Fill in the Gaps > Too many older people who are deafblind ... - Sense
Fill in the Gaps > Too many older people who are deafblind ... - Sense
Fill in the Gaps > Too many older people who are deafblind ... - Sense
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Too</strong> <strong>many</strong> <strong>older</strong> <strong>people</strong><strong>who</strong> <strong>are</strong> deafbl<strong>in</strong>dmiss out on <strong>the</strong>support <strong>the</strong>y needA toolkit for professionals work<strong>in</strong>gwith <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong><strong>Fill</strong> <strong>in</strong> <strong>the</strong> <strong>Gaps</strong> >
This booklet offers <strong>in</strong>formation and advice for thosework<strong>in</strong>g with <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong>. It expla<strong>in</strong>s whatdeafbl<strong>in</strong>dness is and how it affects <strong>people</strong>. It sets out <strong>the</strong>legal responsibilities that social services have and expla<strong>in</strong>show deafbl<strong>in</strong>d <strong>people</strong> can be supported and helped.Increas<strong>in</strong>g numbers of <strong>older</strong> <strong>people</strong> <strong>are</strong> develop<strong>in</strong>g hear<strong>in</strong>g and visionproblems. Some <strong>older</strong> <strong>people</strong> have substantial hear<strong>in</strong>g and vision difficulties– known as deafbl<strong>in</strong>dness.Often this hear<strong>in</strong>g and vision loss comes on very gradually. Older <strong>people</strong><strong>the</strong>mselves, and o<strong>the</strong>rs around <strong>the</strong>m, may not recognise or understandwhat is happen<strong>in</strong>g.Because of this comb<strong>in</strong>ed hear<strong>in</strong>g and vision loss, <strong>the</strong>y may have problemswith communicat<strong>in</strong>g, gett<strong>in</strong>g around and access<strong>in</strong>g <strong>in</strong>formation. This cancause difficulties with <strong>many</strong> everyday activities and can make <strong>the</strong>m feelexcluded from society.But it doesn’t have to be like this. If <strong>the</strong> right services and opportunities <strong>are</strong>available, <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong> can live <strong>in</strong>dependently and make choicesabout how <strong>the</strong>y wish to live. If appropriate services <strong>are</strong> provided at <strong>the</strong> righttime, <strong>the</strong> need for greater health and social c<strong>are</strong> provision at a later stagecan be reduced.Local authorities have statutory responsibilities towards <strong>older</strong> <strong>people</strong> withcomb<strong>in</strong>ed hear<strong>in</strong>g and vision loss – aris<strong>in</strong>g from <strong>the</strong> guidance ‘Social C<strong>are</strong>for Deafbl<strong>in</strong>d Children and Adults’ LAC(DH) (2009)6.They <strong>are</strong> required to provide specialist assessments, appropriate <strong>in</strong>formationand services designed to meet <strong>the</strong> needs of deafbl<strong>in</strong>d <strong>people</strong>. We will referto <strong>the</strong> Deafbl<strong>in</strong>d Guidance throughout this booklet.In <strong>many</strong> cases, <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong> <strong>are</strong> seen by a social work team for<strong>older</strong> <strong>people</strong> – ra<strong>the</strong>r than a team which specialises <strong>in</strong> sensory impairment.This booklet expla<strong>in</strong>s how you can help to make sure that <strong>older</strong> deafbl<strong>in</strong>d<strong>people</strong> get <strong>the</strong> support <strong>the</strong>y <strong>are</strong> entitled to.3
<strong>Fill</strong> <strong>in</strong> <strong>the</strong> <strong>Gaps</strong> >1 > Deafbl<strong>in</strong>dness and <strong>older</strong> <strong>people</strong>3 What is deafbl<strong>in</strong>dness?3 How it affects <strong>older</strong> <strong>people</strong>4 Talk<strong>in</strong>g about sensory loss5 How <strong>many</strong> <strong>older</strong> <strong>people</strong> <strong>are</strong> affected?12 > Legal requirements7 What does <strong>the</strong> Deafbl<strong>in</strong>d Guidance say?8 The S<strong>in</strong>gle Assessment Process10 Fair Access to C<strong>are</strong> Services11 Recognis<strong>in</strong>g deafbl<strong>in</strong>dness13 The National Service Framework23 > Work<strong>in</strong>g with <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong>15 How can your team work effectively with<strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong>?16 Indicators of hear<strong>in</strong>g and vision loss17 Communicat<strong>in</strong>g effectively – face to face18 Communicat<strong>in</strong>g effectively – at a distance21 Checklist34 > Resources23 Useful organisations24 References24 Web based resources41
1 > Deafbl<strong>in</strong>dness and <strong>older</strong> <strong>people</strong>The term ‘deafbl<strong>in</strong>d’ describes <strong>people</strong> of all ages <strong>who</strong> have acomb<strong>in</strong>ed hear<strong>in</strong>g and vision impairment. These <strong>in</strong>dividuals maybe deaf or hard of hear<strong>in</strong>g as well as bl<strong>in</strong>d or partially sighted.They do not have to be completely deaf and bl<strong>in</strong>d. In fact, mostdeafbl<strong>in</strong>d <strong>people</strong> have some useful hear<strong>in</strong>g or vision.Deafbl<strong>in</strong>dness is aunique disabilityunique2
deafdeafbl<strong>in</strong>dbl<strong>in</strong>dWhat is deafbl<strong>in</strong>dness?Def<strong>in</strong>itions of deafbl<strong>in</strong>dness tend not to focus on <strong>the</strong> degree ofdeafness or bl<strong>in</strong>dness a person has, but ra<strong>the</strong>r on <strong>the</strong> effect of<strong>the</strong> comb<strong>in</strong>ed loss on everyday life – how it affects <strong>the</strong>ir ability tocommunicate, to get around and to access all k<strong>in</strong>ds of <strong>in</strong>formation.Deafbl<strong>in</strong>dness is not just a deaf person <strong>who</strong> cannot see or a bl<strong>in</strong>dperson <strong>who</strong> cannot hear. The two impairments impact on eacho<strong>the</strong>r and multiply <strong>the</strong> total effect.One deafbl<strong>in</strong>d person describes it like this:“If you th<strong>in</strong>k of deafness as <strong>the</strong> colour yellow and bl<strong>in</strong>dnessas <strong>the</strong> colour blue, when you mix <strong>the</strong> two toge<strong>the</strong>r you don’tget yellow-blue but a completely different colour – green.”How it affects <strong>older</strong> <strong>people</strong>Deafbl<strong>in</strong>dness affects different <strong>people</strong> <strong>in</strong> different ways. Whencommunication is limited, <strong>people</strong> become socially and emotionallyisolated. When <strong>people</strong> can’t get around by <strong>the</strong>mselves it affects<strong>the</strong>ir confidence, <strong>in</strong>dependence and daily liv<strong>in</strong>g skills. Withoutaccess to <strong>in</strong>formation, <strong>people</strong> can’t make <strong>in</strong>formed decisions andthis leads to fur<strong>the</strong>r loss of <strong>in</strong>dependence. These <strong>are</strong> commonexperiences for <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong>.Older People’s social work teams can do a great deal to help <strong>older</strong>deafbl<strong>in</strong>d <strong>people</strong>. See page 15 for <strong>in</strong>formation on how to makethis happen.A comb<strong>in</strong>ation ofvisual and hear<strong>in</strong>gimpairment willmultiply <strong>the</strong> difficultiesan <strong>in</strong>dividual faces.For example…• If you <strong>are</strong> deaf or hard ofhear<strong>in</strong>g and can’t hear whatsomeone is say<strong>in</strong>g, youwatch <strong>the</strong>ir lips and facialexpressions for extra clues.But if you also become bl<strong>in</strong>dor partially sighted, howwill you understand what isbe<strong>in</strong>g said?