Synapse 2013 Vol. 1 - The Chester County Hospital
Synapse 2013 Vol. 1 - The Chester County Hospital
Synapse 2013 Vol. 1 - The Chester County Hospital
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
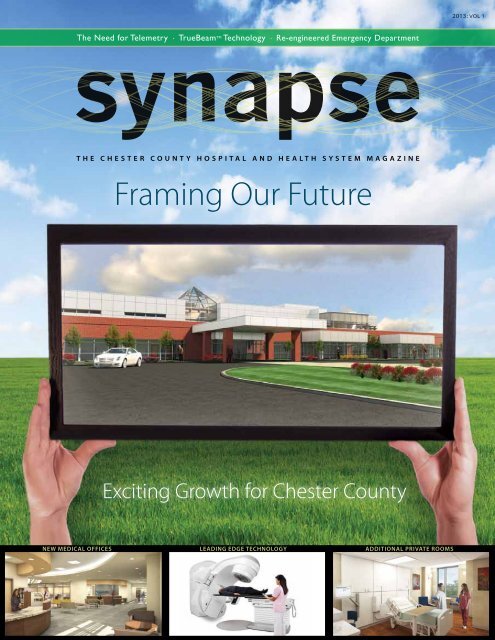
Extending our Reach... continuedalso committed to being a good neighbor.“What we try to do with all our buildings is create apatient-focused design that provides ‘one-stop shopping’for health care. We strive to create a calming and reassuringenvironment within a building design that is easyto maneuver,” says Crowley.Inside the building, guests will be greeted by aconcierge who can assist them with questions and helpthem navigate the building. <strong>The</strong> lobby will have a seatingarea and a café for refreshments and light meals forpurchase. Well-located community rooms will become aentral location for wellness programs, physician outreachevents and health fairs. This space will also be availableto community groups to use as a gathering placefor independent events.Outside, the large property will complement the naturallandscape and beauty of southern <strong>Chester</strong> <strong>County</strong>.It will include high-quality, natural materials with warmcolor tones and a lot of natural light, much like the fields,farms and forests that are so indicative of the area.Anchor doesn’t build cookie-cutter buildings, butrather it seeks inspiration from the location itself.<strong>The</strong> concepts for the plant materials and stone workhave been inspired by the historic national landmarksthat characterize the area. <strong>The</strong> property will maintainmuch of its greenery and wooded features, and aexterior renderingJenners VillageMedical Campus> Primary care, Internal Medicineand Family Practice Physicians> Specialty Physician Offices> After-hours Family PracticeCare and X-ray for urgentmedical situations> Diagnostic services, such asRadiology* and LaboratoryInterior rendering> Physical <strong>The</strong>rapy> Ambulatory surgery Centerfor outpatient procedures> Amenities, such as concierge,café, and communityconference space* <strong>The</strong> state-of-the-art Radiology suitewill include MRI, CT, X-ray, DigitalMammography, DEXA, and Ultrasound—withroom to expand.4synapse
wellness path will be added toallow members of the communityto enjoy the land as they achievetheir own fitness milestones.“We understand the cultureof <strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong>and Health System,” says Crowley,“And that personality willbe reflected in the character ofthis project.”So, much like the main <strong>Hospital</strong>facility in West <strong>Chester</strong>, the newMedical Office Building will strikethe balance between providingpatients a high-tech environmentwithin a warm and friendly workof architecture. <strong>The</strong> <strong>Hospital</strong>’s93,000-square-foot Tower Project,too, has been designed to<strong>The</strong> Jennersvilleproperty will maintainmuch of its greenery andwooded features, anda wellness path will beadded to allow membersof the community toenjoy the land as theyachieve their ownfitness milestones.complement the Italianate stylethat is unique to the <strong>Hospital</strong>, whileproviding state-of-the art medicalcare within those new walls.A developing new partnershipwith the University of PennsylvaniaHealth System will blend the clinicalexcellence and innovations of bothinstitutions for the benefit of everyone.Although there have beenmany changes through the years,one thing remains the same: <strong>The</strong><strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong> and HealthSystem is grounded in the communityfrom which it grew. And italways will be. <strong>The</strong> future has neverheld so much promise.By Lisa M. Huffman andLauren A. Speakmanlearn More atwww.chestercountyhospital.org/synapse<strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong> and Health System 5
Stable RhythmsAdditional Telemetry rooms Will Expand Heart Monitoring capacityIf you saw the last issue of <strong>Synapse</strong>, you learned about the newPatient Tower and all of its patient-centered features—fromprivate rooms filled with natural light, to more space forvisitors, to bathrooms with fall-prevention features. (If youmissed the issue, visit chestercountyhospital.org/synapse.)Now we want to tell you more about the first unit that willopen on the top floor this summer: Telemetry. In addition tobeing patient-centered, the unit is intentionally designed tomeet the needs of clinical staff, whose input was critical tothe project.Over the past decade or so, many healthcare serviceshave shifted from inpatient to outpatient settings, allowingmore patients to have surgery and other treatmentswithout entering a hospital. As a result, patients admitted tohospitals tend to be more critically ill than ever before. <strong>The</strong>yalso are older and often dealing with chronic conditionssuch as cardiovascular disease and diabetes. Many of themneed more careful monitoring—not at the level given byan Intensive Care Unit, but more than the typical Medical/Surgical Unit provides.In line with this trend, <strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong> hasexperienced increasing demand for the beds in its currentTelemetry Unit, where patients’ electrical heart rhythms andother vital signs are continuously tracked and transmittedto a central monitoring station. <strong>The</strong>re, two trained technicianswatch the rhythms and report any unusual changes tothe patient’s nurse, who is also specially trained to interpretheart rhythms. Right away, these nurses can know what ishappening with their patients without being at the bedside.Such close monitoring, along with a 4-to-1 patient-nurseratio, ensures that these patients get any necessary interventionquickly for heart-related issues.