JCAR890120-1011664r08 1 This version includes all HFS 1st ...
JCAR890120-1011664r08 1 This version includes all HFS 1st ...
JCAR890120-1011664r08 1 This version includes all HFS 1st ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
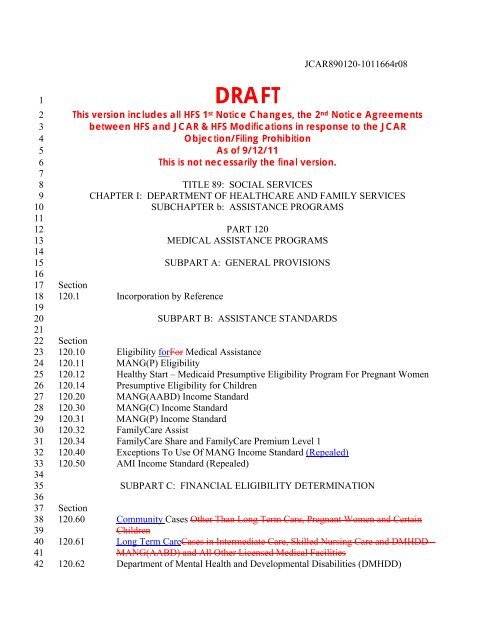
<strong>JCAR890120</strong>-<strong>1011664r08</strong>123456789101112131415161718192021222324252627282930313233343536373839404142DRAFT<strong>This</strong> <strong>version</strong> <strong>includes</strong> <strong>all</strong> <strong>HFS</strong> 1 st Notice Changes, the 2 nd Notice Agreementsbetween <strong>HFS</strong> and JCAR & <strong>HFS</strong> Modifications in response to the JCARObjection/Filing ProhibitionAs of 9/12/11<strong>This</strong> is not necessarily the final <strong>version</strong>.TITLE 89: SOCIAL SERVICESCHAPTER I: DEPARTMENT OF HEALTHCARE AND FAMILY SERVICESSUBCHAPTER b: ASSISTANCE PROGRAMSPART 120MEDICAL ASSISTANCE PROGRAMSSUBPART A: GENERAL PROVISIONSSection120.1 Incorporation by ReferenceSUBPART B: ASSISTANCE STANDARDSSection120.10 Eligibility forFor Medical Assistance120.11 MANG(P) Eligibility120.12 Healthy Start – Medicaid Presumptive Eligibility Program For Pregnant Women120.14 Presumptive Eligibility for Children120.20 MANG(AABD) Income Standard120.30 MANG(C) Income Standard120.31 MANG(P) Income Standard120.32 FamilyCare Assist120.34 FamilyCare Share and FamilyCare Premium Level 1120.40 Exceptions To Use Of MANG Income Standard (Repealed)120.50 AMI Income Standard (Repealed)SUBPART C: FINANCIAL ELIGIBILITY DETERMINATIONSection120.60 Community Cases Other Than Long Term Care, Pregnant Women and CertainChildren120.61 Long Term CareCases in Intermediate Care, Skilled Nursing Care and DMHDD –MANG(AABD) and All Other Licensed Medical Facilities120.62 Department of Mental Health and Developmental Disabilities (DMHDD)
<strong>JCAR890120</strong>-<strong>1011664r08</strong>8687888990919293949596979899100101102103104105106107108109110111112113114115116117118119120121122123124125126127128120.225 Social Security Numbers (Repealed)120.230 Unearned Income (Repealed)120.235 Exempt Unearned Income (Repealed)120.236 Education Benefits (Repealed)120.240 Unearned Income In-Kind (Repealed)120.245 Earmarked Income (Repealed)120.250 Lump Sum Payments and Income Tax Refunds (Repealed)120.255 Protected Income (Repealed)120.260 Earned Income (Repealed)120.261 Budgeting Earned Income (Repealed)120.262 Exempt Earned Income (Repealed)120.270 Recognized Employment Expenses (Repealed)120.271 Income From Work/Study/Training Program (Repealed)120.272 Earned Income From Self-Employment (Repealed)120.273 Earned Income From Roomer and Boarder (Repealed)120.275 Earned Income In-Kind (Repealed)120.276 Payments from the Illinois Department of Children and Family Services(Repealed)120.280 Assets (Repealed)120.281 Exempt Assets (Repealed)120.282 Asset Disregards (Repealed)120.283 Deferral of Consideration of Assets (Repealed)120.284 Spend-down of Assets (AMI) (Repealed)120.285 Property Transfers (Repealed)120.290 Persons Who May Be Included in the Assistance Unit (Repealed)120.295 Payment Levels for AMI (Repealed)SUBPART H: MEDICAL ASSISTANCE – NO GRANT (MANG) ELIGIBILITY FACTORSSection120.308 Client Cooperation120.309 Caretaker Relative120.310 Citizenship120.311 Residence120.312 Age120.313 Blind120.314 Disabled120.315 Relationship120.316 Living Arrangements120.317 Supplemental Payments120.318 Institutional Status120.319 Assignment of Rights to Medical Support and Collection of Payment120.320 Cooperation in Establishing Paternity and Obtaining Medical Support
