Facilitating Cross-National Comparisons of Indicators for Patient ...
Facilitating Cross-National Comparisons of Indicators for Patient ...
Facilitating Cross-National Comparisons of Indicators for Patient ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
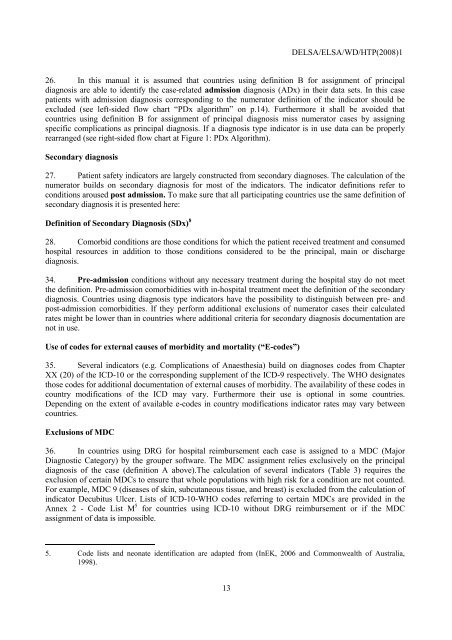
DELSA/ELSA/WD/HTP(2008)126. In this manual it is assumed that countries using definition B <strong>for</strong> assignment <strong>of</strong> principaldiagnosis are able to identify the case-related admission diagnosis (ADx) in their data sets. In this casepatients with admission diagnosis corresponding to the numerator definition <strong>of</strong> the indicator should beexcluded (see left-sided flow chart “PDx algorithm” on p.14). Furthermore it shall be avoided thatcountries using definition B <strong>for</strong> assignment <strong>of</strong> principal diagnosis miss numerator cases by assigningspecific complications as principal diagnosis. If a diagnosis type indicator is in use data can be properlyrearranged (see right-sided flow chart at Figure 1: PDx Algorithm).Secondary diagnosis27. <strong>Patient</strong> safety indicators are largely constructed from secondary diagnoses. The calculation <strong>of</strong> thenumerator builds on secondary diagnosis <strong>for</strong> most <strong>of</strong> the indicators. The indicator definitions refer toconditions aroused post admission. To make sure that all participating countries use the same definition <strong>of</strong>secondary diagnosis it is presented here:Definition <strong>of</strong> Secondary Diagnosis (SDx) 828. Comorbid conditions are those conditions <strong>for</strong> which the patient received treatment and consumedhospital resources in addition to those conditions considered to be the principal, main or dischargediagnosis.34. Pre-admission conditions without any necessary treatment during the hospital stay do not meetthe definition. Pre-admission comorbidities with in-hospital treatment meet the definition <strong>of</strong> the secondarydiagnosis. Countries using diagnosis type indicators have the possibility to distinguish between pre- andpost-admission comorbidities. If they per<strong>for</strong>m additional exclusions <strong>of</strong> numerator cases their calculatedrates might be lower than in countries where additional criteria <strong>for</strong> secondary diagnosis documentation arenot in use.Use <strong>of</strong> codes <strong>for</strong> external causes <strong>of</strong> morbidity and mortality (“E-codes”)35. Several indicators (e.g. Complications <strong>of</strong> Anaesthesia) build on diagnoses codes from ChapterXX (20) <strong>of</strong> the ICD-10 or the corresponding supplement <strong>of</strong> the ICD-9 respectively. The WHO designatesthose codes <strong>for</strong> additional documentation <strong>of</strong> external causes <strong>of</strong> morbidity. The availability <strong>of</strong> these codes incountry modifications <strong>of</strong> the ICD may vary. Furthermore their use is optional in some countries.Depending on the extent <strong>of</strong> available e-codes in country modifications indicator rates may vary betweencountries.Exclusions <strong>of</strong> MDC36. In countries using DRG <strong>for</strong> hospital reimbursement each case is assigned to a MDC (MajorDiagnostic Category) by the grouper s<strong>of</strong>tware. The MDC assignment relies exclusively on the principaldiagnosis <strong>of</strong> the case (definition A above).The calculation <strong>of</strong> several indicators (Table 3) requires theexclusion <strong>of</strong> certain MDCs to ensure that whole populations with high risk <strong>for</strong> a condition are not counted.For example, MDC 9 (diseases <strong>of</strong> skin, subcutaneous tissue, and breast) is excluded from the calculation <strong>of</strong>indicator Decubitus Ulcer. Lists <strong>of</strong> ICD-10-WHO codes referring to certain MDCs are provided in theAnnex 2 - Code List M 5 <strong>for</strong> countries using ICD-10 without DRG reimbursement or if the MDCassignment <strong>of</strong> data is impossible.5. Code lists and neonate identification are adapted from (InEK, 2006 and Commonwealth <strong>of</strong> Australia,1998).13






![Successful Ministry to the Retarded[ETowns] - Elmer Towns](https://img.yumpu.com/47721906/1/190x252/successful-ministry-to-the-retardedetowns-elmer-towns.jpg?quality=85)