National best practice and evidence based guidelines for wound ...
National best practice and evidence based guidelines for wound ...
National best practice and evidence based guidelines for wound ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
3.5 Guidelines <strong>for</strong> the prevention <strong>and</strong> management of Diabetic foot ulceration<br />
Introduction<br />
The basic principles of prevention <strong>and</strong> management of diabetic foot ulceration described here are <strong>based</strong><br />
on the international consensus <strong>and</strong> practical <strong>guidelines</strong> on the management <strong>and</strong> prevention of<br />
the diabetic foot (IWGDF 2007). They are aimed at health care workers involved in the care of people<br />
with diabetes. It should be noted that the full set of <strong>guidelines</strong> are available through the International<br />
Working Group on Diabetic Foot (www.iwgdf.org).<br />
This section is divided into two distinct parts:<br />
Part A deals with the non-ulcerated limb<br />
Part B deals with the ulcerated limb<br />
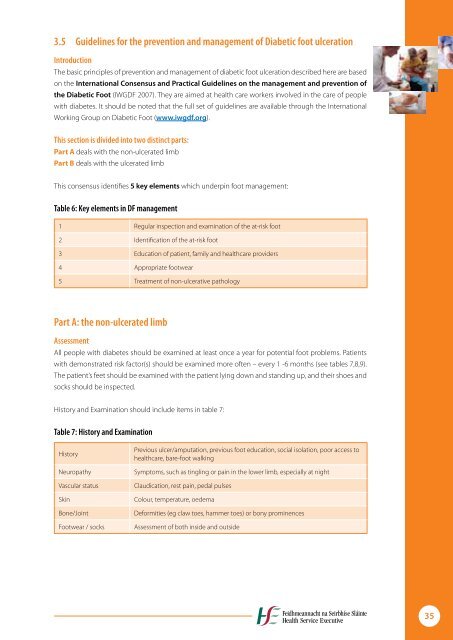
This consensus identifies 5 key elements which underpin foot management:<br />
Table 6: Key elements in DF management<br />
1 Regular inspection <strong>and</strong> examination of the at-risk foot<br />
2 Identification of the at-risk foot<br />
3 Education of patient, family <strong>and</strong> healthcare providers<br />
4 Appropriate footwear<br />
5 Treatment of non-ulcerative pathology<br />
Part A: the non-ulcerated limb<br />
Assessment<br />
All people with diabetes should be examined at least once a year <strong>for</strong> potential foot problems. Patients<br />
with demonstrated risk factor(s) should be examined more often – every 1 -6 months (see tables 7,8,9).<br />
The patient’s feet should be examined with the patient lying down <strong>and</strong> st<strong>and</strong>ing up, <strong>and</strong> their shoes <strong>and</strong><br />
socks should be inspected.<br />
History <strong>and</strong> Examination should include items in table 7:<br />
Table 7: History <strong>and</strong> Examination<br />
History<br />
Previous ulcer/amputation, previous foot education, social isolation, poor access to<br />
healthcare, bare-foot walking<br />
Neuropathy Symptoms, such as tingling or pain in the lower limb, especially at night<br />
Vascular status Claudication, rest pain, pedal pulses<br />
Skin Colour, temperature, oedema<br />
Bone/Joint De<strong>for</strong>mities (eg claw toes, hammer toes) or bony prominences<br />
Footwear / socks Assessment of both inside <strong>and</strong> outside<br />
35