Eosinophilic Pustular Folliculitis (Ofuji Disease) Manifested ... - Cutis
Eosinophilic Pustular Folliculitis (Ofuji Disease) Manifested ... - Cutis
Eosinophilic Pustular Folliculitis (Ofuji Disease) Manifested ... - Cutis
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
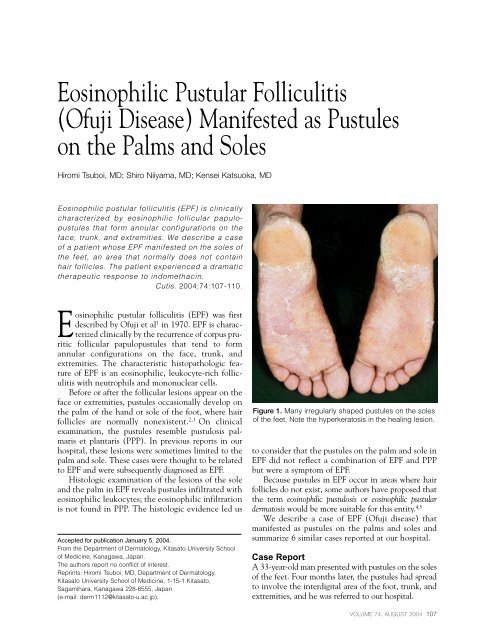
<strong>Eosinophilic</strong> <strong>Pustular</strong> <strong>Folliculitis</strong>(<strong>Ofuji</strong> <strong>Disease</strong>) <strong>Manifested</strong> as Pustuleson the Palms and SolesHiromi Tsuboi, MD; Shiro Niiyama, MD; Kensei Katsuoka, MD<strong>Eosinophilic</strong> pustular folliculitis (EPF) is clinicallycharacterized by eosinophilic follicular papulopustulesthat form annular configurations on theface, trunk, and extremities. We describe a caseof a patient whose EPF manifested on the soles ofthe feet, an area that normally does not containhair follicles. The patient experienced a dramatictherapeutic response to indomethacin.<strong>Cutis</strong>. 2004;74:107-110.<strong>Eosinophilic</strong> pustular folliculitis (EPF) was firstdescribed by <strong>Ofuji</strong> et al 1 in 1970. EPF is characterizedclinically by the recurrence of corpus pruriticfollicular papulopustules that tend to formannular configurations on the face, trunk, andextremities. The characteristic histopathologic featureof EPF is an eosinophilic, leukocyte-rich folliculitiswith neutrophils and mononuclear cells.Before or after the follicular lesions appear on theface or extremities, pustules occasionally develop onthe palm of the hand or sole of the foot, where hairfollicles are normally nonexistent. 2,3 On clinicalexamination, the pustules resemble pustulosis palmariset plantaris (PPP). In previous reports in ourhospital, these lesions were sometimes limited to thepalm and sole. These cases were thought to be relatedto EPF and were subsequently diagnosed as EPF.Histologic examination of the lesions of the soleand the palm in EPF reveals pustules infiltrated witheosinophilic leukocytes; the eosinophilic infiltrationis not found in PPP. The histologic evidence led usAccepted for publication January 5, 2004.From the Department of Dermatology, Kitasato University Schoolof Medicine, Kanagawa, Japan.The authors report no conflict of interest.Reprints: Hiromi Tsuboi, MD, Department of Dermatology,Kitasato University School of Medicine, 1-15-1 Kitasato,Sagamihara, Kanagawa 228-8555, Japan(e-mail: derm1112@kitasato-u.ac.jp).Figure 1. Many irregularly shaped pustules on the solesof the feet. Note the hyperkeratosis in the healing lesion.to consider that the pustules on the palm and sole inEPF did not reflect a combination of EPF and PPPbut were a symptom of EPF.Because pustules in EPF occur in areas where hairfollicles do not exist, some authors have proposed thatthe term eosinophilic pustulosis or eosinophilic pustulardermatosis would be more suitable for this entity. 4,5We describe a case of EPF (<strong>Ofuji</strong> disease) thatmanifested as pustules on the palms and soles andsummarize 6 similar cases reported at our hospital.Case ReportA 33-year-old man presented with pustules on the solesof the feet. Four months later, the pustules had spreadto involve the interdigital area of the foot, trunk, andextremities, and he was referred to our hospital.VOLUME 74, AUGUST 2004 107
