non-newtonian effects of pulsatile blood flow in a realistic bypass ...
non-newtonian effects of pulsatile blood flow in a realistic bypass ...
non-newtonian effects of pulsatile blood flow in a realistic bypass ...
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
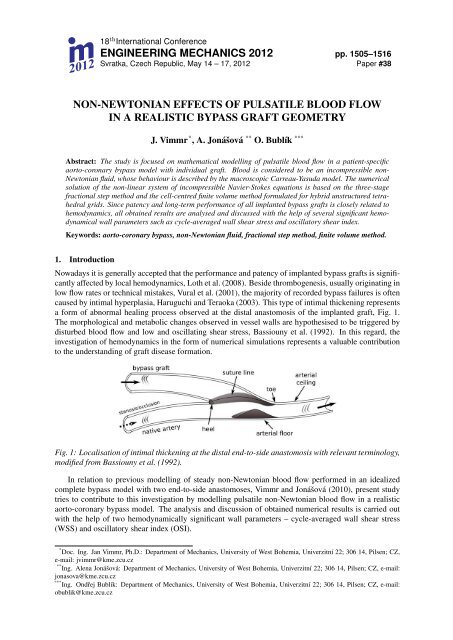
. 18m 2012th International ConferenceENGINEERING MECHANICS 2012 pp. 1505–1516Svratka, Czech Republic, May 14 – 17, 2012 Paper #38NON-NEWTONIAN EFFECTS OF PULSATILE BLOOD FLOWIN A REALISTIC BYPASS GRAFT GEOMETRYJ. Vimmr * , A. Jonášová ** O. Bublík ***Abstract: The study is focused on mathematical modell<strong>in</strong>g <strong>of</strong> <strong>pulsatile</strong> <strong>blood</strong> <strong>flow</strong> <strong>in</strong> a patient-specificaorto-coronary <strong>bypass</strong> model with <strong>in</strong>dividual graft. Blood is considered to be an <strong>in</strong>compressible <strong>non</strong>-Newtonian fluid, whose behaviour is described by the macroscopic Carreau-Yasuda model. The numericalsolution <strong>of</strong> the <strong>non</strong>-l<strong>in</strong>ear system <strong>of</strong> <strong>in</strong>compressible Navier-Stokes equations is based on the three-stagefractional step method and the cell-centred f<strong>in</strong>ite volume method formulated for hybrid unstructured tetrahedralgrids. S<strong>in</strong>ce patency and long-term performance <strong>of</strong> all implanted <strong>bypass</strong> grafts is closely related tohemodynamics, all obta<strong>in</strong>ed results are analysed and discussed with the help <strong>of</strong> several significant hemodynamicalwall parameters such as cycle-averaged wall shear stress and oscillatory shear <strong>in</strong>dex.Keywords: aorto-coronary <strong>bypass</strong>, <strong>non</strong>-Newtonian fluid, fractional step method, f<strong>in</strong>ite volume method.1. IntroductionNowadays it is generally accepted that the performance and patency <strong>of</strong> implanted <strong>bypass</strong> grafts is significantlyaffected by local hemodynamics, Loth et al. (2008). Beside thrombogenesis, usually orig<strong>in</strong>at<strong>in</strong>g <strong>in</strong>low <strong>flow</strong> rates or technical mistakes, Vural et al. (2001), the majority <strong>of</strong> recorded <strong>bypass</strong> failures is <strong>of</strong>tencaused by <strong>in</strong>timal hyperplasia, Haruguchi and Teraoka (2003). This type <strong>of</strong> <strong>in</strong>timal thicken<strong>in</strong>g representsa form <strong>of</strong> abnormal heal<strong>in</strong>g process observed at the distal anastomosis <strong>of</strong> the implanted graft, Fig. 1.The morphological and metabolic changes observed <strong>in</strong> vessel walls are hypothesised to be triggered bydisturbed <strong>blood</strong> <strong>flow</strong> and low and oscillat<strong>in</strong>g shear stress, Bassiouny et al. (1992). In this regard, the<strong>in</strong>vestigation <strong>of</strong> hemodynamics <strong>in</strong> the form <strong>of</strong> numerical simulations represents a valuable contributionto the understand<strong>in</strong>g <strong>of</strong> graft disease formation.Fig. 1: Localisation <strong>of</strong> <strong>in</strong>timal thicken<strong>in</strong>g at the distal end-to-side anastomosis with relevant term<strong>in</strong>ology,modified from Bassiouny et al. (1992).In relation to previous modell<strong>in</strong>g <strong>of</strong> steady <strong>non</strong>-Newtonian <strong>blood</strong> <strong>flow</strong> performed <strong>in</strong> an idealizedcomplete <strong>bypass</strong> model with two end-to-side anastomoses, Vimmr and Jonášová (2010), present studytries to contribute to this <strong>in</strong>vestigation by modell<strong>in</strong>g <strong>pulsatile</strong> <strong>non</strong>-Newtonian <strong>blood</strong> <strong>flow</strong> <strong>in</strong> a <strong>realistic</strong>aorto-coronary <strong>bypass</strong> model. The analysis and discussion <strong>of</strong> obta<strong>in</strong>ed numerical results is carried outwith the help <strong>of</strong> two hemodynamically significant wall parameters – cycle-averaged wall shear stress(WSS) and oscillatory shear <strong>in</strong>dex (OSI).* Doc. Ing. Jan Vimmr, Ph.D.: Department <strong>of</strong> Mechanics, University <strong>of</strong> West Bohemia, Univerzitní 22; 306 14, Pilsen; CZ,e-mail: jvimmr@kme.zcu.cz** Ing. Alena Jonášová: Department <strong>of</strong> Mechanics, University <strong>of</strong> West Bohemia, Univerzitní 22; 306 14, Pilsen; CZ, e-mail:jonasova@kme.zcu.cz*** Ing. Ondřej Bublík: Department <strong>of</strong> Mechanics, University <strong>of</strong> West Bohemia, Univerzitní 22; 306 14, Pilsen; CZ, e-mail:obublik@kme.zcu.cz
