Use of sodium citrate anticoagulant for routine hematology - Carden ...
Use of sodium citrate anticoagulant for routine hematology - Carden ...
Use of sodium citrate anticoagulant for routine hematology - Carden ...
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
ISLHLaboratory Hematology 4:156–162© 1998 <strong>Carden</strong> Jennings Publishing Co., Ltd.#98-1.Perrotta.Spring98Official Publication<strong>Use</strong> <strong>of</strong> <strong>sodium</strong> <strong>citrate</strong> <strong>anticoagulant</strong> <strong>for</strong> <strong>routine</strong><strong>hematology</strong> analysis on the CELL-DYN ® 4000:An opportunity to enhance efficiency in theclinical laboratoryG. PERROTTA, 1 L. ROBERTS, 1 J. GLAZIER, 2 H.R. SCHUMACHER 11 Department <strong>of</strong> Pathology and Laboratory Medicine, University <strong>of</strong> Cincinnati Medical Center, Cincinnati, OH2 Abbott Laboratories, Abbott Park, ILABSTRACTBlood from 67 sophomore medical students was used to evaluatedifferences in complete blood count (CBC) normal ranges inspecimens collected in either liquid tripotassium ethylene diaminetetraacetic acid (EDTA) or liquid tri<strong>sodium</strong> <strong>citrate</strong> and analyzedby the Abbott CELL-DYN 4000 <strong>hematology</strong> system (AbbottDiagnostics, Abbott Park, IL). The data support the premise that<strong>citrate</strong> is a suitable <strong>anticoagulant</strong> <strong>for</strong> <strong>routine</strong> CBC analysis providedthat a dilution correction factor <strong>for</strong> counts, hematocrit, andhemoglobin is applied automatically, either as a built-in algorithmin the s<strong>of</strong>tware <strong>of</strong> the cell counter or <strong>of</strong> the laboratory in<strong>for</strong>mationsystem. Once the corrections were made, the results showed excellentagreement between the two <strong>anticoagulant</strong>s. In addition,peripheral blood smears prepared from <strong>citrate</strong>d blood showedgood morphology. Overall, the data demonstrate the suitability <strong>of</strong>per<strong>for</strong>ming a CBC with a <strong>citrate</strong>d specimen, once it has been corrected<strong>for</strong> the dilution. This observation could facilitate the adaptation<strong>of</strong> one tube <strong>for</strong> two major analyses (<strong>hematology</strong> and coagulationparameters), especially considering the advances in in<strong>for</strong>maticsand robotics technology. Immediate operational efficienciescould be realized throughout the testing process. Some would generatecost savings by eliminating the EDTA tube <strong>for</strong> <strong>routine</strong> CBCtesting. Other savings could be generated in the pre-analyticalphase, principally in the specimen collection process because fewertubes and labels, and decreased sorting, routing, and phlebotomytime would be required. The authors suggest that larger and morethorough studies be per<strong>for</strong>med to ascertain that these findings inAddress correspondence to Gerardo Perrotta, MPA, Department <strong>of</strong> Pathologyand Laboratory Medicine, University <strong>of</strong> Cincinnati, PO Box 670529, Cincinnati,OH 45267-0529.Received 29 January 1998; accepted 3 April 1998<strong>citrate</strong>d samples are valid across a broad spectrum <strong>of</strong> <strong>hematology</strong>conditions, and that they can be easily generated in the evolvingand reconfigured laboratory operations. Lab Hematol 4:156–162, 1998KEY WORDS: Automated CBC · EDTA ·Hematology analyzersINTRODUCTIONThe purpose <strong>of</strong> this study was to compare tripotassium ethylenediamine tetraacetic acid (K 3 EDTA) with tri<strong>sodium</strong> <strong>citrate</strong> collectiontubes in regard to automated <strong>hematology</strong> parameters, and toevaluate the latter <strong>for</strong> reliablity and effectiveness. Using a single tube<strong>for</strong> two major tests in the clinical laboratory promotes both operationaland technical efficiencies. Advances in in<strong>for</strong>matic and robotictechnology present opportunities or reasons to evaluate other <strong>anticoagulant</strong>sthat have been considered impractical or expensive [1,2].The use <strong>of</strong> tri<strong>sodium</strong> <strong>citrate</strong> requires