“It used to be that just those with heart problems orrhythm problems required telemetry, but now we havemore patients who require this type of monitoring,” says JeffreyWahl, M.D., Medical Director of the Telemetry Unit anda cardiologist with Cardiology Consultants of Philadelphia–<strong>Chester</strong> <strong>County</strong> Cardiology Associates. “Patients are sickerand the demand has escalated.”“Cardiovascular conditions do remain our leading cause ofdeath and disability, and when patients have a known problem,we must watch their heart rhythms so we can managethe treatment,” says Tina Maher, RN, BSN, NE-BC, Director ofTelemetry, Post-Interventional Unit, and Critical Care Support.“If we can intervene early at the first sign of a problem,we can prevent a lot of complications, and get our patientshome and on their way to recovery.“<strong>The</strong>re are other patients who are acutely ill with otherconditions that could threaten cardiac stability, so theyneed to be monitored as well,” she says.Heather Iademarco, RN, BSN, MS, a nurse on the TelemetryUnit for six years, cites a range of conditions that she hasseen in her own patients, which makes the unit the safestplace for them to be.“<strong>The</strong>re are many conditions that can cause heart rhythms >6synapse
to go awry: Lyme disease, low magnesium or potassiumlevels, alcohol withdrawal and even the flu in some people,as we’ve seen with the early winter outbreak,” she says. “If apatient is starting a new blood pressure medicine or a betablocker, they may need to be monitored. In this and manyother situations, it’s best practice to have them on telemetrybecause the system is watching them even when I’m not atthe bedside, and it can document what is going on with theheart 24/7. We can go back and look atwhat happened throughout the day orloved one who wishes to stay overnight.“Our care delivery model is based on the relationships wehave with our patients, their family and visitors,” says TinaMaher. “<strong>The</strong> design of the room really reflects that.”Maher and several staff members from the current TelemetryUnit played a key role in planning the new spaces to bestmeet the needs not only of patients and families, but also ofnurses, physicians, and other clinical staff. A couple of yearsago, the <strong>Hospital</strong> assembled a committeethat included telemetry nurses, nursingovernight, and share it with the physician.”With increasing demand assistants, a unit secretary, the chargenurse and clinical manager to work withfor monitored beds, theIn 2004, the <strong>Hospital</strong> also addedthe architectural firm Ballinger to designremote telemetry capability, whichenables us to equip patients on any unitwith a transmitter that sends their heartcurrent Telemetry Unitis always an active anddynamic department. Thisthe new unit.“We met with the architects frequentlyand went over every nuance of the newrhythms to the central monitoring stationnear the Telemetry Unit. This allowsterms of the overall flow and design? Howspace,” Maher says. “What makes sense inJuly to accommodate thetechnicians to keep a watchful eye on upto 38 additional lower-risk patients.This is why the Medical Staff and clinicalcommunity’s need,they will welcome 24 newprivate rooms as part ofcan we best accommodate the patientand caregiver? Throughout the planningprocess, we would pull in staff from differ-team are excited that an additionalent disciplines—information technology,the Tower Project.Telemetry Unit will be the first area toenvironmental services, and so on—toopen in the Patient Tower in just a fewmonths. <strong>The</strong> unit will feature 24 privaterooms with two nurses’ stations, along with “touchdown”areas between rooms for clinicians to collaborate. Each roomis large enough to accommodate family members and othervisitors, and it includes a sofa that converts to a bed for aget their input on what would work best.”Nichole Coleman, RN, BSN, PCCN, theday shift charge nurse on the Telemetry Unit, participated onthe committee and appreciated what she calls the ongoing“back and forth” between the group and Ballinger. Especiallyhelpful was a mockup room that Ballinger set up across thecontinued...<strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong> and Health System 7
Stable Rhythms... continuedstreet from the main <strong>Hospital</strong>, where Coleman and hercolleagues could go to try out different configurationsand other ideas. Coleman was also part of a core groupthat traveled to Hill-Rom’s headquarters in Indiana tolook at beds and other medical equipment.“Working with Ballinger was a great experience,”Coleman says. “We know the clinical side of things—thisis what we do every day—and they have the architecturaland design expertise. This was a chance to take what weknow and create a space that would foster a betterexperience for the patients and make our workflow easier.We got the best possible outcome, and I know patientsare going to love and also benefit from the private rooms.”New Nurses Station renderingMonitor surveillance Technician Mary Alfano-Brown (pictured above)and JoAnne Higgins (pictured on page 1) have been with the <strong>Hospital</strong>since the inception of the Heart Monitoring Program. monitor techsare responsible for watching the heart rhythms of the patientsfrom Telemetry, the Post-Interventional Unit (PINU) and variousbeds throughout the <strong>Hospital</strong>.Our Generous Community<strong>The</strong> vision for the Tower Project was made a realityin part by the support of many donors. Recently,<strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong> Foundation received agenerous pledge of $5 million from Oscar and VivianLasko to fit out the two remaining floors of the <strong>Hospital</strong>’snew Patient Tower. <strong>The</strong>ir gift will also supportthe renovation of the Emergency Department (see p.16). With their extraordinary support, our <strong>Hospital</strong> willbe transformed into an even more patient-centeredfacility, which will further improve patient care andthe overall experience at the <strong>Hospital</strong>.Dr. Wahl points out that the entire Telemetry Unitalso has been designed for the future, which relies heavilyon information technology.