1506 Eng<strong>in</strong>eer<strong>in</strong>g Mechanics 2012, #382. Problem formulationThe ma<strong>in</strong> objective <strong>of</strong> this study is the analysis <strong>of</strong> hemodynamics <strong>in</strong> an <strong>in</strong>dividual aorto-coronary <strong>bypass</strong>graft. In cardiovascular surgery, the term <strong>in</strong>dividual denotes a vascular graft with one distal end-to-sideanastomosis, i.e., the graft provides a direct connection between the aorta and the stenosed or occludedcoronary artery. The <strong>bypass</strong> model considered <strong>in</strong> this study is reconstructed from CT data provided by thecourtesy <strong>of</strong> the University Hospital <strong>in</strong> Pilsen, Czech Republic. The reconstruction process and computationalmesh generation are carried out <strong>in</strong> s<strong>of</strong>tware packages Amira and Altair Hypermesh, respectively.An example <strong>of</strong> primary reconstruction <strong>of</strong> the chest region and <strong>of</strong> the <strong>in</strong>dividual <strong>bypass</strong> graft is shown<strong>in</strong> Fig. 2. The f<strong>in</strong>al shape <strong>of</strong> the <strong>bypass</strong> model after smooth<strong>in</strong>g is displayed <strong>in</strong> Fig. 3. The unstructuredcomputational mesh used for all numerical simulations consists <strong>of</strong> 362,437 tetrahedral cells.Fig. 2: CT reconstruction <strong>of</strong> the chest region (left) and <strong>of</strong> the aorto-coronary <strong>bypass</strong> graft (right)For the purpose <strong>of</strong> <strong>blood</strong> <strong>flow</strong> simulations <strong>in</strong> the prepared <strong>in</strong>dividual graft, we choose an approachsimilar to that found <strong>in</strong> other studies published to the theme <strong>of</strong> <strong>bypass</strong> hemodynamics, see the reviewpaper Loth et al. (2008). Firstly, tak<strong>in</strong>g <strong>in</strong>to account the fact that at the end <strong>of</strong> the arterialisation process,venous grafts lose their compliance, all the <strong>bypass</strong> walls are, <strong>in</strong> this study, modelled as impermeable andrigid, <strong>in</strong>clud<strong>in</strong>g the wall <strong>of</strong> the aorta. In the light <strong>of</strong> this simplification, we are aware that the neglectedaortic elasticity represents a considerable limitation <strong>of</strong> the present study. We hope to rectify it <strong>in</strong> one <strong>of</strong>our future projects by solv<strong>in</strong>g the fluid-structure <strong>in</strong>teraction problem. In this study, we further assume astatic aorto-coronary <strong>bypass</strong> model, i.e., the impact <strong>of</strong> heart beat<strong>in</strong>g is not considered. This assumptionis based on the f<strong>in</strong>d<strong>in</strong>gs published <strong>in</strong> Zeng et al. (2003), where it was shown that the arterial motiondoes not significantly affect <strong>blood</strong> <strong>flow</strong> <strong>in</strong> the case <strong>of</strong> <strong>flow</strong> pulsatility. In order to model <strong>blood</strong>’s complexrheological properties, we <strong>in</strong>troduce the macroscopic <strong>non</strong>-Newtonian Carreau-Yasuda model, which wehave successfully applied <strong>in</strong> our previous simulations, Vimmr and Jonášová (2010),η( ˙γ) = η ∞ + (η 0 − η ∞ )[1 + ( λ ˙γ ) ] a n−1a, (1)where η 0 and η ∞ are the zero and <strong>in</strong>f<strong>in</strong>ite shear viscosities, respectively, λ is the characteristic relaxationtime and n is the <strong>flow</strong> <strong>in</strong>dex. The five parameters occurr<strong>in</strong>g <strong>in</strong> the Carreau-Yasuda model (1) maybe determ<strong>in</strong>ed by numerical fitt<strong>in</strong>g <strong>of</strong> experimental data. In this study, we adopt data mentioned <strong>in</strong>Cho and Kensey (1991): η ∞ = 3.45 · 10 −3 Pa · s, η 0 = 56 · 10 −3 Pa · s, λ = 1.902 s, a = 1.25,n = 0.22. The shear rate is given as ˙γ = 2 √ D II , where D II denotes the second <strong>in</strong>variant <strong>of</strong> the rate <strong>of</strong>deformation tensor D = 1 (2 ∇v + (∇v)T ) . For the <strong>in</strong>compressible fluid, the second <strong>in</strong>variant is def<strong>in</strong>edas D II = 1 2 d ijd ij , i, j = 1, 2, 3, where d ij are the components <strong>of</strong> the rate <strong>of</strong> deformation tensor D. Forthe Newtonian <strong>flow</strong>, the molecular viscosity is kept constant and equal to <strong>in</strong>f<strong>in</strong>ite shear viscosity η ∞ .F<strong>in</strong>ally, note that the coronary arteries shown <strong>in</strong> Fig. 3 are considered to be occluded (with no <strong>in</strong><strong>flow</strong>) sothat the only relevant <strong>in</strong>com<strong>in</strong>g <strong>flow</strong> will be that <strong>of</strong> the <strong>bypass</strong> graft.