correcting the dilution eithermanually or by transfer to another personal computer and wouldsubstantially affect the turnaround time <strong>of</strong> coagulation testing givenpresent-day laboratory configurations. Heparin has always beenconsidered expensive and to interfere with the staining properties <strong>of</strong>cells. The oxalates cause cell shrinkage or swelling, depending onthe potassium or ammonium salt used.Thus, given its general availability, ease <strong>of</strong> preparation, widespreaduse, and relatively low cost, a salt <strong>of</strong> EDTA has become the<strong>anticoagulant</strong> <strong>of</strong> choice. The National Committee <strong>for</strong> Clinical LaboratoryStandards (NCCLS) H1-A4 standard [3] recommendsEDTA as the preferred <strong>anticoagulant</strong> <strong>for</strong> complete blood countanalysis and WBC differential, principally <strong>for</strong> its overall cell preservationproperties. However, an attempt to select and standardize thedry powder (di-<strong>sodium</strong> or dipotassium) or liquid (tripotassium) salt<strong>of</strong> EDTA through a tentative standard (H35-T) process has beendiscontinued and replaced by the H1-A standard. For its part, the156
Sodium Citrate CBCs on the CD-4000 157International Council <strong>for</strong> Standards in Hematology (ICSH) ExpertPanel on Cytometry has evaluated the three EDTA salts and recommendsK 2 EDTA [4]. In the United States, 50% <strong>of</strong> laboratoriesuse the recommended <strong>anticoagulant</strong>. Regardless <strong>of</strong> its current status,many practitioners appreciate certain limitations <strong>of</strong> EDTA, whichstem from a wide range <strong>of</strong> additives (powder, liquid, spray; di- ortri-salts <strong>of</strong> <strong>sodium</strong> or potassium) and evacuated tube sizes and typesstill available in the market. These variables coupled with inconsistentspecimen volume draws and a variety <strong>of</strong> mixing, storing, andtransporting conditions produce questionable results [5–7].On the other hand, <strong>sodium</strong> <strong>citrate</strong> would preclude many <strong>of</strong> thevariables mentioned above. Because <strong>sodium</strong> <strong>citrate</strong> has been used asan <strong>anticoagulant</strong> primarily <strong>for</strong> coagulation studies, phlebotomistsare attuned to the full draw requirement <strong>of</strong> the coagulation (bluetop)tubes regardless <strong>of</strong> their size. The ratio <strong>of</strong> <strong>anticoagulant</strong> toblood is better maintained with <strong>citrate</strong> than with EDTA, thusachieving a greater standardization currently lacking with EDTA.The growing complexity <strong>of</strong> modern laboratory systems and thegreater emphasis on developing cost-efficient and innovative solutionsto numerous problems increase the need to explore and developnew concepts without sacrificing quality across the spectrum <strong>of</strong>care. At our institution, approximately 150,000 CBCs and 50,000coagulation tests (prothrombin time [PT] and activated partialthromboplastin time [aPTT]) are per<strong>for</strong>med annually. Up to 25%<strong>of</strong> the CBCs are accompanied by a coagulation request; conversely,80–90% <strong>of</strong> the <strong>routine</strong> coagulation tests are accompanied by aCBC request. If these CBC and coagulation requests were submittedin a single tube, significant efficiencies and cost benefits couldbe realized by an increased use <strong>of</strong> an expanding biotechnology andin<strong>for</strong>matics industry in the clinical laboratory.MATERIALS AND METHODSBlood SamplesPeripheral blood samples from 67 second-year medical students(42 men, 25 women), ranging in age from 19 to 41 years (mean <strong>of</strong>25 years) were used <strong>for</strong> this study.Specimens were collected in 3-mL vacutainer Hemogard tubes(K 3 EDTA; Becton Dickinson, Franklin Lakes, NJ) and 5-mLblue-top tubes (3.2% tri<strong>sodium</strong> <strong>citrate</strong>; Becton Dickinson) using21-gauge 1.5" needles. Specimens were mixed by gentle inversion,labeled, and prepared <strong>for</strong> analysis. Only paired specimens (i.e., oneK 