VERTEBRIS Lumbar-Thoracic - Richard Wolf
VERTEBRIS Lumbar-Thoracic - Richard Wolf
VERTEBRIS Lumbar-Thoracic - Richard Wolf
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
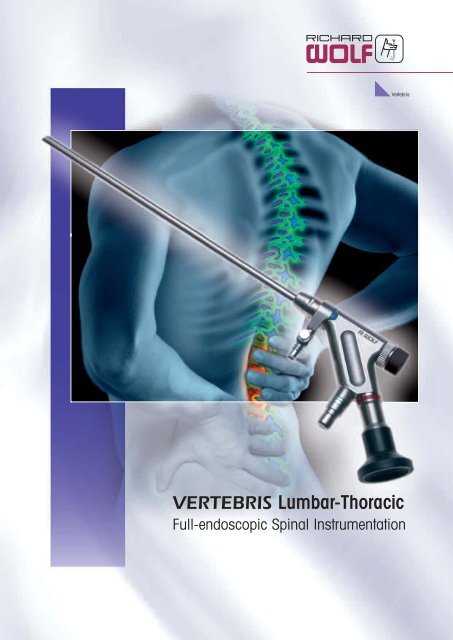
Vertebris<strong>VERTEBRIS</strong> <strong>Lumbar</strong>-<strong>Thoracic</strong>Full-endoscopic Spinal Instrumentation
<strong>VERTEBRIS</strong> lumbar-thoracic,full-endoscopic techniquesTable of contentsVertebris<strong>VERTEBRIS</strong> lumbar 4Introduction 4The full-endoscopic trans- and extraforaminal technique 6• Positioning of patient 8• Determination of lateral access route 8• Creation of lateral access 9• Performance of operation 12• Creation of posterolateral access 13• Creation of extraforaminal access 14• Bone resection 15• Biportal access 16The full-endoscopic interlaminar technique 17• Positioning of patient 19• Determination of access route 19• Creation of access 20• Performance of operation 21• Bone resection 24<strong>VERTEBRIS</strong> thoracic 25Introduction 25The full-endoscopic transforaminal technique 26The full-endoscopic interlaminar technique 27<strong>VERTEBRIS</strong> basic sets• <strong>VERTEBRIS</strong> lumbar trans-/extraforaminal basic set 28• <strong>VERTEBRIS</strong> lumbar and thoracic interlaminar basic set 29• <strong>VERTEBRIS</strong> thoracic transforaminal basic set 30• <strong>VERTEBRIS</strong> instruments 31-39Literature 40Notes 41-423
<strong>VERTEBRIS</strong> lumbarIntroductionLateral approach for the full-endoscopic transforaminaloperationMusculoskeletal pain is one of themost common reasons for visiting thedoctor. Degenerative diseases of thespine form part of daily medical practiceand their treatment is complicatedby medical and socioeconomic problems.Where severe pain or neurologic deficitspersist and all conservative treatmentoptions have been exhausted,surgery may be required. Though conventionaloperations can achieve goodresults, damage may ensue due totraumatization. It is therefore importantthat the surgical techniques usedbe optimized on a continuous basis.The latest research results and technicalinnovations must be critically reviewedso that optimal treatment strategiescan be formulated. The aimshould be to minimize surgically inducedtrauma and negative long-termsequelae, taking existing quality standardsinto account.Minimally invasive techniques can reducetissue damage and its consequences.Endoscopic operations withcontinuous irrigation have advantagesthat have made them the gold standardin a number of areas. Transforaminalprocedures with posterolateralaccess have been performed inthe lumbar spine for more than 20years now, mostly for intradiscal andintra and extraforaminal procedures.In our Department of Spine Surgeryand Pain Therapy we have thereforebeen developing a lateral transforaminaland an interlaminar approach forfull-endoscopic access to the spinalcanal since 1998. These approachesbroaden the range of indications andpermit the use in selected indicationsof a visually controlled procedure thatis as effective as conventional surgerywhile benefiting from all the advantagesof truly minimally invasive surgery.Until fairly recently, the endoscopicapproach was subject to technicalproblems in that the intraendoscopicworking channel of the available opticalsystems was small and the repertoireof instruments that could be usedwas correspondingly limited. Insurmountabledifficulties could arise inthe resection of hard tissue and interms of limited anatomic access andmobility. Work on the affected tissuewas limited and sometimes had to beperformed without direct visualization.New rod lenses with a 4.1 mm intraendoscopicworking channel and correspondingnew instruments, as wellas shavers and burrs, were thereforedeveloped so that full-endoscopicoperations could be performed undercontinuous and precise visual control.This also permitted adequate boneresection. The range of indications forendoscopic spinal surgery was thusbroadened to include intervertebraldisc herniations, spinal canal stenosis,and stabilization techniques.Continuous irrigation provides outstandingintraoperative visualizationThe latest generation of endoscopes have alarge (4.1 mm) working channel4
VertebrisFull-endoscopic surgery has now wona firm place in the surgery of lumbarspine conditions. Provided that the indicationsfor its use are observed, it representsa useful and safe addition oralternative to conventional surgery. Fullendoscopicoperations can also be performedon the cervical and thoracic spine.Recent technical developments andthe use of new access routes have ledling the end of existing operative standards;rather, it should be seen as avaluable additional option within thefield of spinal surgery.Herne, July 2007Dr. Sebastian Ruetten, M.D.Head Department of Spine Surgery andPain TherapyThe development of new instruments broadensthe range of possible proceduresto a change that suggests the onset ofa revolution in spinal surgery similar tothat which occurred in orthopedics withthe introduction of arthroscopic procedures.Nevertheless, conventional andmaximally invasive operations will continueto play an indispensable role inspinal surgery. Surgeons will need to beable to perform these techniques too inorder to overcome problems and complicationsof full-endoscopic operationssuch as can occur with any invasiveprocedure.The development of full-endoscopictechniques should not be seen as spel-Department of Spine Surgery and Pain TherapyHead: Dr. Sebastian Ruetten, M.D.Center for Orthopaedics and TraumatologySt. Anna Hospital, Herne, GermanyDirector: Prof. Georgios Godolias, M.D.at the Department of Radiology and MicrotherapyUniversity of Witten/Herdecke5
