrangements. The audit committee is assisted inits work by the internal audit service which, in thecourse of the year, performs the detailed scrutinyof selected trust-wide risks. Internal audit <strong>report</strong>sits findings to the audit committee, commenting,for example, on the appropriateness of the risk keycontrols, the validity of the assurances provided forthat risk and the appropriateness of the plannedadditional risk-mitigating actions.Similarly, in the course of the year, the clinical auditservice performed audits across the trust, focussingon the historically high-risk clinical activities e.g.‘engagement and observation’. The audit findingsare <strong>report</strong>ed to and reviewed by the trust clinicalaudit governance group.The governance arrangements at CSU and directoratelevel complement the governance arrangements atboard and board sub-committee level.The trust’s risk control framework includes theprovision to staff of appropriate induction andrefresher training covering key risk areas e.g.clinical risk, counter-fraud, human resources,financial, health and safety, etc. The trust-widelevel of compliance by staff with their mandatorytraining requirements is monitored monthly by thetrust management team.All staff within the organisation have aresponsibility for risk management. Servicemanagers are required to record on their servicerisk register (and, subsequently, manage effectively)any significant risks affecting their service. The riskescalation process means that risks which cannotbe managed entirely within one CSU or directorateare escalated to the trust-wide risk register.46 <strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>47
5. Reviewing the effectiveness of riskmanagement and internal controlThe trust’s risk management arrangements have beeneffective, enabling the trust to identify potentiallysignificant risks at an early stage and take suitableaction to either prevent those risks developing furtheror, if necessary, control those risks.In February 20<strong>13</strong>, the trust was assessed as complyingwith level 1 of the <strong>NHS</strong> litigation authority (<strong>NHS</strong> LA)risk management standards, the trust complying withall 50 of the risk management standards.RSM Tenon, the trust’s internal auditors, hasjudged the trust to have a risk maturity statusof ‘risk managed’. This provides independentevidence of the robustness and effectiveness of thetrust’s risk management arrangements. This is anotable improvement compared to last year, whenthe trust was judged to have ‘risk defined’ status.The trust is working towards achieving‘risk enabled’, the highest level possible (seetable below).In carrying out audits across the trust, the workof internal audit provides assurance on theeffectiveness of certain risk controls. Where thoseaudits reveal areas for improvement, these are fedback to the service manager concerned and theCSU director so suitable action can be taken.In order to confirm that the trust has effectivesystems in place which link clinical audit to theboard’s assurance framework an advisory review ofclinical audit was undertaken by the trust’s internalauditors during 2011/12. This concluded that theIncreasing risk maturitytrust has taken active steps for ensure that its clinicalaudit function is in line with identified best practice.The medical director commissioned an externalreview of the trust’s clinical governancearrangements which assessed the trust against thequality governance requirements for foundationtrusts. The review was undertaken by KPMG. Thisfound that the trust has invested significantly instructures and processes designed to ensure that thequality of clinical services can be defined, measuredand <strong>report</strong>ed both openly and clearly. The reviewidentified certain areas for further developmentwhich are in the process of being addressed.External assurance was provided on aspectsof the trust’s quality account for 2011/12 byPricewaterhouseCoopers LLP.Clinical risk managementThe trust in accordance with <strong>NHS</strong>LA requirementsfor biennial review was re assessed against the<strong>NHS</strong>LA standards in February 20<strong>13</strong>. The trust wassuccessful in retaining the mental health <strong>NHS</strong>LAlevel 1 standards. The director of nursing andpatient experience has responsibility for <strong>NHS</strong>LAand performance monitoring is undertaken by thetrust management team meetingThe trust’s complaints policy is in line with theNational <strong>Health</strong> Service (complaints) regulations. Thesystem of managing complaints is reviewed by thequality committee to ensure that improvements incare as a result of complaints are evident. There isnow an improved process in place for managementand learning from complaints. Compliance with thetimescales for responding to complaints is <strong>report</strong>edAware Defined Managed EnabledInformal approachto risk managementRisk managementapproach adoptedto meet basicexpectations ofstakeholdersRisk managementapproach built intonormal businesspracticeRisk managementsupports the deliveryof strategic aimsmonthly to the board. Internal audit providedpositive assurance over these processes.The trust has an electronic incident <strong>report</strong>ingsystem throughout the organisation for <strong>report</strong>ingall incidents, including “near misses”. A summaryof “complaints, incidents and claims” is presentedto the quality committee to ensure that issuesidentified are shared more widely.Infection control & registrationThe trust continues to implement its infectioncontrol action plan which is overseen by the trustwideinfection control group and <strong>report</strong>ed to thepatient safety and safeguarding sub committee.An annual <strong>report</strong> is submitted to the qualitycommittee. Monthly audits are undertaken andactions implemented accordingly.Finance, resources & environmentThe trust has a robust system to maintain regularoversight of its financial position. This includes thefinance & investment committee.As an employer with staff entitled to membershipof the <strong>NHS</strong> pension scheme, control measures are inplace to ensure all employer obligations containedwithin the scheme regulations are complied with.This includes ensuring that deductions from salary,employer’s contributions and payments in tothe scheme are in accordance with the schemerules, and that member pension scheme recordsare accurately updated in accordance with thetimescales detailed in the regulations.Control measures are in place to ensure that all theorganisation’s obligations under equality, diversityand human rights legislation are complied withand this is led by the equalities steering groupwhich <strong>report</strong>s through the clinical effectiveness andcompliance committee into the quality committee.The trust continues to undertake risk assessmentsin accordance with emergency preparedness andcivil contingency requirements (based on UKCIP2009 weather projections) to ensure it meets itsobligations under the Climate Change Act andthe adaptation <strong>report</strong>ing requirements. Businesscontinuity plans (BCPs) include heat wave andsevere weather episodes. The BCP annual reviewprocess captures flood events at applicablesites and acknowledges and addresses the risksthat climate change poses to the continuedfunction and performance of the trust. Capitalredevelopment projects consider the impactsof climate change on drainage and flood riskmanagement strategies.Carbon reduction delivery plans have beendeveloped to cover trust buildings, transportand travel, procurement and other key areas.These are in the process of being implementedfollowing the approval of the trust’ssustainability strategy in 2011/12.CapitalThe trust has two major capital redevelopmentprojects, one relating to Broadmoor Hospitaland the other to the redevelopment of our StBernard’s site in Ealing, that present an area of riskin terms of capital resources and delivery. I gainassurance that risk is adequately managed throughthe programme boards, one of which I chair(Broadmoor) and the other which is chaired by thedirector of finance / deputy chief executive. Bothprogrammes have <strong>report</strong>ed to the trust board on aregular basis in <strong>2012</strong>/<strong>13</strong>.The trust received an advisory audit on the StBernard’s redevelopment programme in <strong>2012</strong>/<strong>13</strong>.The audit had an overall rating of “green” andcontained no recommendations. Procurementand compliance with standing orders was also thesubject of an advisory audit and had an overallrating of “amber/green”, with 6 medium priorityand 1 low priority recommendations which will beimplemented in 20<strong>13</strong>/14.48 <strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>49
