Essential Revision Notes for MRCP Third Edition - PasTest
Essential Revision Notes for MRCP Third Edition - PasTest
Essential Revision Notes for MRCP Third Edition - PasTest
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
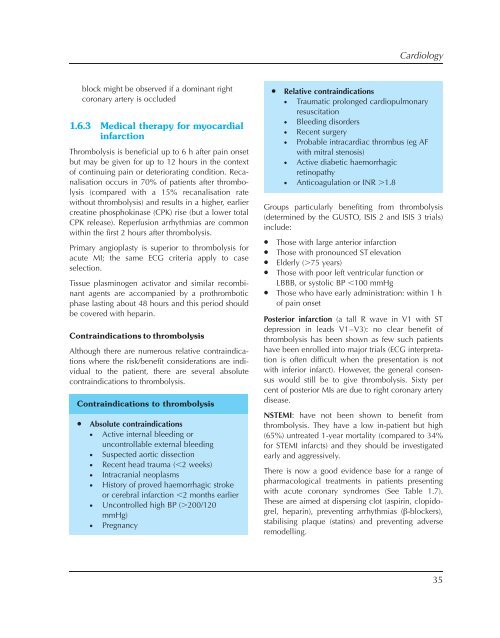
Cardiologyblock might be observed if a dominant rightcoronary artery is occluded1.6.3 Medical therapy <strong>for</strong> myocardialinfarctionThrombolysis is beneficial up to 6 h after pain onsetbut may be given <strong>for</strong> up to 12 hours in the contextof continuing pain or deteriorating condition. Recanalisationoccurs in 70% of patients after thrombolysis(compared with a 15% recanalisation ratewithout thrombolysis) and results in a higher, earliercreatine phosphokinase (CPK) rise (but a lower totalCPK release). Reperfusion arrhythmias are commonwithin the first 2 hours after thrombolysis.Primary angioplasty is superior to thrombolysis <strong>for</strong>acute MI; the same ECG criteria apply to caseselection.Tissue plasminogen activator and similar recombinantagents are accompanied by a prothromboticphase lasting about 48 hours and this period shouldbe covered with heparin.Contraindications to thrombolysisAlthough there are numerous relative contraindicationswhere the risk/benefit considerations are individualto the patient, there are several absolutecontraindications to thrombolysis.Contraindications to thrombolysis• Absolute contraindications• Active internal bleeding oruncontrollable external bleeding• Suspected aortic dissection• Recent head trauma (,2 weeks)• Intracranial neoplasms• History of proved haemorrhagic strokeor cerebral infarction ,2 months earlier• Uncontrolled high BP (.200/120mmHg)• Pregnancy• Relative contraindications• Traumatic prolonged cardiopulmonaryresuscitation• Bleeding disorders• Recent surgery• Probable intracardiac thrombus (eg AFwith mitral stenosis)• Active diabetic haemorrhagicretinopathy• Anticoagulation or INR .1.8Groups particularly benefiting from thrombolysis(determined by the GUSTO, ISIS 2 and ISIS 3 trials)include:• Those with large anterior infarction• Those with pronounced ST elevation• Elderly (.75 years)• Those with poor left ventricular function orLBBB, or systolic BP ,100 mmHg• Those who have early administration: within 1 hof pain onsetPosterior infarction (a tall R wave in V1 with STdepression in leads V1–V3): no clear benefit ofthrombolysis has been shown as few such patientshave been enrolled into major trials (ECG interpretationis often difficult when the presentation is notwith inferior infarct). However, the general consensuswould still be to give thrombolysis. Sixty percent of posterior MIs are due to right coronary arterydisease.NSTEMI: have not been shown to benefit fromthrombolysis. They have a low in-patient but high(65%) untreated 1-year mortality (compared to 34%<strong>for</strong> STEMI infarcts) and they should be investigatedearly and aggressively.There is now a good evidence base <strong>for</strong> a range ofpharmacological treatments in patients presentingwith acute coronary syndromes (See Table 1.7).These are aimed at dispersing clot (aspirin, clopidogrel,heparin), preventing arrhythmias (â-blockers),stabilising plaque (statins) and preventing adverseremodelling.35