Vimmr J., Jonášová A., Bublík O. 1507Fig. 3: Individual graft – unstructured computational mesh and relevant term<strong>in</strong>ology3. Mathematical modelLet us consider a time <strong>in</strong>terval (0, T ), T > 0 and a bounded three-dimensional computational doma<strong>in</strong>Ω ⊂ R 3 with boundary ∂Ω = ∂Ω I ∪ ∂Ω O ∪ ∂Ω W , where ∂Ω I , ∂Ω O and ∂Ω W denote the <strong>in</strong>let, theoutlet and the walls <strong>of</strong> the computational doma<strong>in</strong>, respectively. In this study, coronary <strong>blood</strong> <strong>flow</strong> ismodelled as unsteady lam<strong>in</strong>ar isothermal <strong>flow</strong> <strong>of</strong> <strong>in</strong>compressible generalised Newtonian fluid that <strong>in</strong> thespace-time cyl<strong>in</strong>der Ω T = Ω × (0, T ) is mathematically described by the <strong>non</strong>-l<strong>in</strong>ear system <strong>of</strong> <strong>in</strong>compressibleNavier-Stokes (NS) equations written <strong>in</strong> the <strong>non</strong>-dimensional form∂v i= 0 , (2)∂x i∂v i∂t + ∂ (v i v j ) + ∂p = 1 [ (∂ ∂viη( ˙γ) + ∂v )]jfor i, j = 1, 2, 3 , (3)∂x j ∂x i Re ∂x j ∂x j ∂x iwhere t ∈ (0, T ) is the time, v i is the i-th component <strong>of</strong> the velocity vector v = [v 1 , v 2 , v 3 ] T correspond<strong>in</strong>gto the Cartesian component x i <strong>of</strong> the space variables vector x = [x 1 , x 2 , x 3 ] T ∈ Ω, p is the pressure,Re is the reference Reynolds number and η( ˙γ) is the shear-dependent viscosity given by Eq. (1).All variables appear<strong>in</strong>g <strong>in</strong> Eqs. (2) – (3) are <strong>non</strong>-dimensionalized by the reference velocity U ref > 0and characteristic length D ref > 0. For the <strong>bypass</strong> model considered <strong>in</strong> this study, the characteristiclength value was chosen to be equal to the aorta diameter D ref ≡ D (A) = 0.036 m and the referencevelocity is stated as U ref = 4Q 0 /(π Dref 2 ) = 0.1592 m · s−1 , where average aortic <strong>in</strong>let <strong>flow</strong> rate isQ 0 = 112.56 · 10 −6 m 3 · s −1 , see Fig. 6 (left). As for the reference Reynolds number, it is determ<strong>in</strong>edas Re = U ref D ref ϱ/η ref = 1 744.3, where ϱ = 1050 kg · m −3 and η ref ≡ η ∞ = 3.45 · 10 −3 Pa · s.For the sake <strong>of</strong> completeness, reference pressure and reference time are computed as p ref = ϱ Uref 2 andt ref = D ref /U ref , respectively.4. Numerical methodThe numerical solution <strong>of</strong> the <strong>non</strong>-l<strong>in</strong>ear time-dependent system <strong>of</strong> <strong>in</strong>compressible NS equations (2) –(3) is based on the projection method. In this study, the computation <strong>of</strong> velocity components v<strong>in</strong>+1 , whichsatisfy the divergence-free condition (2), employs the three-stage fractional step scheme, Ferziger andPerić (1999). In the first stage, <strong>in</strong>termediate velocity components vi ∗ are explicitly computed from theconvective part <strong>of</strong> the NS equation (3) asv ∗ i − vn i∆t+ ∂∂x j(v n i v n j ) = 0 , i, j = 1, 2, 3 . (4)
1508 Eng<strong>in</strong>eer<strong>in</strong>g Mechanics 2012, #38For the second stage <strong>of</strong> the fractional step scheme, the <strong>in</strong>termediate velocity components ˆv i are computedapply<strong>in</strong>g the unconditionally stable implicit Crank-Nicolson scheme to the viscous term <strong>of</strong> Eq. (3)ˆv i − vi∗ = 1 [ (∂ ∂(ˆvi + vi ∗ η( ˙γ)) + ∂(ˆv j + vj ∗))], i, j = 1, 2, 3. (5)∆t 2Re ∂x j ∂x j ∂x iLet us l<strong>in</strong>earise the shear-dependent dynamic viscosity η( ˙γ) as η( ˙γ) = η( ˙γ(v ∗ )) and <strong>in</strong>troduce an auxil-(iary variable d ij = 1 ∂vi2 ∂x j+ ∂v j∂x i), which <strong>in</strong> this case is equal to the components <strong>of</strong> the rate <strong>of</strong> deformationtensor D mentioned <strong>in</strong> section 2. Then Eq. (5) can be rewritten as a system <strong>of</strong> two l<strong>in</strong>ear equationsˆv i − v ∗ i∆t= 1 ∂[ (η( ˙γ) ˆdij + dRe ∂xij)]∗ , (6)jˆd ij = 1 ( ∂ˆvi+ ∂ˆv )j. (7)2 ∂x j ∂x iIn the third stage, pressure is used for the projection <strong>of</strong> the <strong>in</strong>termediate velocity vector ˆv onto a space<strong>of</strong> divergence-free velocity field to get the values <strong>of</strong> velocity and pressure at the next time level (n + 1).Hence, the velocity components v<strong>in</strong>+1 are computed fromv n+1i− ˆv i∆twhere p n+1 is computed from the Poisson equation for pressure+ ∂pn+1∂x i= 0 , i = 1, 2, 3, (8)∂ 2 p n+1= 1 ∂ˆv i. (9)∂x i ∂x i ∆t ∂x iIt can be easily shown that sum <strong>of</strong> Eqs. (4), (5) and (8) yields the approximation <strong>of</strong> NS equations <strong>of</strong>first order time accuracy. F<strong>in</strong>ally, the whole algorithm <strong>of</strong> the fractional step method may be written fori, j = 1, 2, 3 as followsˆv i∆t − 1 Rev ∗ i∂(η( ˙γ)∂x ˆd)ijjˆd ij − 1 ( ∂ˆvi+ ∂ˆv )j2 ∂x j ∂x i= v n i − ∆t∂ 2 p n+1∂x i ∂x i= 1 ∆tv n+1i= v∗ i∆t + 1 Re∂ (vn∂x i v n )j , (10)j∂∂x j(η( ˙γ) d∗ij), (11)= 0 , (12)∂ˆv i∂x i, (13)= ˆv i − ∆t ∂pn+1∂x i. (14)The space discretization <strong>of</strong> the system <strong>of</strong> Eqs. (10) – (14) is performed us<strong>in</strong>g the cell-centred f<strong>in</strong>itevolume method for hybrid unstructured tetrahedral grids. The idea <strong>of</strong> apply<strong>in</strong>g