PiCCO2 Nurse Booklet - PULSION Medical Systems SE
PiCCO2 Nurse Booklet - PULSION Medical Systems SE
PiCCO2 Nurse Booklet - PULSION Medical Systems SE
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
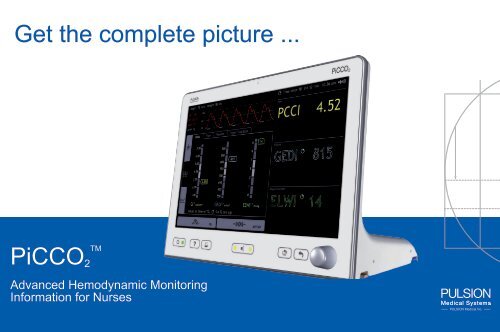
Get the complete picture ...<br />
TM<br />
<strong>PiCCO2</strong><br />
Advanced Hemodynamic Monitoring<br />
Information for <strong>Nurse</strong>s
TM<br />
<strong>PiCCO2</strong> - A complete hemodynamic picture<br />
• Continuous cardiac output<br />
• Volumetric preload<br />
• Afterload<br />
• Contractility<br />
• Volume responsiveness<br />
• Pulmonary edema / Lung water<br />
TM<br />
<strong>PiCCO2</strong> 2
Table of contents<br />
Overview..................................................................................................................<br />
Fields of Application ................................................................................................<br />
TM<br />
PiCCO Disposables and Set up 2<br />
..........................................................................<br />
TM<br />
Principles of PiCCO Technology 2<br />
..........................................................................<br />
Parameter Overview ................................................................................................<br />
TM<br />
<strong>PiCCO2</strong> Monitor .....................................................................................................<br />
Normal Ranges........................................................................................................<br />
Decision Tree Model ................................................................................................<br />
Summary of Benefits ...............................................................................................<br />
Recommended Literature ........................................................................................<br />
Contact Information ................................................................................................. 32<br />
4 - 6<br />
7<br />
8 - 11<br />
12 - 14<br />
15 - 25<br />
26<br />
27<br />
28<br />
29<br />
30<br />
3
Cardiac Output - Optimizing Oxygen delivery<br />
O 2 uptake O 2 transport O 2 extraction O 2 utilization<br />
Which therapy?<br />
Volume?<br />
PiCCO-Technology<br />
Vasopressors?<br />
Inotropes?<br />
4
Is measuring just the CO enough?<br />
Stroke volume<br />
SV<br />
Preload<br />
GEDV, SVV, PPV<br />
Pulmonary edema<br />
EVLW<br />
Volume?<br />
Cardiac output<br />
CO<br />
Heart rate<br />
HR<br />
Afterload<br />
SVR, MAP<br />
Vasopressors?<br />
Contractility<br />
CFI<br />
Inotropes?<br />
5
TM<br />
<strong>PiCCO2</strong> – See more than others<br />
Optimize CO<br />
• Continuous cardiac output<br />
• Volumetric preload<br />
• Afterload<br />
• Contractility<br />
• Volume responsiveness<br />
Protect the lungs<br />
• Monitor Pulmonary Edema<br />
(lung water) at the bedside.<br />
• Respond quickly<br />
• More reliable than Chest X Ray<br />
6
Fields of Application<br />
Intensive Care<br />
• Septic Shock<br />
• Cardiogenic Shock<br />
• Burns<br />
• Trauma / Hypovolemic Shock<br />
• ARDS / Acute Lung Injury<br />