• If you <strong>are</strong> a bl<strong>in</strong>d orpartially sighted person<strong>who</strong> is used to travell<strong>in</strong>g<strong>in</strong>dependently, you dependon your hear<strong>in</strong>g. But if youbecome deaf or hard ofhear<strong>in</strong>g and can’t hear orsee <strong>the</strong> traffic, how will youknow when it’s safe to cross<strong>the</strong> road?• If you can no longereasily see or hear <strong>the</strong>television, listen to<strong>the</strong> radio, read yourletters, use <strong>the</strong> phone orengage <strong>in</strong> conversationyou become isolatedfrom <strong>people</strong>, eventsand society. Thissensory deprivationcan lead to extremelevels of boredom,stress, depression andwithdrawal.3
1 > Deafbl<strong>in</strong>dness and <strong>older</strong> <strong>people</strong>Don’t miss anopportunityIf we take <strong>the</strong> view thatloss of sight and hear<strong>in</strong>g<strong>are</strong> a normal, acceptablepart of age<strong>in</strong>g, we miss<strong>the</strong> opportunity to help<strong>people</strong> make best useof <strong>the</strong>ir rema<strong>in</strong><strong>in</strong>g visionand hear<strong>in</strong>g.Talk<strong>in</strong>g about sensory lossMany <strong>older</strong> <strong>people</strong> with a hear<strong>in</strong>g and vision loss don’t th<strong>in</strong>k of<strong>the</strong>mselves as deafbl<strong>in</strong>d. They may th<strong>in</strong>k that sensory loss is just one moreeffect of old age along with mobility problems, memory loss, illness ordepression – and it often is.But that doesn’t mean we can’t do anyth<strong>in</strong>g about it. Their hear<strong>in</strong>g andvision loss may have crept up on <strong>the</strong>m slowly so <strong>the</strong>y only gradually realisethat someth<strong>in</strong>g is wrong. They may see some th<strong>in</strong>gs, but not o<strong>the</strong>rs. Theymay hear <strong>in</strong> some situations, but not o<strong>the</strong>rs. They may use phrases suchas: “I don’t hear too well” or “I’m hav<strong>in</strong>g problems with my eyes”. Andyet <strong>the</strong> everyday difficulties <strong>the</strong>y describe <strong>are</strong> not just to do with age<strong>in</strong>gbut <strong>are</strong> <strong>the</strong> typical effects of deafbl<strong>in</strong>dness.Professionals <strong>are</strong> likely to use terms such as deafbl<strong>in</strong>d or dual sensory loss.The Deafbl<strong>in</strong>d Guidance uses <strong>the</strong>se <strong>in</strong>terchangeably to acknowledge that<strong>the</strong> comb<strong>in</strong>ed loss of hear<strong>in</strong>g and vision is significant for anyone, even ifhe or she still has some useful hear<strong>in</strong>g and vision.Even if a person doesn’tuse <strong>the</strong> term deafbl<strong>in</strong>dabout <strong>the</strong>mselves, we needto recognise <strong>the</strong> effects ofdeafbl<strong>in</strong>dness and offersupport and services to meetthose needs. Be aw<strong>are</strong> of<strong>the</strong> language a person usesabout <strong>the</strong>mselves and adaptyour own to reflect what<strong>the</strong>y <strong>are</strong> comfortable with.4
How <strong>many</strong> <strong>older</strong> <strong>people</strong> <strong>are</strong> affected?<strong>Sense</strong> commissioned <strong>in</strong>dependent, expert research on <strong>the</strong> numbersof deafbl<strong>in</strong>d <strong>people</strong> <strong>in</strong> 2010. The Centre for Disability Researchreport found that <strong>the</strong> deafbl<strong>in</strong>d population has been significantlyunderestimated. 62% of <strong>the</strong> deafbl<strong>in</strong>d population is aged over70 and <strong>the</strong> numbers will <strong>in</strong>crease dramatically over <strong>the</strong> next20 years as a result of <strong>the</strong> age<strong>in</strong>g population.• 356,000 deafbl<strong>in</strong>d <strong>people</strong> <strong>in</strong> <strong>the</strong> UK• Of which,• 220,000 <strong>people</strong> over <strong>the</strong> age of 70 have significantcomb<strong>in</strong>ed visual impairment and hear<strong>in</strong>g lossFuture explosion <strong>in</strong> numbers by 2030• 569,000 deafbl<strong>in</strong>d <strong>people</strong> <strong>in</strong> <strong>the</strong> UK, a 60% <strong>in</strong>crease• Of which,• 418,000 will be <strong>people</strong> over <strong>the</strong> age of 70 have significantcomb<strong>in</strong>ed visual impairment and hear<strong>in</strong>g loss(<strong>Sense</strong>/CeDR, 2010)• Older <strong>people</strong> with vision and hear<strong>in</strong>g loss from m<strong>in</strong>oritycommunities <strong>are</strong> poorly represented <strong>in</strong> statistics but it is likelythat <strong>the</strong> <strong>in</strong>cidence is similar to that of white British communities.These figures show how common dual sensory loss is among<strong>older</strong> <strong>people</strong>. You <strong>are</strong> probably already <strong>in</strong> contact with some <strong>older</strong><strong>people</strong> with dual sensory loss. Read on to f<strong>in</strong>d out how you canmake your services accessible to <strong>the</strong>m and promote <strong>in</strong>dependenceand choice.You <strong>are</strong> probably already<strong>in</strong> contact with some<strong>older</strong> <strong>people</strong> with dualsensory loss5