the hybrid unstructuredgrid for the numerical solution <strong>of</strong> time-dependent <strong>in</strong>compressible NS equations <strong>in</strong> 2D was <strong>in</strong>troduced <strong>in</strong>Kim and Choi (2000). The pr<strong>in</strong>ciple <strong>of</strong> this grid system lies <strong>in</strong> the coupl<strong>in</strong>g between an <strong>in</strong>terpolationmethod, which will be described later, and the <strong>non</strong>-staggered grid system. Be<strong>in</strong>g <strong>in</strong>spired with this idea,we consider <strong>in</strong> this study a control volume Ω k <strong>in</strong> the form <strong>of</strong> tetrahedron, Fig. 4. The hybrid grid systemdef<strong>in</strong>es the values <strong>of</strong> pressure and Cartesian velocity components <strong>in</strong> the centre <strong>of</strong> the control volume Ω kand the values <strong>of</strong> face-normal velocity V m , which has the direction <strong>of</strong> outward unit vector n m knormal tothe m-th face Γ m k <strong>of</strong> the control volume Ω k, is def<strong>in</strong>ed <strong>in</strong> the middle <strong>of</strong> the face Γ m k .After the <strong>in</strong>tegration <strong>of</strong> Eqs. (10) – (14) over each control volume Ω k , Fig. 4, k = 1, 2, . . . , N CV ,where N CV is the number <strong>of</strong> control volumes with<strong>in</strong> the hybrid unstructured tetrahedral computationalmesh, after the <strong>in</strong>troduction <strong>of</strong> <strong>in</strong>tegral average for an arbitrary <strong>flow</strong> quantity Φ over the control volumeΩ k(Φ) k = 1 ∫ΦdΩ, (15)|Ω k |Ω k
Vimmr J., Jonášová A., Bublík O. 1509Fig. 4: A tetrahedral control volume Ω k = A 1 A 2 A 3 A 4 with boundary ∂Ω k =hybrid unstructured computational mesh.⋃ 4 Γ m km=1belong<strong>in</strong>g to thewhere |Ω k | is the volume <strong>of</strong> the tetrahedral control volume Ω k , and f<strong>in</strong>ally, after the application <strong>of</strong> theGauss-Ostrogradsky theorem, which converts the volume <strong>in</strong>tegrals to surface <strong>in</strong>tegrals, we get(vi ∗ ) k = (vi n ) k − ∆t ∮(vn|Ω k | j · jn )k · vni dΓ, (16)∂Ω k1∆t (ˆv i) k − 1 ∮η( ˙γ)Re|Ω k |ˆd ij · jn k dΓ = 1 ∆t (v∗ i ) k + 1 ∮η( ˙γ) d ∗ ij · jn k dΓ, (17)Re|Ω k |∂Ω k ∂Ω k⎛⎞( )ˆdij − 1 ∮⎜⎝ ˆv i · jn∮k dΓ + ˆv j · <strong>in</strong> ⎟k dΓ⎠ = 0 , (18)k 2∂Ω k ∂Ω k∮∂p n+1dΓ = 1 ∮ˆv i · <strong>in</strong> k dΓ, (19)∂n k ∆t∂Ω k ∂Ω k(v<strong>in</strong>+1 ) k = (ˆv i ) k − ∆t ∮p n+1 · <strong>in</strong> k dΓ, (20)|Ω k |∂Ω kwhere i n k is the i-th component <strong>of</strong> the outward unit vector n k = [ 1 n k , 2 n k , 3 n k ] T normal to the boundary∂Ω k <strong>of</strong> the tetrahedral control volume Ω k , Fig. 4. In order to achieve the satisfaction <strong>of</strong> the cont<strong>in</strong>uityequation for the normal velocity V = v i · <strong>in</strong> k , the system <strong>of</strong> Eqs. (16) – (20) is completed with follow<strong>in</strong>gequationV n+1 = ˆV − ∆t ∂pn+1∂n k. (21)This equation def<strong>in</strong>es the normal velocity V n+1 at the time level (n + 1) hav<strong>in</strong>g the direction <strong>of</strong> theoutward unit vector n k normal to the boundary ∂Ω k <strong>of</strong> the control volume Ω k . For the <strong>in</strong>termediatenormal velocity ˆV , it is valid that ˆV = ˆv i · <strong>in</strong> k .Further, we perform the approximation <strong>of</strong> surface <strong>in</strong>tegrals <strong>in</strong> the system <strong>of</strong> Eqs. (16) – (20). Firstly,each <strong>in</strong>tegral is replaced by the sum <strong>of</strong> <strong>in</strong>tegrals over each face Γ m k<strong>of</strong> the control volume Ω k, Fig. 4, and
1510 Eng<strong>in</strong>eer<strong>in</strong>g Mechanics 2012, #38then approximated by the midpo<strong>in</strong>t rule∮Φ dΓ =∂Ω k4∑∫m=1Γ m k4∑Φ dΓ ≈ Φ m |Γ m k |, (22)m=1where |Γ m k |, m = 1, . . . , 4 is the area <strong>of</strong> the m-th face Γm k<strong>of</strong> the control volume Ω k and Φ m is the value<strong>of</strong> an arbitrary <strong>flow</strong> quantity at the <strong>in</strong>tegration po<strong>in</strong>t at the same face. The <strong>in</strong>terpolation process neededfor the determ<strong>in</strong>ation <strong>of</strong> Φ m at the m-th face Γ m k<strong>of</strong> the control volume Ω k will be described later. Us<strong>in</strong>gEq. (22), the system <strong>of</strong> Eqs. (16) – (21) is modified as follows(ˆv i ) k∆t(v ∗ i ) k = (v n i ) k − ∆t|Ω k |4∑m=1(V n m · v n i m| upw<strong>in</strong>d)|Γ m k | , (23)14∑−η( ˙γ) m m ˆdRe |Ω k |ij · jn m k |Γm k | = (v∗ i ) k 14∑+η( ˙γ) m d ∗mij · jn m k∆t Re |Ωm=1k ||Γm k |, (24)m=1(( )4∑)ˆdij − 1 ˆv i m · jn4∑mkk 2| Γm k | + ˆv j m · <strong>in</strong> m k | Γm k | = 0 , (25)m=1m=14∑ ∂p n+1∂n m |Γ m k | = 1 4∑ˆv i m · <strong>in</strong> m km=1 k∆t| Γm k | ≡ 1 4∑ˆV m |Γ m k |, (26)∆tm=1m=1(v<strong>in</strong>+1 ) k = (ˆv i ) k − ∆t 4∑p n+1m · <strong>in</strong> m k|Ω k ||Γm k | , (27)V n+1mm=1= ˆV m − ∆t ∂pn+1∂n m k, (28)where i n m k is the i-th component <strong>of</strong> the outward unit vector nm k= [1 n m k , 2 n m k , 3 n m k ]T normal to the m-thface Γ m k<strong>of</strong> the control volume Ω k and for the <strong>in</strong>termediate face-normal velocity ˆV m at the m-th face Γ m k<strong>of</strong> the control volume Ω k , it is valid that