• Pediatrics<br />
OR/Post surgery<br />
• Cardiac Surgery<br />
• Major Surgery<br />
• Neuro Surgery<br />
• Pediatrics<br />
7
Use your existing CVC and the PiCCO arterial line<br />
Central venous line<br />
(Standard CVC)<br />
Internal jugular, subclavian, femoral<br />
Arterial line<br />
(PiCCO Catheter available in different sizes)<br />
Brachial, axillary or femoral artery<br />
8
PiCCO arterial catheters - The choice is yours<br />
Axillary artery<br />
Adults: 4F 8 cm / 3.15 in<br />
Small adults: 3F 7 cm / 2.76 in<br />
Brachial artery<br />
Adults: 4F 16 cm / 6.29 in<br />
Adults: 4F 22 cm / 8.66 in<br />
Femoral artery<br />
Adults: 5F 20 cm / 7.78 in<br />
Adults: 4F 22 cm / 8.66 in<br />
Small adults: 4F 16 cm / 6.29 in<br />
Children: 3F 7 cm / 2.76 in and 4F 8 cm / 3.15 in<br />
9
TM<br />
<strong>PiCCO2</strong> Setup<br />
Thermodilution<br />
D<br />
F<br />
C<br />
B<br />
CVP line<br />
A G<br />
E<br />
Flush bag<br />
A<br />
B<br />
C<br />
D<br />
E<br />
F<br />
G<br />
Pressure output adapter<br />
PiCCO Catheter<br />
Distal lumen of CVC<br />
Injectate sensor housing<br />
Injectate sensor cable<br />
Arterial connection cable<br />
PiCCO thermistor plug<br />
Pressure connection<br />
cable<br />
10
PiCCO - Two principles for reliable information<br />
Transpulmonary thermodilution Pulse contour analysis<br />
Intermittent parameters from<br />
thermodilution technique<br />
• Thermodilution cardiac output (CO) /<br />
cardiac index (CI)<br />
• Volumetric preload (GEDV/GEDI)<br />
• Contractility (CFI)<br />
• Lung water (EVLW/ELWI)<br />
Calibration<br />
Continuous parameters from analysis of<br />
the arterial waveform (pulse contour)<br />
• Pulse contour cardiac output (PCCO) /<br />
cardiac index (PCCI)<br />
• Afterload (SVR/SVRI)<br />
• Volume responsiveness (SVV, PPV)<br />
• Stroke volume (SV/SVI)<br />
11
PiCCO - Transpulmonary Thermodilution (TD)<br />
Bolus<br />
injection<br />
Bolus<br />
detection<br />
• The bolus injection of cold saline is detected by the temperature sensor attached to the CVC<br />
• The saline bolus passes through the heart and lungs and is detected downstream by the<br />
thermistor on the tip of the PiCCO arterial line<br />
• The change in temperature between the two thermistors provides a TD curve<br />
• Mathematical analysis of the TD curve gives the cardiac output CO<br />
• Further analysis of the TD curve allows determination of preload volumes and lung water<br />
12
PiCCO - Pulse Contour Analysis<br />
• Stroke volume is the area under the systolic part of the pressure curve (red area)<br />
of one heart beat<br />
• Cardiac output is calculated and updated beat-by-beat: stroke volume x heart rate<br />
• In severely “shocked” patients organ perfusion pressure and pulse contour CO is<br />
more reliably represented by central arterial pressure (femoral / brachial / axillary)<br />
than by radial arterial pressure<br />
13
CI<br />
Thermodilution (TD) Cardiac Output / Index<br />
Cardiac Output - Volume of blood pumped by the heart in one minute<br />
- Important determinant for oxygen delivery to the body<br />
TD Results<br />
CI<br />
GEDI<br />
ELWI<br />
T<br />
10:18 am 10:20 am 10:22 am 10:26 am<br />
