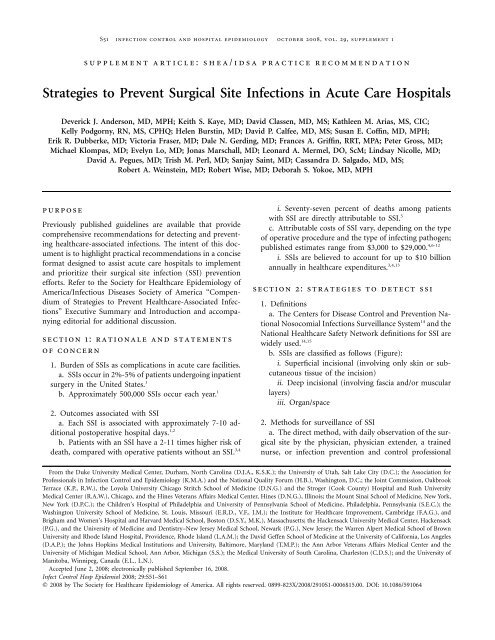
Strategies to Prevent Surgical Site Infections in Acute Care Hospitals
Strategies to Prevent Surgical Site Infections in Acute Care Hospitals
Strategies to Prevent Surgical Site Infections in Acute Care Hospitals
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
S52 <strong>in</strong>fection control and hospital epidemiology oc<strong>to</strong>ber 2008, vol. 29, supplement 1figure. The Centers for Disease Control and <strong>Prevent</strong>ion National Healthcare Safety Network classification for surgical site <strong>in</strong>fection(SSI). Reproduced from Horan et al. 14start<strong>in</strong>g 24-48 hours after surgery, is the most accuratemethod of surveillance. 2,16-18i. Although the direct method is used as the “goldstandard” for studies, it is rarely used <strong>in</strong> practice becauseof its resource utilization requirements andimpracticality.b. The <strong>in</strong>direct method of SSI surveillance consists of acomb<strong>in</strong>ation of the follow<strong>in</strong>g:i. Review of microbiology reports and patient medicalrecordsii. Surgeon and/or patient surveysiii. Screen<strong>in</strong>g for readmission of surgical patientsiv. Other <strong>in</strong>formation, such as coded diagnoses oroperative reportsc. The <strong>in</strong>direct method of SSI surveillance is less timeconsum<strong>in</strong>g and can be readily performed by <strong>in</strong>fection preventionand control personnel dur<strong>in</strong>g surveillance rounds.d. The <strong>in</strong>direct method of SSI surveillance is both reliable(sensitivity, 84%-89%) and specific (specificity,99.8%), compared with the “gold standard” of directsurveillance. 19,20e. Au<strong>to</strong>mated data systems can be used <strong>to</strong> broaden SSIsurveillance.i. SSI surveillance can be expanded by us<strong>in</strong>g hospitaldatabases that <strong>in</strong>clude data on adm<strong>in</strong>istrative claims,days of antimicrobial use, readmission <strong>to</strong> the hospital,and return <strong>to</strong> the operat<strong>in</strong>g room, and/or by implement<strong>in</strong>ga system that imports au<strong>to</strong>mated microbiologicculture data, surgical procedure data, and general demographic<strong>in</strong>formation <strong>in</strong><strong>to</strong> a s<strong>in</strong>gle surveillance database.21-23ii. These methods improve the sensitivity of <strong>in</strong>directsurveillance for detection of SSI and reduce theneed for efforts by <strong>in</strong>fection prevention and controlprofessionals. 213. Postdischarge surveillancea. <strong>Surgical</strong> procedures have been shift<strong>in</strong>g <strong>to</strong> the outpatientsett<strong>in</strong>g dur<strong>in</strong>g the past 3 decades. 24i. Patients now have shorter pos<strong>to</strong>perative stays. 25b. No standardized or reliable method for postdischargesurveillance has been established. Different methods ofpostdischarge/outpatient SSI surveillance have been employed.Postdischarge surveillance based on surgeon andpatient questionnaire results have been shown <strong>to</strong> have poorsensitivity and specificity. Regardless of which method isused, the overall rate of SSI for an <strong>in</strong>stitution typically<strong>in</strong>creases after postdischarge surveillance methods areimplemented. 26c. SSIs occurr<strong>in</strong>g and managed <strong>in</strong> the outpatient sett<strong>in</strong>gare usually superficial <strong>in</strong>cisional <strong>in</strong>fections. In contrast,deep <strong>in</strong>cisional and organ/space <strong>in</strong>fections typically requirereadmission <strong>to</strong> the hospital for management.section 3: strategies <strong>to</strong> prevent ssi1. Exist<strong>in</strong>g guidel<strong>in</strong>es, recommendations, and requirementsa. Hospital Infection Control Practices Advisory Committeeguidel<strong>in</strong>esi. The most recently published guidel<strong>in</strong>es for preventionof SSI were released <strong>in</strong> 1999 by Mangram et al. 5ii. The pathogenesis of and likelihood of develop<strong>in</strong>g
table 1.Selected Risk Fac<strong>to</strong>rs for and Recommendations <strong>to</strong> <strong>Prevent</strong> <strong>Surgical</strong> <strong>Site</strong> <strong>Infections</strong> (SSIs)Risk fac<strong>to</strong>r Recommendation Grade aIntr<strong>in</strong>sic, patient related (preoperative)UnmodifiableAgeModifiableGlucose control, diabetesObesitySmok<strong>in</strong>g cessationImmunosuppressive medicationsExtr<strong>in</strong>sic, procedure related (perioperative)Preparation of patientHair removalabPreoperative <strong>in</strong>fectionsOperative characteristics<strong>Surgical</strong> scrub (surgical team members’hands and forearms)Sk<strong>in</strong> preparationNo formal recommendation: relationship <strong>to</strong> <strong>in</strong>creased riskof SSI may be secondary <strong>to</strong> comorbidities or immunesenescence [28-30]Control serum blood glucose levels [5]; reduce glycosylatedhemoglob<strong>in</strong> A1c levels <strong>to</strong> !7% before surgery, ifpossible [31]Increase dos<strong>in</strong>g of prophylactic antimicrobial agent formorbidly obese patients [32]Encourage smok<strong>in</strong>g cessation with<strong>in</strong> 30 days beforeprocedure [5]No formal recommendation; <strong>in</strong> general, avoid immunosuppressivemedications <strong>in</strong> perioperative period, ifpossibleDo not remove unless hair will <strong>in</strong>terfere with the operation[5]; if hair removal is necessary, remove by clipp<strong>in</strong>gand do not use razorsIdentify and treat <strong>in</strong>fections (eg, ur<strong>in</strong>ary tract <strong>in</strong>fection)remote <strong>to</strong> the surgical site before elective surgery [5]Use appropriate antiseptic agent <strong>to</strong> perform 2-5–m<strong>in</strong>utepreoperative surgical scrub [5] or use an alcohol-basedsurgical hand antisepsis productWash and clean sk<strong>in</strong> around <strong>in</strong>cision site; use an appropriateantiseptic agent [5]Antimicrobial prophylaxis Adm<strong>in</strong>ister only when <strong>in</strong>dicated [5] A-ITim<strong>in</strong>gAdm<strong>in</strong>ister with<strong>in</strong> 1 hour before <strong>in</strong>cision <strong>to</strong> maximize A-Itissue concentration b [5, 33]ChoiceSelect appropriate agents on the basis of surgical procedure,most common pathogens caus<strong>in</strong>g SSI for aspecific procedure, and published recommendations [5,33]A-IDuration of therapyS<strong>to</strong>p prophylaxis with<strong>in</strong> 24 hours after the procedure forall procedures except cardiac surgery; for cardiacsurgery, antimicrobial prophylaxis should be s<strong>to</strong>ppedwith<strong>in</strong> 48 hours [5, 33]Surgeon skill/technique Handle tissue carefully and eradicate dead space [5] A-IIIAsepsisAdhere <strong>to</strong> standard pr<strong>in</strong>ciples of operat<strong>in</strong>g room asepsis A-III[5]Operative timeNo formal recommendation <strong>in</strong> most recent guidel<strong>in</strong>es;m<strong>in</strong>imize as much as possible [34]A-IIIOperat<strong>in</strong>g room characteristicsVentilationFollow American Institute of Architects’ recommendationsC-I[5]Traffic M<strong>in</strong>imize operat<strong>in</strong>g room traffic [5] B-IIEnvironmental surfacesUse a US Environmental Protection Agency–approvedhospital dis<strong>in</strong>fectant <strong>to</strong> clean surfaces and equipment[5]B-IIISterilization of surgical equipmentSee Table 2 for def<strong>in</strong>itions.Vancomyc<strong>in</strong> and fluoroqu<strong>in</strong>olones can be given 2 hours before <strong>in</strong>cision.Sterilize all surgical equipment accord<strong>in</strong>g <strong>to</strong> publishedguidel<strong>in</strong>es; m<strong>in</strong>imize the use of flash sterilization [5]…A-IIA-IIA-IIC-IIA-IA-IIA-IIA-IIA-IB-I