<strong>VERTEBRIS</strong> lumbarThe full-endoscopic trans- and extraforaminal techniquePercutaneous operations aimed atachieving intradiscal decompression oflumbar intervertebral discs were firstdescribed in the early 1970s. Opticalsystems designed for inspecting theintervertebral space after open operationwere introduced in the early 1980s.Later, a full-endoscopic technique usinga transforaminal approach was developed.In anatomic terms, this means thatthe intervertebral disc is reached via aposterolateral approach through theintervertebral foramen between the exitingand traversing nerve roots withoutneed for resection of bony or ligamentousstructures. The skin entry point foroperative access is determined in centimetersfrom the midline. Most suchoperations are performed for the purposeof intradiscal or extradiscal foraminaltherapy. Reduction of intradiscalvolume and pressure can reduce discrelatedcompression. Removal of intraand extraforaminal disc material istechnically possible. Sequestered materiallying within the spinal canal cangenerally be resected in retrogradefashion intradiscally via the annulardefect. This is done using an "in-out"technique.Sequestered nuclear material is foundwithin the spinal canal dorsal to the annulusin the ventral epidural space medialto the medial pedicular line. Inmany cases it extends to the midline oreven to the contralateral side. Clinicalexperience has shown that the annulardefect is often smaller than the diameterof the sequestered material. In addition,there is generally no longer any directconnection to the intradiscal space. Inthe case of badly degenerated discs orolder disc herniations, the continuity ofthe sequestered material has often beenlost and removal in one piece is generallynot possible. These factors oftenmake it difficult to resect sequesterednuclear material using an intradiscal retrogradeapproach. In order to achieveadequate decompression, it is thereforenecessary to access the extradiscalventral epidural space directly undercontinuous visual control.The most frequent site of lumbar intervertebraldisc herniations is in the lowersegments. The diameter of the intervertebralforamen decreases in a cranial tocaudal direction. Additional narrowingmay result from degenerative changes.Particularly at the lower lumbar levels,these anatomic factors often make itdifficult to gain extradiscal access to theventral epidural space under visualcontrol when using the posterolateralapproach. Similarly, lateral placementof the endoscope in order to reach thespinal canal tangentially after accesshas been created is technically difficultdue to the preceding passage throughsoft tissue and the zygapophyseal joint.These problems make it difficult toachieve adequate decompression on areliable basis when using the posterolateralapproach.The skin entry point for the well-known posterolateralapproach is measured in centimetersfrom the midlineFor these reasons a lateral transforaminalapproach has been developed inrecent years.*In this technique the skin entry point isdetermined not by measurement in centimeters,but on an individual anatomicbasis under radiographic control. Theapproach permits tangential access tothe spinal canal and consequently thedirect visualization of the ventral epiduralspace with continuous irrigation thatis required in order to achieve adequatedecompression. Used in combinationwith newly developed endoscopes witha large working channel and correspondingnew instruments, shavers,and burrs, this technique has a broadbut clearly defined range of indications.As a guideline for decompression of thespinal canal, caudal and cranial mobilityshould extend to the middle andstart of the pedicle, respectively. Narrowedforamina are no longer a limitation,since they can be broadened. Thepelvis can prevent the required lateralaccess, therefore in an orthograde lateralradiographic view it should notWith the posterolateral approach the workingarea is mostly intradiscal6
Vertebrisproject beyond the middle of the cranialpedicle. At the highest lumbar levels thelaterality of the approach is limited bythe thoracic and abdominal organs.Because of the greater size of the intervertebralforamen cranially and the possibilityof bone resection, a larger radiusof action is achieved here andconsequently a less lateral access routecan be chosen. In the case of intra andextraforaminal decompression operationsthere are no restrictions. Here, too,a lateral approach is attempted in orderto permit atraumatic passage below theexiting spinal root. The surgical accesstechnique for intra- or extraforaminaldisc herniations and foraminal stenosismay differ from the conventional techniquein order to avoid damaging exitingnerve roots that are dislocated or notdefinitely localizable. In such cases theextraforaminal approach is used.Intradiscal procedures such as thoserequired for fusion or infection often callfor the posterolateral approach. The approachis always determined by the targetpoint, account being taken of individualpathology and anatomy. Outsideof the established indications for itsuse, the transforaminal approach hasdefinite limitations.* Ruetten et al. (2005) An extreme lateral accessfor the surgery of lumbar disc herniationsinside the spinal canal using the full-endoscopicuniportal transforaminal approach.– Technique and prospective results of 463patients. Spine 30:2570–2578Ruetten et al. (2007) Use of newly developedinstruments and endoscopes: full-endoscopicresection of lumbar disc herniations via theinterlaminar and lateral transforaminal approach.J Neurosurg Spine 6:521-530The lateral transforaminal approach providesaccess to the spinal canal in the lower lumbarsegmentsIn the lower lumbar segments the pelviscan prevent the required lateral transforaminalaccessThe lateral transforaminal approach shiftsthe working area to the spinal canal7