“It is very busy in a Telemetry Unit and everyoneneeds access to a computer,” he says. “Everything isdone electronically: ordering, review, making notes,preparing the discharge plan. Traditional unitsweren’t built with workspaces large enough for thisway of doing medicine, but this new Telemetry Unitis. Clinicians will be able to function much moreefficiently.” In addition, each room features a bedsidecomputer for clinicians’ use.<strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong> is now immersed inthe process of orchestrating how the two TelemetryUnits will work together in terms of staffingand coordination of care. By the time the new unitopens on the fourth floor of the Patient Tower thissummer, all of these details will be in place. Moreimportantly, the <strong>Hospital</strong> will be able to betteraccommodate area residents who come throughour Emergency Department and need continuouscardiac monitoring as part of their care. This newunit will give the clinical team the ability to stabilizethem in the Emergency Department and then getthem into a bed quickly, starting them on the pathto healing.By Kristine M. ConnerPhotos by Rick Davislearn More atwww.chestercountyhospital.org/synapse8synapse
vital signsPutting the spotlight on some of the extraordinarywork being done by our Medical Staff.Case ManagementPhysician AdvisorInternal Medicine <strong>Hospital</strong>ist Dr.Stephanie Ciccarelli, a member ofthe Medical Staff since July 2007,has been named Physician Advisorfor Case Management and ClinicalDocumentation Improvement at<strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong>. For much of her time with the<strong>Hospital</strong>, she has also been a member of the Medical Staff CaseManagement Committee, providing valuable contributions ina number of critical areas, especially coding and documentationand observation-admission criteria. Dr. Ciccarelli’s primaryrole as Physician Advisor will be to serve as a consultant to allmembers of the <strong>Hospital</strong>’s multidisciplinary team in regard toappropriate utilization of hospital acute care resources, clinicaldocumentation and interactions with Medical Directors atthird-party payor organizations.Vice Chair RepresentsAllergists NationwideAsthma, Allergy and Clinical Immunology of <strong>Chester</strong> <strong>County</strong>is pleased to announce that Dr. Andrew Murphy has beenelected Vice Chair of the Federation of Regional, State andLocal Allergy, Asthma and Immunology Societies (RSLAAIS)representing allergists in the United States. <strong>The</strong> RSLAAIS consistsof nearly 70 regional, state and local societies that advocatefor allergists/immunologists at a grassroots level in providingoptimal delivery of quality patient care. “I am very humbledto be elected by my peers to represent them and our allergypatients,” says Dr. Murphy. “<strong>The</strong> practice of medicine is rapidlychanging, and I look forward to the challenges this positionwill entail.”Educator forPhysician PeersDr. Robert P. Liss was theSenior Instructor for the AmericanAcademy of Ophthalmology(AAO) lab course entitledAdvanced Refractive CataractSurgery and Anterior Segment Reconstruction. Thiscourse was offered to ophthalmologists from aroundthe world at the AAO’s annual meeting held November2012 in Chicago. Dr. Liss also served as instructor ofthree other 2012 AAO courses. <strong>The</strong> meeting was thefourth Joint Meeting with the Asia-Pacific Academyof Ophthalmology. As an educator to his peers, Dr. Lissis a leader in the advancement for cataract andglaucoma treatments.Medical Oncologist winsAward of HopeDr. Maureen Hewitt, HematologyOncology, received theNorma E. Ciccarone Award ofHope from Cuddle My Kids.Dr. Hewitt was honored due toher significant and enduringcontributions to the cancercommunity, including thetime she spends educating Cuddle My Kids volunteersduring their orientation. Cuddle My Kids provides inhomesupport, wellness support, a community supportgroup, educational resources, and a drop-off programfor children of cancer patients in our community.Published Authorof Research StudyDr. Sunil Saroha, HematologyOncology, was cited as oneof the authors of a researchstudy titled “Lymphopeniais an Independent Predictorof Inferior Outcome in ClearCell Renal Carcinoma.” <strong>The</strong> study was published in theJournal of Urology in February <strong>2013</strong>.<strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong> and Health System 9