<strong>Ofuji</strong> <strong>Disease</strong>Visual examination of the soles revealed numerouspustules, each with a red halo, 1 to 3 mm, roundto irregular, and slightly elevated (Figure 1). Manyfollicular papules the size of a half grain of rice werescattered within an egg-sized pigmentation area onthe trunk and extremities. An annular configurationwas not obvious (Figure 2).Histologic examination of the pustules on thesoles revealed subcorneal multilocular pustules,which were filled with neutrophils and eosinophilicleukocytes. Mild intracellular edema was observedaround the pustules. Emigration by eosinophilicleukocytes to the epidermis and infiltration into theupper dermis also were detected (Figure 3). Histologicexamination of trunk lesions showed spongiosisof the follicles infiltrated by lymphocytes andeosinophilic leukocytes (Figure 4).A diagnosis of EPF was made based on typicalclinical and histologic findings, and indomethacintreatment was prescribed. All eruptions cleared withoral administration of indomethacin 75 mg per dayfor 4 weeks. The eruption was subsequently controlledwith oral administration of minocycline andantiallergic drugs for 5 months.The Table summarizes the clinical histories of6 male patients treated at our hospital who werediagnosed with EPF based on the appearance of typicaleosinophilic pustules of the follicles on the face,trunk, and extremities.Figure 2. Red follicular papules the size of half grains ofrice scattered over the trunk.Figure 3. Subcornealpustules on the sole filledwith neutrophils andeosinophilic leukocytes(H&E, original magnification100).108 CUTIS ®
<strong>Ofuji</strong> <strong>Disease</strong>Characteristics of <strong>Eosinophilic</strong> <strong>Pustular</strong> <strong>Folliculitis</strong> <strong>Manifested</strong> as Pustulesof the Sole and Palm in 6 Male PatientsHistologicDuration AfterDistribution Features AppearanceAge, Initial of of Sole Treatment of Initialy Site Lesions Lesions Treatment Response Course Lesion43 Sole, Face, palm, Psoriatic, intradermal Steroid oint- Not Lost to 3 mointerdigital interdigital infiltration with ment and effective follow-uparea of area of eosinophilic antiallergicfoot hand leukocytes drugs for 1 y66 Sole, palm, None Intraepithelial Indomethacin Effective Treatmentinterdigital pustules infiltrated 75 mg for with indoareaof with eosinophilic 2 wk methacinfoot leukocytes and 50 mg forneutrophils3 y50 Sole Face, Not done Indomethacin Effective Controlled 9 yextremities, 75 mg for withpalm 4 wk indomethacinfor 4 wk. Lostto follow-up30 Sole Face, Intraepithelial Indomethacin Effective No recurrence 19 motrunk, pustules infiltrated 100 mg and for with indoextremitieswith eosinophilic minocycline 2 mo methacin andleukocytes and 200 mg minocyclineneutrophilsfor 1 y45 Sole Trunk, Not done Naproxen Effective Controlled 1 yextremities 300 mg and for 1 mo with naproxendiphenyland diphenylsulphonesulphone for75 mg 5 y. Lost tofollow-up33 Sole Trunk, Intraepithelial Indomethacin Effective Controlled with 4 moextremities, pustules infiltrated 75 mg and for 1 mo minocyclineinterdigital with eosinophilic minocycline for 5 mo.area of foot leukocytes and 100 mg Lost toneutrophilsfollow-upCommentEPF lesions are not always confined to hair follicles.In addition to the typical locations on theface, trunk, and extremities, these lesions also havebeen reported to occur on the palm and the sole. 2Aoyama and Tagami 3 reported that the skin lesionsbegan on the palms, soles, or both in 8% of theirEPF patients (18 male and 3 female). In theJapanese literature, 18% of EPF patients exhibitedpustules on the sole and palm. In a few cases, allthe pustules were palmoplantar lesions. 6The clinical appearance of the pustules on thesole and palm is similar to that of the lesions inPPP. If the lesions are limited to the sole and palm,either EPF or PPP is a possible diagnosis. Theappearance of typical follicular lesions on the face,trunk, or extremities rules out the diagnosis of PPPand confirms the diagnosis of EPF. Saruta andVOLUME 74, AUGUST 2004 109