<strong>VERTEBRIS</strong> lumbarThe full-endoscopic trans- and extraforaminal technique1. Positioning of the patientThe patient is positioned prone on aradiolucent table with a pelvic and athoracic roll. Use of a C-arm is requiredduring the operation.Prone position with pelvic and thoracic roll2. Determination of lateralaccess routeAccess is determined on the basis ofanatomic landmarks under orthogradelateral and posteroanterior fluoroscopicguidance, account being taken of thepathology. Depending on the level, thepossibility of injury to abdominal organsmust be excluded.Determination of maximum ventrality on the basis of individual anatomic landmarks and markingof the entry line on the skinDetermination of the intervertebral disc level under orthograde posteroanterior fluoroscopicguidance and determination of the skin entry point8
Vertebris3. Creation of lateralaccessAfter the skin entry point has beendetermined and the puncture incisionmade, a spinal cannula is introducedunder fluoroscopic guidance, care beingtaken not to damage neural structures.Positioning in relation to the spinalcanal is determined individually inaccordance with the target point. Theguidewire is then introduced and thespinal cannula removed.Introduced spinal cannulaThe spinal cannula touches the dorsal annulus at the medial pedicular line at the beginning of thespinal canalThe spinal cannula is advanced in the dorsal annulus towards the spinal canal9
<strong>VERTEBRIS</strong> lumbarThe full-endoscopic trans- and extraforaminal techniqueUsing rotatory movements, the dilatoris passed along the guidewire as far asthe foramen. After removal of theguidewire it is – depending on thepathology – inserted into the spinalcanal.A beveled working sleeve is then insertedover the dilator and the dilator isremoved. Care must be taken to protectneural structures during all workingsteps.The guidewire is positioned and the spinalcannula is removedThe dilator is inserted over the guidewireand is in the final position in the spinalcanal or dorsal annular defect10
VertebrisThe working sleeve is positioned via thedilator and the dilator is removed. Thebeveled opening is situated inside thespinal canal dorsal to the annulus11
<strong>VERTEBRIS</strong> lumbarThe full-endoscopic trans- and extraforaminal technique4. Performance of operationThe endoscope is passed through theworking sleeve. The operation is performedvia the intraendoscopic workingchannel using alternating sets of instrumentsunder full visual control and withcontinuous irrigation.The sealing caps for the optic undworking sleeve should be used only forbrief periods when bleeding obscuresvision, since with long operation timesand unnoticed obstruction to backflowof irrigation fluid there is a theoreticalrisk of volume overload and increasedpressure within the spinal canal and inthe associated and adjacent structures.Experience has shown that, as with allnew techniques, the risk of complicationsis greatest during the learningperiod.The lateral approach makes it possible to work in the spinal canal under full visual control12
Vertebris5. Creation of posterolateralaccessObstruction of lateral access by the pelvisor the risk of causing injury to abdominalor thoracic organs in the craniallumbar segments can necessitate amore posterior or even a posterolateralapproach in intradiscal operations. Theskin entry point depends on the individualpathology and anatomy and canbe either measured in centimeters fromthe midline or determined by appropriatepositioning of the introducedspinal cannula. The subsequent steps,including insertion of the guidewire, thedilator, the sheath, and finally the optic,are the same as in the procedure describedabove.Measurement of the skin entry point incentimeters from the midlineThe introduced spinal cannula at the desiredtarget point can determine the site of thepuncture incisionThe maximum laterality of access can bedetermined on the basis of a preoperativeCT scan so as to prevent injury to organsOperation with posterolateral transforaminalapproach13
<strong>VERTEBRIS</strong> lumbarThe full-endoscopic trans- and extraforaminal technique6. Creation of extraforaminalaccessIn intra- and extraforaminal intervertebraldisk herniations and in foraminalstenosis, the exiting nerve roots may beat increased risk of injury when the accessinstruments are passed throughthe foramen. This may necessitate anextraforaminal approach. The skin entrypoint can be posterolateral to lateral.Instead of being inserted through theforamen into the spinal canal, the spinalcannula is advanced onto the caudalpedicle of the segment to be operatedon. This is the safest area in termsof the exiting nerve roots and its use reducesthe risk of access-related injury.Subsequently the guidewire, the dilator,and the sheath are likewise advanceduntil they make bony contact with thepedicle. The anatomic structures of thecaudal foramen are then dissected underdirect vision, the exiting nerve rootis identified, and the operation is performedwithout damaging the nerve root.The caudal pedicle is a safe area in terms ofthe exiting spinal nerve rootInsertion of the spinal cannula as far as the caudal pedicleDissection of the anatomic structures of the caudal foramen and the exiting spinal nerve root14
Vertebris7. Bone resectionResection of bone may be required inorder to increase mobility within thespinal canal or when problems ariseduring access. This can occur, forexample, in cases of degenerative orhereditary foraminal stenosis and inrecess stenosis operations. The skinentry point can be posterolateral to lateral.After trans- or extraforaminal accesshas been obtained the bony structuresmust be dissected for this purpose. Inmost cases ventral parts of the ascendingfacet are resected. When parts of thecaudal pedicle are resected it must beremembered that this is a weightbearingstructure. Extensive resection can weakenthe biomechanical structure andresult in pedicle fractures.A range of burrs and bone punches areavailable for bone resectionSometimes damaging of the joint in order toreach the medial edge of the ascendingfacet can not be avoidedIn most cases ventral parts of the ascending facet are resected15