Information governanceA revision (version 10) of the informationgovernance self assessment was published byConnecting for <strong>Health</strong> in June <strong>2012</strong>. In anticipationof this revision a comprehensive informationgovernance work plan was put in place in April<strong>2012</strong> which was reviewed when informationgovernance toolkit version 10 was published.The medical director is executive lead forinformation governance in addition to being thetrust Caldicott Guardian. The director of finance/ deputy chief executive is the senior informationresponsible officer.The trust has achieved a score of 71%(satisfactory) for <strong>2012</strong>/<strong>13</strong>. Internal audit hasassessed a sample of the scores that we selfassessedto give additional assurance.<strong>NHS</strong> organisations are also required to include intheir annual <strong>report</strong>s details of serious incidentsinvolving data loss or breach of confidentiality.There were no such major incidents in <strong>West</strong><strong>London</strong> <strong>Mental</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong> in <strong>2012</strong>/<strong>13</strong>.Other personal data-related incidents in<strong>2012</strong>/<strong>13</strong>:Category Nature of incident TotalI Loss of inadequately protected electronic equipment, devices or paper 0documents from secured <strong>NHS</strong> premisesII Loss of inadequately protected electronic equipment, devices or paper 0documents from outside secured <strong>NHS</strong> premisesIII Insecure disposal of inadequately protected electronic equipment, 0devices or paper documentsIV Unauthorised disclosure 5V Other 11“Other” covers minor potential internal breaches of confidentiality where there are no actual personal data losses.When incidents are <strong>report</strong>ed they are reviewed and appropriate action taken and any wider lessonslearned shared.6. Review of effectivenessAs accountable officer, I have responsibilityfor reviewing the effectiveness of the systemof internal control. My review is informed in anumber of ways:1. The head of internal audit provides me with anopinion on the overall arrangements for gainingassurance through the assurance frameworkand on the controls reviewed as part of theinternal audit work.Opinion on the effectiveness ofthe system of internal controlBased on the work undertaken in <strong>2012</strong>/<strong>13</strong>,significant assurance can be given thatthere is a generally sound system ofinternal control, designed to meet theorganisation’s objectives, and that controlsare generally being applied consistently.2. Executive directors within the organisation whohave responsibility for the development andmaintenance of the system of internal controlprovide me with assurance.3. The assurance framework itself provides mewith evidence that effectiveness of controls thatmanage risks to the organisation achieving itsprincipal objectives have been reviewed.4. Registration with the CQC - the trust isregistered with the Care Quality Committeewith no conditions.I have been advised on the implications of theresult of my review of the effectiveness of thesystem of internal control by the followingcommittees within the trust:• Audit committee• Quality committee• Finance & investment committee• <strong>Trust</strong> management teamThe board will continue to review progress aspart of eliminating weakness and ensuring that aprocess of continuous improvement is in place inthe trust in 20<strong>13</strong>/14 through the following actions:• Work towards <strong>NHS</strong>LA level 2 accreditation.• Improve staff engagement processes andarrangements.• Consider the recommendations of the Francis<strong>report</strong> in the context of this organisation andimplement any required improvements.• Embed new, strengthened arrangements forgovernance and nursing leadership.• Establish a senior leadership developmentprogramme.• Through our quality action plan and priorities,ensure service users are treated with the highestlevels of dignity, compassion and respect.• The timely implementation of any internal andexternal audit recommendations.SignedDate 29/05/20<strong>13</strong>Steve Shrubb Chief Executive, Accountable Officer50 <strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>51