3 EDTA and one tri<strong>sodium</strong> <strong>citrate</strong> sample from the same student)were used <strong>for</strong> analysis. Samples that did not meet minimum volumerequirements were discarded. All tubes were bar coded andplaced on the autosampler <strong>for</strong> automatic processing.CBC pr<strong>of</strong>iles were generated, first <strong>for</strong> the <strong>citrate</strong>d and then theEDTA tubes. All specimens were kept at room temperaturethroughout the study. Results were completed within 7 hours <strong>of</strong>collection and stored in the data management system <strong>of</strong> the CELL-DYN 4000 (Abbott Diagnostics, Santa Clara, CA). Peripheralblood smears were prepared within 3 hours <strong>of</strong> collection andstained with Wright’s stain in an Ames Hematek stainer (Miles,Diagnostic Division, Elkhart, IN).Hematology AnalyzerUsing the s<strong>of</strong>tware package R7-3 and reagents supplied by AbbottDiagnostics, the CELL-DYN 4000 was calibrated according to manufacturerguidelines and produced results within the acceptable rangeon all control samples. Three levels <strong>of</strong> controls (low, normal, andhigh) were within established limits <strong>for</strong> that specific lot number. Parallelquality control assessment with the CELL-DYN 3500 revealedthat the two instruments were in agreement <strong>for</strong> all values.Suspect flags were preset by the manufacturer and the high-lowdistributional flags were defined and preset by the laboratory.The CELL-DYN 4000 is the latest fully automated <strong>hematology</strong>analyzer that uses four-angle argon-laser light scatter, two-color fluorescence,high-resolution focused flow impedance, and hemoglobinspectrophotometry [8].Peripheral Blood SmearsPush wedge slides were prepared manually and stained withWright’s-Giemsa on the Hematek stainer (Miles). The slide preparedfrom the EDTA sample was used as the control. All cell lineswere examined <strong>for</strong> the EDTA and <strong>citrate</strong> samples using magnification20 and oil immersion with constant light intensity. A blindedstudy was conducted to determine if one (H.R.S.) could identifywhether a slide was from EDTA or <strong>citrate</strong> origin.Data ManagementData were generated by and stored in the data management system<strong>of</strong> the CELL-DYN 4000. It was later downloaded on diskettefrom the CELL-DYN 4000 Datalog in accordance with a protocolprovided by Abbott [9]. Corrections <strong>for</strong> cell counts and hemoglobinmeasurements were per<strong>for</strong>med with Micros<strong>of</strong>t Excel 5.0(Micros<strong>of</strong>t, Redmond, WA).The WBC, red blood cell count (RBC), hemoglobin (Hb),hematocrit (HCT), and platelet (Plt) results were multiplied by afactor <strong>of</strong> 1.1 to correct <strong>for</strong> sample dilution. The absolute leukocytecounts (neutrophils, lymphs, monocytes, eosinophils, andbasophils) also were multiplied by the same factor; however, thepercent leukocytes were recalculated by a simple percent ratio <strong>of</strong>absolute leukocyte to total WBC 100.Sized parameters (mean corpuscular volume [MCV], red bloodcell distribution width [RDW], and mean platelet volume [MPV])and proportional parameters (mean corpuscular hemoglobin[MCH] and mean corpuscular hemoglobin concentration[MCHC]) required no correction because these measurements wereunaffected by dilution.StatisticsThe results produced from analyses and corrected parameters wereanalyzed by descriptive statistics to determine standard deviations andmeans <strong>for</strong> each parameter. Multiple regression analysis (R 2 ) was usedto compare counts, paired Student’s t-test to compare means andRDW, and chi-square to evaluate peripheral blood smears.Statistical analyses and evaluations were calculated using theMicros<strong>of</strong>t Excel 5.0 and Jandel SigmaStat 2.0 (SPSS, Chicago, IL).ResultsData obtained in the present study with the resulting paired dataanalyses (R 2 <strong>for</strong> counts and p <strong>for</strong> means and distribution widths) arelisted in Table 1. Results from the <strong>citrate</strong>d samples are corrected <strong>for</strong>the dilution. The mean and range <strong>of</strong> all parameters determinedfrom the <strong>citrate</strong>d samples compare well with those from the EDTAsamples, except <strong>for</strong> the parameters marked with an asterisk. Thesehighlighted parameters show a poor statistical correlation <strong>for</strong> theabsolute basophil counts <strong>of</strong> females and monocyte counts <strong>of</strong> the