ˆV m = ˆv im · <strong>in</strong> m k. Note that the values <strong>of</strong> face-normal velocityVmn+1 computed with the help <strong>of</strong> Eq. (28) are used as values <strong>of</strong> face-normal velocity Vm n <strong>in</strong> Eq. (23) atthe next time level.Explicit schemes are known for their disadvantage <strong>in</strong> the form <strong>of</strong> restricted time steps. The CFLstability condition imposed on the time step size becomes essential when it is applied for grids with largedifferences <strong>in</strong> cell size, e.g., <strong>in</strong> complex geometries. In this case, the efficiency <strong>of</strong> explicit schemes islost, s<strong>in</strong>ce the cell with the most restrictive local time step determ<strong>in</strong>es the size <strong>of</strong> the global time step forall grid cells. One <strong>of</strong> possible solutions to this problem lies <strong>in</strong> the application <strong>of</strong> the well-known localtime-stepp<strong>in</strong>g method. This method, whose approach is also employed <strong>in</strong> our developed solver, enableseach cell <strong>of</strong> the computational grid to run with its own time step <strong>in</strong> a time-consistent manner.Interpolation methodTo perform numerical computations accord<strong>in</strong>g to Eqs. (23) – (28), it is necessary to determ<strong>in</strong>e values<strong>of</strong> vi n m | upw<strong>in</strong>d , ˆv i m, p n+1m and derivatives ∂ˆv i ∂v∂n m i,∗k ∂n m , ∂pn+1k ∂n m at the m-th face Γ m k<strong>of</strong> the control volumekΩ k . The value <strong>of</strong> vi n m | upw<strong>in</strong>dis computed by the upw<strong>in</strong>d scheme, whose first order accuracy is <strong>in</strong>creasedby l<strong>in</strong>ear reconstruction with Barth’s limiter,v n i m| upw<strong>in</strong>d={(vni ) L + σLBarth(vi n) R + σRBarth· ∂(vn i ) L∂x j· r jL , Vm n > 0 ,· ∂(vn i ) R∂x j· r jR , Vm n ≤ 0 ,(29)where σ Barth ∈ [0, 1] is the Barth’s limiter, Barth and Jesperson (1989), and vectors r L , r R are denoted<strong>in</strong> Fig. 5 (left). Further, the value Φ m <strong>of</strong> an arbitrary <strong>flow</strong> quantity Φ at the mid-po<strong>in</strong>t O <strong>of</strong> the m-thface Γ m k, Fig. 5 (right), can be stated with the help <strong>of</strong> second order accurate l<strong>in</strong>ear <strong>in</strong>terpolation from
Vimmr J., Jonášová A., Bublík O. 1511values (Φ) k and (Φ) lm def<strong>in</strong>ed <strong>in</strong> cell-centres S k and S lm <strong>of</strong> two adjacent control volumes Ω k and Ω lm ,respectively,Φ m = (Φ) k + (Φ) l m− (Φ) kγ k + γ lm· γ k = γ l m(Φ) k + γ k (Φ) lmγ k + γ lm, (30)where γ k and γ lm are the m<strong>in</strong>imal distances to the cell-face Γ m k from cell-centres S k and S lm <strong>of</strong> theadjacent control volumes Ω k and Ω lm , respectively, Fig. 5 (right). The derivative <strong>of</strong> <strong>flow</strong> quantity Φ <strong>in</strong>the direction <strong>of</strong> the outward unit vector n m k normal to the m-th face Γm k <strong>of</strong> the control volume Ω k, isapproximated at the mid-po<strong>in</strong>t O <strong>of</strong> the face Γ m k, Fig. 5 (right), as∣∂Φ∂n m k∣∣Γ mk≈ (Φ) l m− (Φ) kγ k + γ lm. (31)A crucial part <strong>of</strong> the <strong>in</strong>terpolation method is the application <strong>of</strong> Eq. (31) to the normal derivative <strong>in</strong>Eqs. (26) and (28). In this way, it is ensured that the face-normal velocity Vmn+1 satisfies the cont<strong>in</strong>uityequation at the time level (n + 1) exactly, see Eq. (37). However, <strong>in</strong> general velocities (v<strong>in</strong>+1 ) k <strong>in</strong>cell-centres <strong>of</strong> control volumes Ω k do not satisfy the cont<strong>in</strong>uity equation.Fig. 5: Def<strong>in</strong>ition <strong>of</strong> the vectors r L and r R for two adjacent tetrahedral control volumes Ω L and Ω R(left). Two adjacent tetrahedral control volumes Ω k = A 1 A 2 A 3 A 4 and Ω lm = A 1 A 2 A 3 A 5 with theircontact face Γ m k= ∆A 1A 2 A 3 (right).Regard<strong>in</strong>g the implementation <strong>of</strong> <strong>non</strong>-dimensional boundary conditions at the boundary ∂Ω <strong>of</strong> thecomputational doma<strong>in</strong> Ω ⊂ R 3 , three boundary types are considered <strong>in</strong> this study:• <strong>in</strong>let Γ m k⊂ ∂Ω I – In this case, Dirichlet boundary conditions for the velocity components v i mand the auxiliary variable d m ij are prescribedv i m = v i I , d m ij · jn = 0. (32)The value <strong>of</strong> face-normal velocity Vm I at the face Γ m kis computed as V m I = v i I · <strong>in</strong> m k, where valuesv i I are given accord<strong>in</strong>g to section 5. For the normal derivative <strong>of</strong> the pressure p n+1 at the face Γ m k ,we prescribe∂p n+1∂n m ∣ = 0. (33)k Γ mk• rigid and impermeable wall Γ m k ⊂ ∂Ω W – Velocity components v i m at the face Γ m kare set equalto zerov i m = 0 , (34)lead<strong>in</strong>g to zero value <strong>of</strong> the face-normal velocity Vm W = v i m · <strong>in</strong> m k = 0 at the face Γm k. For theauxiliary variable dij m , we apply the Dirichlet boundary condition <strong>in</strong> the follow<strong>in</strong>g formd m ij · jn = 0 . (35)Further, zero normal derivative <strong>of</strong> the pressure p n+1 (33) is prescribed at the wall.