strategies for prevention of ssiS55b<strong>in</strong>ed <strong>in</strong><strong>to</strong> concise, efficient, and effective recommendationsthat are easily unders<strong>to</strong>od and remembered. 39ii. Provide education regard<strong>in</strong>g the outcomes associatedwith SSI, risks for SSI, and methods <strong>to</strong> reducerisk <strong>to</strong> all patients, patients’ families, surgeons, and perioperativepersonnel.iii. Education for patients and patients’ families is aneffective method <strong>to</strong> reduce risk associated with <strong>in</strong>tr<strong>in</strong>sicpatient-related SSI risk fac<strong>to</strong>rs. 40,41c. Computer-assisted decision support and au<strong>to</strong>matedrem<strong>in</strong>dersi. Several <strong>in</strong>stitutions have successfully employedcomputer-assisted decision-support methodology <strong>to</strong> improvethe rate of appropriate adm<strong>in</strong>istration of antimicrobialprophylaxis (<strong>in</strong>clud<strong>in</strong>g redos<strong>in</strong>g dur<strong>in</strong>g prolongedcases). 42-44ii. Computer-assisted decision support, however, ispotentially expensive, can be time consum<strong>in</strong>g <strong>to</strong> implement,and, <strong>in</strong> a s<strong>in</strong>gle study, was reported <strong>to</strong> <strong>in</strong>itially<strong>in</strong>crease the rate of adverse drug reactions. 45iii. Institutions must appropriately validate computer-assisteddecision-support systems after implementation.d. Utilization of au<strong>to</strong>mated datai. Install <strong>in</strong>formation technology <strong>in</strong>frastructure <strong>to</strong> facilitatedata transfer, receipt, and organization <strong>to</strong> aid withthe track<strong>in</strong>g of process and outcome measures.section 4: recommendations forimplement<strong>in</strong>g prevention andmoni<strong>to</strong>r<strong>in</strong>g strategiesRecommendations for prevent<strong>in</strong>g and moni<strong>to</strong>r<strong>in</strong>g SSIs aresummarized <strong>in</strong> the follow<strong>in</strong>g section. They are designed <strong>to</strong>assist acute care hospitals <strong>in</strong> prioritiz<strong>in</strong>g and implement<strong>in</strong>gtheir SSI prevention efforts. Criteria for grad<strong>in</strong>g of thestrength of recommendation and quality of evidence are described<strong>in</strong> Table 2.I. Basic practices for prevention and moni<strong>to</strong>r<strong>in</strong>g of SSI:recommended for all acute care hospitalsA. Surveillance of SSI1. Perform surveillance for SSI (A-II).a. Identify high-risk, high-volume operative procedures<strong>to</strong> be targeted for SSI surveillance on the basis of a riskassessment of patient populations, operative proceduresperformed, and available SSI surveillance data.b. Identify, collect, s<strong>to</strong>re, and analyze data needed forthe surveillance program. 5i. Implement a system for collect<strong>in</strong>g data needed <strong>to</strong>identify SSIs.ii. Develop a database for s<strong>to</strong>r<strong>in</strong>g, manag<strong>in</strong>g, and access<strong>in</strong>gcollected data on SSIs.iii. Prepare periodic SSI reports (the time frame willdepend on hospital needs and volume of targetedprocedures).iv. Collect denom<strong>in</strong>a<strong>to</strong>r data on all patients undergo<strong>in</strong>gtargeted procedures, <strong>to</strong> calculate SSI rates for eachtype of procedure. 39v. Identify trends (eg, <strong>in</strong> rates of SSI and pathogenscaus<strong>in</strong>g SSIs).c. Use Centers for Disease Control and <strong>Prevent</strong>ion NationalHealthcare Safety Network def<strong>in</strong>itions of SSI. 14d. Perform <strong>in</strong>direct surveillance for targeted procedures.19,20,47,48e. Perform pos<strong>to</strong>perative surveillance for 30 days; extendthe pos<strong>to</strong>perative surveillance period <strong>to</strong> 12 months ifprosthetic material is implanted dur<strong>in</strong>g surgery. 14f. Surveillance should be performed for patients readmitted<strong>to</strong> the hospital.i. If an SSI is diagnosed at your <strong>in</strong>stitution but thesurgical procedure was performed elsewhere, notify thehospital where the orig<strong>in</strong>al procedure was performed.g. Develop a system for rout<strong>in</strong>e review and <strong>in</strong>terpretationof SSI rates <strong>to</strong> detect significant <strong>in</strong>creases or outbreaksand <strong>to</strong> identify areas where additional resourcesmight be needed <strong>to</strong> improve SSI rates. 472. Provide ongo<strong>in</strong>g feedback on SSI surveillance and processmeasures <strong>to</strong> surgical and perioperative personnel andleadership (A-II).a. Rout<strong>in</strong>ely provide feedback on SSI rates and processmeasures <strong>to</strong> <strong>in</strong>dividual surgeons and hospital leadership. 5i. For each type of procedure performed, provide riskadjustedrates of SSI.ii. Anonymously benchmark procedure-specific riskadjustedrates of SSI among peer surgeons. 5b. Confidentially provide data <strong>to</strong> <strong>in</strong>dividual surgeons,the surgical division, and/or department chiefs.3. Increase the efficiency of surveillance through the useof au<strong>to</strong>mated data (A-II).a. Implement a method <strong>to</strong> electronically transfer operativedata, <strong>in</strong>clud<strong>in</strong>g process measures when available, <strong>to</strong><strong>in</strong>fection prevention and control personnel <strong>to</strong> facilitate acquisitionof denom<strong>in</strong>a<strong>to</strong>r data and calculation of SSI ratesfor various procedures.b. If <strong>in</strong>formation technology and <strong>in</strong>frastructure resourcesare available, develop au<strong>to</strong>mated methods for detectionof SSI by use of au<strong>to</strong>mated data on readmissions,microbiological test results, and antimicrobial dispens<strong>in</strong>g. 23i. Implementation of au<strong>to</strong>mated surveillance may improvethe sensitivity of surveillance.B. Practice1. Adm<strong>in</strong>ister antimicrobial prophylaxis <strong>in</strong> accordancewith evidence-based standards and guidel<strong>in</strong>es (A-I). 5,49,50
S56 <strong>in</strong>fection control and hospital epidemiology oc<strong>to</strong>ber 2008, vol. 29, supplement 1table 2.Category/gradeStrength of Recommendation and Quality of EvidenceStrength of recommendationABCQuality of evidenceIIIIIIDef<strong>in</strong>itionGood evidence <strong>to</strong> support a recommendation for useModerate evidence <strong>to</strong> support a recommendation for usePoor evidence <strong>to</strong> support a recommendationEvidence from x1 properly randomized, controlled trialEvidence from x1 well-designed cl<strong>in</strong>ical trial, withoutrandomization; from cohort or case-control analyticstudies (preferably from 11 center); from multipletime series; or from dramatic results from uncontrolledexperimentsEvidence from op<strong>in</strong>ions of respected authorities, basedon cl<strong>in</strong>ical experience, descriptive studies, or reports ofexpert committeesnote. Adapted from the Canadian Task Force on the Periodic Health Exam<strong>in</strong>ation. 46a. Adm<strong>in</strong>ister prophylaxis with<strong>in</strong> 1 hour before <strong>in</strong>cision<strong>to</strong> maximize tissue concentration. 