Medical Management Guide, 2009, Version 3.0 - Tricare
Medical Management Guide, 2009, Version 3.0 - Tricare
Medical Management Guide, 2009, Version 3.0 - Tricare
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
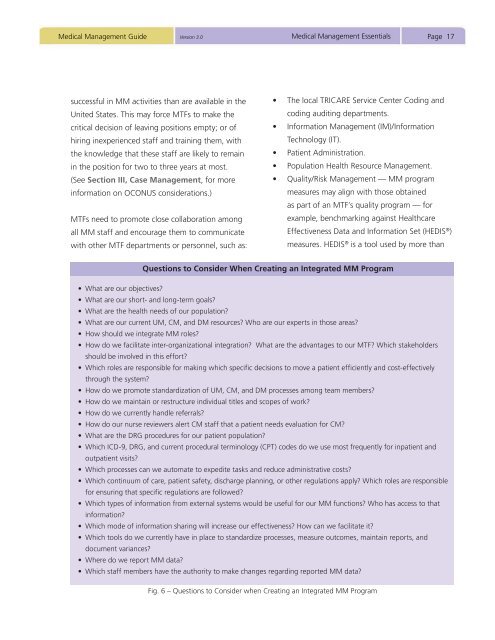
<strong>Medical</strong> <strong>Management</strong> <strong>Guide</strong> <strong>Version</strong> <strong>3.0</strong><strong>Medical</strong> <strong>Management</strong> EssentialsPage 17successful in MM activities than are available in theUnited States. This may force MTFs to make thecritical decision of leaving positions empty; or ofhiring inexperienced staff and training them, withthe knowledge that these staff are likely to remainin the position for two to three years at most.(See Section III, Case <strong>Management</strong>, for moreinformation on OCONUS considerations.)MTFs need to promote close collaboration amongall MM staff and encourage them to communicatewith other MTF departments or personnel, such as:• The local TRICARE Service Center Coding andcoding auditing departments.• Information <strong>Management</strong> (IM)/InformationTechnology (IT).• Patient Administration.• Population Health Resource <strong>Management</strong>.• Quality/Risk <strong>Management</strong> — MM programmeasures may align with those obtainedas part of an MTF’s quality program — forexample, benchmarking against HealthcareEffectiveness Data and Information Set (HEDIS ® )measures. HEDIS ® is a tool used by more thanQuestions to Consider When Creating an Integrated MM Program• What are our objectives?• What are our short- and long-term goals?• What are the health needs of our population?• What are our current UM, CM, and DM resources? Who are our experts in those areas?• How should we integrate MM roles?• How do we facilitate inter-organizational integration? What are the advantages to our MTF? Which stakeholdersshould be involved in this effort?• Which roles are responsible for making which specific decisions to move a patient efficiently and cost-effectivelythrough the system?• How do we promote standardization of UM, CM, and DM processes among team members?• How do we maintain or restructure individual titles and scopes of work?• How do we currently handle referrals?• How do our nurse reviewers alert CM staff that a patient needs evaluation for CM?• What are the DRG procedures for our patient population?• Which ICD-9, DRG, and current procedural terminology (CPT) codes do we use most frequently for inpatient andoutpatient visits?• Which processes can we automate to expedite tasks and reduce administrative costs?• Which continuum of care, patient safety, discharge planning, or other regulations apply? Which roles are responsiblefor ensuring that specific regulations are followed?• Which types of information from external systems would be useful for our MM functions? Who has access to thatinformation?• Which mode of information sharing will increase our effectiveness? How can we facilitate it?• Which tools do we currently have in place to standardize processes, measure outcomes, maintain reports, anddocument variances?• Where do we report MM data?• Which staff members have the authority to make changes regarding reported MM data?Fig. 6 – Questions to Consider when Creating an Integrated MM Program