Annual report 2012-13 - West London Mental Health NHS Trust
Annual report 2012-13 - West London Mental Health NHS Trust
Annual report 2012-13 - West London Mental Health NHS Trust
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
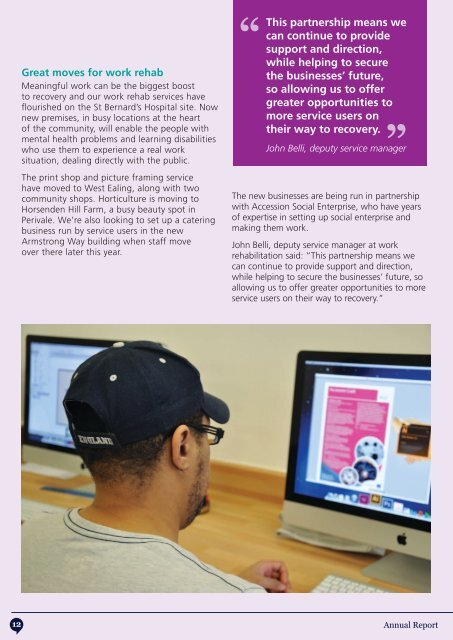
Great moves for work rehabMeaningful work can be the biggest boostto recovery and our work rehab services haveflourished on the St Bernard’s Hospital site. Nownew premises, in busy locations at the heartof the community, will enable the people withmental health problems and learning disabilitieswho use them to experience a real worksituation, dealing directly with the public.The print shop and picture framing servicehave moved to <strong>West</strong> Ealing, along with twocommunity shops. Horticulture is moving toHorsenden Hill Farm, a busy beauty spot inPerivale. We’re also looking to set up a cateringbusiness run by service users in the newArmstrong Way building when staff moveover there later this year.“This partnership means wecan continue to providesupport and direction,while helping to securethe businesses’ future,so allowing us to offergreater opportunities tomore service users ontheir way to recovery.“John Belli, deputy service managerThe new businesses are being run in partnershipwith Accession Social Enterprise, who have yearsof expertise in setting up social enterprise andmaking them work.John Belli, deputy service manager at workrehabilitation said: “This partnership means wecan continue to provide support and direction,while helping to secure the businesses’ future, soallowing us to offer greater opportunities to moreservice users on their way to recovery.”Helping from experiencePeer support workers are key to our recoveryapproach. Having experienced mental distressthemselves, they are well placed to work alongsideothers with similar stories, helping them to recoverby promoting hope and providing support basedon their common experience.Peer support workers are given training, and havetheir own personal supervisor throughout the course.Edward Dixon is the first paid peer supportworker with the early intervention team for clientsexperiencing their first episode of psychosis.“Service users are experts by experience,” he says.“We are making a move away from the patient/expert relationship. Our role is to act as coachesor mentors and enable the individual to take backcontrol of their lives and ownership of their illness.We can help to find and maintain hope until thatperson is able to maintain hope for themselves.“I feel that believing that I could do it made abig difference in my recovery. I had learned byexperience to embody my aspirations and keepmotivated, determined, and positive in order tosucceed as well as keeping the goals realistic. Thiszeal and enthusiasm is something I hope to sharewith everyone I work with.“Supporting mental healthin general hospitalsThis year we expanded our liaison psychiatry teamto provide more comprehensive services in the three<strong>London</strong> boroughs we cover. One aspect of liaisonpsychiatry services is to provide ageless (16+) specialistmental health care to patients in the general hospitalsetting, who have coinciding physical health andmental health problems. A person’s physical healthcan have a profound effect on their mental health (andvice versa), particularly for those people living with longterm physical ill-health. This year we developedinpatient liaison psychiatry pilot teams at EalingHospital and <strong>West</strong> Middlesex University Hospital, aswell as maintaining the pre-existing services we runat Charing Cross Hospital, Hammersmith and QueenCharlotte’s & Chelsea Hospital.Bruce Mamvura, team manager says: “I amenormously proud to currently manage the liaisonpsychiatry service at Ealing Hospital as I believe theseservices are in a unique position to make a positivedifference to the psychiatric care and treatment ofpatients within the general hospital setting.“This includes providing assessment and treatment topatients with long term chronic physical illnesses thatmay, for example, have also become depressed. Theteam’s work is very diverse and we are able to respondurgently to the care of any patients presenting withsignificant risks to them self or others, usually in A&E,as well as also extending support to elderly patientswith delirium and dementia. There is no greaterreward than to see patients recover quicker withimproved longer term outcomes, by receiving the rightintervention for their mental health needs, at the sametime as their physical healthcare.”In addition, this year, clinicians from our liaisonpsychiatry teams have been contributing to theintegrated care pilot in north west <strong>London</strong> (NWL). Thisinitiative aims to improve outcomes for patients withlong term conditions (such as diabetes, coronary heartdisease and chronic obstructive pulmonary disease),create access to better, more integrated care outsideof hospital, reduce unnecessary hospital admissionsand enable effective working of health and socialcare professionals across provider boundaries. In thismodel of care we see clinicians working together inmulti-disciplinary groups which include acute providers,general practice, community care, social care andmental health to provide collaborative and cohesivecare for patients with complex problems. Due tothe success of this pilot the work will continue to bedeveloped in the coming year.12<strong>Annual</strong> Report <strong>2012</strong>/20<strong>13</strong><strong>13</strong>