<strong>SE</strong>P 23 <strong>SE</strong>P 23 <strong>SE</strong>P 23 <strong>SE</strong>P 23<br />
3.47 3.11 3.15 3.76 3.44<br />
705 626 678 764 698<br />
9 9 10 10 9<br />
1.18 1.17 0.30 1.20<br />
Inj. Volume<br />
98.1<br />
10:26 am 15 ml<br />
<strong>SE</strong>P 23<br />
CVP<br />
5 mmHg<br />
START<br />
98.6<br />
READY 0s 10s 20s<br />
30s Exit<br />
Time since TD 0 h 52 min 10:26 am<br />
Flow<br />
PCCI<br />
SVRI 1735<br />
-5 2<br />
5.0<br />
3.0<br />
4.52<br />
l/min/m2 SVI 47<br />
ml/m<br />
Volume<br />
2<br />
l/min/m2 dyn*s*cm m<br />
CO – Cardiac Output<br />
CI – Cardiac Index<br />
The Thermodilution CO is used to “calibrate“ the continuous CO obtained from the arterial waveform<br />
(pulse contour) analysis.<br />
14
Pulse Contour Cardiac Output / Index<br />
Cardiac Output - Following thermodilution a “calibrated” continuous CO can be obtained<br />
Time since TD 0 h 52 min 10:26 am<br />
PCCI<br />
Flow<br />
PCCI<br />
SVRI 1735<br />
PCCO – Pulse Contour Cardiac Output<br />
PCCI – Pulse Contour Cardiac Index<br />
Volume<br />
• Product of stroke volume and heart rate<br />
• Determination beat-by-beat MAP<br />
• Reliability and patient safety possible due to calibration technique<br />
-5 2<br />
dyn*s*cm m<br />
5.0<br />
3.0<br />
4.52<br />
l/min/m2 SVI 47<br />
ml/m 2<br />
l/min/m 2<br />
ml/m 2<br />
15
Preload Volume instead of filling SVRI pressures 1735<br />
PCCI<br />
MAP<br />
Volume<br />
SVV 9<br />
-5 2<br />
dyn*s*cm m<br />
Preload - Volume of blood in the heart, available to be pumped<br />
l/min/m 2<br />
SVI 47<br />
ml/m 2<br />
l/min/m2 Volumetric preload parameters are superior to filling pressures (CVP / PCWP) Michard, YICM 2004<br />
ml/m 2<br />
GEDV – Global End-Diastolic Volume / GEDI – Global Organ End-Diastolic Function Volume Index<br />
• Combined diastolic volume of all four heart chambers<br />
• Adequate preload is an important prerequisite for adequate cardiac output (Frank-Starling curve)<br />
• GEDI is indexed to “predicted body surface area” *<br />
* Indexing particular SVRI parameters i.g. to the predicted body weight (EVLW) or predicted body surface area (GEDV) rather<br />
than the actual body weight or body surface area is more accurate particularly in overweight patients.<br />
ml/kg<br />
%<br />
16
Lung Water – Pulmonary MAP edema assessment at the bedside<br />
SVRI<br />
Volume<br />
EVLW – Extravascular Lung Water reflects pulmonary edema<br />
SVV 9<br />
Organ Function<br />
ml/m 2<br />
ml/kg<br />
AP/CVP<br />
EVLW – Extravascular Lung Water / ELWI – Extravascular Lung Water 1/min Index<br />
• Extravascular lung water (EVLW) represents the extravascular water content of the lung tissue<br />
• Includes intra-cellular, interstitial and intra-alveolar water (not pleural effusion)<br />
• ELWI is indexed to “Predicted Body Weight”<br />
*Predicted body weight is determined from the body height, gender and age<br />
%<br />
17
Fluid management using lung water (ELWI)<br />
Improved patient outcomes<br />
Organ function - Lung water<br />
Days<br />
Control group<br />
PCWP<br />
Ventilation days<br />
reduced by<br />
59%<br />
Protocol group<br />
EVLW<br />
Comparison of fluid therapy targeting lung water (protocol<br />