ACTIVE STAFFGuy Bernstein, MDDepartment of Surgery, Section ofUrology. Dr. Bernstein graduated fromColumbia University College of Physiciansand Surgeons in New York, completed aninternship at Cornell University MedicalCollege in New York and a residency atBrigham & Women’s <strong>Hospital</strong> in Massachusetts.Dr. Bernstein is Board Certifiedin Urology and is in practice with UrologyHealth Specialists, LLC.• our new physicians•JamesHays, MDDepartment ofMedicine, Sectionof Endocrinology.Dr. Hays graduated from theUniversity of Kansas School of Medicine,completed an internship and residencyat the University of Kansas Medical Centerand a fellowship at the National NavalMedical Center in Bethesda, Maryland.Deanna Brasile, DODepartment of OB/GYN,Section of ReproductiveEndocrinology. Dr. Brasilegraduated from PhiladelphiaCollege of OsteopathicMedicine, completed aninternship at PhiladelphiaCollege of OsteopathicMedicine and a residency at Cooper UniversityMedical Center. Dr. Brasile is BoardCertified in OB/GYN and has joined MainLine Fertility.Benjamin Denenberg, DPMDepartment of Surgery, Section ofPodiatry. Dr. Denenberg graduated from<strong>The</strong> Ohio College of Podiatric Medicine,completed a residency at Chestnut Hill<strong>Hospital</strong> and has joinedFoot and Ankle Associates.AneeshaDhargalkar, MDDepartment ofEmergency Medicine.Dr. Dhargalkargraduated fromJefferson MedicalCollege and completeda residencyat Temple University<strong>Hospital</strong>. Dr. Dhargalkaris Board Certifiedin EmergencyMedicine and hasjoined EmergencyCare Specialists.Lorraine Dugoff, MDSophia Francis-Stewart, MDDepartment of Medicine,Section of Telepsychiatry. Dr.Francis-Stewart graduated fromUMDNJ – Robert Wood JohnsonMedical School, and completeda residency and fellowshipat Zucker Hillside <strong>Hospital</strong> inNew York. Dr. Francis-Stewartis Board Certified in Psychiatryand is in practice with Centerfor Family Guidance, PC.Joseph Graversen, MDDepartment of Surgery, Sectionof Urology. Dr. Graversengraduated from Louisiana StateUniversity School of Medicine,completed an internship at OchsnerClinic Foundation in Louisiana,a residency at LouisianaState University and a fellowshipat Columbia University College ofPhysicians and Surgeons and theUniversity of California. Dr. Graversenis in practice with UrologyHealth Specialists, LLC.Department of OB/GYN, Section ofMaternal Fetal Medicine. Dr. Dugoffgraduated from Georgetown UniversitySchool of Medicine, and completedher post graduate and fellowship trainingin OB/GYN, Clinical Genetics andMaternal Fetal Medicine at Pennsylvania<strong>Hospital</strong> and the University of Colorado Schoolof Medicine. Dr. Dugoff is Board Certified in all threedisciplines and has joined the Maternal FetalMedicine Services of the University of Pennsylvania.Richard Highbloom, MDDepartment of Surgery, Section of CardiacSurgery. Dr. Highbloom graduated fromTemple University School of Medicine, completedan internship and residency at AlbertEinstein Medical Center and a residencyat <strong>The</strong> <strong>Hospital</strong> of the Good Samaritan inCalifornia. Dr. Highbloom is Board Certified inThoracic and Cardiac Surgery.Ke Hong, MDDepartment ofMedicine, Section ofInternal Medicine.Dr. Hong graduatedfrom Shanghai Medical University in China,completed an internship and residency at<strong>The</strong> First Affiliate <strong>Hospital</strong> of Anhui MedicalUniversity in China and Montgomery <strong>Hospital</strong>.Dr. Hong is Board Certified in FamilyMedicine and has joined Medical InpatientCare Associates (MICA).Jeffrey Hurley, MDDepartment ofMedicine, Sectionof Dermatology.Dr. Hurley graduatedfrom BostonUniversity School ofMedicine, completedan internshipat Framingham Union <strong>Hospital</strong> inMassachusetts, a residency at HenryFord Memorial <strong>Hospital</strong> in Michiganand a fellowship at Scripps Clinic andResearch Foundation/Naval <strong>Hospital</strong>in California. Dr. Hurley is Board Certifiedin Dermatology and has an officein West <strong>Chester</strong>.10synapse
ZainalHussain, MDDepartment ofMedicine, Sectionof Cardiology. Dr.Hussain graduated from GandhiMedical College in India, completedan internship at the University ofIllinois at Urbana, and a residencyand fellowship at St. Louis University<strong>Hospital</strong>. Dr. Hussain is Board Certifiedin Cardiology and has joined West<strong>Chester</strong> Cardiology.Thomas Lanchoney, MDIlya Nasrallah, MDDepartment of Radiology.Dr. Nasrallah graduatedfrom the Universityof Pennsylvania School ofMedicine, and completedan internship, residency andfellowship at the <strong>Hospital</strong> ofthe University of Pennsylvania.Dr. Nasrallah is BoardCertified in Radiology andis part of the Penn Radiologyservice at <strong>The</strong> <strong>Chester</strong><strong>County</strong> <strong>Hospital</strong>.New Teleradiology Physicians<strong>The</strong> following physicians are Board Certified in Radiologyand are part of the Penn Radiology service at <strong>The</strong> <strong>Chester</strong><strong>County</strong> <strong>Hospital</strong>.Jacob Abraham, MD graduated from Wayne StateUniversity School of Medicine in Michigan, completedan internship at St. John <strong>Hospital</strong> and Medical Center inMichigan, a residency at the Medical University of SouthCarolina Medical Center and a fellowship at Henry Ford<strong>Hospital</strong> in Michigan.Jose Arjona, MD graduated from UniversidadCentral del Caribe School of Medicine in Puerto Rico,completed an internship at Miami Children’s <strong>Hospital</strong>and a residency at Brook Army Medical Center in Texas.Department of Surgery, Section of Urology. Dr. Lanchoney graduated fromthe University of Pennsylvania School of Medicine, and completed an internshipand residency at the <strong>Hospital</strong> of the University of Pennsylvania. Dr. Lanchoney isBoard Certified in Urology and is in practice with Urology Health Specialists, LLC.Francis Ferraro, MD graduated from New YorkUniversity School of Medicine, and completed a residencyat Cedars-Sinai Medical Center in California and afellowship at Brigham and Women’s <strong>Hospital</strong> in Massachusetts.David Mankoff, MDDepartment of Radiology.Dr. Mankoff graduatedfrom the Universityof Pennsylvania School ofMedicine, and completeda residency at the Universityof Washington Schoolof Medicine. Dr. Mankoff isBoard Certified in Radiology/NuclearMedicine andis part of the Penn Radiologyservice at <strong>The</strong> <strong>Chester</strong><strong>County</strong> <strong>Hospital</strong>.Sheela Moorthy, MDDepartmentof Pediatrics,Section ofNeonatology.Dr. Moorthygraduatedfrom the UniversityIslamSumatra Utara in Indonesia,completed a residency atRichmond University MedicalCenter and a fellowship at theUniversity of Maryland MedicalSystem. Dr. Moorthy is BoardCertified in Pediatrics and ispart of CHOP Newborn Care at<strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong>.MaggieSolimeo, DPMDepartment ofSurgery, Section ofPodiatry. Dr. Solimeograduated fromTemple University School of PodiatricMedicine, and completed a residencyat Frankford <strong>Hospital</strong> in Philadelphiaand Good Samaritan <strong>Hospital</strong> in NewYork. Dr. Solimeo is in practice withBryn Mawr Foot & Ankle Center.Mark Tantorski, DODepartment of Surgery, Sectionof Orthopedics. Dr. Tantorskigraduated from the University ofNew England College of Medicine,completed an internship andresidency at Philadelphia Collegeof Osteopathic Medicine and afellowship at NewEngland Baptist<strong>Hospital</strong>. Dr. Tantorskihas joined PremierOrthopaedics– <strong>Chester</strong> <strong>County</strong>Orthopaedics.To find a Doctor, call610.738.2300, or search online atwww.chestercountyhospital.org/synapsePejman Firouztale, MD graduated from KeckSchool of Medicine and University of Southern California,completed an internship at Loma Linda UniversityMedical Center in California, a residency at Saint LouisUniversity <strong>Hospital</strong> and a fellowship at the University ofSouthern California.Henry Jones, MD graduated from the Universityof Kentucky College of Medicine, and completed aresidency and fellowship at Indiana University MedicalCenter.Gautham Mallampati, MD graduated fromTemple University School of Medicine, completed aninternship at Abington Memorial <strong>Hospital</strong>, a residencyat Temple University <strong>Hospital</strong> and a fellowship at the<strong>Hospital</strong> of the University of Pennsylvania.Ashford McAllister, MD graduated from New YorkUniversity School of Medicine, completed an internshipat St. Vincent’s <strong>Hospital</strong> and Medical Center in York, aresidency at New York University Medical Center and afellowship at the <strong>Hospital</strong> of the University of Pennsylvania.Andrew McDonnell, MD graduated from AlbanyMedical College, completed an internship at Stony BrookUniversity Medical Center in New York, a residency at St.Vincent’s Medical Center of Richmond and a fellowshipat Albany Medical Center.Jana Sulzer, MD graduated from Vanderbilt UniversitySchool of Medicine in Tennessee, and completed aresidency at Yale University – New Haven in Connecticutand Case Western Reserve School of Medicine in Ohio.<strong>The</strong>se physicians hold Medical Staff privileges at <strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong> but they are not necessarily employees of <strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong> and Health System.<strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong> and Health System 11
TrueBeamBringingto the community...Leading-edgetechnology of the future<strong>The</strong> scene looks futuristic, like something bornin the imagination of a science-fiction writer. A cancerpatient lies still on a radiation treatment couch, as whatlooks like space-age machinery starts circling aroundthem to deliver precise radiation treatment with a remarkablelevel of control and synchronization. <strong>The</strong> couch alsomoves to reposition the patient as needed. Called True-Beam, this advanced cancer treatment technology representsa quantum leap forward in the speed, accuracy andsafety of radiation therapy.<strong>The</strong> TrueBeam system makes it possible to aggressively,accurately and safely attack tumors in the lung, breast,prostate, reproductive organs, head, neck, brain and elsewherewith greater precision and in far less time than earliergenerations of radiation delivery systems. Previous and manycurrent models rely much more on human intervention andmanual control, whereas the TrueBeam has built-in capabilitiesthat enable it to automatically and specifically targetand destroy tumors with maximum doses of radiation whileprotecting surrounding healthy tissue.<strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong> and Health System recentlypurchased a new TrueBeam linear accelerator for its RadiationOncology program, bringing the highest level of cancercare to the community. <strong>The</strong> TrueBeam can deliver variousforms of radiation therapy; including image-guided radiotherapy(IGRT), intensity-modulated radiotherapy (IMRT) and<strong>Vol</strong>umetric Modulated-beam <strong>The</strong>rapy (VMAT) like RapidArc®radiotherapy. <strong>The</strong> TrueBeam at <strong>Chester</strong> <strong>County</strong> will additionallyfeature a fast Gated RapidArc® – allowing it to deliver sophisticatedand complex treatments accounting for patientrespiratory movements.According to Medical Physicist Andre Kalend, PhD, theTrueBeam far surpasses its predecessors with its onboarddigital ability to synchronize all the different componentsinvolved in radiation therapy – including imaging,treatment delivery as well aspatient positioning, and breathing and motion detection.“TrueBeam is much more than cutting-edge technology;it is the leading edge of radiation therapy. It goes beyondwhat is considered state-of-the-art today. Having theTrueBeam means we have secured the state-of-the-artradiotherapy technology of the future,” said Dr. Kalend.