Medicare Part B Newsline March 2012 - Cahaba GBA
Medicare Part B Newsline March 2012 - Cahaba GBA
Medicare Part B Newsline March 2012 - Cahaba GBA
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
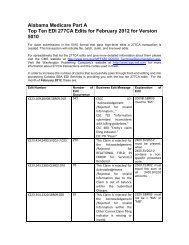
Alabama <strong>Medicare</strong> <strong>Part</strong> BTop Five Reasons for EDI Claim Rejections for January <strong>2012</strong>Audit trails show which of your claims were accepted by the <strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A processing system, alongwith claims that were rejected and the reason for the rejection. Referring to this report will allow you tocorrect and resubmit claims quickly, resulting in a dramatically reduced turnaround time. You will alsobecome aware of any major problems with your claims so they can be corrected before they create aninterruption in your cash flow. Audit trail reports are available the next business day for files that arereceived before 3:30 p.m. Central Time. If you are not receiving your audit trails contact your softwarevendor, billing service, or clearing house.See Audit Trail Explanations for a more complete list of edits, along with descriptions of loops that mightbe referenced in an edit.In order to increase the number of claims that successfully pass through audit trails and into processing<strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A EDI Services is providing you with the top five reasons for claim rejections. For themonth of January <strong>2012</strong>, these are:Claim DescriptionRejection213 INVALID PAYER ID OR QUAL IN 2010BBA payer ID or qualifier was submitted in the 2010BB loop(Payer Name) that is not valid for <strong>Medicare</strong> <strong>Part</strong> B.434 PROC CODE REQUIRES REFERRING NPIProcedure code billed was for a diagnostic procedure such as anx-ray or lab work which requires the NPI of the orderingphysician, or a consultation, which requires the NPI of thereferring physician, and this was not submitted on the claim.421 DIAG CODE (XXXXX) INVALID FOR DATE SVCThe date of service was outside of the effective date range ofthe diagnosis code used. The invalid diagnosis code will appearinside the parenthesis.888 INSTREAM REJECTIONThere was a problem involving HIPAA required loops,segments, or values. The specific loop will be identified, forexample, 'ELEMENT N401 (D.E. 19) AT COL. 4 ISMISSING, THOUGH MARKED "MUST BE USED"(LOOP:2010BA POS:3140)'. The number after 'POS' indicatesthe position in the file where the error occurred377 PAID & ADJUSTMENT AMOUNTS DO NOT EQUALCLAIM CHARGThe claim was submitted as <strong>Medicare</strong> Secondary Payer but theprimary paid amount plus the primary adjustment amounts donot equal the total claim charge.Number ofClaims701689595447439<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 10