group) or wedge pressure (standard group)<br />
Control group<br />
PCWP<br />
ICU days<br />
reduced by<br />
53%<br />
Protocol group<br />
EVLW<br />
Source: Improved outcome based on fluid management in critically ill patients requiring pulmonary artery catheterization<br />
Mitchell JP, Schuller D, Calandrino FS, Schuster DP, Am Rev Respir Dis 1992; 145(5): 990-8<br />
18
Afterload - the systemic vascular Flow resistance<br />
PCCI<br />
MAP<br />
Volume<br />
Time since TD 0 h 52 min 10:26 am<br />
PCCI 4.52<br />
l/min/m2 Systemic vascular resistance - Represents the vascular “tone” of the blood vessels.<br />
SVR - Systemic Vascular Resistance<br />
SVRI - Systemic Vascular Resistance Index<br />
• Helps to determine levels of vasodilation or vasoconstriction<br />
• Useful for guiding vasopressor management.<br />
SVRI 1735<br />
-5 2<br />
dyn*s*cm m<br />
5.0<br />
3.0<br />
SVI 47<br />
ml/m 2<br />
l/min/m 2<br />
ml/m 2<br />
19
Heart Contractility<br />
SVRI<br />
AP/CVP<br />
SVV 9<br />
Contractility – describes the performance of the cardiac muscle<br />
Organ Function<br />
CFI - Cardiac Function Index<br />
• Parameter of the global cardiac contractility<br />
• The cardiac function index is the ratio of flow and preload<br />
• CFI = CO (Cardiac Output) / GEDV (Global End-Diastolic Volume)<br />
%<br />
1/min<br />
ml/m 2<br />
ml/kg<br />
20
Balance fluid and inotrope therapy correctly<br />
SV (ml)<br />
80<br />
40<br />
600 800<br />
Inotropic drugs<br />
preload<br />
GEDI (ml/m 2 )<br />
The Frank-Starling curve reflects the interaction between preload and stroke volume<br />
1. Increase preload volume to its optimum<br />
2. Increased contractility shifts the curve upwards (see graphic)<br />
2<br />
1 increase preload<br />
Frank-Starling<br />
curve<br />
21
Volume Responsiveness<br />
Volume<br />
Volume<br />
Volume<br />
Volume Responsiveness - predicts MAPwhether<br />
cardiac output will improve with volume resuscitation<br />
SVRI SVRI<br />
SVRI<br />
MAP MAP<br />
SVV SVV 9<br />
SVV 9 9 %<br />
%<br />
%<br />
Organ Function<br />
Organ Function<br />
Organ Function<br />
l/min/m2 l/min/m2 l/min/m2 ml/m 2<br />
ml/m 2<br />
ml/m 2<br />
SVV – Stroke Volume Variation<br />
ml/kg<br />
• Variation in stroke volume over the breathing cycle during positive pressure ventilation ml/kg<br />
ml/kg<br />
PPV – Pulse Pressure Variation<br />
• Variation in pulse pressure over the breathing cycle during positive pressure ventilation<br />
AP/CVP<br />
1/min<br />
Limitations: Only applicable in fully<br />
AP/CVP<br />
AP/CVP mechanically ventilated 1/min patients<br />
1/min<br />
in sinus rhythm<br />
22
Determination of Volume Responsiveness<br />
SVmax<br />
inspiration<br />
Mechanical Ventilation<br />
SVmin<br />
expiration<br />
PPmax<br />
inspiration<br />
PPmin<br />
expiration<br />
Intrathoracic pressure fluctuations<br />
Changes in intrathoracic blood volume<br />
Preload changes<br />
Fluctuations in stroke volume<br />
and pulse pressure<br />
23
Different views - Early warning, details, response to treatment<br />
Overview<br />
SVI<br />
SVV<br />
PCCI<br />
SVRI<br />
MAP<br />
’SpiderVision TM ’ screen<br />
Dynamic status indicator<br />