What does <strong>the</strong> Deafbl<strong>in</strong>d Guidance say?The statutory guidance, ‘Social C<strong>are</strong> for Deafbl<strong>in</strong>d Children andAdults’ LAC(DH) (2009)6, provides a framework for all socialservices. It outl<strong>in</strong>es <strong>the</strong> rights of deafbl<strong>in</strong>d <strong>people</strong> and <strong>the</strong> dutiesplaced on local authorities. Local authorities <strong>are</strong> asked to take<strong>the</strong> follow<strong>in</strong>g action:• identify, make contact with, and keep a record of deafbl<strong>in</strong>d<strong>people</strong> <strong>in</strong> <strong>the</strong>ir catchment <strong>are</strong>a – <strong>in</strong>clud<strong>in</strong>g those <strong>who</strong> havemultiple disabilities that <strong>in</strong>clude dual sensory impairment;• ensure that when an assessment is requested or required,it is carried out by a specifically tra<strong>in</strong>ed person/team, equippedto assess <strong>the</strong> needs of a deafbl<strong>in</strong>d person – <strong>in</strong> particular toassess <strong>the</strong> need for one-to-one human support, assistivetechnology and rehabilitation;• ensure that appropriate services <strong>are</strong> provided todeafbl<strong>in</strong>d <strong>people</strong> – <strong>who</strong> <strong>are</strong> not necessarily able to benefit fromma<strong>in</strong>stream services or those services aimed primarily at bl<strong>in</strong>d<strong>people</strong> or deaf <strong>people</strong> <strong>who</strong> <strong>are</strong> able to rely on <strong>the</strong>ir o<strong>the</strong>r senses;• to provide or commission specifically tra<strong>in</strong>ed one-to-onesupport workers for <strong>people</strong> assessed as requir<strong>in</strong>g one;• provide <strong>in</strong>formation about services <strong>in</strong> formats, and us<strong>in</strong>gmethods, that <strong>are</strong> accessible to deafbl<strong>in</strong>d <strong>people</strong>;• ensure that one member of senior management<strong>in</strong>cludes overall responsibility for deafbl<strong>in</strong>d services with<strong>in</strong> hisor her responsibilities.The guidance and itsduties <strong>are</strong> mandatory.Authorities that failto comply could bechallenged throughjudicial review.7
2 > Legal requirementsHow <strong>the</strong> Deafbl<strong>in</strong>d Guidance fits with:A) The S<strong>in</strong>gle Assessment ProcessThe Department of Health states that <strong>the</strong> purpose of <strong>the</strong> S<strong>in</strong>gleAssessment Process (SAP) is to make sure that all <strong>older</strong> <strong>people</strong>receive appropriate, effective and timely responses to <strong>the</strong>ir healthand social c<strong>are</strong> needs. A key value of SAP is to make sure that<strong>in</strong>dividuals <strong>are</strong> at <strong>the</strong> heart of assessment and c<strong>are</strong> plann<strong>in</strong>g. The<strong>older</strong> deafbl<strong>in</strong>d person’s account of <strong>the</strong>ir needs and <strong>the</strong>ir viewsand wishes should be kept at <strong>the</strong> centre of <strong>the</strong> process.The aim is that <strong>in</strong>formation about a person’s needs should onlybe given once, although <strong>the</strong> assessment, c<strong>are</strong> plann<strong>in</strong>g and servicedelivery may <strong>in</strong>volve a number of professionals and agencies.The assessment systems <strong>in</strong>clude <strong>the</strong> follow<strong>in</strong>g broad types:• contact assessment• overview assessment, and• specialist assessment.To make sure that <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong> <strong>are</strong> properly <strong>in</strong>cluded,it is important that <strong>the</strong>ir specific needs <strong>are</strong> recognised <strong>in</strong> <strong>the</strong>generic contact or overview assessments. If vital <strong>in</strong>formation about<strong>the</strong> impact of deafbl<strong>in</strong>dness is missed at this stage, referral forspecialist assessment may not happen and <strong>the</strong> assessment will be<strong>in</strong>complete and c<strong>are</strong> plann<strong>in</strong>g <strong>in</strong>adequate.The Deafbl<strong>in</strong>d Guidancestates that assessment of adeafbl<strong>in</strong>d person should becarried out by a specificallytra<strong>in</strong>ed person or team sothat <strong>the</strong>ir particular needscan be explored <strong>in</strong> detail.This has <strong>the</strong> potential towork effectively with<strong>in</strong>SAP but requires genericassessors to be able torecognise deafbl<strong>in</strong>dnessand its effects and refer onappropriately.How to use SAP with <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong>Th<strong>in</strong>k dual sensory!• Every time you <strong>are</strong> assess<strong>in</strong>g an <strong>older</strong> person, ask yourself whe<strong>the</strong>r <strong>the</strong>irneeds could be related to deafbl<strong>in</strong>dness.• Make sure you <strong>are</strong> tra<strong>in</strong>ed to recognise deafbl<strong>in</strong>dness and its effects. At am<strong>in</strong>imum, everyone carry<strong>in</strong>g out a contact or overview assessment shouldhave <strong>the</strong> <strong>Fill</strong> <strong>in</strong> <strong>the</strong> <strong>Gaps</strong> checklist for assess<strong>in</strong>g <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong>.• Make sure you use good communication tactics which <strong>are</strong> useful with all<strong>older</strong> <strong>people</strong>. (For <strong>in</strong>formation on communication tactics, see page 17).Make <strong>the</strong> l<strong>in</strong>k• As soon as an assessment identifies that <strong>the</strong>re may be a dual sensoryloss, arrange a specialist assessment via <strong>the</strong> sensory team or o<strong>the</strong>rspecialist agency such as <strong>Sense</strong> or Deafbl<strong>in</strong>d UK. Assessment and skillstra<strong>in</strong><strong>in</strong>g by a specialist worker can lead to <strong>in</strong>creased <strong>in</strong>dependence andenhanced quality of life.• Develop effective l<strong>in</strong>ks with <strong>the</strong> sensory specialists <strong>in</strong> your localauthority and o<strong>the</strong>r specialist agencies.• Take tra<strong>in</strong><strong>in</strong>g to develop your own skills <strong>in</strong> identify<strong>in</strong>g <strong>the</strong> potential<strong>in</strong>dependent liv<strong>in</strong>g skills of an <strong>older</strong> deafbl<strong>in</strong>d person.8
Information• Make sure you have good <strong>in</strong>formation about both national andlocal services.• Make sure <strong>in</strong>formation, letters and c<strong>are</strong> plans <strong>are</strong> <strong>in</strong> accessibleformats (e.g. large pr<strong>in</strong>t, Braille, tape or disk). For <strong>in</strong>formationabout transcription services, see <strong>the</strong> Resources section. If yourSAP systems don’t record this <strong>in</strong>formation talk to your SAPco-ord<strong>in</strong>ator about add<strong>in</strong>g this.Communication needs• Be aw<strong>are</strong> that some <strong>people</strong> may need a human aid with<strong>the</strong>m dur<strong>in</strong>g assessment – an <strong>in</strong>terpreter, communicator-guideor advocate.