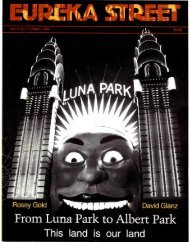
n - Eureka Street
n - Eureka Street
n - Eureka Street
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
0 NM"c" 25, 1997 the membm olthe Commonwealth Senate voted, 38 to 33,to confirm the resolution of their colleaguesin the House of Representatives that thePrivate Member's Euthanasia Bill shouldbecome law.The Bill, introduced into the LowerHouse six months previously by Liberalback-bencher Kevin Andrews, had been approvedby 88 votes to 35 in the House ofRepresentatives.The effect of the Senate vote was tooverturn the Northern Territoryvoluntary euthanasia legislation, TheRights of the Terminally Ill Act 1995,which had been approved with a narrowmajority by the Territory's parliamentarianson May 25th, 1995.The debate which attended the passingof the Andrews' Bill, in both theLower and Upper Houses was complicatedby the following factors:• the support given to the Bill by boththe Prime Minister and the Leader ofthe Opposition;• the whole question of States' andTerritories' rights,• the inadequacies of the NorthernT erritory legislative drafting;• the wider implications that the TerritoryAct might have for the continuingaccess of the Aboriginal community tohealth care;•the distinction between private moralityand public legislation;• the posturings of some of the proponentson both sides.T he way in which variou s responseswere represented in the media confused theissue even further. But those who listenedto the parliamentary hearings and thediscussion in both Houses were on thew hole impressed by the qu ality of thedebate. The manner of our dying, especiallyin this age of m edico-scientific technology,is obviously a matter that concerns usgreatly. The fact that there were over 12,000submissions to the Senate Committee isabundant evidence of this.At the height of the debate on February17th, 1997, three of the m ost outspokensupporters of the N orthern Territory legislationand of active voluntary euthanasiapublished a research study on 'End-of-lifeETHICSW.J. U RENLife and death mattersDecisions in Australian Medical Practice'in the Medical Journal of Australia. T heywere Dr Helga Kuhse and Professor PeterSinger, from the Monash University Centreof Human Bioethics, and Professor PeterBaume, from the School of Community Medicineat the University of New South Wales.They based their study on the 24 itemsof a questionnaire which replicated onecirculated origina lly to medicalpractitioners in the Netherlands by theRemmelink Commission in 1990 and 1995.Questionnaires were mailed to 3000Australian doctors who might possibly beinvolved in m aking end-of-life m edicaldecisions. There were 1918 responses ( 64percent) of whom 1361 hadattendedanonacutedeath within the last 12 months. Thisfield was further narrowed 'by excludingdoctors who in respect of that death had nocontact with the patient until after thatdeath or where the death had been suddenand totally unexpected'. Of the remaining111 2 doctors, 800 doctors reported m akinga decision either intended to shorten life orforeseen as probably or certainly shorteninglife. The other 3 12 doctors did not makesuch a decision .In analysing the responses from these1112 doctors the authors of the researchdrew as a 'main finding' that 30 per cent(±3.3 per cent) of all Australian deaths werepreceded by a m edical decision explicitlyintended to hasten the patient's dea th:doctors prescribed, supplied or administereddrugs with the explicit intention ofending the patient's li fe in 5.3 per cent(±lper cent) of these deaths, and withdrewor withheld life-prolonging treatment withthe explicit intention of not prolonging lifeor of hastening death in 24.7 per cent (±3 .1 percent) of these deaths.Further, 'in 22.5 per cent ('3. 1per cent)of all Australian deaths, doctors withheldor withdrew treatment from patients withoutthe patient's explicit request, with theexplicit intention of ending life' (M[A,17 February 1997, p195) . TheseAustralian figures, it was furthermaintained, are in the range of 50per cent higher than the figures forcorresponding categories"""J"'"' in the Netherlands..1. HE CONCLUSION DRAWN by the authorsof the study from their analysis of thesurvey was that one of the reasons whysome Australian doctors may be choosingintentionally to end the li ves of theirpatients without consulting the patientsthemselves, was that existing Australianlaws prohibiting euthanasia maymake doctors 'reluctant to discussm edical end-of-life decisions with theirpatients lest these decisions be construedas collaboration in euthanasia or in theintentional termination of life'.The authors are then, in effect, arguingfor a relaxation of the existing laws topermit active voluntary euthanasia. This,they say, will ensure that patients would beconsulted by their doctors, where possible(i.e. if they are competen t) both before lifeprolongingtreatment is withdrawn or withheldwith a lethal intention, and beforeanalgesic drugs were administered in suchquantities that the hastening of death wasnot only intended but virtually inevitable.This line of argument may well seem tobe more than a little paradoxical. One isinclined to subsume: if this is what ishappening when there is no legislationcondoning active voluntary euthanasia, willnot the practice of all forms of euthanasiabecome even more prevalent if it is legalised?The authors of the study argue to thecontrary. Not only will such legislation,they say, promote the autonom y of those18 EUREKA STREET • MAY 1997