1512 Eng<strong>in</strong>eer<strong>in</strong>g Mechanics 2012, #38• outlet Γ m k⊂ ∂Ω O – Follow<strong>in</strong>g type <strong>of</strong> boundary condition is statedp m n m k − 1 Re 2 η( ˙γ)m d m ij · jn m k = p On m k , (36)where p O is the given value <strong>of</strong> the outlet pressure, for details see section 5.Substitut<strong>in</strong>g the derivative ∂pn+1∂n m <strong>in</strong> Eq. (26) with Eq. (28), we getk4∑ ∂p n+1∂n m |Γ m k | = 1 4∑m=1 k∆tm=14∑=⇒m=1( )ˆVm − Vmn+1 |Γ m k | = 1 ∆t4∑m=1ˆV m |Γ m k |Vm n+1 |Γ m k | = 0, (37)i.e., face-normal velocities Vmn+1 satisfy the cont<strong>in</strong>uity equation exactly. At this po<strong>in</strong>t, let us mentionthat at the outlet boundary ∂Ω O , i.e., at the face Γ m k <strong>of</strong> the control volume Ω k, where Γ m k ⊂ ∂Ω O, values∂p n+1∂n m kare unknown. In order to ensure the satisfaction <strong>of</strong> the cont<strong>in</strong>uity equation (37) for this controlvolume Ω k , it is necessary to compute the face-normal velocity Vm n+1 at the face Γ m k ⊂ ∂Ω O asVm n+1O= − 1 4∑|Γ m VOm n+1 |Γ m k |, (38)k|m=1m≠m Owhere m O is the <strong>in</strong>dex <strong>of</strong> the outlet face Γ m Ok<strong>of</strong> the control volume Ω k . For the whole computationaldoma<strong>in</strong> Ω ⊂ R 3 at the time t = 0, follow<strong>in</strong>g <strong>in</strong>itial conditions are used(vi 0 ) k = 1 ∫v i (x, 0)dΩ = 0, (p 0 ) k = 1 ∫p(x, 0)dΩ = p <strong>in</strong>itial , k = 1, 2, . . . , N CV ,|Ω k ||Ω k |Ω k Ω kwhere p <strong>in</strong>itial is a <strong>non</strong>-dimensional value <strong>of</strong> static pressure.5. Numerical resultsIn accordance with the boundaries <strong>of</strong> the computational doma<strong>in</strong> denoted <strong>in</strong> Fig. 3 for the model <strong>of</strong> the<strong>in</strong>dividual aorto-coronary <strong>bypass</strong>, the numerical simulations <strong>of</strong> <strong>pulsatile</strong> Newtonian and <strong>non</strong>-Newtonian<strong>blood</strong> <strong>flow</strong> are carried out with follow<strong>in</strong>g values <strong>of</strong> the time-dependent boundary conditions:• aortic <strong>in</strong>let ∂Ω (A)I– constant time-dependent velocity pr<strong>of</strong>ile |v I | accord<strong>in</strong>g to the <strong>flow</strong> rate waveformQ(t) shown <strong>in</strong> Fig. 6 (left);• aortic outlet ∂Ω (A)O– time-dependent pressure p(t) shown <strong>in</strong> Fig. 6 (right), where the aortic pressureis plotted <strong>in</strong> the medical units <strong>of</strong> millimeters <strong>of</strong> mercury (1 mmHg = 133.333 Pa);• coronary outlets ∂Ω (CA)O– constant pressure related to average arterial pressure <strong>of</strong> 12 000 Pa;• rigid and impermeable walls ∂Ω W – <strong>non</strong>-slip boundary condition.Note that the boundary values mentioned above are, for the computation, <strong>non</strong>-dimensionalized us<strong>in</strong>g thereference values mentioned <strong>in</strong> section 3. The implementation <strong>of</strong> the boundary conditions <strong>in</strong> the numericalcode is described <strong>in</strong> detail <strong>in</strong> section 4.For the analysis <strong>of</strong> computed numerical results, we <strong>in</strong>troduce two significant hemodynamical wallparameters – the cycle-averaged wall shear stress (WSS) and the oscillatory shear <strong>in</strong>dex (OSI) that areevaluated accord<strong>in</strong>g to formulas mentioned <strong>in</strong> Xiong and Chong (2008) and He and Ku (1996), respectively,⎡|τ W | = 1 ∫ T|τ W |dt , OSI = 1 ∫⎢T ⎛∫ T ⎞⎣1 −T2τ W dt∣ ∣ · ⎝ |τ W |dt⎠−1 ⎤ ⎥ ⎦ , (39)0where |τ W | is the WSS magnitude and T = 1 s is the duration <strong>of</strong> one cardiac cycle, Fig. 6.00
Vimmr J., Jonášová A., Bublík O. 1513450400350300Q(t) [ml/s]2502001501005000 0.2 0.4 0.6 0.8 1time [s]Fig. 6: Time-dependent boundary conditions for the aorta – <strong>in</strong>let <strong>flow</strong> rate Q(t) (left) and outlet pressurep(t) (right), data taken from Olufsen et al. (2000)Firstly, let us analyse the velocity pr<strong>of</strong>iles <strong>of</strong> the <strong>non</strong>-Newtonian <strong>blood</strong> <strong>flow</strong> <strong>in</strong> Fig. 7 for three selectedtime <strong>in</strong>stants, correspond<strong>in</strong>g to systole, diastole and late diastole, respectively. Dur<strong>in</strong>g the systolic phase(t 1 = 0.16 s), Fig. 7 (left), the graft’s proximal anastomosis becomes exposed to the <strong>in</strong>creased <strong>flow</strong> rate<strong>in</strong> the aorta. Although the skewed velocity pr<strong>of</strong>iles at the graft entrance may <strong>in</strong>dicate <strong>in</strong>com<strong>in</strong>g <strong>blood</strong><strong>flow</strong>, the real graft fill<strong>in</strong>g occurs later. By compar<strong>in</strong>g the pictures <strong>in</strong> Fig. 7, it becomes quite apparentthat the systolic phase <strong>of</strong> the cardiac cycle is represented