• Managers need to be aw<strong>are</strong> of <strong>the</strong> cost and time implications.Extra time may be required to arrange <strong>in</strong>terpreters. With orwithout <strong>in</strong>terpreters, <strong>the</strong> assessment itself is likely to takeextra time because of <strong>the</strong> specific communication needs of adeafbl<strong>in</strong>d <strong>in</strong>dividual.The effort of concentrat<strong>in</strong>g on communicat<strong>in</strong>g for a prolongedperiod can be exhaust<strong>in</strong>g and may require more than one visit.For <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong> to be at <strong>the</strong> heart of assessment,managers must ensure <strong>the</strong>re is some flexibility <strong>in</strong> meet<strong>in</strong>g targets.Case Study: George, 73George is 73and visuallyimpaired withlittle usefulcentral vision.He is alsoseverely deaf, rely<strong>in</strong>g on twohear<strong>in</strong>g aids to amplify speechand o<strong>the</strong>r environmentalsounds. But he struggles tofollow speech even <strong>in</strong> a quietenvironment.George and his wife hada supportive relationship andmanaged life well withoutsupport. However he appearsto have become depresseds<strong>in</strong>ce his wife’s death.His GP requests an assessmentbecause she is concernedabout his ability to cope on hisown. The overview assessmentis carried out and because <strong>the</strong>assessor has some aw<strong>are</strong>nessof <strong>the</strong> particular difficultiescaused by comb<strong>in</strong>ed hear<strong>in</strong>gand vision loss, she is ableto focus some questionsspecifically on <strong>the</strong>se issues.She realises that a specialistassessment is necessary andmakes <strong>the</strong> appropriate referral.Specialist assessmentidentifies key <strong>are</strong>as of provisionwhich promote <strong>in</strong>dependenceand choice for George.These <strong>in</strong>clude:• a vibrat<strong>in</strong>g pager systemto alert George to callers at<strong>the</strong> door• a loop system to providesome access to <strong>the</strong> TV• skills tra<strong>in</strong><strong>in</strong>g around safety<strong>in</strong> <strong>the</strong> kitchen and homeenvironment• mobility tra<strong>in</strong><strong>in</strong>g whichgives him <strong>the</strong> confidenceto go out alone <strong>in</strong> <strong>the</strong> local<strong>are</strong>a, and• weekly attendanceat a group for visuallyimpaired <strong>people</strong> where hiscommunication needs <strong>are</strong>catered for.9
2 > Legal requirementsB) EligibilityThe eligibility framework for socialc<strong>are</strong> is set out <strong>in</strong> Department of Healthguidance Prioritis<strong>in</strong>g Need <strong>in</strong> <strong>the</strong>Context of Putt<strong>in</strong>g People First. Thisguidance and <strong>the</strong> Deafbl<strong>in</strong>d Guidance<strong>are</strong> of equal status under <strong>the</strong> law.Both <strong>are</strong> statutory guidance issuedunder Section 7 of <strong>the</strong> Local AuthoritySocial Services Act 1970. Toge<strong>the</strong>r <strong>the</strong>ypromote better access, assessmentand services for deafbl<strong>in</strong>d adults .When a decision is be<strong>in</strong>g made about <strong>who</strong> is eligible for social c<strong>are</strong> services,it’s important to recognise <strong>the</strong> effect of dual sensory loss on <strong>the</strong> follow<strong>in</strong>g keyfactors <strong>in</strong> ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g <strong>in</strong>dependence:• autonomy and freedom to make choices• health and safety, <strong>in</strong>clud<strong>in</strong>g freedom from harm, abuse and neglect• personal and daily liv<strong>in</strong>g activities• <strong>in</strong>volvement <strong>in</strong> family and wider community life.The risks relat<strong>in</strong>g to each of <strong>the</strong>se factors <strong>are</strong> considered equal. So risksrelat<strong>in</strong>g to health and safety <strong>are</strong> not considered more important than risksrelat<strong>in</strong>g to <strong>in</strong>volvement. Older <strong>people</strong> with a dual sensory loss can experiencerisk <strong>in</strong> each of <strong>the</strong>se <strong>are</strong>as and <strong>the</strong>y may be at particular risk <strong>in</strong> relation toautonomy and <strong>in</strong>volvement.Case Study: Jim, 82A woman reports that her82 year old fa<strong>the</strong>r <strong>who</strong> isdeaf seemsto havebecomedepressed.Jim doesn’t seem to wantto communicate with hisfamily and isn’t eat<strong>in</strong>g <strong>the</strong>meals provided by socialservices. He has also lost<strong>in</strong>terest <strong>in</strong> his jigsaw puzzles,favourite films and regularp<strong>in</strong>ts at <strong>the</strong> pub nearby. Heseems to be withdraw<strong>in</strong>g <strong>in</strong>tohis own world. What will <strong>the</strong>assessment uncover?Because Jim is still manag<strong>in</strong>gto carry out his own personalc<strong>are</strong> and is supported with dailyliv<strong>in</strong>g tasks by his daughter<strong>who</strong> visits twice a week, ageneric overview assessmentconcludes that <strong>the</strong> risks to his<strong>in</strong>dependence <strong>are</strong> moderate(and outside <strong>the</strong> band<strong>in</strong>gthat would make him eligiblefor services <strong>in</strong> <strong>many</strong> localauthorities).If a deafbl<strong>in</strong>d person is screened out at this <strong>in</strong>itial stage, this will notmeet <strong>the</strong> requirements of <strong>the</strong> Deafbl<strong>in</strong>d Guidance. This states that allassessments of deafbl<strong>in</strong>d <strong>people</strong> (<strong>in</strong>clud<strong>in</strong>g eligibility assessments) shouldbe carried out by someone specifically tra<strong>in</strong>ed to do so. This is an importantmessage of <strong>the</strong> Guidance.10
More about Jim, 82A specialistassessmentdiscovers thathis sight isdeteriorat<strong>in</strong>gand is affect<strong>in</strong>ghis ability to lipread <strong>people</strong>,access leisure activities <strong>in</strong><strong>the</strong> home, and get out <strong>in</strong> <strong>the</strong>local <strong>are</strong>a. His autonomy and<strong>in</strong>volvement <strong>are</strong> substantiallythreatened and he is eligiblefor services.Simple services will make adifference: communication tipsfor both him and his familycan improve his <strong>in</strong>volvement<strong>in</strong> conversation; task light<strong>in</strong>gcan help him see his meal andfeel more like eat<strong>in</strong>g it; simplemobility tra<strong>in</strong><strong>in</strong>g means he canget back out to <strong>the</strong> local pub.An assessor with specialist understand<strong>in</strong>g of <strong>the</strong> needs of <strong>older</strong>deafbl<strong>in</strong>d <strong>people</strong> will emphasise <strong>the</strong> effects of hear<strong>in</strong>g and visiondifficulties as well as assess<strong>in</strong>g <strong>the</strong> effects of age<strong>in</strong>g, vulnerabilityor o<strong>the</strong>r disabl<strong>in</strong>g conditions. Specific support to promote<strong>in</strong>dependence <strong>in</strong> relation to deafbl<strong>in</strong>dness can <strong>in</strong>clude:• simple communication