<strong>VERTEBRIS</strong> lumbarThe full-endoscopic trans- and extraforaminal technique8. Biportal accessA biportal approach can be required incertain indications such as spondylodiscitisand insertion of implants andwhen working with special instruments.Access is normally posterolateral usingthe standard technique. The endoscopecan be inserted either unilaterally or inalternating fashion.Biportal transforaminal access16
<strong>VERTEBRIS</strong> lumbarThe full-endoscopic interlaminar techniqueVertebrisFull-endoscopic interlaminar accessDirect access to the epidural space undercontinuous vision is a preconditionfor the performance of satisfactory operationswithin the spinal canal. When thefull-endoscopic transforaminal techniqueis used, the lateral approach is often requiredfor this purpose. The bony andneural boundaries of the neuroforamenimpose limits to mobility and thus alsoto the indications for operations of thistype. Moreover, in the lower lumbar segmentsthe required lateral access can beblocked by the pelvis. It has been foundthat these limitations make it technicallyimpossible to operate on some pathologiesusing the full-endoscopic transforaminalapproach.In order to reduce the incidence of surgicallyinduced traumatization of the structuresof the spinal canal, it is expedientto make use of anatomically preformedaccess routes. In addition to the intervertebralforamen, these include the sacralhiatus and the interlaminar window. Fortechnical reasons, epiduroscopy via thesacral hiatus does not permit resectionof large structures. This leaves open thepossibility of surgical access via theinterlaminar window, a long-establishedand commonly used technique in lumbarspine surgery that was first describedin the early 1920s. Various alternativemethods were developed in later years,e.g. posterolateral biopsy of the spine inthe late 1940s and intradiscal decompressionby means of chemonucleolysisin the early 1970s. Endoscopic inspectionof the intervertebral space after opendecompression was described in theearly 1980s. Full-endoscopic operationswere performed mostly using the transforaminaltechnique with posterolateral access.A microsurgical technique performedwith the aid of a microscope was developedin the late 1970s and went onUse of the endoscope based on the joystickprinciple provides mobilityto become the gold standard for interlaminardecompression of the spinal canal.An endoscopically guided technique,or microendoscopic operation, wasdescribed in the late 1990s. This usedan endoscope to provide visualization ofthe exposed surgical site on a monitor.With the conventional technique, thespinal canal has to be opened in orderto gain access to the epidural space.This generally involves not only incisionof the ligamentum flavum, but also resectionof bone. The basic requirementis to achieve adequate access that providesvisualization of the spinal canaland permits work with instruments.Problems can arise as a result of traumatizationof the access pathway, resectionof stabilizing structures, and –especially in relation to the possibleneed for revision operations – scarring.The basic role of the microscope is toreduce the size of the access route andprovide optimal conditions of light andvision. Resection of structures of thespinal canal is generally unavoidable.The microendoscopic technique providesaccess with less trauma than doesthe microscopic technique. Its advantagelies in the smaller distancebetween the working area and the visualizingsystem. Visual conditions andillumination are generally worse. It isnot a full-endoscopic technique in thestrict sense. Nowadays microendoscopicaccess is sometimes combined witha microscopic surgical technique. Commonto all of these techniques is thefact that the access pathway generallyhas to be bigger than would be necessaryfor the actual work to be performedin the spinal canal.The full-endoscopic interlaminar approachwas therefore developed in recentyears in order to exploit the knownadvantages of transforaminal operationsand arthroscopy.** Ruetten et al. (2006) A new full-endoscopictechnique for the interlaminar operation oflumbar disc herniations using 6 mm endoscopes:Prospective 2-year results of 331 patients.Minim Invasive Neurosurgery 49:80-87Ruetten et al. (2007) Use of newly developedinstruments and endoscopes: full-endoscopicresection of lumbar disc herniations via theinterlaminar and lateral transforaminal approach.J Neurosurg Spine 6:521-53017
<strong>VERTEBRIS</strong> lumbarThe full-endoscopic interlaminar techniqueThe fact that the lighting and imagingsystem with its 25° angle of vision issituated right in the working area makesit possible to minimize traumatizationnot only of the access pathway, butalso of structures of the spinal canal.Continuous irrigation provides excellentvisual conditions. Mobility is achievedby handling of the new endoscope usingthe joystick technique. Neural structuresare protected by use of the beveled operatingsheath as a nerve hook. Whenused in conjunction with the newly developedinstruments, this is a genuinelyminimally invasive technique.more limitations than the interlaminarapproach, but causes less tissue damage.Due to anatomic and pathologicfactors, the ratio of transforaminal tointerlaminar procedures in clinical practiceis about 40 to 60.The main indications are pathologiessituated within the spinal canal. Attentionmust be paid to the width of theinterlaminar window, which if too narrowmay prevent free passage of theendoscope. If this occurs the bone canbe resected with a burr until the targetpoint is reached without opening the ligamentumflavum or damaging thezygapophyseal joints. Bone resectionshould generally be avoided, though incases of spinal canal stenosis it maybe necessitated by the pathology. Theincision in the ligamentum flavum canbe limited to a few millimeters, sincepenetration into the spinal canal is facilitatedby the elasticity of the ligament.Mobility to the contralateral side is similarto that with conventional operations.In order to minimize resection of structuresof the spinal canal, craniocaudalaccess via neighboring lumbar segmentsmay be considered. The full-endoscopicinterlaminar technique permitsselective surgery on pathologies situatedwithin the spinal canal withminimal access-induced traumatization.The transforaminal technique isgenerally more suitable for intradiscaland intra- or extraforaminal work. Thetransforaminal approach is subject toThe interlaminar approach provides outstandingvisualization of the structures of the spinalcanal18