by decreased <strong>blood</strong> <strong>flow</strong> through the <strong>in</strong>dividual<strong>bypass</strong> graft, whereas an opposite effect is observed dur<strong>in</strong>g most <strong>of</strong> the diastolic phase (t 2 = 0.47 s andt 3 = 0.98 s). In this case, the velocity <strong>in</strong>crease observed along the <strong>in</strong>dividual graft is also accompaniedby skewed or otherwise shaped velocity pr<strong>of</strong>iles that are a result <strong>of</strong> the out-<strong>of</strong>-plane geometry and thegraft’s w<strong>in</strong>d<strong>in</strong>g around the heart, see Fig. 2. At the distal end-to-side anastomosis, Fig. 7c, the <strong>in</strong>com<strong>in</strong>g<strong>blood</strong> <strong>flow</strong> seems to prefer the closer branch <strong>of</strong> the coronary artery more than the second one. Moreover,the closer coronary artery shows a tendency to considerably <strong>in</strong>crease velocity magnitude downstreamfrom the anastomosis. The reason for this phenome<strong>non</strong> is a partly stenosed coronary artery.The comparison between the Newtonian and <strong>non</strong>-Newtonian <strong>blood</strong> <strong>flow</strong> is illustrated by the distributions<strong>of</strong> the cycle-averaged WSS and OSI <strong>in</strong> Figs. 8 and 9, respectively. At this po<strong>in</strong>t, note thelowered value range <strong>in</strong> Fig. 8, which is chosen accord<strong>in</strong>g to conclusions mentioned <strong>in</strong> Haruguchi andTeraoka (2003) and He and Ku (1996). Namely, that low WSS, as compared to the normal range between1 − 2 Pa <strong>in</strong> healthy arteries, is one <strong>of</strong> the confirmed triggers <strong>of</strong> vessel remodell<strong>in</strong>g, plaque growthand <strong>in</strong>timal thicken<strong>in</strong>g. In light <strong>of</strong> this fact, we will further assess the result<strong>in</strong>g shear distribution, whichregardless <strong>of</strong> the viscosity model (Newtonian or <strong>non</strong>-Newtonian), seems to be <strong>non</strong>-uniform at both anastomoses,Fig. 8. One <strong>of</strong> the dist<strong>in</strong>ct areas with extremely low shear is situated at the entrance <strong>of</strong> thegraft, where it is caused by a large recirculation zone that is present there most <strong>of</strong> the cardiac cycle. Thisnegative stimulation <strong>of</strong> the proximal suture l<strong>in</strong>e is also confirmed by the high OSI shown <strong>in</strong> Fig. 9. At thedistal anastomosis, shear values below 1 Pa are observed at the heel and the arterial floor <strong>in</strong> accordancewith the sites <strong>of</strong> <strong>in</strong>timal hyperplasia displayed <strong>in</strong> Fig. 1. In this case, the critical shear stress also showsa oscillatory tendency as is apparent from the OSI distribution <strong>in</strong> Fig. 9.The objective <strong>of</strong> our previous study, Vimmr and Jonášová (2010), was the <strong>in</strong>vestigation <strong>of</strong> <strong>blood</strong>’s<strong>non</strong>-Newtonian behaviour <strong>in</strong> complete <strong>bypass</strong> models with coronary or femoral native arteries. Thenumerical simulations were carried out under steady <strong>flow</strong> conditions and for an idealized <strong>bypass</strong> geometry.In the present study, we want to extend our previous conclusions about the importance <strong>of</strong> <strong>blood</strong>’s<strong>non</strong>-Newtonian modell<strong>in</strong>g <strong>in</strong> coronary <strong>bypass</strong>es by consider<strong>in</strong>g <strong>pulsatile</strong> <strong>blood</strong> <strong>flow</strong> and a <strong>realistic</strong> andmore complex <strong>bypass</strong> geometry. As is illustrated by Figs. 8 – 9, the <strong>in</strong>fluence <strong>of</strong> <strong>non</strong>-Newtonian <strong>flow</strong>conditions is very small or rather negligible (as is the case <strong>of</strong> the velocity pr<strong>of</strong>iles). On the basis <strong>of</strong>these observations, we can draw a conclusion similar to that mentioned <strong>in</strong> Vimmr and Jonášová (2010).Namely, that <strong>blood</strong>’s <strong>non</strong>-Newtonian behaviour does not have any significant impact on the hemodynamics<strong>in</strong> coronary <strong>bypass</strong>es. In light <strong>of</strong> this observation and our present experience with the modell<strong>in</strong>g<strong>of</strong> <strong>non</strong>-Newtonian <strong>blood</strong> <strong>flow</strong>, it may be said that an hemodynamic study <strong>in</strong> patient-specific femoral <strong>bypass</strong>eswould be more promis<strong>in</strong>g <strong>in</strong> regard to the occurrence <strong>of</strong> <strong>non</strong>-Newtonian <strong>effects</strong> as was concluded<strong>in</strong> our previous study Vimmr and Jonášová (2010). This problem will be addressed <strong>in</strong> the future.
