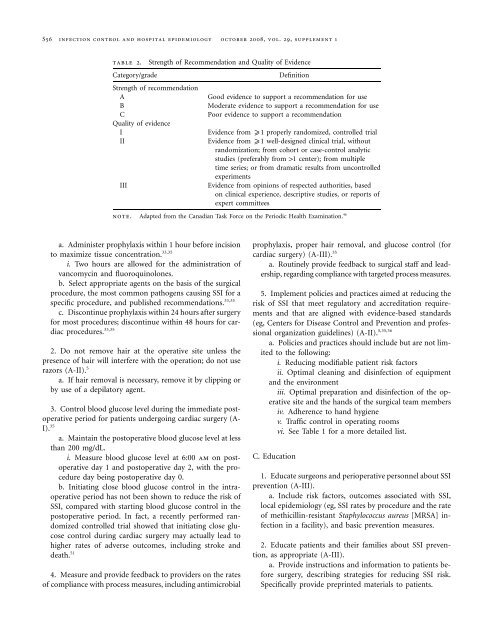
S56 <strong>in</strong>fection control and hospital epidemiology oc<strong>to</strong>ber 2008, vol. 29, supplement 1table 2.Category/gradeStrength of Recommendation and Quality of EvidenceStrength of recommendationABCQuality of evidenceIIIIIIDef<strong>in</strong>itionGood evidence <strong>to</strong> support a recommendation for useModerate evidence <strong>to</strong> support a recommendation for usePoor evidence <strong>to</strong> support a recommendationEvidence from x1 properly randomized, controlled trialEvidence from x1 well-designed cl<strong>in</strong>ical trial, withoutrandomization; from cohort or case-control analyticstudies (preferably from 11 center); from multipletime series; or from dramatic results from uncontrolledexperimentsEvidence from op<strong>in</strong>ions of respected authorities, basedon cl<strong>in</strong>ical experience, descriptive studies, or reports ofexpert committeesnote. Adapted from the Canadian Task Force on the Periodic Health Exam<strong>in</strong>ation. 46a. Adm<strong>in</strong>ister prophylaxis with<strong>in</strong> 1 hour before <strong>in</strong>cision<strong>to</strong> maximize tissue concentration. 33,35i. Two hours are allowed for the adm<strong>in</strong>istration ofvancomyc<strong>in</strong> and fluoroqu<strong>in</strong>olones.b. Select appropriate agents on the basis of the surgicalprocedure, the most common pathogens caus<strong>in</strong>g SSI for aspecific procedure, and published recommendations. 33,35c. Discont<strong>in</strong>ue prophylaxis with<strong>in</strong> 24 hours after surgeryfor most procedures; discont<strong>in</strong>ue with<strong>in</strong> 48 hours for cardiacprocedures. 33,352. Do not remove hair at the operative site unless thepresence of hair will <strong>in</strong>terfere with the operation; do not userazors (A-II). 5a. If hair removal is necessary, remove it by clipp<strong>in</strong>g orby use of a depila<strong>to</strong>ry agent.3. Control blood glucose level dur<strong>in</strong>g the immediate pos<strong>to</strong>perativeperiod for patients undergo<strong>in</strong>g cardiac surgery (A-I). 35a. Ma<strong>in</strong>ta<strong>in</strong> the pos<strong>to</strong>perative blood glucose level at lessthan 200 mg/dL.i. Measure blood glucose level at 6:00 am on pos<strong>to</strong>perativeday 1 and pos<strong>to</strong>perative day 2, with the procedureday be<strong>in</strong>g pos<strong>to</strong>perative day 0.b. Initiat<strong>in</strong>g close blood glucose control <strong>in</strong> the <strong>in</strong>traoperativeperiod has not been shown <strong>to</strong> reduce the risk ofSSI, compared with start<strong>in</strong>g blood glucose control <strong>in</strong> thepos<strong>to</strong>perative period. In fact, a recently performed randomizedcontrolled trial showed that <strong>in</strong>itiat<strong>in</strong>g close glucosecontrol dur<strong>in</strong>g cardiac surgery may actually lead <strong>to</strong>higher rates of adverse outcomes, <strong>in</strong>clud<strong>in</strong>g stroke anddeath. 514. Measure and provide feedback <strong>to</strong> providers on the ratesof compliance with process measures, <strong>in</strong>clud<strong>in</strong>g antimicrobialprophylaxis, proper hair removal, and glucose control (forcardiac surgery) (A-III). 35a. Rout<strong>in</strong>ely provide feedback <strong>to</strong> surgical staff and leadership,regard<strong>in</strong>g compliance with targeted process measures.5. Implement policies and practices aimed at reduc<strong>in</strong>g therisk of SSI that meet regula<strong>to</strong>ry and accreditation requirementsand that are aligned with evidence-based standards(eg, Centers for Disease Control and <strong>Prevent</strong>ion and professionalorganization guidel<strong>in</strong>es) (A-II). 