33,35i. Two hours are allowed for the adm<strong>in</strong>istration ofvancomyc<strong>in</strong> and fluoroqu<strong>in</strong>olones.b. Select appropriate agents on the basis of the surgicalprocedure, the most common pathogens caus<strong>in</strong>g SSI for aspecific procedure, and published recommendations. 33,35c. Discont<strong>in</strong>ue prophylaxis with<strong>in</strong> 24 hours after surgeryfor most procedures; discont<strong>in</strong>ue with<strong>in</strong> 48 hours for cardiacprocedures. 33,352. Do not remove hair at the operative site unless thepresence of hair will <strong>in</strong>terfere with the operation; do not userazors (A-II). 5a. If hair removal is necessary, remove it by clipp<strong>in</strong>g orby use of a depila<strong>to</strong>ry agent.3. Control blood glucose level dur<strong>in</strong>g the immediate pos<strong>to</strong>perativeperiod for patients undergo<strong>in</strong>g cardiac surgery (A-I). 35a. Ma<strong>in</strong>ta<strong>in</strong> the pos<strong>to</strong>perative blood glucose level at lessthan 200 mg/dL.i. Measure blood glucose level at 6:00 am on pos<strong>to</strong>perativeday 1 and pos<strong>to</strong>perative day 2, with the procedureday be<strong>in</strong>g pos<strong>to</strong>perative day 0.b. Initiat<strong>in</strong>g close blood glucose control <strong>in</strong> the <strong>in</strong>traoperativeperiod has not been shown <strong>to</strong> reduce the risk ofSSI, compared with start<strong>in</strong>g blood glucose control <strong>in</strong> thepos<strong>to</strong>perative period. In fact, a recently performed randomizedcontrolled trial showed that <strong>in</strong>itiat<strong>in</strong>g close glucosecontrol dur<strong>in</strong>g cardiac surgery may actually lead <strong>to</strong>higher rates of adverse outcomes, <strong>in</strong>clud<strong>in</strong>g stroke anddeath. 514. Measure and provide feedback <strong>to</strong> providers on the ratesof compliance with process measures, <strong>in</strong>clud<strong>in</strong>g antimicrobialprophylaxis, proper hair removal, and glucose control (forcardiac surgery) (A-III). 35a. Rout<strong>in</strong>ely provide feedback <strong>to</strong> surgical staff and leadership,regard<strong>in</strong>g compliance with targeted process measures.5. Implement policies and practices aimed at reduc<strong>in</strong>g therisk of SSI that meet regula<strong>to</strong>ry and accreditation requirementsand that are aligned with evidence-based standards(eg, Centers for Disease Control and <strong>Prevent</strong>ion and professionalorganization guidel<strong>in</strong>es) (A-II). 5,35,36a. Policies and practices should <strong>in</strong>clude but are not limited<strong>to</strong> the follow<strong>in</strong>g:i. Reduc<strong>in</strong>g modifiable patient risk fac<strong>to</strong>rsii. Optimal clean<strong>in</strong>g and dis<strong>in</strong>fection of equipmentand the environmentiii. Optimal preparation and dis<strong>in</strong>fection of the operativesite and the hands of the surgical team membersiv. Adherence <strong>to</strong> hand hygienev. Traffic control <strong>in</strong> operat<strong>in</strong>g roomsvi. See Table 1 for a more detailed list.C. Education1. Educate surgeons and perioperative personnel about SSIprevention (A-III).a. Include risk fac<strong>to</strong>rs, outcomes associated with SSI,local epidemiology (eg, SSI rates by procedure and the rateof methicill<strong>in</strong>-resistant Staphylococcus aureus [MRSA] <strong>in</strong>fection<strong>in</strong> a facility), and basic prevention measures.2. Educate patients and their families about SSI prevention,as appropriate (A-III).a. Provide <strong>in</strong>structions and <strong>in</strong>formation <strong>to</strong> patients beforesurgery, describ<strong>in</strong>g strategies for reduc<strong>in</strong>g SSI risk.Specifically provide prepr<strong>in</strong>ted materials <strong>to</strong> patients.
strategies for prevention of ssiS57b. Examples of pr<strong>in</strong>ted materials for patients are availablefrom the follow<strong>in</strong>g Web pages:i. JAMA patient page: wound <strong>in</strong>fections (from theJournal of the American Medical Association; available at:http://jama.ama-assn.org/cgi/repr<strong>in</strong>t/294/16/2122)ii. <strong>Surgical</strong> <strong>Care</strong> Improvement Project consumer <strong>in</strong>fosheet (available at: http://www.ofmq.com/Websites/ofmq/Images/FINALconsumer_tips2.pdf)iii. What you need <strong>to</strong> know about <strong>in</strong>fections aftersurgery: a fact sheet for patients and their family members(available at: http://www.ihi.org/NR/rdonlyres/0EE409F4-2F6A-4B55-AB01-16B6D6935EC5/0/<strong>Surgical</strong><strong>Site</strong><strong>Infections</strong>PtsandFam.pdf)D. Accountability1. The hospital’s chief executive officer and senior managementare responsible for ensur<strong>in</strong>g that the healthcare systemsupports an <strong>in</strong>fection prevention and control programthat effectively prevents the occurrence of SSIs and the transmissionof epidemiologically significant pathogens.2. Senior management is accountable for ensur<strong>in</strong>g that anadequate number of tra<strong>in</strong>ed personnel are assigned <strong>to</strong> the<strong>in</strong>fection prevention and control program.3. Senior management is accountable for ensur<strong>in</strong>g thathealthcare personnel, <strong>in</strong>clud<strong>in</strong>g licensed and nonlicensed personnel,are competent <strong>to</strong> perform their job responsibilities.4. Direct healthcare providers (such as physicians, nurses,aides, and therapists) and ancillary personnel (such as housekeep<strong>in</strong>gand equipment-process<strong>in</strong>g personnel) are responsiblefor ensur<strong>in</strong>g that appropriate <strong>in</strong>fection prevention and controlpractices are used at all times (<strong>in</strong>clud<strong>in</strong>g hand hygiene;strict adherence <strong>to</strong> aseptic technique; clean<strong>in</strong>g and dis<strong>in</strong>fectionof equipment and the environment; clean<strong>in</strong>g, dis<strong>in</strong>fection,and sterilization of medical supplies and <strong>in</strong>struments;and appropriate surgical prophylaxis pro<strong>to</strong>cols).5. Hospital and unit leaders are responsible for hold<strong>in</strong>gpersonnel accountable for their actions.6. The person that manages the <strong>in</strong>fection prevention andcontrol program is responsible for ensur<strong>in</strong>g that an activeprogram <strong>to</strong> identify SSIs is implemented, that data on SSIsare analyzed and regularly provided <strong>to</strong> those who can use the<strong>in</strong>formation <strong>to</strong> improve the quality of care (eg, unit staff,cl<strong>in</strong>icians, and hospital adm<strong>in</strong>istra<strong>to</strong>rs), and that evidencebasedpractices are <strong>in</strong>corporated <strong>in</strong><strong>to</strong> the program.7. Personnel responsible for healthcare personnel and patienteducation are accountable for ensur<strong>in</strong>g that appropriatetra<strong>in</strong><strong>in</strong>g and educational programs <strong>to</strong> prevent SSIs are developedand provided <strong>to</strong> personnel, patients, and families.8. Personnel from the <strong>in</strong>fection prevention and controlprogram, the labora<strong>to</strong>ry, and <strong>in</strong>formation technology departmentsare responsible for ensur<strong>in</strong>g that systems are <strong>in</strong>place <strong>to</strong> support the surveillance program.II. Special approaches for the prevention of SSIPerform an SSI risk assessment. These special approaches arerecommended for use <strong>in</strong> locations and/or populations with<strong>in</strong>the hospital that have unacceptably high SSI rates despiteimplementation of the basic SSI prevention strategies listedabove.1. Perform expanded SSI surveillance <strong>to</strong> determ<strong>in</strong>e thesource and extent of the problem and <strong>to</strong> identify possibletargets for <strong>in</strong>tervention (B-II).a. Expand surveillance <strong>to</strong> <strong>in</strong>clude additional proceduresand possibly <strong>to</strong> all National Healthcare Safety Networkprocedures. 