SustainabilityDelivering a sustainable healthcare service forthe trust is embracing the connection between awell designed healing environment and improvedhealthcare safety and quality for service users,carers and staff, and the associated cost savings,looking at pathways of care, not only to cut outwaste but to see what can be done differently fora better patient experience and providing healthcare that is accessible to all, financially viable anddelivered with little impact to the environment.<strong>West</strong> <strong>London</strong> <strong>Mental</strong> <strong>Health</strong> <strong>Trust</strong> is bound by theoverall <strong>NHS</strong> target which aims to reduce carbonfootprint by 10% between 2009 and 2015. Thetrust is determined to ensure a planned andsustainable reduction of its impact, maximisingbenefits to service users, staff and the widercommunity and reducing the amount of energyused in our buildings contributes to this goal.Greenhouse gas emissionsOur measured greenhouse gas emissions have increased by 527 tonnes of CO 2this year. This is attributable tothe colder winter we have experienced this year. However, the breakdown shows a decrease in our greenhousegas emissions from electricity by 285 tonnes of CO 2.During the <strong>2012</strong>/<strong>13</strong>, our gross expenditure on the carbon reduction commitment (CRC) energy efficiencyscheme was £154,054. This amount included our cost for carbon allowances, subsistence fees to theEnvironment Agency and the cost of auditing our <strong>report</strong>s and evidence pack as required on the scheme.The CRC energy efficiency scheme is a mandatory scheme aimed at improving energy efficiency andcutting emissions in large public and private sector organisations.EnergyOur energy costs have reduced by 2% in <strong>2012</strong>/<strong>13</strong>. We have put plans in place to reduce carbonemissions and improve our environmental sustainability. Over the next 10 years we expect to save£650,000 as a result of these measures.£Total energy consumptionOur total energy consumption has risen during the year, from 42,725 to 44,231 MWh and the changesrelates to an increase in gas consumption mostly used for space heating. However, we have seen areduction in the amount of electricity use resulting in the 2% cost reduction.MWh2,300,0002,250,0002,200,0002,150,0002,100,0002,050,0002,000,0001,950,0001,900,0001,850,0001,800,000We are working on plans to build an energy centre which will reduce our emission by up to 19%.60000500004000030000200001000002008/9 2009/10 2010/11 2011/12 <strong>2012</strong>/<strong>13</strong>2008/9 2009/10 2010/11 2011/12 <strong>2012</strong>/<strong>13</strong>ElectricityGasTonnes CO 2e800007000060000500004000030000200001000002008/9 2009/10 2010/11 2011/12 <strong>2012</strong>/<strong>13</strong>Water consumptionOur water consumption has increased by 5,188 cubic meters in the recent financial year. In <strong>2012</strong>/<strong>13</strong> wespent £246,214 on water.175,000170,000165,000160,000155,000150,000145,000140,0002008/9 2009/10 2010/11 2011/12 <strong>2012</strong>/<strong>13</strong> ** The increase in water consumption may be attributable to construction works being undertaken as part of theredevelopment of St Bernard’s site.RoadElectricityGas52 <strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>53
Who runsthe trustWasteWe currently recover or recycle 169 tonnes ofwaste, 21% of the total waste we produce and weare working to ensure we reduce the amount ofwaste that is sent to landfill through infrastructurechanges and a behaviour change programme.169tonnes820 tonnesRecycledwasteTotalwasteWe consider both the potential need to adapt theorganisation’s activities and buildings and estates as aresult of climate change. Adaptation to climate changewill pose a challenge to both service delivery andinfrastructure in the future. It is therefore appropriatethat we consider it when planning how we will bestserve patients in the future.Sustainability issues are not yet included in our analysisof risks facing our organisation although we haveincluded sustainability risks within our risk register. <strong>NHS</strong>organisations have a statutory duty to assess the risksposed by climate change. Risk assessment, includingthe quantification and prioritisation of risk, is animportant part of managing complex organisations.For <strong>2012</strong>/<strong>13</strong> the trust board comprised:ChairmanMr Nigel McCorkellNon executive directorsDame Sally Powell (to 30 September <strong>2012</strong>)Ms Christine HigginsMrs Barbara KerinExecutive directorsMrs Barbara ByrneDirector of finance & information /deputy chief executiveMrs Jo Smith (from 1 May to 24 June <strong>2012</strong>)Acting director of financeDr Nicholas BroughtonMedical directorOur expenditure on waste in the last two yearswas incurred as follows:£1600001400001200001000008000060000400002000002011/12 <strong>2012</strong>/<strong>13</strong>Wasteincinerated/ energyfrom