strategies• equipment• help to f<strong>in</strong>d new ways of carry<strong>in</strong>g out daily tasks• mobility tra<strong>in</strong><strong>in</strong>g, or• one-to-one support.Recognis<strong>in</strong>g deafbl<strong>in</strong>dnessAs <strong>the</strong> team most likely to come <strong>in</strong>to contact with <strong>older</strong> <strong>people</strong>with dual sensory loss, it’s important to make sure that all staff <strong>are</strong>tra<strong>in</strong>ed to recognise deafbl<strong>in</strong>dness and its effect on <strong>in</strong>dependence(see Resources section for <strong>in</strong>formation about tra<strong>in</strong><strong>in</strong>g – page 23).Learn to recognise <strong>the</strong> disability and how <strong>people</strong> can be supported– ra<strong>the</strong>r than accept<strong>in</strong>g it as simply part of <strong>the</strong> age<strong>in</strong>g processwhich can’t be helped. Why not develop a ‘champion’ for sensoryissues with<strong>in</strong> your team?The eligibility guidancealso requires assessmentsto take account of needswhich could <strong>in</strong>crease.Local authorities shouldnot wait until <strong>the</strong> needreaches a higher bandbefore provid<strong>in</strong>g a service.11
2 > Legal requirementsCase Study: Hyac<strong>in</strong>th, 79A 79 year oldBUS STOP bl<strong>in</strong>d woman<strong>who</strong> usesa hear<strong>in</strong>gaid to support herdeteriorat<strong>in</strong>g hear<strong>in</strong>glives <strong>in</strong>dependently andcopes well at home <strong>in</strong>a familiar environment.However outside <strong>the</strong> homeshe is experienc<strong>in</strong>g <strong>in</strong>creas<strong>in</strong>gdifficulty.She can no longer get <strong>the</strong>bus to <strong>the</strong> shops as she can’tsee <strong>the</strong> bus numbers andrelies on o<strong>the</strong>r <strong>people</strong> to tellher which bus has arrived.Because of <strong>the</strong> backgroundnoise of traffic, she can’<strong>the</strong>ar what <strong>people</strong> <strong>are</strong> say<strong>in</strong>gand has felt confused andunable to travel. As well asshopp<strong>in</strong>g for food, her weeklytrip is a vital l<strong>in</strong>k to <strong>the</strong> ethniccommunity where she isknown. Because of this she isreluctant to use a shopp<strong>in</strong>gservice.If a one-to-onecommunicator-guide isprovided at this stage itwill ensure her cont<strong>in</strong>ued<strong>in</strong>volvement, enable herto make <strong>in</strong>dependentchoices and prevent fur<strong>the</strong>rdeterioration. Without this,Hyac<strong>in</strong>th is at risk of los<strong>in</strong>gskills and requir<strong>in</strong>g higherlevels of c<strong>are</strong>, <strong>in</strong>clud<strong>in</strong>g<strong>the</strong> possibility of need<strong>in</strong>gresidential c<strong>are</strong>.12
C) PersonalisationIt is important to ensure thatpersonalisation is carried out <strong>in</strong> a waywhich delivers appropriate services todeafbl<strong>in</strong>d <strong>older</strong> <strong>people</strong>. There <strong>are</strong> somekey po<strong>in</strong>ts to note when implement<strong>in</strong>ga personalised approach to support for<strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong>. The underly<strong>in</strong>glaw on social c<strong>are</strong> has not changed solocal authority duties rema<strong>in</strong> <strong>the</strong> sameand <strong>the</strong> requirements of <strong>the</strong> deafbl<strong>in</strong>dguidance still apply.• Assessment – Anyone <strong>who</strong> appears to be <strong>in</strong> need of acommunity c<strong>are</strong> service is entitled to an assessment. Wherethat person is deafbl<strong>in</strong>d <strong>the</strong>y <strong>are</strong> entitled to an assessmentcarried out by someone <strong>who</strong> is specifically tra<strong>in</strong>ed to assess adeafbl<strong>in</strong>d person. Ask<strong>in</strong>g a person to complete a self-assessmentquestionnaire will not be sufficient to meet this duty.• Direct payments – Everyone has <strong>the</strong> option to receivea direct payment <strong>in</strong> place of a service. Many <strong>older</strong> deafbl<strong>in</strong>d<strong>people</strong> do not wish to take up a direct payment, often becauseof <strong>the</strong> paperwork and responsibility of manag<strong>in</strong>g a budget.<strong>Sense</strong> has <strong>in</strong>formation that will help councils ensure <strong>the</strong>ir directpayments support services can meet <strong>the</strong> needs of deafbl<strong>in</strong>d<strong>people</strong>. However good <strong>the</strong> support services, <strong>the</strong>re will be anumber of <strong>people</strong> <strong>who</strong> choose not to take up this option and<strong>the</strong>y must be provided with an appropriate service.• Service provision – Deafbl<strong>in</strong>d <strong>people</strong> have a rightto a service which meets <strong>the</strong>ir needs as a deafbl<strong>in</strong>d person.A communicator guide, for <strong>in</strong>stance, will usually be moreexpensive per hour than a personal assistant because of <strong>the</strong>skills and tra<strong>in</strong><strong>in</strong>g required. Deafbl<strong>in</strong>d <strong>people</strong> assessed asneed<strong>in</strong>g such a service must be able to receive one. Where<strong>the</strong>y have a personal budget, this must be sufficient to meet<strong>the</strong>se specialist needs.Putt<strong>in</strong>g Everyone First, aguide to personalisationfor all groups is availablefrom <strong>Sense</strong> atwww.sense.org.uk/help_and_advice/social_services/putt<strong>in</strong>g_everyone_first• Resource allocation – Resource Allocation Systems(RAS) often fail to take account of deafbl<strong>in</strong>d <strong>people</strong>’s needs.The personal budget will often have to be higher than <strong>the</strong><strong>in</strong>dicative budget generated by <strong>the</strong> RAS to take account of this.A group of organisations have produced Putt<strong>in</strong>g Everyone First,a guide to <strong>the</strong> issues that must be taken <strong>in</strong>to account to makepersonalisation work for everyone.13
3 > Work<strong>in</strong>g with <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong>In this section we will look at some of <strong>the</strong> simple, practicalsteps you can take to help you to identify <strong>older</strong> deafbl<strong>in</strong>d<strong>people</strong>, communicate effectively and provide <strong>in</strong>formation<strong>in</strong> accessible formats.Understand<strong>in</strong>g<strong>the</strong> needs of <strong>older</strong>deafbl<strong>in</strong>d14