5 Align expanded surveillance with the hospital’sstrategic plan.III. Approaches that should not be considered a rout<strong>in</strong>epart of SSI prevention1. Do not rout<strong>in</strong>ely use vancomyc<strong>in</strong> for antimicrobial prophylaxis(B-II).a. Vancomyc<strong>in</strong> should not rout<strong>in</strong>ely be used for antimicrobialprophylaxis, but it can be an appropriate agentfor specific scenarios. Reserve vancomyc<strong>in</strong> for specific cl<strong>in</strong>icalcircumstances, such as a proven outbreak of SSI due<strong>to</strong> MRSA, high endemic rates of SSI due <strong>to</strong> MRSA, targetedhigh-risk patients who are at <strong>in</strong>creased risk for SSI due <strong>to</strong>MRSA (<strong>in</strong>clud<strong>in</strong>g cardiothoracic surgical patients and elderlypatients with diabetes), and high-risk surgical proceduresdur<strong>in</strong>g which an implant is placed. 52i. No def<strong>in</strong>itions for “high endemic rates of SSI due<strong>to</strong> MRSA” have been established.ii. Studies of the efficacy of vancomyc<strong>in</strong> prophylaxiswere published before the emergence of communityacquiredMRSA.b. A recent meta-analysis of 7 studies compar<strong>in</strong>g glycopeptideprophylaxis with b-lactam prophylaxis beforecardiothoracic surgery showed that there was no difference<strong>in</strong> rates of SSI between the 2 antimicrobial prophylaxisregimens. 53c. No study has prospectively analyzed the effect of provid<strong>in</strong>gboth glycopeptide and b-lactam antimicrobials forpreoperative antimicrobial prophylaxis. Thus, it is unclearwhether treatment with vancomyc<strong>in</strong>, when <strong>in</strong>dicated,should be added <strong>to</strong> or used <strong>in</strong> place of standard recommendedantimicrobial prophylaxis. Because vancomyc<strong>in</strong>does not have activity aga<strong>in</strong>st gram-negative pathogens,some experts recommend add<strong>in</strong>g vancomyc<strong>in</strong> treatment <strong>to</strong>standard antimicrobial prophylaxis for the specific cl<strong>in</strong>icalcircumstances described above.
S58 <strong>in</strong>fection control and hospital epidemiology oc<strong>to</strong>ber 2008, vol. 29, supplement 12. Do not rout<strong>in</strong>ely delay surgery <strong>to</strong> provide parenteralnutrition (A-I).a. Preoperative adm<strong>in</strong>istration of <strong>to</strong>tal parenteral nutritionhas not been shown <strong>to</strong> reduce the risk of SSI <strong>in</strong>prospective, randomized controlled trials and may <strong>in</strong>creasethe risk of SSI. 54,55IV. Unresolved issues1. Preoperative bath<strong>in</strong>g with chlorhexid<strong>in</strong>e-conta<strong>in</strong><strong>in</strong>gproductsa. Preoperative shower<strong>in</strong>g with agents such as chlorhexid<strong>in</strong>ehas been shown <strong>to</strong> reduce bacterial colonizationof the sk<strong>in</strong>. 56 Several studies have exam<strong>in</strong>ed the utility ofpreoperative showers, but none has def<strong>in</strong>itively proven thatthey decrease SSI risk. A recent Cochrane review 57 evaluatedthe evidence for preoperative bath<strong>in</strong>g or shower<strong>in</strong>g withantiseptics for SSI prevention. Six randomized, controlledtrials evaluat<strong>in</strong>g the use of 4% chlorhexid<strong>in</strong>e gluconatewere <strong>in</strong>cluded <strong>in</strong> the analysis, with no clear evidence ofbenefit noted. To ga<strong>in</strong> the maximum antiseptic effect ofchlorhexid<strong>in</strong>e, it must be allowed <strong>to</strong> dry completely andnot be washed off.2. Rout<strong>in</strong>e screen<strong>in</strong>g for MRSA or rout<strong>in</strong>e attempts <strong>to</strong>decolonize surgical patients with an antistaphylococcal agent<strong>in</strong> the preoperative sett<strong>in</strong>ga. A recent double-bl<strong>in</strong>ded, randomized, controlled trial<strong>in</strong>volv<strong>in</strong>g more than 4,000 patients showed that <strong>in</strong>tranasalapplication of mupiroc<strong>in</strong> did not significantly reduce theS. aureus SSI rate. 58 In a secondary analysis of these data,however, the use of <strong>in</strong>tranasal mupiroc<strong>in</strong> was associatedwith an overall decreased rate of nosocomial S. aureus <strong>in</strong>fectionamong the S. aureus carriers. 58 Mupiroc<strong>in</strong> resistancehas been documented. 59b. In contrast, other studies have suggested that mupiroc<strong>in</strong>may be effective for particular patient groups, <strong>in</strong>clud<strong>in</strong>gpatients undergo<strong>in</strong>g orthopedic 60,61 or cardiothoracic 62,63surgery. However, these were not randomized controlledtrials.3. Ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g oxygenation with supplemental oxygendur<strong>in</strong>g and after colorectal proceduresa. Three randomized cl<strong>in</strong>ical trials have been publishedcompar<strong>in</strong>g 80% fraction of <strong>in</strong>spired oxygen (FiO 2 ) with30%-35% FiO 2 dur<strong>in</strong>g the <strong>in</strong>tra- and pos<strong>to</strong>perative periods.i. Two trials showed a significant decrease <strong>in</strong> the rateof SSI associated with the higher FiO 2 value, 64,65 and oneactually showed a significant <strong>in</strong>crease <strong>in</strong> the rate of SSI. 66ii. Both studies with results show<strong>in</strong>g a beneficial effec<strong>to</strong>f supplemental oxygen <strong>in</strong>cluded patients who underwentcolorectal surgery, whereas the study with resultsshow<strong>in</strong>g a negative effect of supplemental oxygen <strong>in</strong>cludedall types of patients.iii. When results of the 3 studies are pooled, the rateof SSI decreases from 15.2% among patients who received30%-35% supplemental FiO 2 <strong>to</strong> 11.5% amongpatients who received 80% FiO 2 dur<strong>in</strong>g surgery (3.7%absolute risk reduction; P p .10). 674. Ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g normothermia (temperature higher than36.0C) immediately after colorectal surgerya. One randomized trial with 200 patients undergo<strong>in</strong>gcolorectal surgery found that <strong>in</strong>fection rates were significantlyreduced among patients randomized <strong>to</strong> have normothermiama<strong>in</strong>ta<strong>in</strong>ed dur<strong>in</strong>g surgery. 68b. Controversy still exists regard<strong>in</strong>g this recommendation,because of the follow<strong>in</strong>g:i. The trial exam<strong>in</strong>ed the effect of <strong>in</strong>traoperative normothermia,not pos<strong>to</strong>perative normothermia, and didnot <strong>in</strong>clude risk adjustment for type of procedure.ii. An observational study showed no impact of normothermiaon <strong>in</strong>fection rates. 