Vertebris1. PositioningThe patient is positioned prone on aradiolucent table with a pelvic and athoracic roll. Use of a C-arm is requiredduring the operation.Prone position with pelvic and thoracic roll2. Determination of access routeAccess is determined on the basis ofanatomic landmarks under posteroanteriorfluoroscopic guidance, accountbeing taken of the pathology. The skinincision should be made as far mediallyin the interlaminar window as possiblein order to permit insertion in alateral direction below the obliquely orientedzygapophyseal joints.Marking of skin entry pointThe skin entry point should be as medial aspossibleEntry below the zygapophyseal joints shouldbe made possiblePuncture incision19
<strong>VERTEBRIS</strong> lumbalThe full-endoscopic interlaminar technique3. Creation of accessAfter the skin entry point has beendetermined and the puncture incisionmade, the dilator is inserted as far asthe ligamentum flavum under posteroanteriorfluoroscopic guidance. Thesubsequent procedure is performed underlateral fluoroscopic guidance. Theworking sleeve with a beveled openingis advanced towards the ligament viathe dilator and the dilator is removed.Insertion firstly of the dilator and then of the sheath to the ligamentum flavum under fluoroscopicguidance20
Vertebris4. Performance of operationThe endoscope is passed through theworking sleeve. The operation is performed via the intraendoscopic workingchannel using alternating sets of instrumentsunder full visual control and withcontinuous irrigation. Once the ligamentumflavum has been opened, thespinal canal can be entered. Mobility isachieved by handling the endoscopeusing the joystick technique. The operatingsheath with its beveled openingserves as a second instrument and canbe rotated so as to protect the neuralstructures.The operating sheath with its beveled openingcan be rotated so as to serve as a secondinstrument21
<strong>VERTEBRIS</strong> lumbalThe full-endoscopic interlaminar techniqueThe sealing caps for the optic undworking sleeve should be used only forbrief periods when bleeding obscuresvision, since with long operation timesand unnoticed obstruction to backflowof irrigation fluid there is a theoreticalrisk of volume overload and increasedpressure within the spinal canal and inthe associated and adjacent structures.In order to reduce the risk of neurologicdamage particularly in the cranial segments,prolonged and continuous excessivemedial retraction of the neuralstructures with the working sleeve mustbe avoided or else retraction must beperformed on an intermittent basis.Experience has shown that, as with allnew techniques, the risk of complicationsis greatest during the learningperiod.Use of the endoscope based on the joystick principle provides mobilityOpening of the ligamentum flavumView of L5-S1 axilla22
VertebrisBone can be resected as necessary using theavailable instruments and burrsThe interlaminar approach makes it possible towork in the spinal canal under visual control23
<strong>VERTEBRIS</strong> lumbalThe full-endoscopic interlaminar technique5. Bone resectionResection of bone may be required inorder to increase mobility within thespinal canal or when problems ariseduring access. This can occur, for example,in cases of sequestered discherniations or small interlaminar windowand in recess stenosis operations.After access has been obtained, the bonystructures are dissected. It may beuseful to start decompression at thecaudal end of the descending facet.Depending on the pathology, medialparts of the descending or ascendingfacet or of the caudal and cranial laminaare then resected.It may be useful to start decompression atthe caudal end of the descending facetThe extent of bone resection depends on the pathologyA range of burrs and bone punches that canbe introduced through the intraendoscopicworking channel are available for boneresectionLateral bone resection is performed on the floorof the spinal canal in the working area24
<strong>VERTEBRIS</strong> thoracicIntroductionVertebrisDepending on the individual pathologyand anatomy, transforaminal and interlaminarprocedures can also be performedin the thoracic spine. The principalindication is thoracic intervertebraldisc herniations without major spinalcord compression that remains symptomaticdespite conservative therapy.Only laterally situated pathologies aregenerally amenable to operation, sincemanipulation of the spinal cord must beavoided because of the risk of injuryand because lateral transforaminal accessis prevented by the thoracic organs.When a transforaminal procedurethe lumbar spine. Compared to thelumbar spine, the thoracic spine is subjectto a greater risk of injury to neuraland surrounding structures and hencealso to technical limitations in termsof access and surgical procedure. Incases that are borderline in terms ofanatomy, pathology, or clinical features,a conventional operation may bethe only suitable option.<strong>Thoracic</strong> disc herniationis planned, a preoperative CT scanshould always be performed in order todetermine the exact skin entry point andthe possibility of free access to the intervertebraldisc. Interlaminar accessnormally requires resection of bone,since the size of the interlaminar windowis generally insufficient, especiallylateral to the spinal cord. Operationsusing either access route can be performedanywhere from the cervicothoracicto the thoracolumbar junction andare performed in the same way as in25