158 G Perrotta et al.TABLE 1. CBC pr<strong>of</strong>ile parameters and comparative ranges using the CELL-DYN ® 4000; EDTA vs. <strong>citrate</strong>Women (n=25)Men (n=42)Mean ± 2SD rangeMean ± 2SD rangeAnalyte SI unit EDTA Citrate ( 1.1) R 2 EDTA Citrate ( 1.1) R 2WBC 10 9 /L 5.9 (2.9–8.9) 6.0 (2.9–9.1) 0.88 5.8 (3.4–8.3) 5.6 (3.3–8.0) 0.94Neutrophil 10 9 /L 3.4 (1–5.8) 3.5 (1–6) 0.91 3.2 (1–5.5) 3.1 (0.9–5.3) 0.98Lymphocyte 10 9 /L 1.9 (1–2.8) 2 (1–2.9) 0.89 1.9 (1.2–2.6) 1.9 (1.2–2.6) 0.84Monocyte 10 9 /L 0.4 (0.1–0.7) 0.4 (0.2–0.7) 0.83 0.5 (0.3–0.8) 0.4 (0.1–0.7) 0.54 aEosinophil 10 9 /L 0.1 (0–0.3) 0.1 (0–0.3) 0.84 0.2 (0–0.4) 0.2 (0–0.3) 0.86Basophil 10 9 /L 0.03 (0–0.08) 0.03 (0–0.07) 0.00 a 0.04 (0–0.1) 0.04 (0–0.12) 0.86RBC 10 12 /L 4.52 (3.76–5.28) 4.5 (3.66–5.35) 0.93 4.99 (4.0–5.98) 5.04 (4.09–5.98) 0.90Hb g/dL 13.8 (12–15.5) 13.8 (11.6–16) 0.95 15.3 (12.3–18.2) 15.6 (12.9–18.2) 0.80HCT % 40.3 (35–45.5) 40.8 (34.9–46.7) 0.87 44.5 (36.4–52.6) 45.2 (37.8–52.6) 0.89Plt 10 9 /L 240 (150–329) 231 (139–323) 0.89 222 (134–311) 210 (136–285) 0.96p ≤ 0.05 p ≤ 0.05Neutrophil % 57.3 (40.1–73.9) 57 (39.7–74.3) 0.284 54.1 (37.3–70.9) 54.5 (38–71.1) 0.082Lymphocyte % 32.7 (18.2–47.2) 33.3 (18–48.6) 0.912 33 (18.6–47.4) 34.7 (19.6–49.7)
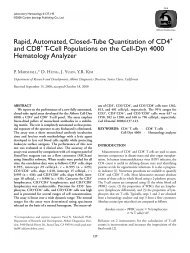
160 G Perrotta et al.Cell(s) EDTA CitrateNeutrophil/Platelet/RBCABEosinophilCDBasophilEFLymphocyteGHMonocyteIJFIGURE 1. Characteristic view <strong>of</strong> cells in EDTA vs. <strong>citrate</strong> oil immersion (1000).samples, however, was considered impractical [1]. Recently, Gulatiet al. [13] suggested mixing the blood by vortex to disaggregateplatelet clumps. Lippi et al. [12] have <strong>for</strong>mulated a dry <strong>citrate</strong>-pyridoxal5 phosphate (CPT) <strong>anticoagulant</strong> to improve cell countsand sizing, especially <strong>for</strong> platelets and MPV. Although these studiesfocus on improving platelet counts, we maintain that adopting theexisting <strong>sodium</strong> <strong>citrate</strong> tube <strong>for</strong> CBC analysis holds greater benefit<strong>for</strong> <strong>routine</strong> laboratories as they continue to undergo major reengineeringto achieve the highest efficiencies at the lowest operationalcost. In our view, CPT anticoagulated samples could not be easilyadopted <strong>for</strong> <strong>routine</strong> coagulation testing within the same time framerequired <strong>for</strong> the tri<strong>sodium</strong> <strong>citrate</strong> samples. All reference ranges <strong>for</strong>
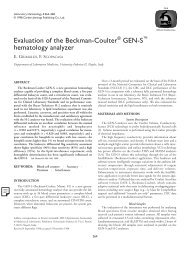
Sodium Citrate CBCs on the CD-4000 161EDTACitrateABFIGURE 2. Characteristic scatterplots and histograms <strong>of</strong> EDTA vs. <strong>citrate</strong>.coagulation tests would have to be determined on CPT samples—amore costly and laborious proposition with far-reaching impact onpatient care (i.e., monitoring Coumadin and heparin therapies).To our knowledge, no other studies have approached the question<strong>of</strong> per<strong>for</strong>ming CBCs from <strong>sodium</strong> <strong>citrate</strong> tubes to improvework flow and cost containment and to facilitate further laboratoryreengineering to accommodate the expanding role <strong>of</strong> robotics andin<strong>for</strong>mation technology.Medical students represent a normal group <strong>for</strong> establishing initialcomparability and acceptability and determining the feasibility<strong>of</strong> adopting an unconventional <strong>anticoagulant</strong> <strong>for</strong> CBC parameters.Because medical students represent a distinct and healthy agegroup,however, similar studies with other age-groups and varyingclinical conditions and pathologies will be required.The evolution <strong>of</strong> the <strong>hematology</strong> analyzer is converging withthat <strong>of</strong> in<strong>for</strong>matics and robotics. Expansion <strong>of</strong> bio-in<strong>for</strong>matics technologymakes it possible to alter past methods <strong>for</strong> more practicalapplications in today’s cost-restrictive health care environment [14].This study promotes the idea that CBCs can be per<strong>for</strong>med on<strong>citrate</strong>d samples provided that manufacturers <strong>of</strong> <strong>hematology</strong> analyzersincorporate algorithms or s<strong>of</strong>tware programs that automaticallycorrect <strong>for</strong> the <strong>citrate</strong> dilution. These programs can be located withineither the instrument data management system or the laboratoryin<strong>for</strong>mation system. All parameters reported per unit volumewould require a multiplication factor <strong>of</strong> 1.1 to account <strong>for</strong> the dilution<strong>of</strong> the sample. Mean and proportional parameters can bedirectly reported. Additional benefits also may be realized <strong>for</strong>patients and laboratories.The amount <strong>of</strong> blood needed <strong>for</strong> the most frequently orderedand fully automated test would be decreased. This reduced amount<strong>of</strong> blood translates into good public relations because <strong>of</strong> patient concernsabout the amount <strong>of</strong> blood drawn per test, and <strong>of</strong>fers betterpatient care and reduced risk <strong>of</strong> producing iatrogenic anemia. Operationally,the pre-analytic phase <strong>of</strong> a CBC will undergo a reductionin collection time. For example, less time will be spent on the phlebotomyprocedure, thus freeing the phlebotomists or nurse assistantsto per<strong>for</strong>m other ward responsibilities. Consequently, it may reducethe number <strong>of</strong> phlebotomists needed, thus generating more savings.Within the laboratory, the pre-analytic phase also would be curtailedbecause there would be fewer tubes to handle and process,favoring a more mechanized operation. This would result in technicaltime savings. Other cost factors also would be significantly and favorablyaffected. Inventory cost <strong>for</strong> lavender-top tubes and labels wouldbe reduced by the number <strong>of</strong> CBCs per<strong>for</strong>med. For example, in ourinstitution the conversion to a single <strong>citrate</strong> tube would generate asavings <strong>of</strong> $2000 per annum based on 150,000 CBCs and 50,000<strong>routine</strong> coagulation tests per<strong>for</strong>med annually at a cost <strong>of</strong> $0.06 and$0.07 <strong>for</strong> each tube needed <strong>for</strong> the tests, respectively. Other savingsmay be generated by a reduction <strong>of</strong> infectious waste that many laboratoriespay to have hauled away. In our area, the cost <strong>of</strong> infectiouswaste disposal ranges from $0.10 to $0.30 per pound, depending onwhether it is pre-treated (sterilized on site) be<strong>for</strong>e discarding.More importantly, per<strong>for</strong>ming CBCs and coagulation testingfrom one tube positions the laboratory to improve efficiency andthus become more cost-effective when it transitions to a fully automated,roboticized, and in<strong>for</strong>matics-driven system. Several vendors
162 G Perrotta et al.TABLE 4. LimitationsSample questions to be addressed in future studies1. Does the observation made on the CELL-DYN 4000 hold true <strong>for</strong>other <strong>hematology</strong> instruments?2. Is the sample stability <strong>of</strong> WBC, RBC, and Plt parameters similar in<strong>citrate</strong> and EDTA in terms <strong>of</strong> time intervals (0–24 or 72 hours),temperature (room vs. refrigerator), transportation (manual vs.automated), and quantity or volume <strong>of</strong> sample?3. What is the impact on coagulation testing after a sample has beenprocessed<strong>for</strong> CBC analysis, e.g., mixing and cap piercing?4. What protocols should be established <strong>for</strong> rechecking CBC orcoagulation results?5. What laboratory re-design would be needed to facilitate workflowprocesses <strong>for</strong> aliquoting, sorting, spinning and sampling?6. What would be the most efficient algorithm to adopt <strong>for</strong> correctingthe dilution effect <strong>of</strong> <strong>citrate</strong>, i.e., within the data managementsystem <strong>of</strong> the analyzer or <strong>of</strong> the LIS?7. What changes are needed in bar code systems to print labels withcodes <strong>for</strong> EDTA or <strong>citrate</strong>, <strong>for</strong> combined CBC and coagulant testingwith or without differential, CBC, or hemoglobin, and <strong>for</strong>hematocrit only and coagulation (PT, APTT, or fibrinogen) only?are introducing consolidated <strong>hematology</strong> workstations that areoperated by robotics and in<strong>for</strong>mation technology. Although not yetavailable, one could add a coagulation analyzer to this workstationand have the CBCs and coagulation tests per<strong>for</strong>med from the samevial with the aid <strong>of</strong> computerized (programmed) articulated robots.Technically, the use <strong>of</strong> <strong>citrate</strong>d samples provides opportunites toexpand and improve evaluation <strong>of</strong> platelets. It also would open newavenues to investigate whether <strong>sodium</strong> <strong>citrate</strong> is acceptable <strong>for</strong> thepotential incorporation <strong>of</strong> limited cytometric functions(immunophenotyping) with the more advanced <strong>hematology</strong> analyzerssuch as the CELL-DYN 4000.The data presented support the premise that <strong>sodium</strong> <strong>citrate</strong>samples provide similar interpretation <strong>of</strong> results within the normalrange when compared with previously established ranges. Becausethis conversion would happen over time, work flow systems wouldbe designed to accommodate both <strong>anticoagulant</strong>s <strong>for</strong> a while. Thesesystems may be achieved with existing bar code technology, whichcurrently deciphers whether a CBC gets a differential.The observation made in this study needs to be confirmedacross the wide range <strong>of</strong> <strong>hematology</strong> conditions and varying laboratorypractices and instrumentations.Additional and more comprehensive studies are necessary toaddress the limitations <strong>of</strong> this study, as listed in Table 4.REFERENCES1 KOEPKE JA: Tips on technology. MLO Med Lab Obs 13:15, 19812 CARTWRIGHT GE: Diagnostic Laboratory Hematology, 4th edition. NewYork, NY, Grune & Stratton, 1968, p. 273 NATIONAL COMMITTEE FOR CLINICAL LABORATORY STANDARDS: Evacuatedtubes and additives <strong>for</strong> blood specimen collection, 4th edition.Approved Standard. NCCLS Document H1-A4, Villanova, PA, 19964 INTERNATIONAL COUNCIL FOR STANDARDIZATION IN HEMATOLOGY:Expert panel on cytometry recommendations <strong>of</strong> the International Council<strong>for</strong> Standardization in Hematology <strong>for</strong> ethylene diamine tetraacetic acidanticoagulation <strong>of</strong> blood <strong>for</strong> blood cell counting and sizing. Am J ClinPathol 100:371, 19935 SAVAGE RA: Pseudoleukocytosis due to EDTA-induced platelet clumping.Am J Clin Pathol 81:317, 19846 RABINOVITCH A: Anticoagulants, platelets and instrument problems. Am JClin Pathol 82:132, 19847 KOEPKE JA: Laboratory Hematology. New York, NY, Churchill Livingstone,19848 CELL-DYN ® 4000: Principles <strong>of</strong> Operation, revision 3. Abbott Park, IL,Abbott Diagnostics, 19979 CELL-DYN ® 4000: DataLog Extract Procedure <strong>for</strong> the Efficiency Evaluation<strong>of</strong> the CELL-DYN ® 4000. Abbott Park, IL, Abbott Diagnostics, 199710 HUYN BH, ASHTON JK, DOLAN K: Practical Hematology: A LaboratoryGuide With Accompanying Filmstrips. Philadelphia, PA, WB Saunders, 197511 BRUNSON D, SMITH D, BAK A, PRZYK E, SHERIDAN B, MUNCER D: Comparing<strong>hematology</strong> <strong>anticoagulant</strong>s: K2EDTA vs. K3EDTA. Lab Hematol1:112, 199512 LIPPI U, SCHINELLA M, MODENA N, NICOLI M, LIPPI G: Advantages <strong>of</strong> anew <strong>anticoagulant</strong> in <strong>routine</strong> <strong>hematology</strong> on the Coulter Counter S PlusSTKR analyzer. Am J Clin Pathol 93:760, 199013 GULATI GL, ASSELTA A, CHEN C: Using vortex to disaggregate plateletclumps. Lab Med 28:665, 199714 WILKINSON DS: The role <strong>of</strong> technology in the clinical laboratory <strong>of</strong> thefuture. Clin Lab Manage Rev 11:322, 1997