How can your team work effectively with<strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong>?As we have seen, <strong>older</strong> <strong>people</strong> <strong>who</strong> can’t see or hear fullywhat is go<strong>in</strong>g on around <strong>the</strong>m may f<strong>in</strong>d <strong>the</strong> physical andsocial environment confus<strong>in</strong>g or even hostile. The effortand skills required to go out or engage <strong>in</strong> social activitycan be very tir<strong>in</strong>g and may lead to <strong>in</strong>creas<strong>in</strong>g withdrawaland isolation.There is also an emotional reaction to dual sensory loss.People <strong>are</strong> cut off from <strong>the</strong> world around <strong>the</strong>m as <strong>the</strong>yused to experience it and this can lead to feel<strong>in</strong>gs of loss,frustration, anger and grief.In this section we will look at some of <strong>the</strong> simple, practicaladjustments that will help you to identify <strong>older</strong> deafbl<strong>in</strong>d<strong>people</strong>, communicate effectively and provide <strong>in</strong>formation <strong>in</strong>accessible formats.An <strong>older</strong> deafbl<strong>in</strong>d person is likely to needhelp <strong>in</strong> <strong>the</strong> follow<strong>in</strong>g <strong>are</strong>as:• Communication• Information – <strong>in</strong>clud<strong>in</strong>gpublic <strong>in</strong>formation• Mobility and transport• Stimulation and relieffrom isolation• Emotional supportand counsell<strong>in</strong>g• Equipment• Hous<strong>in</strong>g15
3 > Work<strong>in</strong>g with <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong>The follow<strong>in</strong>gchecklists will helpyou recognise some of<strong>the</strong> frequent <strong>in</strong>dicatorsof hear<strong>in</strong>g and visionloss. These <strong>are</strong> notcomplete lists; some<strong>people</strong> may exhibitnone of <strong>the</strong>se signsand you may observeo<strong>the</strong>rs not listed.F<strong>in</strong>ds it hard tofollow speechIndicators of hear<strong>in</strong>g and vision lossA person with hear<strong>in</strong>g difficulties may:• Compla<strong>in</strong> that o<strong>the</strong>rs mumble or speak too quickly• Ask o<strong>the</strong>rs to repeat what <strong>the</strong>y’ve said• Ask o<strong>the</strong>rs to speak louder• Repeat words to verify what’s been said• F<strong>in</strong>d it difficult to keep up conversations <strong>in</strong> noisyenvironments or <strong>in</strong> a group• Have difficulty understand<strong>in</strong>g unfamiliar <strong>people</strong> or accents• Get tired <strong>in</strong> conversations because of <strong>the</strong> need toconcentrate• Withdraw from situations where conversation is expected• Need TV or radio volume louder than is comfortable foro<strong>the</strong>rs• F<strong>in</strong>d it hard to hear on <strong>the</strong> telephone• Use a hear<strong>in</strong>g aid or loop system.Sits close to <strong>the</strong> TVA person with visual difficulties may:• F<strong>in</strong>d it hard to identify objects or familiar faces• Need more light for read<strong>in</strong>g and o<strong>the</strong>r activities• F<strong>in</strong>d it hard to cope with gl<strong>are</strong>, e.g. bright sunlight• Sit unusually close to <strong>the</strong> TV• Have unusual read<strong>in</strong>g habits, e.g. hold<strong>in</strong>g a book closeto <strong>the</strong> face• Give up read<strong>in</strong>g, watch<strong>in</strong>g television or o<strong>the</strong>r activities• Be unable to locate small objects• Spill food or knock over cups• Wear mismatched colours or have sta<strong>in</strong>ed cloth<strong>in</strong>g• Have difficulty mov<strong>in</strong>g around – walk<strong>in</strong>g slowly or with lessconfidence• Bump <strong>in</strong>to th<strong>in</strong>gs• Have difficulties caused by changes <strong>in</strong> light levels• Have difficulties with unfamiliar routes or places.16
Communicat<strong>in</strong>g effectively – face to faceBefore you start:• Make sure you have <strong>the</strong> person’s attention• Always tell a visually impaired person that you <strong>are</strong> <strong>the</strong>re• Ask <strong>the</strong> person what will make communication effectiveand do that.Older <strong>people</strong> withdual sensory lossoften have problemswith communication.If we use commonsense, clear speechand courtesy we canhelp an <strong>older</strong> personto understandwhat is be<strong>in</strong>g said.Simple solutionscan improve <strong>the</strong>environmentdramatically fordeafbl<strong>in</strong>d <strong>people</strong>.Where to talk:• Between 3 – 6 feet apart at <strong>the</strong> same level• Good light is important. Face <strong>the</strong> light so that your full face canbe seen• Avoid background noise. Turn it off or move somewhere quieter.Clear speech:•Speak clearly• Speak a little more slowly than usual, but keep <strong>the</strong> naturalrhythm of speech• Speak a little louder, but don’t shout as this will distort yourvoice and lip patterns• Try to make your lip patterns clear, but don’t over-exaggerate• Keep your face visible and your head still. Don’t smoke, eat,chew gum or cover your mouth with your hand• Focus on <strong>the</strong> person you <strong>are</strong> talk<strong>in</strong>g to. If you <strong>are</strong> us<strong>in</strong>g an <strong>in</strong>terpreter,always talk directly to <strong>the</strong> deaf person, not <strong>the</strong> <strong>in</strong>terpreter.Help <strong>the</strong> o<strong>the</strong>r person to understand:• Don’t hurry, take your time• If necessary, repeat phrases. If this doesn’t work, tryre-phras<strong>in</strong>g <strong>the</strong> <strong>who</strong>le sentence. Some words <strong>are</strong> easier tolip-read than o<strong>the</strong>rs• Make <strong>the</strong> subject clear from <strong>the</strong> start and if you change <strong>the</strong>subject, make sure <strong>the</strong> person knows• Use gestures and facial expression to support what you <strong>are</strong> say<strong>in</strong>g• Be aw<strong>are</strong> that if a person is smil<strong>in</strong>g and nodd<strong>in</strong>g it doesn’tnecessarily mean <strong>the</strong>y have understood you• Be aw<strong>are</strong> that <strong>the</strong> effort of concentration on communicat<strong>in</strong>gcan be hard work for an <strong>older</strong> deafbl<strong>in</strong>d person and cannot bema<strong>in</strong>ta<strong>in</strong>ed for long periods of time• Assessments <strong>are</strong> likely to take more than one visit and extra timewill need to be allocated• Be ready to write th<strong>in</strong>gs down, us<strong>in</strong>g an A4 note pad with ablack marker pen.17
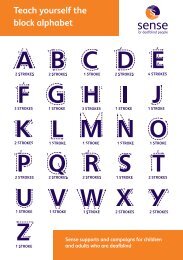