“Radiation Oncology is complex technology-driven medicine.With this purchase, <strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong> ispoised to stay ahead of the innovation curve of radiationoncology in the region.”Indeed, the level of precision with which the TrueBeamdelivers radiation treatment is unprecedented. <strong>The</strong> systemis able to target cancers with sub-millimeter exactness as itcontinually monitors more than 100,000 points of patientlive images and data. Another key to the system’s pinpointaccuracy is that it includes sophisticated user-friendly imagingtools that physicians and therapists can use to generatevarious anatomical views 60% faster than previous accelerators.<strong>The</strong>se advances also reduce overall imaging radiationexposure by 25% and offer greater patient comfort by shorteningtheir treatment duration on the delivery couch. Typicalirradiation duration that took 10 to 15 minutes takes a mere1 to 2 minutes on TrueBeam.According to Radiation Oncologist Ann Marie Siegal, MD,the increased precision of the TrueBeam has significantlyfine-tuned an often-challenging treatment delivery process.Many tumors are located in places that are affected by the12synapse
ody’s slightest movement. With the TrueBeam, radiationfields can be tailored tightly, directly targeting the canceror area at risk.“When we are treating some of the more challengingcancers – where tumors are in areas exposed to lots oforgans and healthy tissues – we have to be very careful.Movement is inherent to the human body and can’t beavoided, so precision is absolutely paramount when targetinga tumor. <strong>The</strong> slightest shift in the patient’s positionor movement in the body, even the lungs as they expandduring breathing, can throw off radiation targeting,” explainsDr. Siegal, who is also a Clinical Assistant Professor at theUniversity of Pennsylvania Health System.She adds, “<strong>The</strong> TrueBeam can detect the smallestmovements during a treatment session. It has the ability toautomatically adjust where the delivery beam is directed;allowing radiation to hit its intended target, protectinghealthy organs and tissues.”As the patient breathes and the lungs inflate and deflate,tumors are pushed in different directions, becoming bothmoving and shape-changing targets. TrueBeam containsa respiratory-motion management feature that is specificallydesigned to track movement of tumors as the patientbreathes. <strong>The</strong> system ensures that radiation is only deliveredwhen the tumor is within the beam’s line of sight. It evenrecognizes unplanned disruptions in the patient’s breathingcycle, such as coughing or sneezing.<strong>The</strong> added safety of the TrueBeam does not end withprecision when targeting the tumor. <strong>The</strong> TrueBeam also hasan internal collision protection and avoidance componentthat protects the entire patient while the linear accelerator’sgantry (the head of the machine) moves around their body,which means safeguarding patient positioning does notsolely rest on the professionals operating the equipment.<strong>The</strong> system itself continually monitors where the patientis located throughout treatment, using special sensors tocontinued...Radiation Oncology Team Back row, from left: Robert E. Krisch, MD, PhD, Radiation Oncologist;Kathleen Devlin, RT(T), Radiation <strong>The</strong>rapist; Eileen McDevitt, RT(T), CMD, Dosimetrist; Amy Ferris, RT(R)(T), Supervisor; RamahWilliams, RT(R), Student therapist; Andre Kalend, PhD, Physicist. Front, from left: Ann Marie Siegal, MD, Radiation Oncologist;Monica Sekela, RN, BSN; Lynne Davis, RT(R)(T), Radiation <strong>The</strong>rapist; Susan Nichols, Unit Secretary; and Marcella Kubovsak, RN.<strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong> and Health System 13
TrueBeam... continueddetect where the patient couch is in proximity to themachinery circling around the patient.“As treatments become more complex, it is essentialthat we have accelerator systems in place that monitorpatient safety,” said Dr. Kalend. “TrueBeam has its ownGPS-like capabilities that check itself to make sure thegantry never encroaches into the patient’s space. If there isever an issue, the machine will immediately stop, move thepatient out of the gantry path and then bring the patientback again to the treatment position. Prior to the True-Beam, machines were ‘blind’ to the location of the patientand the couch when the beam was on. Only the operatorwas aware of the patient’s location.”<strong>The</strong> advances in the TrueBeam system have significantlyshortened the duration a patient has to spend onthe couch undergoing treatment, even for those requiringhigh doses of radiation. <strong>The</strong> length of time neededfor radiation sessions is always determined by the type ofcancer a patient has, what dose of radiation is needed, andthe individualized treatment plan. However, in many cases,delivery time will now be reduced by 50% or more withthe TrueBeam. For example, treatments for patients withprostate cancer or some of the more difficult head andneck cancers that may take up to a half hour or longer withconventional linear accelerators can now be delivered injust 2 to 7 minutes with the TrueBeam.“Faster treatments make the whole experience mucheasier for our patients,” said Dr. Siegal. “And the TrueBeamhas a two-way communication system so therapists are inconstant contact with patients and vice versa. That is veryreassuring to patients.”<strong>The</strong> purchase of the TrueBeam linear accelerator is asignificant milestone for <strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong>,expanding the services provided by its Radiation OncologyDepartment and opening the door to new possibilities fortreating cancers that are more complicated closer to home.A new vault for the TrueBeam was incorporated into plansfor the <strong>Hospital</strong>’s Tower Project, a $45.2 million expansionslated to open this summer. <strong>The</strong> <strong>Hospital</strong> will begin schedulingpatients on the TrueBeam this coming July.