<strong>Ofuji</strong> <strong>Disease</strong>eosinophilic leukocytes and neutrophils supportedthe diagnosis of EPF.The causes of EPF remain unknown; some caseshave been associated with fungal or bacterial infectionor immunologic disorders, 8 in particular, HIVinfection. 9 Three cases of EPF associated with drugsalso have been described. 10Systemic treatment with the cyclooxygenaseinhibitorindomethacin and other anti-inflammatorydrugs provides produces dramatic improvement inpatients with EPF. 11,12In conclusion, the palmoplantar lesions of EPFand PPP are difficult to differentiate by clinical differencesalone; however, histologic examinationcan reveal the eosinophilic pustules in the epidermisthat characterize EPF. The efficacy of oralindomethacin treatment is useful in the diagnosisof cases of EPF with palmoplantar lesions.Figure 4. Spongiosis of the follicular keratinocytes infiltratedwith lymphocytes and eosinophils on the trunk(H&E, original magnification 100).Nakamizo 7 reported some clinical characteristics ofEPF lesions that differentiate them from PPP. EPFlesions are larger than PPP lesions, and they tendto merge and display irregular margins. The surfacesof EPF lesions are erosive, and the pustulestend to be elevated and to invade interdigital areas.The clinical findings of the case reported here(pustules on the soles and palms) are similar tothose of PPP.Histologic examination of EPF lesions revealsmultilocular, subcorneal, and intraepidermal pustulesfilled with numerous eosinophilic leukocytesand neutrophils. Other histologic features includeperivascular infiltration of eosinophilic leukocytesinto the upper dermis and their emigration to theepidermis. In contrast, subcorneal monolocularneutrophilic pustules are indicative of PPP. In ourpatient’s case, the presence of subcorneal, intraepidermal,multilocular pustules containing numerousREFERENCES1. <strong>Ofuji</strong> S, Ogino A, Horio T, et al. <strong>Eosinophilic</strong> pustularfolliculitis. Acta Derm Venereol. 1970;50:195-203.2. Takematsu H, Nakamura K, Igarasi M, et al. <strong>Eosinophilic</strong>pustular folliculitis: report of two cases with a review of theJapanese literature. Arch Dermatol. 1985;121:917-920.3. Aoyama H, Tagami H. <strong>Eosinophilic</strong> pustular folliculitisstarting initially only with palmoplantar pustular lesions.Dermatology. 1992;185:276-280.4. Vakilzadeh F, Sauter L, Knop J, et al. <strong>Eosinophilic</strong> pustulosiswith pemphigus-like antibody. Dermatologica.1981;162:265-272.5. Orfans CE, Sterry W. Sterile eosinophilic pustulose.Dermatologica. 1978;157:193-205.6. Adachi Y, Ishikawa H, Hattori A. Two cases of eosinophilicpustular folliculitis. Rinsho Derma. 1982;36:213-219.7. Saruta T, Nakamizo Y. <strong>Eosinophilic</strong> pustularfolliculitis–particularly with reference to lesions on thepalm of the hand and sole of the foot. J Dermatol.1980;7:239-246.8. Haupt HM, Stern JB, Weber CB. <strong>Eosinophilic</strong> pustular folliculitis:fungal folliculitis? J Am Acad Dermatol.1990;23:1012-1014.9. Basarab T, Russell Jones R. HIV-associated eosinophilicfolliculitis: case report and review of the literature. Br JDermatol. 1996;134:499-503.10. Maejima H, Mukai H, Eto H. <strong>Eosinophilic</strong> pustular folliculitisinduced by allopurinol and timepidium bromide. ActaDerm Venereol. 2002;82:316-317.11. Youn CS, Cho KH. <strong>Eosinophilic</strong> pustular folliculitis treatedwith naproxen. Br J Dermatol. 2001;145:514-515.12. Ota T, Hata Y, Tanikawa A, et al. <strong>Eosinophilic</strong> pustular folliculitis(<strong>Ofuji</strong>’s disease): indomethacin as a first choice oftreatment. Clin Exp Dermatol. 2001;26:179-181.110 CUTIS ®