Height 70 inch Weight 182 lbs Time since TD 0 h 52 min 10:26 am<br />
HR 86<br />
Basic<br />
140<br />
AP 132/71<br />
AP<br />
MAP 91<br />
(CVP 9) Details<br />
70<br />
7.00<br />
6.00<br />
5.00<br />
4.00<br />
3.00<br />
2.00<br />
1.00<br />
CI l/min/m2 2.86<br />
Flow Volume Organ Function<br />
900<br />
850<br />
800<br />
750<br />
700<br />
650<br />
600<br />
550<br />
815<br />
ml/m 2<br />
Values at time of TD, 0 h 52 min ago<br />
11<br />
TD AP/CVP<br />
9<br />
7<br />
5<br />
3<br />
1<br />
0<br />
14<br />
ELWI ml/kg<br />
’Profiles’ screen<br />
Detailed insight at parameter<br />
level<br />
Flow<br />
PCCI 4.52<br />
Volume<br />
Organ Function 90<br />
Trends<br />
120<br />
AP<br />
60<br />
9.0<br />
PCCI/CI<br />
5.0<br />
1.0<br />
2800<br />
SVRI<br />
2100<br />
1400<br />
x<br />
xxx<br />
-6h -5h -4h<br />
-3h -2h<br />
-1h 10:26 am<br />
’Trends’ screen<br />
Clinical trends and therapy results<br />
24
Innovative operation - via touch-screen or navigation dial<br />
Real-time<br />
pressure curve<br />
Innovative<br />
data<br />
visualization<br />
Information bar<br />
Direct access buttons<br />
Parameter<br />
fields<br />
25
PiCCO Catheter codes and descriptions<br />
Application Artery Article No. Diameter Usable length<br />
Adults Femoral PV2015L20N 5F / (~14G) / 1,7 mm 20 cm / 7.78 in<br />
Adults Brachial Cubital PV2014L22N 4F / (~16G) / 1,3 mm 22 cm / 8.66 in<br />
Adults Femoral PV2014L22N 4F / (~16G) / 1,3 mm 22 cm / 8.66 in<br />
Adults Brachial Proximal PV2014L16N 4F / (~16G) / 1,3 mm 16 cm / 6.29 in<br />
Small adults Femoral PV2014L16N 4F / (~16G) / 1,3 mm 16 cm / 6.29 in<br />
Adults Axillary PV2014L08N 4F / (~16G) / 1,3 mm 8 cm / 3.15 in<br />
Children Femoral PV2014L08N 4F / (~16G) / 1,3 mm 8 cm / 3.15 in<br />
Children Femoral PV2013L07N 3F / (~18G) / 1,0 mm 7 cm / 2.76 in<br />
Small adults Axillary PV2013L07N 3F / (~18G) / 1,0 mm 7 cm / 2.76 in<br />
26
Hemodynamic Measurement Guide - Normal Values<br />
Cardiac Index<br />
CI<br />
3.0 – 5.0<br />
I/min/m<br />
Stroke Volume Index<br />
SVI<br />
40 – 60<br />
Global End-Diastolic Volume Index GEDI<br />
680 – 800<br />
Stroke Volume Variation<br />
SVV<br />
< 10<br />
Pulse Pressure Variation<br />
PPV<br />
< 10<br />
Systemic Vascular Resistance Index SVRI<br />
1970 - 2390<br />
Cardiac Function Index<br />
CFI<br />
4.5 – 6.5<br />
Mean Arterial Pressure<br />
MAP<br />
70 – 90<br />
Extravascular Lung Water Index ELWI<br />
< 10<br />
2<br />
ml/m2 ml/m2 %<br />
%<br />
dyn*s*cm-5 *m2 Parameter Abbreviation Range Unit<br />
1/min<br />
mmHg<br />
ml/kg<br />
WARNING: <strong>PULSION</strong> <strong>Medical</strong> <strong>Systems</strong> is a medical device manufacturer and does not practice medicine.<br />
<strong>PULSION</strong> does not recommend these normal values for a specific patient. The treating physician is responsible<br />
for determining and utilizing the appropriate diagnostic and therapeutic measures for each individual patient.<br />
27
Hemodynamic Measurement Guide<br />
This decision model is not obligatory. It cannot replace the individual therapeutic decisions of the treating physician.<br />
CI (l/min/m<br />
Measured Values<br />
2)<br />
GEDI (ml/m2) ELWI (ml/kg)<br />