<strong>The</strong> Radiation Oncology Department is a key componentof the <strong>Hospital</strong>’s comprehensive Cancer Program,which has been part of the Penn Cancer Network since1995. Because of the <strong>Hospital</strong>’s existing and growing connectionto Penn Medicine, radiation oncology and medicaloncology patients seeking treatment in <strong>Chester</strong> <strong>County</strong>will benefit from direct and immediate access to theresources of the university health system – including thelatest oncology clinical trials.As <strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong> moves forward with itsnew TrueBeam system, its team of experts will not only betraining with Varian – the vendor that manufactures theTrueBeam – but will also draw from the clinical expertisefrom Penn Medicine staff that have hands-on experiencewith the equipment. Patients can feel confident they arebeing treated by experts from one of the top academicinstitutions in the country, while being cared for close tohome at <strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong>.Bringing the TrueBeam to <strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong>will dramatically expand its clinical treatment capabilities,and it demonstrates the Health System’s firm commitmentto expanding services and adding the future of technologyto treat a broader spectrum of cancer patients with themost sophisticated program between Philadelphiaand Lancaster.By Beth EburnTeam Photo by Rick Davislearn More atwww.chestercountyhospital.org/synapse14synapse
points of prideHigh Marks forPatient SafetyIn February, <strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong>was honored with an “A” <strong>Hospital</strong> SafetyScore by <strong>The</strong> Leapfrog Group, an independentnational nonprofit run by employersand other large purchasers of health benefits.<strong>The</strong> score was awarded in the latestupdate to the <strong>Hospital</strong> Safety Score SM ,the A, B, C, D, or F scores assigned to U.S.hospitals based on preventable medicalerrors, injuries, accidents and infections.“<strong>Hospital</strong>s like this that earn an ‘A’ havedemonstrated their commitment to theirpatients and their community,” said LeahBinder, president and CEO of <strong>The</strong> LeapfrogGroup. “I congratulate <strong>The</strong> <strong>Chester</strong> <strong>County</strong><strong>Hospital</strong> for its safety excellence, and lookforward to the day when all hospitals willmatch this standard.”Four-Year Winning StreakFor the fourth consecutive year, PressGaney Associates has bestowed its SummitAward to Professional Providers, Inc., aphysician practice management subsidiaryof <strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong> and HealthSystem. <strong>The</strong> Press Ganey Summit Award isthe health care satisfaction industry’s mostcoveted symbol of achievement bestowedannually. Professional Providers is just oneof only 13 to receive it for achieving andsustaining excellence in patient satisfactionfor 2012. “To attain this award for thefourth year means the medical practiceshave received a 95% or higher patient satisfactionrating for more than seven years,”explains Michael J. Duncan, President andCEO of the Health System. “<strong>The</strong>se positivepatient experiences and accolades area direct result of the hard work andprofessionalism of our health care team.”Top 10 % in the Country<strong>The</strong> Cardiac Surgery program at <strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong>has been ranked in the top 10% in the nation by <strong>The</strong> Society ofThoracic Surgeons National Adult Cardiac Surgery Database.<strong>The</strong> program has also received a “three star” rating for cardiacsurgery by the Society of Thoracic Surgeons (STS). According toCardiac Surgeon Brian Priest, MD, the “three star” rating denotesthe highest category of quality placing the <strong>Hospital</strong> in the top10-15% in the country. He adds, “In the current analysis of nationaldata covering the period from July 1, 2011 through June30, 2012, our cardiac surgery performance was found to lie in thehighest quality tier, thereby receiving an STS three-star rating.”ACE Accreditation for Cardiac Catheterizationand Percutaneous Coronary Intervention<strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong> has been accredited for cardiac catheterizationand percutaneous coronary intervention by Accreditationfor Cardiovascular Excellence (ACE), an organization dedicated to ensuringadherence to the highest quality standards for cardiovascularand endovascular care. <strong>The</strong> <strong>Hospital</strong> is one of 11 hospitals nationallyand the only hospital in Southeastern Pennsylvania to receive thisaccreditation. “For more than 20 years, we have strived to be the bestby continually improving the quality and safety of the care we deliverto our community,” notes Timothy Boyek, MD, Director, InterventionalCardiology. “We do this by utilizing national standards and analyzingpatient outcome data to drive a process of ongoing improvement.”Interventional cardiology Team<strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong> and Health System 15