695. Preoperative <strong>in</strong>tranasal and pharyngeal chlorhexid<strong>in</strong>etreatment for patients undergo<strong>in</strong>g cardiothoracic procedures70a. Although data exist from a randomized, controlledtrial <strong>to</strong> support its usage, chlorhexid<strong>in</strong>e nasal cream is neitherapproved by the US Food and Drug Adm<strong>in</strong>istrationnor commercially available <strong>in</strong> the United States.section 5: performance measuresI. Internal report<strong>in</strong>gThese performance measures are <strong>in</strong>tended <strong>to</strong> support <strong>in</strong>ternalhospital quality improvement efforts and do not necessarilyaddress external report<strong>in</strong>g needs.The process and outcome measures suggested here are derivedfrom published guidel<strong>in</strong>es, other relevant literature, andthe op<strong>in</strong>ion of the authors. Report process and outcome measures<strong>to</strong> senior hospital leadership, nurs<strong>in</strong>g leadership, andcl<strong>in</strong>icians who care for patients at risk for SSI.A. Process measures1. Compliance with antimicrobial prophylaxis guidel<strong>in</strong>esa. Measure the percentage of procedures <strong>in</strong> which antimicrobialprophylaxis was appropriately provided. Appropriateness<strong>in</strong>cludes (1) correct type of agent, (2) star<strong>to</strong>f adm<strong>in</strong>istration of the agent with<strong>in</strong> 1 hour before <strong>in</strong>cision(2 hours allowed for vancomyc<strong>in</strong> and fluoroqu<strong>in</strong>olones)and (3) discont<strong>in</strong>uation of the agent with<strong>in</strong> 24 hours aftersurgery (48 hours for cardiac procedures).i. Numera<strong>to</strong>r: number of patients who appropriatelyreceived antimicrobial prophylaxis.ii. Denom<strong>in</strong>a<strong>to</strong>r: <strong>to</strong>tal number of selected operationsperformed.iii. Multiply by 100 so that the measure is expressedas a percentage.
strategies for prevention of ssiS592. Compliance with hair-removal guidel<strong>in</strong>esa. Measure the percentage of procedures for which hairremoval is appropriately performed (ie, clipp<strong>in</strong>g, use of adepila<strong>to</strong>ry, or no hair removal, rather than use of a razor).i. Numera<strong>to</strong>r: number of patients with appropriateperioperative hair removal.ii. Denom<strong>in</strong>a<strong>to</strong>r: <strong>to</strong>tal number of selected operationsperformed.iii. Multiply by 100 so that the measure is expressedas a percentage.3. Compliance with perioperative glucose control guidel<strong>in</strong>esa. Measure the percentage of procedures for which serumglucose levels are ma<strong>in</strong>ta<strong>in</strong>ed below 200 mg/dL at6:00 am on pos<strong>to</strong>perative day 1 and pos<strong>to</strong>perative day 2after cardiac surgery.i. Numera<strong>to</strong>r: number of patients with appropriatelyma<strong>in</strong>ta<strong>in</strong>ed serum glucose at 6:00 am on both pos<strong>to</strong>perativeday 1 and pos<strong>to</strong>perative day 2 after cardiacsurgery.ii. Denom<strong>in</strong>a<strong>to</strong>r: <strong>to</strong>tal number of cardiac proceduresperformed.iii. Multiply by 100 so that measure is expressed asa percentage.B. Outcome measures1. <strong>Surgical</strong> site <strong>in</strong>fection ratea. Use National Healthcare Safety Network def<strong>in</strong>itionsand risk adjustment methods. 15i. Numera<strong>to</strong>r: number of patients with surgical site<strong>in</strong>fections after selected operations.ii. Denom<strong>in</strong>a<strong>to</strong>r: <strong>to</strong>tal number of selected operationsperformed.iii. Multiply by 100 so that measure is expressed asa percentage.iv. Risk adjustment: rates of SSI can be risk adjustedby use of one of 2 methods: stratification us<strong>in</strong>g the NationalNosocomial <strong>Infections</strong> Surveillance risk <strong>in</strong>dex 27 orcalculation of the standardized <strong>in</strong>fection ratio. 71(a) The National Nosocomial <strong>Infections</strong> Surveillancerisk <strong>in</strong>dex is a widely used, operation- and patient-specific,prospectively applied risk score that predictsSSI. 72 This risk <strong>in</strong>dex <strong>in</strong>cludes 3 predic<strong>to</strong>rs of<strong>in</strong>creased risk of SSI: estima<strong>to</strong>rs of wound microbialcontam<strong>in</strong>ation, duration of operation, and markersfor host susceptibility. 73 Because rates of SSI publishedby National Healthcare Safety Network <strong>in</strong>clude superficial<strong>in</strong>cisional <strong>in</strong>fections, it is appropriate <strong>to</strong> collectdata on superficial <strong>in</strong>cisional <strong>in</strong>fections for <strong>in</strong>ternalbenchmark<strong>in</strong>g.(b) The standardized <strong>in</strong>fection ratio (SIR) is theratio of the observed number of SSIs (O) that occurred<strong>to</strong> the expected number for surgeons perform<strong>in</strong>g aspecific type of procedure (E) (ie, SIR p O/E). 71 Theexpected number of SSIs can be obta<strong>in</strong>ed by multiply<strong>in</strong>gthe number of operations done by the surgeon<strong>in</strong> each procedure risk category by the National Nosocomial<strong>Infections</strong> Surveillance rate for the same procedurerisk category and divid<strong>in</strong>g by 100. Values thatexceed 1.0 <strong>in</strong>dicate that more SSIs than expectedoccurred.II. External report<strong>in</strong>gThere are many challenges <strong>in</strong> provid<strong>in</strong>g useful <strong>in</strong>formation<strong>to</strong> consumers and other stakeholders while prevent<strong>in</strong>g un<strong>in</strong>tendedadverse consequences of public report<strong>in</strong>g of healthcare-associated<strong>in</strong>fections. 74 Recommendations for public report<strong>in</strong>gof healthcare-associated <strong>in</strong>fections have beenprovided by the Hospital Infection Control Practices AdvisoryCommittee, 75 the Healthcare-Associated Infection Work<strong>in</strong>gGroup of the Jo<strong>in</strong>t Public Policy Committee, 76 and the NationalQuality Forum. 77The follow<strong>in</strong>g is an example of an external performancemeasure that is currently required by some healthcare stakeholdersand regula<strong>to</strong>rs.A. Process measure1. Compliance with Centers for Medicare and MedicaidServices antimicrobial prophylaxis guidel<strong>in</strong>es (see section5.I.A.1 above: Performance Measures; Internal Report<strong>in</strong>g;Process Measures)a. Measure the percentage of procedures <strong>in</strong> which antimicrobialprophylaxis was appropriately provided. Appropriateness<strong>in</strong>cludes correct type of agent, adm<strong>in</strong>istrationof the agent with<strong>in</strong> 1 hour before <strong>in</strong>cision (2 hours allowedfor vancomyc<strong>in</strong> and fluoroqu<strong>in</strong>olones), and discont<strong>in</strong>uationof the agent with<strong>in</strong> 24 hours after surgery (48 hoursfor cardiothoracic procedures). 38B. State and federal requirements1. Federal requirementsa. <strong>Hospitals</strong> that receive Medicare reimbursement mustcollect and report quality measures required by Centers forMedicare and Medicaid Services (see above).2. State requirementsa. <strong>Hospitals</strong> <strong>in</strong> states that have manda<strong>to</strong>ry report<strong>in</strong>g requirementsmust collect and report the data required bythe state. For <strong>in</strong>formation on state and federal requirements,check with your state or local health department.3. External quality <strong>in</strong>itiativesa. <strong>Hospitals</strong> that participate <strong>in</strong> external quality <strong>in</strong>itiativesmust collect and report the data if required by the<strong>in</strong>itiative.