<strong>VERTEBRIS</strong> thoracic1. The full-endoscopictransforaminal techniqueAccess is determined with the aid of apreoperative CT scan. Structures to bespared are laterally the lung, mediallythe spinal cord, and ventrally the vessels.Access may be prevented by anatomicor degenerative bone structuressuch as ribs, transverse processes, orosteophytes. In general a decidedlyposterior approach is required.In order not to cause injury, the spinalcannula should be inserted parallel tothe intervertebral space under posteroanteriorfluoroscopic guidance; it shouldlie strictly caudally in the foramen andon making contact with the disc shouldbe situated exactly between the medialand the lateral pedicular line in the foramen.For added safety the spinal cannulacan first be advanced onto thebony structures of the intervertebral jointand then directed ventrally along thebone. After the dilator, the operatingsleeve, and the optic have been introduced,particular attention should bepaid during the operation to the mediallysituated spinal cord.26
Vertebris2. The full-endoscopicinterlaminar techniqueThe skin entry point is situated over theintervertebral joint/disc on the medialpedicular line, as in cervical foraminotomy.From this point the spinal canalcan be reached without manipulation ofthe spinal cord.After the dilator, the operating sleeve,and the optic have been introduced, thesize of the interlaminar window is generallyfound to be insufficient to permitentry into the spinal canal without boneresection. A small amount of burring istherefore performed on the medial sideof the joint facets and if necessary onthe cranial and the caudal laminae. Thelateral part of the spinal canal must beaccessible as far as the intervertebraldisc without need to displace the spinalcord medially. There is no limit to craniocaudalextension.27
<strong>VERTEBRIS</strong>Basic set, <strong>VERTEBRIS</strong> lumbar trans-, extraforaminal Set-Nr. 892101111devised by Dr. RuettenArticle Types pcs.Panoview Plus discoscope, 25°, WL 207 mm, Ø 6.9 x 5.6 mm, working channel Ø 4.1 mm 89210.1254 1Conical adapter 8791.751 1Membrane attachment 8792.451 1Spinal cannula set, 10 pieces, sterile, WL 150 mm, Ø 1.25 mm 4792.803 1Dilator, Ø. 6.9 mm 89220.1508 1Working sleeve with bevel, Ø 8.0 mm, WL 185 mm 89220.1078 1Extension sleeve, Ø 8.0 mm 89220.1408 1Working sleeve attachment, Ø 8.0 mm 89200.1008 1Micro-punch, Ø 2.5 mm, WL 360 mm 8792.671 1Micro-rongeur with long jaws, Ø 2.5 mm, WL 360 mm 89240.1125 1Nucleus grasping forceps, Ø 3.0 mm, WL 360 mm 89230.1003 1Nucleus grasping forceps, Ø 4.0 mm, WL 360 mm 89230.1004 1Tube shaft punch, Ø 4.0 mm, WL 360 mm 89240.1904 1Atraumatic dissector, Ø 2.5 mm, WL 350 mm 8792.591 1Atraumatic dissector, Ø 4.0 mm, WL 350 mm 89250.1004 1X-Tractor 89230.0000 1Mallet 8866.956 1Power control generator 2303.001 1Power stick M4 handle 8564.121 1Resector, Ø 4.0 mm, WL 350 mm 89970.1004 1Oval burr, laterally hooded, Ø 4.0 mm, WL 350 mm 89970.1504 1Oval burr, frontally hooded, Ø 4.0 mm; WL 350 mm 89970.1514 1"Surgitron" radiofrequency unit 2343.001/ .002 1Trigger Flex handpiece, complete 8792.691 1Trigger Flex bipolar electrodes 4792.6912 128
<strong>VERTEBRIS</strong>VertebrisBasic set, <strong>VERTEBRIS</strong> lumbar and thoracic interlaminar892102222Set-Nr.Article Types pcs.Panoview Plus discoscope, 25°, WL 165 mm, Ø 6.9 x 5.6 mm, working channel Ø 4.1 mm 89210.3254 1Conical adapter 8791.751 1Membrane attachment 8792.451 1Dilator, Ø 6.9 mm 89220.1508 1Working sleeve with bevel, Ø 8.0 mm, WL 120 mm 89220.3008 1Working sleeve attachment, Ø 8.0 mm 89200.1008 1Micro-punch, Ø 2.5 mm, WL 360 mm 8792.671 1Micro-rongeur with long jaws, Ø 2.5 mm, WL 360 mm 89240.1125 1Nucleus grasping forceps, Ø 3.0 mm, WL 360 mm 89230.1003 1Nucleus grasping forceps, Ø 4.0 mm, WL 360 mm 89230.1004 1Tube shaft punch, Ø 4.0 mm, WL 360 mm 89240.1904 1Atraumatic dissector, Ø 2.5 mm, WL 350 mm 8792.591 1Atraumatic dissector, Ø 4.0 mm, WL 350 mm 89250.1004 1Power control generator 2303.001 1Power stick M4 handle 8564.121 1Resector, Ø 4.0 mm, WL 350 mm 89970.1004 1Oval burr, laterally hooded, Ø 4.0 mm, WL 350 mm 89970.1504 1Oval burr, frontally hooded, Ø 4.0 mm, WL 350 mm 89970.1514 1"Surgitron" radiofrequency unit 2343.001/ .002 1Trigger Flex handpiece, complete 8792.691 1Trigger Flex bipolar electrodes 4792.6912 129
<strong>VERTEBRIS</strong>Basic set, <strong>VERTEBRIS</strong> thoracic transforaminal Set-Nr. 892103333devised by Dr. RuettenArticle Types pcs.Panoview Plus discoscope, 25°, WL 207 mm, Ø 5.9 x 5.0 mm, working channel Ø 3.1 mm 89210.1253 1Conical adaptor 8791.751 1Membrane attachment 8792.451 1Spinal cannula set, 10 pieces, sterile, WL 150 mm, Ø 1.25 mm 4792.803 1Dilator, Ø 5.9 mm 8792.764 1Working sleeve with bevel, Ø 7.0 mm, WL 185 mm 89220.1047 1Extension sleeve, Ø 7.0 mm 89220.1407 1Working sleeve attachment, Ø 7.0 mm 89200.1007 1Micro-punch, Ø 2.5 mm, WL 360 mm 8792.671 1Micro-rongeur with long jaws, Ø 2.5 mm, WL 360 mm 89240.1125 1Nucleus grasping forceps, Ø 3.0 mm, WL 360 mm 89230.1003 1Tube shaft punch, Ø 3.0 mm, WL 360 mm 89240.1903 1Atraumatic dissector, Ø 2.5 mm, WL 350 mm 8792.591 1Atraumatic dissector, Ø 3.0 mm, WL 350 mm 89250.1003 1X-Tractor 89230.0000 1Mallet 8866.956 1Power control generator 2303.001 1Power stick M4 handle 8564.121 1Resector, Ø 3.0 mm, WL 350 mm 89970.1003 1Oval burr, laterally hooded, Ø 3.0 mm, WL 350 mm 89970.1503 1Oval burr, frontally hooded, Ø 3.0 mm, WL 350 mm 89970.1513 1"Surgitron" radiofrequency unit 2343.001/ .002 1Trigger Flex handpiece, complete 8792.691 1Trigger Flex bipolar electrodes 4792.6912 130