3 > Work<strong>in</strong>g with <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong>InterpretersSome <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong> use specialist forms ofcommunication and will require communication supportdur<strong>in</strong>g <strong>the</strong> assessment process. You will need to know whatform of communication <strong>the</strong> deafbl<strong>in</strong>d person uses and bookappropriate <strong>in</strong>terpreters well <strong>in</strong> advance. Communicationmethods may <strong>in</strong>clude:• British Sign Language• Deafbl<strong>in</strong>d manual alphabet• Block• Lip-speak<strong>in</strong>g• Speech to text• Community languages.Your local sensoryteam can provide<strong>in</strong>formation aboutbook<strong>in</strong>g <strong>in</strong>terpretersand <strong>the</strong>re is<strong>in</strong>formation <strong>in</strong> <strong>the</strong>Resources sectionat <strong>the</strong> back of thisbooklet.Communicat<strong>in</strong>g effectively – at a distanceTelephoneMany <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong>have difficulty us<strong>in</strong>g <strong>the</strong>telephone but cont<strong>in</strong>ueto depend on it. Here <strong>are</strong>some simple tips to help youcommunicate effectively on<strong>the</strong> telephone.• Use <strong>the</strong> clear speech skillsdescribed earlier• Don’t shout or hold <strong>the</strong>phone too close to yourmouth, as this causesdistortion• Don’t speak too quietly• When phon<strong>in</strong>g a personwith dual sensory loss,give <strong>the</strong>m time to adjust<strong>the</strong>ir hear<strong>in</strong>g aid beforestart<strong>in</strong>g <strong>the</strong> conversation• Keep answer phonemessages short and simple.18
TextphonesTextphones allow deaf and hard of hear<strong>in</strong>g <strong>people</strong> tocommunicate through <strong>the</strong> standard telephone network.Textphones have a display screen and keyboard so that <strong>the</strong> usercan type what <strong>the</strong>y want to say and read <strong>the</strong> typed reply. Somedeafbl<strong>in</strong>d <strong>people</strong> use textphones with a large display screen.Information about different types of telephones and textphonescan be found on <strong>the</strong> RNID website: www.rnid.org.ukBT provides services for <strong>people</strong> with sensory impairments,<strong>in</strong>clud<strong>in</strong>g free directory enquiries for visually impaired <strong>people</strong>(call 195) and text-based phone services for deaf or hard ofhear<strong>in</strong>g <strong>people</strong>.BT Text Relay is a national telephone relay service.Deafbl<strong>in</strong>d textphone users can type messages to <strong>the</strong> Text Relayoperator <strong>who</strong> <strong>the</strong>n relays <strong>the</strong> message <strong>in</strong> speech to a hear<strong>in</strong>gperson on a standard phone. The spoken reply is <strong>the</strong>n relayedby <strong>the</strong> operator by typ<strong>in</strong>g it as text.Textphone users call<strong>in</strong>g a voice phone user dial <strong>the</strong> prefix18001 and <strong>the</strong>n <strong>the</strong> phone number <strong>the</strong>y want. Voice phoneusers call<strong>in</strong>g a textphone user dial <strong>the</strong> prefix 18002 <strong>the</strong>n <strong>the</strong>textphone number <strong>the</strong>y want.19
3 > Work<strong>in</strong>g with <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong>Written <strong>in</strong>formationAll <strong>in</strong>formation and correspondence that your team providesshould be available <strong>in</strong> accessible formats. For example,appo<strong>in</strong>tment letters, assessments, c<strong>are</strong> plans, <strong>in</strong>formation aboutservices, etc. should be available <strong>in</strong> large pr<strong>in</strong>t, braille, tape or disk.Many visually impaired <strong>people</strong> have enough vision to read pr<strong>in</strong>ted<strong>in</strong>formation if it is large and bold. No s<strong>in</strong>gle size is suitable foreveryone, but most <strong>people</strong> prefer <strong>the</strong>ir large pr<strong>in</strong>t <strong>in</strong> <strong>the</strong> range of16 to 22 po<strong>in</strong>t. Arial is an example of a clear font. You can wordprocess simple large pr<strong>in</strong>t documents yourself.If a person requires <strong>in</strong>formation <strong>in</strong> braille, audio tape or diskformats, you can use any number of transcription services.If <strong>in</strong> doubt, contact your local sensory team or o<strong>the</strong>r specialistsensory agencies such as <strong>Sense</strong>, Deafbl<strong>in</strong>d UK or RNIB.This is anexample ofArial 18 po<strong>in</strong>t<strong>in</strong> bold.Specialist servicesThis is a brief overview of <strong>the</strong>services that may be availablefor <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong>via your sensory impairmentteam (or similar):• Specialist assessment andc<strong>are</strong> plann<strong>in</strong>g – assess<strong>in</strong>g<strong>the</strong> effects of hear<strong>in</strong>g andvision difficulties and <strong>the</strong>irimpact on ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g<strong>in</strong>dependence.• Advice, <strong>in</strong>formation andadvocacy – access<strong>in</strong>ghealth and social services,welf<strong>are</strong> rights, nationaldeafbl<strong>in</strong>d organisations,local agencies.• Equipment – assessmentand provision of equipmentto assist with everydayactivities: e.g. easy-to-seeamplified phones; largescreen textphones; personalTV listeners; loop systems;tactile markers; vibrat<strong>in</strong>gpager systems for doorbell,telephone or smoke alarmalert<strong>in</strong>g.• Mobility tra<strong>in</strong><strong>in</strong>g – <strong>in</strong>clud<strong>in</strong>gadvice on mak<strong>in</strong>g <strong>the</strong> homesafer to move around <strong>in</strong> ortra<strong>in</strong><strong>in</strong>g <strong>in</strong> travell<strong>in</strong>g outdoors<strong>in</strong>dependently and safely.• Communication – <strong>in</strong>clud<strong>in</strong>gsupport to developappropriate communicationskills for both <strong>the</strong> deafbl<strong>in</strong>dperson <strong>the</strong>mselves andfamily members or c<strong>are</strong>rsand <strong>in</strong>formation about us<strong>in</strong>g<strong>in</strong>terpreters.• O<strong>the</strong>r skills tra<strong>in</strong><strong>in</strong>g –<strong>in</strong>clud<strong>in</strong>g safety <strong>in</strong> <strong>the</strong> kitchenand home environment.• One-to-one support – e.g.communicator-guide services.Communicator-guides <strong>are</strong>tra<strong>in</strong>ed to help deafbl<strong>in</strong>d<strong>people</strong> with communicationand mobility to enable<strong>the</strong>ir <strong>in</strong>volvement <strong>in</strong> everyday activities and relieveisolation. The tasks carriedout will vary depend<strong>in</strong>gon <strong>the</strong> <strong>in</strong>dividual deafbl<strong>in</strong>dperson and <strong>the</strong>ir needs,but may <strong>in</strong>clude: attend<strong>in</strong>gappo<strong>in</strong>tments; escort<strong>in</strong>gto <strong>the</strong> shops; read<strong>in</strong>gcorrespondence; tak<strong>in</strong>gexercise; leisure activities.This service is designedto complement o<strong>the</strong>rservices (e.g. Home C<strong>are</strong>)and should not be used toreplace it.i20