Therapy Options<br />
Targeted Values<br />
1. GEDI (ml/m2) 2. Optimise SVV (%)*<br />
CFI (1/min)<br />
ELWI (ml/kg)<br />
(slow response)<br />
< 10<br />
V+?<br />
> 700<br />
< 10<br />
> 4.5<br />
< 3.0<br />
< 700 > 700<br />
> 10<br />
V+?<br />
Cat?<br />
700-800<br />
< 10<br />
> 5.5<br />
< – 10<br />
< 10<br />
Cat?<br />
> 700<br />
< 10<br />
> 4.5<br />
> 10<br />
Cat?<br />
V-?<br />
700-800<br />
< 10<br />
> 5.5<br />
< – 10<br />
< 10<br />
V+?<br />
> 700<br />
< 10<br />
> 3.0<br />
< 700 > 700<br />
> 10<br />
V+?<br />
700-800<br />
< 10<br />
< 10<br />
OK!<br />
> 10<br />
V-?<br />
700-800<br />
V+ = volume loading V- = volume reduction Cat = catecholamine / cardiovascular agents *SVV is only applicable in fully ventilated patients without cardiac arrhythmia<br />
< 10<br />
< – 10<br />
< 10<br />
< – 10<br />
28
The benefits of PiCCO-Technology<br />
• Reliable information from a calibrated system<br />
• A Cardiac Ouput/Index that is more reliable for organ perfusion<br />
• Protect the lungs with lung water assessment at the bedside<br />
• Patient volume status using volumes not filling pressures<br />
• Accurate information means increased patient safety<br />
• Gain a better understanding of your patients’ condition<br />
TM • Simple step by step set up of the <strong>PiCCO2</strong> system<br />
29
Recommended Literature<br />
Outcome Papers<br />
• Performance of Bedside Transpulmonary Thermodilution Monitoring for Goal-Directed HemodynamicManagement After Subarachnoid<br />
Hemorrhage; Mutoh T, Kazumata K, Ishikawa T, Terasaka S Stroke 2009; 40(7): 2368 – 74<br />
• Single transpulmonary thermodilution and continuous monitoring of central venous oxygen saturation during off-pump coronary<br />
surgery; Smetkin AA, Kirov M, Kuzkov VV, Lenkin AI, Eremeev AV, Slastilin VY, Borodin VV, Bjertnaes LJ. Acta Anaesthesiol<br />
Scand 2009; 53: 505-14<br />
• Arterial thermodilution in burn patients suggests a more rapid fluid administration during early resuscitation; Csontos C, Foldi V,<br />
Fischer T, Bogar L. Acta Anaesthesiol Scand 2008; 52(6): 742-9<br />
• Goal directed fluid management reduces vasopressor and catecholamine use in cardiac surgery patients; Goepfert M, Reuter D,<br />
Akyol D, Lamm P, Kilger E, Goetz A. Intensive Care Medicine 2007; 33: 96-103<br />
• Improved outcome based on fluid management in critically ill patients requiring pulmonary artery catheterization; Mitchell JP,<br />
Schuller D, Calandrino FS, Schuster DP. Am Rev Respir Dis 1992; 145(5): 990-8<br />
30
Recommended Literature<br />
Guidelines and Standard Operating Procedures<br />
• Goal directed fluid management reduces vasopressor and catecholamine use in cardiac surgery patients; Goepfert M, Reuter D,<br />
Akyol D, Lamm P, Kilger E, Goetz A. Intensive Care Medicine 2007; 33: 96-103<br />
• Influence of extravascular lung water determination in fluid and vasoactive therapy; Pino-Sanchez F, Lara-Rosales R, Guerrero-<br />
Lopez F, Chamorro-Marin V, Navarrete-Navarro P, Carazo-de la Fuente E, Fernandez-Mondejar E. J Trauma 2009; 67(6): 1220-4<br />
• 2007 American College of Critical Care Medicine clinical practice parameters for hemodynamic support of pediatric and neonatal<br />