<strong>VERTEBRIS</strong>VertebrisEndoscopes, working channel 2.7 mmArticleTypesPanoview Plus discoscope, 20°, Ø 5.8 x 5.1 mm, WL 205 mm 8792.411Panoview Plus discoscope, 20°, Ø 5.8 x 5.1 mm, MRI-compatible, WL 205 mm 8767.412Endoscopes, working channel 3.1 mmArticleTypesPanoview Plus discoscope, 25°, Ø 5.9 x 5.0 mm, WL 207 mm 89210.1253Panoview Plus discoscope, 25°, Ø 5.9 x 5.0 mm, WL 165 mm 89210.3253Endoscopes, working channel 4.1 mmArticleTypesPanoview Plus discoscope, 25°, Ø 6.9 x 5.6 mm, WL 207 mm 89210.1254Panoview Plus discoscope, 25°, Ø 6.9 x 5.6 mm, WL 165 mm 89210.3254Endoscope accessories/attachmentsArticleTypesSealing cap attachment, incl. 10 rubber caps 8792.452Sealing caps Ø up to 2.4 mm, pack of 10 89.00Sealing membrane 15 479.006Membrane attachment 8792.451Tap attachment 8791.951Conical adapter 8791.751O-rings for sealing between fluid adaptor and endoscope, pack of 10 9500.113Plug-on eyepiece funnel for connecting C-mount objectivesto endoscope optics with plug-on connection 8885.901Drip rejector, pack of 20 89200.1000Preparation basket for mechanical preparation and sterilization for discoscopes 89210.xxxx 38044.411Preparation basket for mechanical preparation and sterilization for discoscopes 8792.411, 8767.412 38044.111Antifogging agent 102.02Cleaning brush 6.0331
<strong>VERTEBRIS</strong>Spinal cannula setArticleTypesSpinal cannula set, Ø 1.25 mm, pack of 10, sterile, WL 250 mm 4792.802Spinal cannula set, Ø 1.25 mm, pack of 10, sterile, WL 150 mm 4792.803DilatorsArticleTypesDilator, Ø 5.9 mm, 1-channel for working sleeves Ø 7.0 mm 8792.763Dilator, Ø 5.9 mm, 2-channel for working sleeves Ø 7.0 mm 8792.764Dilator, Ø 6.9 mm, 2-channel for working sleeves Ø 8.0 mm 89220.1508Working sleeves, Ø 7.0 mmArticleTypesWorking sleeve with 30° bevel, WL 120 mm 89220.3007Working sleeve for foraminoplasty, WL 145 mm 89220.1017Working sleeve without window, WL 145 mm 89220.1057Working sleeves, basic set, WL 165 mm 89220.1907Working sleeve with long elevator lip, WL 165 mm 89220.1117Working sleeve with long window, WL 165 mm 89220.1087Working sleeve for foraminoplasty, WL 165 mm 89220.1007Working sleeve with distally closed window, WL 165 mm 89220.1137Working sleeve with dual window, WL 185 mm 89220.1027Working sleeve with elevator lip, WL 185 mm 89220.1157Working sleeve with long elevator lip, WL 185 mm 89220.1167Working sleeve with 30° bevel, WL 185 mm 89220.1047Working sleeve with 45° bevel, WL 185 mm 89220.1037Working sleeve with bevel, WL 185 mm 89220.1147Extension sleeve WL 155 mm 89220.140732
<strong>VERTEBRIS</strong>VertebrisWorking sleeves, Ø 8.0 mmArticleTypesWorking sleeve with 30° bevel, WL 120 mm 89220.3008Working sleeve for foraminoplasty, WL 145 mm 89220.1018Working sleeve, basic set, WL 165 mm 89220.1908Working sleeve with long elevator lip, WL 165 mm 89220.1068Working sleeve with dual window, WL 185 mm 89220.1028Working sleeve with elevator lip, WL 185 mm 89220.1088Working sleeve with long elevator lip, WL 185 mm 89220.1098Working sleeve with 30° bevel, WL 185 mm 89220.1078Working sleeve with 45° bevel, WL 185 mm 89220.1038Extension sleeve, WL 155 mm 89220.1408Fluid adaptorsArticleTypesFluid adaptor, Ø 7.0 mm 89220.1307Fluid adaptor, Ø 8.0 mm 89220.1308Working sleeve attachment, Ø 7.0 mm 89200.1007Working sleeve attachment, Ø 8.0 mm 89200.1008Sealing caps, pack of 10 89.03TrephinesArticleTypesTrephine, WL 195 mm, Ø 5.9 mm, cutting window Ø 3.0 mm 8792.503Trephine, WL 195 mm, Ø 5.9 mm, cutting window Ø 5.3 mm 8792.504Trephine, WL 195 mm, Ø 6.9 mm, cutting window Ø 6.3 mm 89260.110833
<strong>VERTEBRIS</strong>AccessoriesArticleTypesSmall spongiosa funnel, for working sleeve Ø 7.0 mm 89220.1517Large spongiosa funnel, for working sleeve Ø 7.0 mm 89220.1527Spongiosa ram, for working sleeve Ø 7.0 mm 89220.1507Shaver systemArticleTypesPower control 2303.001Power stick M4 8564.121Burrs / rotation knivesArticleTypesOval burr, Ø 2.5 mm, WL 350 mm, laterally hooded 8792.312Resector, Ø 2.5 mm, WL 350 mm, laterally hooded 8792.313Nucleus resector, Ø 3.0 mm, WL 350 mm, laterally hooded 89970.1003Oval burr, Ø 3.0 mm, WL 350 mm, laterally hooded 89970.1503Oval burr, Ø 3.0 mm, WL 350 mm, laterally and frontally hooded 89970.1513Nucleus resector, Ø 4.0 mm, WL 350 mm, laterally hooded 89970.1004Oval burr, Ø 4.0 mm, WL 350 mm, laterally hooded 89970.1504Oval burr, Ø 4.0 mm, WL 350 mm, laterally and frontally hooded 89970.1514Oval burr, Ø 4.5 mm, WL 220 mm, laterally hooded 8792.323Oval burr, Ø 4.5 mm, WL 220 mm, laterally hooded 8792.321Irrigation pump systemArticleTypesFluid control 2203.001Tube system, disposable, with puncture needle, pack of 10 4170.223Tube system, disposable, with Safe Lock, pack of 10 4170.22434
<strong>VERTEBRIS</strong>VertebrisHF / RF generatorsArticleTypesSurgitron radiofrequency unit, 4 MHz 2343.001/ .002Bipolar generator 2352.001/ .002RF accessories/electrodesArticleTypesTrigger Flex handpiece, complete 8792.691Trigger Flex bipolar electrodes, pack of 6 4792.6912HF instruments, bipolarArticleTypesBipolar micro grasping forceps, Ø 2.6 mm, WL 390 mm 89930.1010Bipolar inner part, pack of 3 89930.1001Tube shaft 89930.1002Handle 89930.1000HF electrodes, bipolar, Ø 2.0 mm, WL 400 mmArticleTypesRing electrode 8765.613Button electrode 8765.621Stepped ball electrode 8765.612Connecting piece 8765.554HF electrodes, monopolar, WL 400 mmArticleTypesButton electrode, Ø 1.6 mm 823.05Button electrode, Ø 2.0 mm 823.06Button electrode, Ø 2.6 mm 823.0835