wasteWaste recycled/ reusedWaste sentto landfillOur organisation has an up todate sustainable developmentmanagement planHaving an up to date sustainable developmentmanagement plan is a good way to ensure that an<strong>NHS</strong> organisation fulfils its commitment to conductingall aspects of its activities with due consideration tosustainability, whilst providing high quality patient care.The <strong>NHS</strong> carbon reduction strategy asks for the boardsof all <strong>NHS</strong> organisations to approve such a plan.In addition to our focus on carbon, we are alsocommitted to reducing wider environmental and socialimpacts associated with the procurement of goodsand services. This will be set out within our policies onsustainable procurement.We plan to start work on calculating the carbonemissions associated goods and services we procure.Dr Nick Broughton, the trust’s medical director, is theboard level lead for sustainability. A board level leadfor sustainability ensures that sustainability issues havevisibility and ownership at the highest level of theorganisation.Sustainability issues, such as carbon reduction, arenot currently included in the job descriptions of allstaff. Our staff energy campaign is ongoing becausea sustainable <strong>NHS</strong> can only be delivered through theefforts of all staff.Our organisation has asustainable transport planOur transport plan supports both staff andpatients and continues to look for opportunities toencourage active travel to our sites.The <strong>NHS</strong> places a substantial burden on the transportinfrastructure, whether through patient, clinicianor other business activity. This generates an impacton air quality and greenhouse gas emissions. It istherefore important that we consider what steps areappropriate to reduce or change travel patterns.Mr Geoff RoseMr Neville ManuelMrs Lynne WeedallProfessor Lefkos MiddletonMs Carolyn Gray (from 18 March 20<strong>13</strong>)Chief executiveMr Peter Cubbon (to 30 April <strong>2012</strong>)Mrs Barbara Byrne (from 1 May to 24 June <strong>2012</strong>)Acting chief executiveMr Steve Shrubb (from 25 June <strong>2012</strong>)Mr Steve Trenchard (to 31 January 20<strong>13</strong>)Director of nursing & patient experienceDr Anne Aiyegbusi (from 1 February 20<strong>13</strong>)Interim director of nursing & patient experienceMiss Leeanne McGeeDirector of high secure servicesMr Andy WeirDirector of specialist & forensic servicesMs Jean GeorgeDirector of local servicesOther board directorsMr Nigel Leonard (to 19 October <strong>2012</strong>)Director of planning & corporate affairsMr Charles Allen (from 5 March <strong>2012</strong> to 31December <strong>2012</strong>) Interim director of organisationdevelopment & workforceMrs Rachael Moench (from 17 December <strong>2012</strong>)Director of organisation development & workforceThe chairman and non executive directors havebeen appointed by the secretary of state forhealth, in accordance with national proceduresfor appointments to such positions, for a term ofoffice that may vary from two years to four years.54 <strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>55
Board meetingsOur board held ten business meetings during<strong>2012</strong>/<strong>13</strong> which were open to the public, withagendas and papers available in advance, onour website.We also held an annual public meeting atwhich we presented our annual <strong>report</strong> andaccounts. Last year’s meeting was held on19 September <strong>2012</strong>.CommitteesTo support the work of the board, the trust’scommittee structure and membership is:Audit committeeMs Christine Higgins, chairMr Geoff RoseMr Neville ManuelMrs Lynne WeedallRemuneration committeeMr Nigel McCorkell, chairDame Sally Powell (to 30 September <strong>2012</strong>)Ms Christine HigginsMrs Barbara KerinMr Geoff RoseMr Neville ManuelMrs Lynne WeedallProfessor Lefkos MiddletonMs Carolyn Gray (from 18 March 20<strong>13</strong>)Charitable funds committeeMrs Barbara Kerin, chairMr Nigel McCorkellMs Christine HigginsMr Steve ShrubbMrs Barbara ByrneMs Rachael MoenchMr Steve Trenchard (to 31 January 20<strong>13</strong>)Dr Anne Aiyegbusi (from 1 February 20<strong>13</strong>)Dr Nicholas BroughtonQuality committeeMr Geoff Rose, chairProfessor Lefkos MiddletonMrs Barbara KerinDame Sally Powell (to 30 September <strong>2012</strong>)Dr Nicholas BroughtonMr Steve Trenchard (to 31 January 20<strong>13</strong>)Dr Anne Aiyegbusi (from 1 February 20<strong>13</strong>)Miss Leeanne McGeeMs Jean