septic shock; Brierley J, Choong K, Cornell T, Decaen A,Deymann A, Doctor A, Davis A, Duff J, Dugas MA et al. Crit Care Med 2009;<br />
37(2): 666 – 688<br />
• Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2008; Dellinger RP, Levy<br />
MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach<br />
H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL,<br />
Vincent JL. Intensive Care Med 2008; 34(1): 17-60<br />
• Implementation of an evidence-based „standard operating procedure“ and outcome in septic shock; kortgen A, Niederprün P, Bauer<br />
M. Crit Care Med 2006; 34(4): 939-9<br />
31
Recommended Literature<br />
Cardiac Output – Flow<br />
• Where do we go from here? Cardiac output determination in pediatrics; Hanna BD. Childrens Hospital of Philadelphia Crit Care Med<br />
2008; 36: 1377-8<br />
• Cardiac index measurements during rapid preload changes: a comparison of pulmonary artery thermodilution with arterial pulse<br />
contour, analysis; Felbinger TW, Reuter DA, Eltzschig HK, Bayerlein J, Goetz AE. J Clin Anesth 2005; 17(4):241-8<br />
Preload (Global Enddiastolic Volume)<br />
• Volumetric preload measurement by thermodilution: a comparison with transoesophageal echocardiography; Hofer CK, Furrer L,<br />
Matter-Ensner S, Maloigne M, Klaghofer R, Genoni M, Zollinger A. Br J Anaesth 2005; 94(6):748-55<br />
• Global end-diastolic volume as an indicator of cardiac preload in patients with septic shock; Michard F, Alaya S, Zarka V, Bahloul M,<br />
Richard C, Teboul JL.; Chest 2003 124(5):1900-8<br />
Lung Water<br />
• Extravascular lung water in sepsis-associated acute respiratory distress syndrome: indexing with predicted body weight improves<br />
correlation with severity of illness and survival. Phillips C, Chesnutt M, Smith M. Crit Care Med 2008; 36: 69-73<br />
• Extravascular lung water measurements and hemodynamic monitoring in the critically ill: bedside alternatives to the pulmonary artery<br />
catheter. Isakow W, Schuster DP. ; Am J Physiol Lung Cell Mol Physiol 2006 291: 1118 – 33<br />
• Extravascular lung water in patients with severe sepsis: a prospective cohort study; Martin GS, Eaton S, Mealer M, Moss M. Crit<br />
Care 2005; 9: R74-82<br />
• Improved outcome based on fluid management in critically ill patients requiring pulmonary artery catheterization; Mitchell JP, Schuller<br />
D, Calandrino FS, Schuster DP. Am Rev Respir Dis 1992; 145: 990-8<br />
32
Contact<br />
For further information on:<br />
• Literature for specific fields of application<br />
• Case studies<br />
• Product information<br />
• Educational material<br />
visit www.<strong>PULSION</strong>.com or contact us toll free 877.655.8844<br />
See instructions for use and package insert for full prescribing information. Technical specifications are subject to change without further notice.<br />
© 2010 <strong>PULSION</strong> <strong>Medical</strong> <strong>Systems</strong> AG all rights reserved.<br />
<strong>PULSION</strong> <strong>Medical</strong> Inc. • 2445 Gateway • Drive Suite 110 • Irving, Texas 75063<br />
Toll free 877.655.8844 • Phone 214.446.8500 • Fax 214.446.6702<br />
info@pulsion.com • www.<strong>PULSION</strong>.com<br />
MPI851805US_R00 © <strong>PULSION</strong> ® 05/2010<br />
33