5,35,36a. Policies and practices should <strong>in</strong>clude but are not limited<strong>to</strong> the follow<strong>in</strong>g:i. Reduc<strong>in</strong>g modifiable patient risk fac<strong>to</strong>rsii. Optimal clean<strong>in</strong>g and dis<strong>in</strong>fection of equipmentand the environmentiii. Optimal preparation and dis<strong>in</strong>fection of the operativesite and the hands of the surgical team membersiv. Adherence <strong>to</strong> hand hygienev. Traffic control <strong>in</strong> operat<strong>in</strong>g roomsvi. See Table 1 for a more detailed list.C. Education1. Educate surgeons and perioperative personnel about SSIprevention (A-III).a. Include risk fac<strong>to</strong>rs, outcomes associated with SSI,local epidemiology (eg, SSI rates by procedure and the rateof methicill<strong>in</strong>-resistant Staphylococcus aureus [MRSA] <strong>in</strong>fection<strong>in</strong> a facility), and basic prevention measures.2. Educate patients and their families about SSI prevention,as appropriate (A-III).a. Provide <strong>in</strong>structions and <strong>in</strong>formation <strong>to</strong> patients beforesurgery, describ<strong>in</strong>g strategies for reduc<strong>in</strong>g SSI risk.Specifically provide prepr<strong>in</strong>ted materials <strong>to</strong> patients.
strategies for prevention of ssiS57b. Examples of pr<strong>in</strong>ted materials for patients are availablefrom the follow<strong>in</strong>g Web pages:i. JAMA patient page: wound <strong>in</strong>fections (from theJournal of the American Medical Association; available at:http://jama.ama-assn.org/cgi/repr<strong>in</strong>t/294/16/2122)ii. <strong>Surgical</strong> <strong>Care</strong> Improvement Project consumer <strong>in</strong>fosheet (available at: http://www.ofmq.com/Websites/ofmq/Images/FINALconsumer_tips2.pdf)iii. What you need <strong>to</strong> know about <strong>in</strong>fections aftersurgery: a fact sheet for patients and their family members(available at: http://www.ihi.org/NR/rdonlyres/0EE409F4-2F6A-4B55-AB01-16B6D6935EC5/0/<strong>Surgical</strong><strong>Site</strong><strong>Infections</strong>PtsandFam.pdf)D. Accountability1. The hospital’s chief executive officer and senior managementare responsible for ensur<strong>in</strong>g that the healthcare systemsupports an <strong>in</strong>fection prevention and control programthat effectively prevents the occurrence of SSIs and the transmissionof epidemiologically significant pathogens.2. Senior management is accountable for ensur<strong>in</strong>g that anadequate number of tra<strong>in</strong>ed personnel are assigned <strong>to</strong> the<strong>in</strong>fection prevention and control program.3. Senior management is accountable for ensur<strong>in</strong>g thathealthcare personnel, <strong>in</strong>clud<strong>in</strong>g licensed and nonlicensed personnel,are competent <strong>to</strong> perform their job responsibilities.4. Direct healthcare providers (such as physicians, nurses,aides, and therapists) and ancillary personnel (such as housekeep<strong>in</strong>gand equipment-process<strong>in</strong>g personnel) are responsiblefor ensur<strong>in</strong>g that appropriate <strong>in</strong>fection prevention and controlpractices are used at all times (<strong>in</strong>clud<strong>in</strong>g hand hygiene;strict adherence <strong>to</strong> aseptic technique; clean<strong>in</strong>g and dis<strong>in</strong>fectionof equipment and the environment; clean<strong>in</strong>g, dis<strong>in</strong>fection,and sterilization of medical supplies and <strong>in</strong>struments;and appropriate surgical prophylaxis pro<strong>to</strong>cols).5. Hospital and unit leaders are responsible for hold<strong>in</strong>gpersonnel accountable for their actions.6. The person that manages the <strong>in</strong>fection prevention andcontrol program is responsible for ensur<strong>in</strong>g that an activeprogram <strong>to</strong> identify SSIs is implemented, that data on SSIsare analyzed and regularly provided <strong>to</strong> those who can use the<strong>in</strong>formation <strong>to</strong> improve the quality of care (eg, unit staff,cl<strong>in</strong>icians, and hospital adm<strong>in</strong>istra<strong>to</strong>rs), and that evidencebasedpractices are <strong>in</strong>corporated <strong>in</strong><strong>to</strong> the program.7. Personnel responsible for healthcare personnel and patienteducation are accountable for ensur<strong>in</strong>g that appropriatetra<strong>in</strong><strong>in</strong>g and educational programs <strong>to</strong> prevent SSIs are developedand provided <strong>to</strong> personnel, patients, and families.8. Personnel from the <strong>in</strong>fection prevention and controlprogram, the labora<strong>to</strong>ry, and <strong>in</strong>formation technology departmentsare responsible for ensur<strong>in</strong>g that systems are <strong>in</strong>place <strong>to</strong> support the surveillance program.II. Special approaches for the prevention of SSIPerform an SSI risk assessment. These special approaches arerecommended for use <strong>in</strong> locations and/or populations with<strong>in</strong>the hospital that have unacceptably high SSI rates despiteimplementation of the basic SSI prevention strategies listedabove.1. Perform expanded SSI surveillance <strong>to</strong> determ<strong>in</strong>e thesource and extent of the problem and <strong>to</strong> identify possibletargets for <strong>in</strong>tervention (B-II).a. Expand surveillance <strong>to</strong> <strong>in</strong>clude additional proceduresand possibly <strong>to</strong> all National Healthcare Safety Networkprocedures. 5 Align expanded surveillance with the hospital’sstrategic plan.III. Approaches that should not be considered a rout<strong>in</strong>epart of SSI prevention1. Do not rout<strong>in</strong>ely use vancomyc<strong>in</strong> for antimicrobial prophylaxis(B-II).a. Vancomyc<strong>in</strong> should not rout<strong>in</strong>ely be used for antimicrobialprophylaxis, but it can be an appropriate agentfor specific scenarios. Reserve vancomyc<strong>in</strong> for specific cl<strong>in</strong>icalcircumstances, such as a proven outbreak of SSI due<strong>to</strong> MRSA, high endemic rates of SSI due <strong>to</strong> MRSA, targetedhigh-risk patients who are at <strong>in</strong>creased risk for SSI due <strong>to</strong>MRSA (<strong>in</strong>clud<strong>in</strong>g cardiothoracic surgical patients and elderlypatients with diabetes), and high-risk surgical proceduresdur<strong>in</strong>g which an implant is placed. 52i. No def<strong>in</strong>itions for “high endemic rates of SSI due<strong>to</strong> MRSA” have been established.ii. Studies of the efficacy of vancomyc<strong>in</strong> prophylaxiswere published before the emergence of communityacquiredMRSA.b. A recent meta-analysis of 7 studies compar<strong>in</strong>g glycopeptideprophylaxis with b-lactam prophylaxis beforecardiothoracic surgery showed that there was no difference<strong>in</strong> rates of SSI between the 2 antimicrobial prophylaxisregimens. 53c. No study has prospectively analyzed the effect of provid<strong>in</strong>gboth glycopeptide and b-lactam antimicrobials forpreoperative antimicrobial prophylaxis. Thus, it is unclearwhether treatment with vancomyc<strong>in</strong>, when <strong>in</strong>dicated,should be added <strong>to</strong> or used <strong>in</strong> place of standard recommendedantimicrobial prophylaxis. Because vancomyc<strong>in</strong>does not have activity aga<strong>in</strong>st gram-negative pathogens,some experts recommend add<strong>in</strong>g vancomyc<strong>in</strong> treatment <strong>to</strong>standard antimicrobial prophylaxis for the specific cl<strong>in</strong>icalcircumstances described above.