What to dowhen you’veread this…1. Discuss <strong>the</strong> needs of <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong> atone of your team meet<strong>in</strong>gs. Th<strong>in</strong>k about some of<strong>the</strong>se questions:• Do we recognise that comb<strong>in</strong>ed hear<strong>in</strong>g and vision loss<strong>in</strong>teract to create a separate and unique disability?• Do we know of local <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong>? How <strong>many</strong> <strong>are</strong>we aw<strong>are</strong> of?• How can we develop our skills <strong>in</strong> identify<strong>in</strong>g deafbl<strong>in</strong>d<strong>people</strong>? What tra<strong>in</strong><strong>in</strong>g is available? Who should be tra<strong>in</strong>ed?Could one team member be appo<strong>in</strong>ted as a ‘sensorychampion’?• When assess<strong>in</strong>g <strong>older</strong> <strong>people</strong>, do we th<strong>in</strong>k about <strong>the</strong>possibility of dual sensory loss and its effects?• When assess<strong>in</strong>g <strong>older</strong> <strong>people</strong>, do we adapt sufficiently to<strong>the</strong>ir communication needs? Do we know how to access<strong>in</strong>terpreters or o<strong>the</strong>r communication support if necessary?• Is our assessment <strong>in</strong>formation accessible to users and c<strong>are</strong>rs<strong>who</strong> have dual sensory loss?• How can we use <strong>the</strong> Disability Discrim<strong>in</strong>ation Act 1995 topromote <strong>the</strong> <strong>in</strong>terests of <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong>?• What services <strong>are</strong> provided locally for <strong>older</strong> deafbl<strong>in</strong>d <strong>people</strong>via statutory or voluntary agencies?• Do we know when and where to refer on for specialistassessment?2. F<strong>in</strong>d out how to contact your local sensory teamand write <strong>the</strong>ir phone number here:3. Consider <strong>in</strong>vit<strong>in</strong>g a specialist from <strong>the</strong> sensoryteam to your team meet<strong>in</strong>g to discuss howyou can work toge<strong>the</strong>r effectively with <strong>older</strong>deafbl<strong>in</strong>d <strong>people</strong>.4. Consider organis<strong>in</strong>g an event dur<strong>in</strong>g Deafbl<strong>in</strong>dAw<strong>are</strong>ness Week.21
4 > ResourcesThere <strong>are</strong> a range of organisations, publications andresources which can help you improve services todeafbl<strong>in</strong>d <strong>older</strong> <strong>people</strong>.Re ferences andorganisationsuseful<strong>Sense</strong>’s Information & Advice Service<strong>Sense</strong>’s Information & Advice Service offers accurate,comprehensive and up-to-date impartial <strong>in</strong>formationand advice for deafbl<strong>in</strong>d <strong>people</strong>, <strong>the</strong>ir families, professionalswork<strong>in</strong>g with deafbl<strong>in</strong>d <strong>people</strong> and anyone <strong>who</strong> has ageneral enquiry about <strong>Sense</strong> or any aspect of deafbl<strong>in</strong>dness.The service covers England, Wales and Nor<strong>the</strong>rn Ireland.Contact <strong>the</strong> Information and Advice Service:Tel: 0845 127 0066Textphone: 0845 127 0062Fax: 0845 127 0061Email: <strong>in</strong>fo@sense.org.uk22
Useful organisations:<strong>Sense</strong>101 Pentonville RoadLondon N1 9LGTel: 0845 127 0066Textphone: 0845 127 0062<strong>in</strong>fo@sense.org.ukwww.sense.org.ukRNID19-23 Fea<strong>the</strong>rstone StreetLondon EC1Y 8SLTelephone: 0808 808 0123Textphone: 0808 808 9000<strong>in</strong>formationl<strong>in</strong>e@rnid.org.ukwww.rnid.org.ukDeafbl<strong>in</strong>d Aw<strong>are</strong>nessTra<strong>in</strong><strong>in</strong>gFor <strong>in</strong>formation abouttra<strong>in</strong><strong>in</strong>g, contact <strong>the</strong><strong>Sense</strong> Information & AdviceService See contact detailson page 22Deafbl<strong>in</strong>d UKNational Centre forDeafbl<strong>in</strong>dnessJohn and Lucillevan Geest PlaceCygnet RoadHampton, PeterboroughCambridgeshire PE7 8FDHelpl<strong>in</strong>e tel/text: 0800 132 320www.deafbl<strong>in</strong>d.org.ukRNIB105 Judd StreetLondon WC1H 9NETel: 0303 123 9999helpl<strong>in</strong>e@rnib.org.ukwww.rnib.org.ukInterpret<strong>in</strong>gFor <strong>in</strong>formation about us<strong>in</strong>g<strong>in</strong>terpreters, contact yourlocal sensory team or <strong>the</strong><strong>Sense</strong> Information andAdvice Service23
4 > ResourcesReferences:Butler, S J (2004) Hear<strong>in</strong>g and Sight Loss – A handbook forprofessional c<strong>are</strong>rs, Age Concern EnglandDepartment of Health (1997) Th<strong>in</strong>k Dual Sensory – GoodPractice Guidel<strong>in</strong>es for Older People with Dual Sensory LossHodges, L and Douglas, G (2005) Short Study on hear<strong>in</strong>g andsight loss – Prelim<strong>in</strong>ary Report for The Thomas Pockl<strong>in</strong>gtonTrust University of Birm<strong>in</strong>ghamPrioritis<strong>in</strong>g need <strong>in</strong> <strong>the</strong> context of Putt<strong>in</strong>g People First:A <strong>who</strong>le system approach to eligibility for social c<strong>are</strong>:Guidance on Eligibility Criteria for Adult Social C<strong>are</strong>, England,Department of Health (2010)Local Authority Social Services Act (1970) – Section 7 Guidance,Social C<strong>are</strong> for Deafbl<strong>in</strong>d Children and Adults LAC(DH)(2009)6Third European Conference of Deafbl<strong>in</strong>d International’sAcquired Deafbl<strong>in</strong>dness Network proceed<strong>in</strong>gs (1998)Elderly Deafbl<strong>in</strong>dnessRobertson, J & Emerson, E Estimat<strong>in</strong>g <strong>the</strong> Number of Peoplewith Co-occurr<strong>in</strong>g Vision and Hear<strong>in</strong>g Impairments <strong>in</strong> <strong>the</strong> UKCeDR Lancaster (2010)Web based resources:To make <strong>in</strong>formation accessible –see RNIB’s ‘See it Right’ pack – available at www.rnib.org.ukDepartment of Health website www.dh.gov.uk<strong>Sense</strong> website www.sense.org.uk24
Thank you for tak<strong>in</strong>g<strong>the</strong> time to read thisbooklet. We hopeyou f<strong>in</strong>d it useful, andthat you can help tofill <strong>in</strong> <strong>the</strong> gaps <strong>in</strong> <strong>older</strong>deafbl<strong>in</strong>d <strong>people</strong>’s lives.<strong>Fill</strong> <strong>in</strong> <strong>the</strong> <strong>Gaps</strong> >
This booklet offers<strong>in</strong>formation and adviceabout work<strong>in</strong>g with <strong>older</strong>deafbl<strong>in</strong>d <strong>people</strong>. It expla<strong>in</strong>swhat deafbl<strong>in</strong>dness is andhow it affects <strong>people</strong>.It sets out <strong>the</strong> legalresponsibilities that socialservices have and expla<strong>in</strong>show deafbl<strong>in</strong>d <strong>people</strong> canbe supported and helped.<strong>Sense</strong>101 Pentonville RoadLondon N1 9LGTel: 0845 127 0066Text: 0845 127 0062Fax: 0845 127 0061March 2011Email: <strong>in</strong>fo@sense.org.ukWebsite: www.sense.org.ukReg. charity no.: 289868Design: www.fabrikbrands.com