S60 <strong>in</strong>fection control and hospital epidemiology oc<strong>to</strong>ber 2008, vol. 29, supplement 1acknowledgmentsFor Potential Conflicts of Interest statements and <strong>in</strong>formation on f<strong>in</strong>ancialsupport, please see the Acknowledgments <strong>in</strong> the Executive Summary, on pageS20 of this supplement.Address repr<strong>in</strong>t requests <strong>to</strong> the Repr<strong>in</strong>ts Coord<strong>in</strong>a<strong>to</strong>r, University of ChicagoPress, 1427 E. 60th St., Chicago, IL 60637 (repr<strong>in</strong>ts@press.uchicago.edu)or contact the journal office (iche@press.uchicago.edu).references1. Cruse P. Wound <strong>in</strong>fection surveillance. Rev Infect Dis 1981; 3:734-737.2. Cruse PJ, Foord R. The epidemiology of wound <strong>in</strong>fection: a 10-yearprospective study of 62,939 wounds. Surg Cl<strong>in</strong> North Am 1980; 60:27-40.3. Engemann JJ, Carmeli Y, Cosgrove SE, et al. Adverse cl<strong>in</strong>ical and economicoutcomes attributable <strong>to</strong> methicill<strong>in</strong> resistance among patientswith Staphylococcus aureus surgical site <strong>in</strong>fection. Cl<strong>in</strong> Infect Dis 2003;36:592-598.4. Kirkland KB, Briggs JP, Trivette SL, Wilk<strong>in</strong>son WE, Sex<strong>to</strong>n DJ. Theimpact of surgical-site <strong>in</strong>fections <strong>in</strong> the 1990s: attributable mortality,excess length of hospitalization, and extra costs. Infect Control HospEpidemiol 1999; 20:725-730.5. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guidel<strong>in</strong>efor prevention of surgical site <strong>in</strong>fection, 1999. Hospital Infection ControlPractices Advisory Committee. Infect Control Hosp Epidemiol 1999; 20:250-278; quiz 279-280.6. Coello R, Glenister H, Fereres J, et al. The cost of <strong>in</strong>fection <strong>in</strong> surgicalpatients: a case-control study. J Hosp Infect 1993; 25:239-250.7. Boyce JM, Potter-Bynoe G, Dziobek L. Hospital reimbursement patternsamong patients with surgical wound <strong>in</strong>fections follow<strong>in</strong>g open heartsurgery. Infect Control Hosp Epidemiol 1990; 11:89-93.8. Vegas AA, Jodra VM, Garcia ML. Nosocomial <strong>in</strong>fection <strong>in</strong> surgery wards:a controlled study of <strong>in</strong>creased duration of hospital stays and direct cos<strong>to</strong>f hospitalization. Eur J Epidemiol 1993; 9:504-510.9. VandenBergh MF, Kluytmans JA, van Hout BA, et al. Cost-effectivenessof perioperative mupiroc<strong>in</strong> nasal o<strong>in</strong>tment <strong>in</strong> cardiothoracic surgery.Infect Control Hosp Epidemiol 1996; 17:786-792.10. Hollenbeak CS, Murphy DM, Koenig S, Woodward RS, Dunagan WC,Fraser VJ. The cl<strong>in</strong>ical and economic impact of deep chest surgical site<strong>in</strong>fections follow<strong>in</strong>g coronary artery bypass graft surgery. Chest 2000;118:397-402.11. Whitehouse JD, Friedman ND, Kirkland KB, Richardson WJ, Sex<strong>to</strong>n DJ.The impact of surgical-site <strong>in</strong>fections follow<strong>in</strong>g orthopedic surgery at acommunity hospital and a university hospital: adverse quality of life,excess length of stay, and extra cost. Infect Control Hosp Epidemiol 2002;23:183-189.12. Apisarnthanarak A, Jones M, Waterman BM, Carroll CM, Bernardi R,Fraser VJ. Risk fac<strong>to</strong>rs for sp<strong>in</strong>al surgical-site <strong>in</strong>fections <strong>in</strong> a communityhospital: a case-control study. Infect Control Hosp Epidemiol 2003; 24:31-36.13. Wong ES. <strong>Surgical</strong> site <strong>in</strong>fections. In: Mayhall CG, ed. Hospital Epidemiologyand Infection Control. 3rd ed. Baltimore: Lipp<strong>in</strong>cott, Williams,and Wilk<strong>in</strong>s; 2004:287–310.14. Horan TC, Gaynes RP, Mar<strong>to</strong>ne WJ, Jarvis WR, Emori TG. CDC def<strong>in</strong>itionsof nosocomial surgical site <strong>in</strong>fections, 1992: a modification ofCDC def<strong>in</strong>itions of surgical wound <strong>in</strong>fections. Infect Control Hosp Epidemiol1992; 13:606-608.15. National Healthcare Safety Network (NHSN) members page. Availableat: http://www.cdc.gov/ncidod/dhqp/nhsn_members.html. Accessed August5, 2008.16. Condon RE, Schulte WJ, Malangoni MA, Anderson-Teschendorf MJ.Effectiveness of a surgical wound surveillance program. Arch Surg 1983;118:303-307.17. Kerste<strong>in</strong> M, Flower M, Harkavy LM, Gross PA. Surveillance for pos<strong>to</strong>perativewound <strong>in</strong>fections: practical aspects. Am Surg 1978; 44:210-214.18. Mead PB, Pories SE, Hall P, Vacek PM, Davis JH Jr, Gamelli RL. Decreas<strong>in</strong>gthe <strong>in</strong>cidence of surgical wound <strong>in</strong>fections: validation of a surveillance-notificationprogram. Arch Surg 1986; 121:458-461.19. Baker C, Luce J, Chenoweth C, Friedman C. Comparison of case-f<strong>in</strong>d<strong>in</strong>gmethodologies for endometritis after cesarean section. Am J Infect Control1995; 23:27-33.20. Cardo DM, Falk PS, Mayhall CG. Validation of surgical wound surveillance.Infect Control Hosp Epidemiol 1993; 14:211-215.21. Chalf<strong>in</strong>e A, Cauet D, L<strong>in</strong> WC, et al. Highly sensitive and efficient computer-assistedsystem for rout<strong>in</strong>e surveillance for surgical site <strong>in</strong>fection.Infect Control Hosp Epidemiol 2006; 27:794-801.22. M<strong>in</strong>er AL, Sands KE, Yokoe DS, et al. Enhanced identification of pos<strong>to</strong>perative<strong>in</strong>fections among outpatients. Emerg Infect Dis 2004; 10:1931-1937.23. Yokoe DS, Nosk<strong>in</strong> GA, Cunnigham SM, et al. Enhanced identificationof pos<strong>to</strong>perative <strong>in</strong>fections among <strong>in</strong>patients. Emerg Infect Dis 2004; 10:1924-1930.24. Burke JP. Infection control—a problem for patient safety. N Engl J Med2003; 348:651-656.25. Sands K, V<strong>in</strong>eyard G, Platt R. <strong>Surgical</strong> site <strong>in</strong>fections occurr<strong>in</strong>g afterhospital discharge. J Infect Dis 1996; 173:963-970.26. Mannien J, Wille JC, Snoeren RL, van den Hof S. Impact of postdischargesurveillance on surgical site <strong>in</strong>fection rates for several surgical procedures:results from the nosocomial surveillance network <strong>in</strong> The Netherlands.Infect Control Hosp Epidemiol 2006; 27:809-816.27. Culver DH, Horan TC, Gaynes RP, et al. <strong>Surgical</strong> wound <strong>in</strong>fection ratesby wound class, operative procedure, and patient risk <strong>in</strong>dex. NationalNosocomial <strong>Infections</strong> Surveillance System. Am J Med 1991; 91:152S-157S.28. Pessaux P, Msika S, Atalla D, Hay JM, Flamant Y. Risk fac<strong>to</strong>rs for pos<strong>to</strong>perative<strong>in</strong>fectious complications <strong>in</strong> noncolorectal abdom<strong>in</strong>al surgery:a multivariate analysis based on a prospective multicenter study of 4718patients. Arch Surg 2003; 138:314-324.29. Raymond DP, Pelletier SJ, Crabtree TD, Schulman AM, Pruett TL, SawyerRG. <strong>Surgical</strong> <strong>in</strong>fection and the ag<strong>in</strong>g population. Am Surg 2001; 67:827-832; discussion 832-833.30. Kaye KS, Schmit K, Pieper C, et al. The effect of <strong>in</strong>creas<strong>in</strong>g age on therisk of surgical site <strong>in</strong>fection. J Infect Dis 2005; 191:1056-1062.31. Dronge AS, Perkal MF, Kancir S, Conca<strong>to</strong> J, Aslan M, Rosenthal RA.Long-term glycemic control and pos<strong>to</strong>perative <strong>in</strong>fectious complications.Arch Surg 2006; 141:375-380; discussion 380.32. Forse RA, Karam B, MacLean LD, Chris<strong>to</strong>u NV. Antibiotic prophylaxisfor surgery <strong>in</strong> morbidly obese patients. Surgery 1989; 106:750-756; discussion756-757.33. Bratzler DW, Houck PM. Antimicrobial prophylaxis for surgery: an advisorystatement from the National <strong>Surgical</strong> Infection <strong>Prevent</strong>ion Project.Cl<strong>in</strong> Infect Dis 2004; 38:1706-1715.34. Haley RW, Culver DH, Morgan WM, White JW, Emori TG, Hoo<strong>to</strong>nTM. Identify<strong>in</strong>g patients at high risk of surgical wound <strong>in</strong>fection: a simplemultivariate <strong>in</strong>dex of patient susceptibility and wound contam<strong>in</strong>ation.Am J Epidemiol 1985; 121:206-215.35. Bratzler DW, Hunt DR. The surgical <strong>in</strong>fection prevention and surgicalcare improvement projects: national <strong>in</strong>itiatives <strong>to</strong> improve outcomes forpatients hav<strong>in</strong>g surgery. Cl<strong>in</strong> Infect Dis 2006; 43:322-330.36. Dell<strong>in</strong>ger EP, Hausmann SM, Bratzler DW, et al. <strong>Hospitals</strong> collaborate<strong>to</strong> decrease surgical site <strong>in</strong>fections. Am J Surg 2005; 190:9-15.37. Institute for Healthcare Improvement. Available at: http://www.ihi.org/.Accessed May 1, 2007.38. Medicare program; hospital outpatient prospective payment system andCY 2007 payment rates; CY 2007 update <strong>to</strong> the ambula<strong>to</strong>ry surgicalcenter covered procedures list; Medicare adm<strong>in</strong>istrative contrac<strong>to</strong>rs; andreport<strong>in</strong>g hospital quality data for FY 2008 <strong>in</strong>patient prospective paymentsystem annual payment update program—HCAHPS survey, SCIP, and
strategies for prevention of ssiS61mortality. F<strong>in</strong>al rule with comment period and f<strong>in</strong>al rule. Fed Regist2006; 71:67959-68401.39. van Kasteren ME, Mannien J, Kullberg BJ, et al. Quality improvemen<strong>to</strong>f surgical prophylaxis <strong>in</strong> Dutch hospitals: evaluation of a multi-site<strong>in</strong>tervention by time series analysis. J Antimicrob Chemother 2005; 56:1094-1102.40. Schweon S. Stamp<strong>in</strong>g out surgical site <strong>in</strong>fections. RN 2006; 69:36-40;quiz 41.41. Torpy JM, Burke A, Glass RM. JAMA patient page: wound <strong>in</strong>fections.JAMA 2005; 294:2122.42. Pes<strong>to</strong>tnik SL, Classen DC, Evans RS, Burke JP. Implement<strong>in</strong>g antibioticpractice guidel<strong>in</strong>es through computer-assisted decision support: cl<strong>in</strong>icaland f<strong>in</strong>ancial outcomes. Ann Intern Med 1996; 124:884-890.43. Kanter G, Connelly NR, Fitzgerald J. A system and process redesign <strong>to</strong>improve perioperative antibiotic adm<strong>in</strong>istration. Anesth Analg 2006; 103:1517-1521.44. Webb AL, Flagg RL, F<strong>in</strong>k AS. Reduc<strong>in</strong>g surgical site <strong>in</strong>fections througha multidiscipl<strong>in</strong>ary computerized process for preoperative prophylacticantibiotic adm<strong>in</strong>istration. Am J Surg 2006; 192:663-668.45. Berger RG, Kichak JP. Computerized physician order entry: helpful orharmful? J Am Med Inform Assoc 2004; 11:100-103.46. Canadian Task Force on the Periodic Health Exam<strong>in</strong>ation. The periodichealth exam<strong>in</strong>ation. Can Med Assoc J 1979; 121:1193-1254.47. Lee JT. Wound <strong>in</strong>fection surveillance. Infect Dis Cl<strong>in</strong> North Am 1992; 6:643-656.48. Haley RW, Culver DH, White JW, et al. The efficacy of <strong>in</strong>fection surveillanceand control programs <strong>in</strong> prevent<strong>in</strong>g nosocomial <strong>in</strong>fections <strong>in</strong>US hospitals. Am J Epidemiol 1985; 121:182-205.49. ASHP therapeutic guidel<strong>in</strong>es on antimicrobial prophylaxis <strong>in</strong> surgery.American Society of Health-System Pharmacists. Am J Health Syst Pharm1999; 56:1839-1888.50. Antimicrobial prophylaxis <strong>in</strong> surgery. Med Lett Drugs Ther 2001; 43:92-97.51. Gandhi GY, Nuttall GA, Abel MD, et al. Intensive <strong>in</strong>traoperative <strong>in</strong>sul<strong>in</strong>therapy versus conventional glucose management dur<strong>in</strong>g cardiac surgery:a randomized trial. Ann Intern Med 2007; 146:233-243.52. Dodds Ashley ES, Carroll DN, Engemann JJ, et al. Risk fac<strong>to</strong>rs for pos<strong>to</strong>perativemediast<strong>in</strong>itis due <strong>to</strong> methicill<strong>in</strong>-resistant Staphylococcus aureus.Cl<strong>in</strong> Infect Dis 2004; 38:1555-1560.53. Bolon MK, Morlote M, Weber SG, Koplan B, Carmeli Y, Wright SB.Glycopeptides are no more effective than b-lactam agents for preventionof