charitable givingEmergency DepartmentReconfigurationAimingHighWhen the new 24-bed Telemetry floor of the Tower opens thisJuly, the added room capacity will have a direct impact onpatients seeking care at the <strong>Hospital</strong>’s dynamic Emergency Department,which is often the front door for many people whoare ultimately admitted to Telemetry for heart monitoring.<strong>The</strong> expansion of the Telemetry unit will be quicklyfollowed by and complemented by enhancements tothe Emergency Department (ED), which was madepossible by several generous donors to <strong>The</strong> <strong>Chester</strong><strong>County</strong> <strong>Hospital</strong> Foundation.<strong>The</strong> <strong>Hospital</strong> invited consultants from Penn StateHershey Medical Center to examine all aspects of the ED.<strong>The</strong> <strong>Hospital</strong> is now implementing an innovative model ofcare that combines the highest level of emergency treatmentwith unmatched efficiencies and customer service.At the core of the recommendations is a process calledPhysician Directed Queuing (PDQ).Walk-in patients will see an ED physician or physician assistantfor initial assessment in a Rapid Treatment Area upontheir arrival.Betty Brennan, RN, EdD, CNML, Director of EmergencyDepartment says, “<strong>The</strong> consultants predict PDQ will reducethe total wait times by 77% and the average patientstay in the ED by 53%. This would allow us to treat roughly9,000 more patients each year. We currently see more than40,000 people every year.”To facilitate the transition to this model, the <strong>Hospital</strong>,with philanthropic support from a number of generousdonors, is investing more than $5 million to reconfigureand enhance the ED.With PDQ, one of the essential elements to improvepatient flow and reduce length of stay is the diagnostic testingand results process. A local family foundation, with annterest in funding specific pieces of equipment, hasgenerously provided philanthropic support to purchasemore than $565,000 worth of technology that will speedspecimen collection, expedite lab results, and enhancesafety and quality.Another private family foundation made an extraordinarilygenerous donation of $2.5 million to fund theED renovation. This will enhance the patient experiencefrom the front door to an ED patient bed, and then ontoadmission or discharge. This transformation will occurover the next year.Finally, the <strong>Hospital</strong> administration has always beenparticularly grateful for the long-standing dedication ofthe Women’s Auxiliary, which pledged $500,000 towardthis ED project. Through its numerous annual fundraisingefforts, the 500-women-strong group demonstrates yearafter year that goals can be attained when you are fueledby a vision to help others.<strong>The</strong> result of the overwhelming generosity by thesedonors as well as Oscar and Vivian Lasko (see page 8), the EDenhancements to our facilities will ensure that <strong>The</strong> <strong>Chester</strong><strong>County</strong> <strong>Hospital</strong> continues to provide the highest quality ofcare in a patient-centered environment to all members ofthe community who walk through its doors for care.Here are some of the new enhancementscoming to the Emergency Department.> Sunquest Collection Manager System> GE MAC 5500 EKG Machine with MUSEWireless Capabilities> Digital Census Equipment> Computerized Physician Order Entry devices> Swipe Card AccessTo learn how youcan support the Foundationcall 610.431.5108 or visitwww.chestercountyhospital.org/synapse16synapse
Consulting a physician regularly is an important part of a healthy lifestyle. A primary carephysician or specialist knows your medical history and can provide special insight into anytreatment plan you may need. Together, you and your physician can determine the bestplan to manage your health care needs and achieve your full wellness potential.<strong>The</strong> following are <strong>The</strong> <strong>Chester</strong> <strong>County</strong> <strong>Hospital</strong>and Health System’s affiliated practices:CANCER<strong>Chester</strong> <strong>County</strong>Hematology OncologyTreating each patient as ifthey are a member of ourown families. Locations inWest <strong>Chester</strong>, Exton andKennett Square> CCHemOnc.comWomen’s Specialty CenterDelivering seamlessly integratedspecialty servicesin one convenient location.Based in West <strong>Chester</strong>> <strong>The</strong>WomensSpecialtyCenter.comPRIMARY CAREKennett CareMedical AssociatesProviding patients with comprehensiveand compassionatehealth care services.Based in Kennett Square> KennettCare.comKennett Primary CareProviding the higheststandards of medicalexcellence in a practicespecifically designed forits community. Basedin Kennett Square> KennettPrimaryCare.comLincoln MedicineAssociatesEstablishing trust bytaking the time to listenand understand the needsof each individual. Basedin West <strong>Chester</strong>> LincolnInternalMed.comSouthern <strong>Chester</strong> <strong>County</strong>Family PracticeOffering the best, evidencebasedhealth care anddisease management to ourpatients. Based in West Grove> SCCFamilyPractice.comUnionville Family MedicalCultivating an environmentof respect for our patients,our staff and our providers.Based in Unionville> UnionvilleFamilyMed.comWhiteland MedicalAssociatesCreating compassionate andinnovative service with thehighest level of patient empowerment.Based in Exton> WhitelandMedical.comOBSTETRICSAND GYNECOLOGYAssociates forWomen’s MedicineHelping women stay vibrantand strong during everyphase and milestone of theirlives. Offices in Exton, West-<strong>Chester</strong> and West Grove> AFWMedicine.comFind these or any of ourdoctors online at <strong>Chester</strong>-<strong>County</strong><strong>Hospital</strong>.org or callour Physician Referral Lineat 610.738.2300.expert carein your neighborhood
1892<strong>The</strong> <strong>Chester</strong> <strong>County</strong><strong>Hospital</strong> and Health SystemNON PROFIT ORGU.S. POSTAGEPAIDwest chester, PAPermit #9701 East Marshall StreetWest <strong>Chester</strong>, PA 19380www.chestercountyhospital.org/synapseADD FSC LOGO HEREFollow us...Call 610.738.2793 to update your mailing information.