GeorgeMr Andy WeirIn addition, the following are also members:Dr Craig Richie, director of research anddevelopmentA service user representativeAll trust board members have an open invitationto attend the meetings of this committeeFinance & investment committeeMr Neville Manuel, chairMrs Lynne WeedallMs Christine HigginsMrs Barbara KerinMrs Barbara ByrneMiss Leeanne McGeeMs Jean GeorgeMr Andy WeirMr Nigel Leonard (to 19 October <strong>2012</strong>)In addition, the following are also members:Mr Eric Munro, director of capital, estatesand facilitiesMr Trevor Nelms, director of IM&TMrs Jo Smith, deputy director of financeA service user representativeAll trust board members have an open invitationto attend the meetings of this committee<strong>Mental</strong> health act managers’ committeeMr Geoff Rose, chairA number of lay people appointed as mentalhealth act managersAll non executive directors are eligible to bemembers of this committee<strong>Trust</strong> management teamMr Peter Cubbon (to 30 April <strong>2012</strong>)Mr Steve Shrubb (from 25 June <strong>2012</strong>)Mrs Barbara ByrneMrs Jo Smith (acting director of finance from 1May to 24 June <strong>2012</strong>)Dr Nicholas BroughtonMr Steve Trenchard (to 31 January 20<strong>13</strong>)Dr Anne Aiyegbusi (from 1 February 20<strong>13</strong>)Miss Leeanne McGeeMr Andy WeirMs Jean GeorgeMr Nigel Leonard (to 19 October <strong>2012</strong>)Mr Charles Allen (to 31 December <strong>2012</strong>)Mrs Rachael Moench (from 17 December <strong>2012</strong>)In addition, the following are also members:Dr Kevin Murray, clinical director, high secure servicesDr Michael Phelan, clinical director, local servicesDr Paul Gilluley (to 25 November <strong>2012</strong>), clinicaldirector, specialist and forensic servicesDr Claire Dimond, clinical director, specialist andforensic servicesMrs Helene Feger, director of communicationsand involvement56 <strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>57
Register of members’ interestsIt is a requirement that the chairman and all boardmembers should declare any conflicts of interestthat arise in the course of conducting <strong>NHS</strong> business.During the year, none of the trust board membersor parties related to any of them have undertakenany material transactions with <strong>West</strong> <strong>London</strong> <strong>Mental</strong><strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong>. As at 31 March 20<strong>13</strong>, thefollowing interests are registered.Each director states that as far as (s)he is awarethere is no relevant audit information of which the<strong>NHS</strong> body’s auditors are unaware and (s)he hastaken all the steps that (s)he ought to have takenas a director in order to make themselves aware ofany relevant audit information and establish thatthe <strong>NHS</strong> auditors are aware of it.Mr Nigel McCorkellnoneDame Sally Powell (until 30 September <strong>2012</strong>)Councillor, <strong>London</strong> Borough of Hammersmith& FulhamMs Christine HigginsnoneMrs Barbara KerinDirector & company secretary, Chiltern Citizens’Advice Bureau LtdMr Geoff RoseChief executive, Breakthrough Executive CoachingChair, Dimensions UKNon executive director, WaymarksShadow member of Barnet, Enfield & Haringey<strong>Mental</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong>Mr Neville ManuelGeneral manager, strategy, policy and portfolio,BT Group PLCMrs Lynne WeedallDirector, The Carphone Warehouse LimitedProfessor Lefkos MiddletononeMs Carolyn GraynoneMr Peter CubbonnoneMr Steve ShrubbnoneMrs Barbara ByrneCompany director, trustee & honorary treasurer,healthcare financial management association (HFMA)Husband works for Brent MINDDr Nicholas BroughtonnoneMr Steve TrenchardChair, International Society for thePsychological Treatments of Schizophrenias& Other Psychoses (ISPS UK)Dr Anne AiyegbusinoneMiss Leeanne McGeenoneMr Andy WeirnoneMs Jean GeorgenoneMrs Rachael MoenchnoneMr Nigel Leonard (to 19 October <strong>2012</strong>)noneMr Charles AllennoneResponsibilityExcellenceResponsibilityTogethernessCaringCaringExcellencTogetherness58<strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong>59
<strong>West</strong> <strong>London</strong> <strong>Mental</strong> <strong>Health</strong> <strong>NHS</strong> <strong>Trust</strong>,Uxbridge Road,Southall,Middlesex UB1 3EU020 8354 8354www.wlmht.nhs.uk@WLMHTFor alternative formats please contact the trust’sCommunications Department on 020 8354 8737Design by Lucid – www.lucidgraphics.co.uk