surgical site <strong>in</strong>fection after cardiac surgery: a meta-analysis. Cl<strong>in</strong> InfectDis 2004; 38:1357-1363.54. Brennan MF, Pisters PW, Posner M, Quesada O, Shike M. A prospectiverandomized trial of <strong>to</strong>tal parenteral nutrition after major pancreatic resectionfor malignancy. Ann Surg 1994; 220:436-441; discussion 441-444.55. Perioperative <strong>to</strong>tal parenteral nutrition <strong>in</strong> surgical patients. The VeteransAffairs Total Parenteral Nutrition Cooperative Study Group. NEnglJMed 1991; 325:525-532.56. Kaul AF, Jewett JF. Agents and techniques for dis<strong>in</strong>fection of the sk<strong>in</strong>.Surg Gynecol Obstet 1981; 152:677-685.57. Webster J, Osborne S. Preoperative bath<strong>in</strong>g or shower<strong>in</strong>g with sk<strong>in</strong> antiseptics<strong>to</strong> prevent surgical site <strong>in</strong>fection. Cochrane Database Syst Rev2007; (2):CD004985.58. Perl TM, Cullen JJ, Wenzel RP, et al. Intranasal mupiroc<strong>in</strong> <strong>to</strong> preventpos<strong>to</strong>perative Staphylococcus aureus <strong>in</strong>fections. NEnglJMed2002; 346:1871-1877.59. Miller MA, Dascal A, Portnoy J, Mendelson J. Development of mupiroc<strong>in</strong>resistance among methicill<strong>in</strong>-resistant Staphylococcus aureus after widespreaduse of nasal mupiroc<strong>in</strong> o<strong>in</strong>tment. Infect Control Hosp Epidemiol1996; 17:811-813.60. Kallen AJ, Wilson CT, Larson RJ. Perioperative <strong>in</strong>tranasal mupiroc<strong>in</strong> forthe prevention of surgical-site <strong>in</strong>fections: systematic review of the literatureand meta-analysis. Infect Control Hosp Epidemiol 2005; 26:916-922.61. Wilcox MH, Hall J, Pike H, et al. Use of perioperative mupiroc<strong>in</strong> <strong>to</strong>prevent methicill<strong>in</strong>-resistant Staphylococcus aureus (MRSA) orthopaedicsurgical site <strong>in</strong>fections. J Hosp Infect 2003; 54:196-201.62. Nicholson MR, Huesman LA. Controll<strong>in</strong>g the usage of <strong>in</strong>tranasal mupiroc<strong>in</strong>does impact the rate of Staphylococcus aureus deep sternal wound<strong>in</strong>fections <strong>in</strong> cardiac surgery patients. Am J Infect Control 2006; 34:44-48.63. McKibben L, Horan T, Tokars JI, et al. Guidance on public report<strong>in</strong>g ofhealthcare-associated <strong>in</strong>fections: recommendations of the Healthcare InfectionControl Practices Advisory Committee. Am J Infect Control 2005;33:217-226.64. Belda FJ, Aguilera L, Garcia de la Asuncion J, et al. Supplemental perioperativeoxygen and the risk of surgical wound <strong>in</strong>fection: a randomizedcontrolled trial. JAMA 2005; 294:2035-2042.65. Greif R, Akca O, Horn EP, Kurz A, Sessler DI. Supplemental perioperativeoxygen <strong>to</strong> reduce the <strong>in</strong>cidence of surgical-wound <strong>in</strong>fection. OutcomesResearch Group. N Engl J Med 2000; 342:161-167.66. Pryor KO, Fahey TJ 3rd, Lien CA, Goldste<strong>in</strong> PA. <strong>Surgical</strong> site <strong>in</strong>fectionand the rout<strong>in</strong>e use of perioperative hyperoxia <strong>in</strong> a general surgicalpopulation: a randomized controlled trial. JAMA 2004; 291:79-87.67. Dell<strong>in</strong>ger EP. Increas<strong>in</strong>g <strong>in</strong>spired oxygen <strong>to</strong> decrease surgical site <strong>in</strong>fection:time <strong>to</strong> shift the quality improvement research paradigm. JAMA2005; 294:2091-2092.68. Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia <strong>to</strong> reducethe <strong>in</strong>cidence of surgical-wound <strong>in</strong>fection and shorten hospitalization.Study of Wound Infection and Temperature Group. N Engl J Med 1996;334:1209-1215.69. Barone JE, Tucker JB, Cecere J, et al. Hypothermia does not result <strong>in</strong>more complications after colon surgery. Am Surg 1999; 65:356-359.70. Segers P, Speekenbr<strong>in</strong>k RG, Ubb<strong>in</strong>k DT, van Ogtrop ML, de Mol BA.<strong>Prevent</strong>ion of nosocomial <strong>in</strong>fection <strong>in</strong> cardiac surgery by decontam<strong>in</strong>ationof the nasopharynx and oropharynx with chlorhexid<strong>in</strong>e gluconate:a randomized controlled trial. JAMA 2006; 296:2460-2466.71. Gaynes RP, Culver DH, Horan TC, Edwards JR, Richards C, Tolson JS.<strong>Surgical</strong> site <strong>in</strong>fection (SSI) rates <strong>in</strong> the United States, 1992-1998: theNational Nosocomial <strong>Infections</strong> Surveillance System basic SSI risk <strong>in</strong>dex.Cl<strong>in</strong> Infect Dis 2001;33(Suppl 2):S69-S77.72. Gaynes RP, Solomon S. Improv<strong>in</strong>g hospital-acquired <strong>in</strong>fection rates: theCDC experience. Jt Comm J Qual Improv 1996; 22:457-467.73. The Society for Hospital Epidemiology of America; The Association forPractitioners <strong>in</strong> Infection Control; The Centers for Disease Control; The<strong>Surgical</strong> Infection Society. Consensus paper on the surveillance of surgicalwound <strong>in</strong>fections. Infect Control Hosp Epidemiol 1992; 13:599-605.74. Wong ES, Rupp ME, Mermel L, et al. Public disclosure of healthcareassociated<strong>in</strong>fections: the role of the Society for Healthcare Epidemiologyof America. Infect Control Hosp Epidemiol 2005; 26:210-212.75. McKibben L, Horan TC, Tokars JI, et al. Guidance on public report<strong>in</strong>gof healthcare-associated <strong>in</strong>fections: recommendations of the HealthcareInfection Control Practices Advisory Committee. Infect Control HospEpidemiol 2005; 26:580-587.76. The Healthcare-Associated Infection Work<strong>in</strong>g Group of the Jo<strong>in</strong>t PublicPolicy Committee. Essentials of public report<strong>in</strong>g of healthcare-associated<strong>in</strong>fections: a <strong>to</strong>ol kit. January 2007. Available at: http://www.cdc.gov/ncidod/dhqp/pdf/ar/06_107498_Essentials_Tool_Kit.pdf. Accessed April6, 2007.77. The National Quality Forum. National voluntary consensus standards,endorsed November 15, 2007. Available at: http://www.qualityforum.org/pdf/news/lsCSACMeasures.pdf. Accessed December 20, 2007.