1514 Eng<strong>in</strong>eer<strong>in</strong>g Mechanics 2012, #38Fig. 7: Non-Newtonian <strong>blood</strong> <strong>flow</strong> – velocity pr<strong>of</strong>iles at selected cross-sections <strong>of</strong> the aorto-coronary <strong>bypass</strong> at the time <strong>in</strong>stants t1 = 0.16 s, t2 = 0.47 s andt3 = 0.98 s (from left to right); detailed views at (a) the proximal anastomosis, (b) <strong>in</strong>dividual graft, (c) coronary arteries with the distal anastomosis
Vimmr J., Jonášová A., Bublík O. 1515Fig. 8: Distribution <strong>of</strong> cycle-averaged WSS for the Newtonian (left) and <strong>non</strong>-Newtonian <strong>flow</strong> (right)Fig. 9: Distribution <strong>of</strong> OSI for the Newtonian (left) and <strong>non</strong>-Newtonian <strong>flow</strong> (right)
1516 Eng<strong>in</strong>eer<strong>in</strong>g Mechanics 2012, #38AcknowledgmentsThis study was supported by the European Regional Development Fund (ERDF), project NTIS - NewTechnologies for Information Society, European Centre <strong>of</strong> Excellence, CZ.1.05/1.1.00/02.0090 and bythe <strong>in</strong>ternal student grant project SGS-2010-046 <strong>of</strong> the University <strong>of</strong> West Bohemia.ReferencesBassiouny, H.S., White, S., Glagov, S., Choi, E., Giddens, D.P., Zar<strong>in</strong>s, C.K. (1992), Anastomotic <strong>in</strong>timal hyperplasia:Mechanical <strong>in</strong>jury or <strong>flow</strong> <strong>in</strong>duced. Journal <strong>of</strong> Vascular Surgery, Vol 15, No.4, pp 708-717.Barth, T.J., Jesperson, D.C. (1989), The design and application <strong>of</strong> upw<strong>in</strong>d schemes on unstructured meshes. In:Proceed<strong>in</strong>gs <strong>of</strong> the 27th AIAA Aerospace Sciences Meet<strong>in</strong>g. AIAA Paper 89-0366.Cho, Y.I., Kensey, K.R. (1991), Effects <strong>of</strong> the <strong>non</strong>-Newtonian viscosity <strong>of</strong> <strong>blood</strong> on <strong>flow</strong>s <strong>in</strong> diseased arterialvessels. Part I: Steady <strong>flow</strong>s. Biorheology, Vol 28, No.3-4, pp 241-262.Ferziger, J.H., Perić M. (1999), Computational methods for fluid dynamics, Spr<strong>in</strong>ger, Heidelberg.Haruguchi, H., Teraoka, S. (2003), Intimal hyperplasia and hemodynamic factors <strong>in</strong> arterial <strong>bypass</strong> and arteriovenousgrafts: A review. Journal <strong>of</strong> Artificial Organs, Vol 6, No.4, pp 227-235.He, X., Ku, D.N. (1996), Pulsatile <strong>flow</strong> <strong>in</strong> the human left coronary artery bifurcation: Average conditions. Journal<strong>of</strong> Biomechanical Eng<strong>in</strong>eer<strong>in</strong>g, Vol 118, No.1, pp 74-82.Kim, D., Choi, H. (2000) A second-order time accurate f<strong>in</strong>ite volume method for unsteady <strong>in</strong>compressible <strong>flow</strong> onhybrid unstructured grids. Journal <strong>of</strong> Computational Physics, Vol 162, No.2, pp 411-428.Loth, F., Fischer, P.F., Bassiouny, H.S. (2008) Blood <strong>flow</strong> <strong>in</strong> end-to-side anastomoses. Annual Review <strong>of</strong> FluidMechanics, Vol 40, pp 367-393.Olufsen, M.S., Pesk<strong>in</strong>, C.S., Kim, W.Y., Pedersen, E.M., Nadim, A., Larsen, J. (2000) Numerical simulation andexperimental validation <strong>of</strong> <strong>blood</strong> <strong>flow</strong> <strong>in</strong> arteries with structured-tree out<strong>flow</strong> conditions. Annals <strong>of</strong> BiomedicalEng<strong>in</strong>eer<strong>in</strong>g, Vol 28, No.11, pp 1281-1299.Vimmr, J., Jonášová, A. (2010), Non-Newtonian <strong>effects</strong> <strong>of</strong> <strong>blood</strong> <strong>flow</strong> <strong>in</strong> complete coronary and femoral <strong>bypass</strong>es.Mathematics and Computers <strong>in</strong> Simulation, Vol 80, No.6, pp 1324-1336.Vural, K.M., Şener, E., Taşdemir, O. (2001) Long-term patency <strong>of</strong> sequential and <strong>in</strong>dividual saphenous ve<strong>in</strong> coronary<strong>bypass</strong> grafts. European Journal <strong>of</strong> Cardio-thoracic Surgery, Vol 19, No.2, pp 140-144.Xiong, F.L., Chong, C.K. (2008), A parametric numerical <strong>in</strong>vestigation on haemodynamics <strong>in</strong> distal coronaryanastomoses. Medical Eng<strong>in</strong>eer<strong>in</strong>g & Physics, Vol 30, No.3, pp 311-320.Zeng, D., D<strong>in</strong>g, Z., Friedman, M.H., Ethier, C.R. (2003), Effects <strong>of</strong> cardiac motion on right coronary arteryhemodynamics. Annals <strong>of</strong> Biomedical Eng<strong>in</strong>eer<strong>in</strong>g, Vol 31, No.4, pp 420-429.