<strong>VERTEBRIS</strong>Forceps / punches, Ø 2.0 mmArticleTypesDouble-spoon forceps, WL 360 mm 8793.561Grasping forceps, WL 360 mm 8793.621Micro-punch, WL 360 mm 8793.661Forceps / punches, Ø 2.5 mmArticleTypesMicro-rongeur, WL 290 mm 89240.2025Micro-rongeur, double-action, WL 290 mm 89240.2125Micro-punch, WL 290 mm 89240.2225Micro-bone punch, WL 290 mm 89240.2325Micro-rongeur, WL 360 mm 8792.632Micro-rongeur, double-action, WL 360 mm 8792.636Micro-punch, WL 360 mm 8792.671Micro-rongeur, extended jaws, WL 360 mm 89240.1125Nucleus grasping forceps, WL 360 mm 89230.1125Forceps / punches, Ø 3.0 mmArticleTypes+Micro-rongeur, WL 290 mm 89240.3003Micro-rongeur, double-action, WL 290 mm 89240.3013Micro-punch, WL 290 mm 89240.3023Tube shaft punch, WL 290 mm 89240.3903Micro-rongeur, WL 360 mm 89240.1003Micro-rongeur, double-action, WL 360 mm 89240.1013Micro-punch, WL 360 mm 89240.1023Nucleus grasping forceps, WL 360 mm 89230.1003Spreader, WL 360 mm 89230.1803Scissors, WL 360 mm 89240.1703Tube shaft punch, WL 360 mm 89240.190336
<strong>VERTEBRIS</strong>VertebrisForceps / punches, Ø 4.0 mmArticleTypesMicro-rongeur, WL 290 mm 89240.3004Micro-rongeur, double-action, WL 290 mm 89240.3014Micro-punch, WL 290 mm 89240.3024Tube shaft punch, WL 290 mm 89240.3904Micro-rongeur, WL 360 mm 89240.1004Micro-rongeur, double-action, WL 360 mm 89240.1014Micro-punch, WL 360 mm 89240.1024Nucleus grasping forceps, WL 360 mm 89230.1004Micro-rongeur, curved, WL 360 mm 89240.1624Tube shaft punch, curved, WL 360 mm 89240.1904Micro-rongeur, curved, WL 360 mm 89240.1044Micro-punch, Ø 2.5 mm, curved, WL 360 mm (fits in 4 mm working channel) 89240.1034Forceps / punches, Ø 5.2 mm for use through the working sleeveArticleTypesIntradiscal grasping forceps, articulating, WL 210 mm 8792.623Intradiscal punch, WL 210 mm 8792.663Intradiscal rongeur, conical jaw, WL 210 mm 89240.1052Assorted forceps / punches / scissors for use through the working sleeveArticleTypesPunch, Ø 2.7 mm, WL 210 mm 8792.661Scissors, Ø 2.7 mm, WL 240 mm 8792.641Grasping forceps, Ø 3.4 mm, WL 240 mm 8792.621Punch, Ø 3.4 mm, WL 240 mm 8792.662Suction punch, Ø 4.5 mm, WL 240 mm 8792.681Rongeur, Ø 4.5 x 4.2 mm, WL 210 mm 8791.601Rongeur, Ø 4.5 x 4.2 mm, WL 210 mm 8791.69137
<strong>VERTEBRIS</strong>Hand-held / accessory instruments, sharp-edgedArticleTypesAnnulotome, Ø 2.5 mm, WL 290 mm 89260.2125Bone dissector, Ø 2.5 mm, WL 290 mm 89260.2225Rasp, Ø 2.5 mm, WL 290 mm 89260.2325Trocar, Ø 2.5 mm, WL 290 mm 89260.2425Spoon, Ø 2.5 mm, WL 290 mm 89260.2525Curette, Ø 2.5 mm, WL 290 mm 89260.2625Rasp, Ø 2.5 mm, WL 350 mm 8792.541Trocar, Ø 2.5 mm, WL 350 mm 8792.551Spoon, Ø 2.5 mm, WL 350 mm 8792.562Annulotome, Ø 2.5 mm, WL 350 mm 8792.581Curette, Ø 2.5 mm, WL 350 mm 8792.571End-cut burr, Ø 3.0 mm, WL 350 mm 89260.1113End-cut burr, Ø 4.0 mm, WL 350 mm 89260.1114Hand-held / accessory instruments, atraumaticArticleTypesElevator, Ø 2.5 mm, WL 290 mm 89250.2025Hook probe, Ø 2.5 mm, WL 290 mm 89250.2125Probe, Ø 2.5 mm, WL 290 mm 89250.2225Dissector, Ø 2.5 mm, WL 350 mm 8792.591Dissector, Ø 3.0 mm, WL 350 mm 89250.1003Dissector, Ø 4.0 mm, WL 350 mm 89250.100438
<strong>VERTEBRIS</strong>VertebrisAccessoriesArticleTypesPositioning probe 8791.701Instrument grasping forceps 8793.856"X-Tractor" withdrawal instruments, complete set 89230.0000"X-Tractor" clamping device, small 89230.0003"X-Tractor" clamping device, large 89230.0004"X-Tractor" handle 89230.0008Mallet 8866.956Suction and irrigation accessoriesArtikelArticleTypenTypesFlushing valve, foot-operated 89870.0000Suction connector 89270.1000Sucker, Ø 2.5 mm, WL 290 mm 89270.2025Sucker, Ø 4.0 mm, WL 340 mm 89270.100439
LiteratureRUETTEN S, KOMP M, MERK H, GODO-LIAS GUse of newly developed instrumentsand endoscopes: full-endoscopic resectionof lumbar disc herniations via theinterlaminar and lateral transforaminalapproach.J Neurosurg Spine 2007; 6:521-530RUETTEN S, KOMP M, GODOLIAS G<strong>Lumbar</strong> discectomy with the full-endoscopicinterlaminar approach using newdeveloped optical systems and instruments.WSJ 2006;3:148-156RUETTEN S, KOMP M, GODOLIAS GNew developed devices for the full-endoscopiclateral transforaminal operationof lumbar disc herniations.WSJ 2006;3:157-165RUETTEN S, KOMP M, GODOLIAS GA new full-endoscopic technique for theinterlaminar operation of lumbar discherniations using 6 mm endoscopes:Prospective 2-year results of 331 patients.Minim Invasive Neurosurg 2006, 49:80-87RUETTEN S, KOMP M, GODOLIAS GAn extreme lateral access for the surgeryof lumbar disc herniations inside thespinal canal using the full-endoscopicuniportal transforaminal approach. –Technique and prospective results of463 patients.Spine 2005, 30, 2570-2578RUETTEN S, KOMP M, GODOLIAS GFull-endoscopic interlaminar operationof lumbar disc herniations using newendoscopes and instruments.Orthopaedische Praxis 2005, 10,527532RUETTEN SThe full-endoscopic interlaminar approachfor lumbar disc herniations. In:Mayer HM (ed) Minimally InvasiveSpine Surgery. Springer, BerlinHeidelberg New York, 2005, pp346355YEUNG ATMinimally invasive disc surgery with theYeung Endoscopic Spine System(YESS). Surg Technol Int 8:267-277,2000YEUNG ATThe evolution of percutaneous spinalendoscopy and discectomy: state of theart. Mt Sinai J Med 67:327-332, 2000YEUNG AT, TSOU PMPosterolateral endoscopic excision forlumbar disc herniation: surgical technique,outcome and complications in307 consecutive cases. Spine 27:722-731, 2002YEUNG AT, YEUNG CAAdvances in endoscopic disc and spinesurgery: foraminal approach. SurgTechnol Int 11:255-263, 200340
Notes41
42Notes
spirit of excellenceM E D I C A LV E T E R I N A R YI N D U S T R I A LSubject to change without notice.Printed on paper based on cellulose which has been bleached without the use of chlorine.RICHARD WOLF GmbH · 75434 Knittlingen · PF 1164 · Telephone +49 70 43 35-0 · Telefax +49 70 43 35-300 · GERMANY · info@richard-wolf.com · www.richard-wolf.comB 756.XI.08.GB www.stuetzlepartner.deAUSTRIA · BELGIUM / NETHERLANDS · FRANCE · GERMANY · INDIA · U.A.E. · UK · USA