<strong>JCAR890120</strong>-<strong>1011664r08</strong>129130131132133134135136137138139140141142143144145146147148149150151152153154155156157158159160161162163164165166167168169170171120.321 Good Cause for Failure to Cooperate in Establishing Paternity and ObtainingMedical Support120.322 Proof of Good Cause for Failure to Cooperate in Establishing Paternity andObtaining Medical Support120.323 Suspension of Paternity Establishment and Obtaining Medical Support UponFinding Good Cause120.324 Health Insurance Premium Payment (HIPP) Program120.325 Health Insurance Premium Payment (HIPP) Pilot Program120.326 Foster Care Program120.327 Social Security Numbers120.328 Compliance with Employment and Work Activity Requirements (Suspended;Repealed)120.329 Compliance with Non-Economic Eligibility Requirements of Article IV(Suspended; Repealed)120.330 Unearned Income120.332 Budgeting Unearned Income120.335 Exempt Unearned Income120.336 Education Benefits120.338 Incentive Allowance120.340 Unearned Income In-Kind120.342 Child Support and Spousal Maintenance Payments120.345 Earmarked Income120.346 Medicaid Qualifying Trusts120.347 Treatment of Trusts and Annuities120.350 Lump Sum Payments and Income Tax Refunds120.355 Protected Income120.360 Earned Income120.361 Budgeting Earned Income120.362 Exempt Earned Income120.363 Earned Income Disregard – MANG(C)120.364 Earned Income Exemption120.366 Exclusion From Earned Income Exemption120.370 Recognized Employment Expenses120.371 Income From Work/Study/Training Programs120.372 Earned Income From Self-Employment120.373 Earned Income From Roomer and Boarder120.375 Earned Income In-Kind120.376 Payments from the Illinois Department of Children and Family Services120.379 Provisions for the Prevention of Spousal Impoverishment120.380 ResourcesAssets120.381 Exempt ResourcesAssets120.382 ResourceAsset Disregard120.383 Deferral of Consideration of Assets
<strong>JCAR890120</strong>-<strong>1011664r08</strong>172173174175176177178179180181182183184185186187188189190191192193194195196197198199200201202203204205206207208209210211212213214120.384 Spenddown of ResourcesAssets (AABD MANG)120.385 Factors Affecting Eligibility for Long Term Care ServicesProperty Transfers forApplications Filed Prior to October 1, 1989 (Repealed)120.386 Property Transfers Occurring On or Before August 10, 1993120.387 Property Transfers Occurring On or After August 11, 1993 and Before November1, 2006120.388 Property Transfers Occurring On or After November 1, 2006120.390 Persons Who May Be Included In the Assistance Unit120.391 Individuals Under Age 18 Who Do Not Qualify For AFDC/AFDC-MANG AndChildren Born October 1, 1983, or Later120.392 Pregnant Women Who Would Not Be Eligible For AFDC/AFDC-MANG If TheChild Were Already Born Or Who Do Not Qualify As Mandatory Categoric<strong>all</strong>yNeedy120.393 Pregnant Women And Children Under Age Eight Years Who Do Not Qualify AsMandatory Categoric<strong>all</strong>y Needy Demonstration Project120.395 Payment Levels for MANG (Repealed)120.399 Redetermination of Eligibility120.400 Twelve Month Eligibility for Persons under Age 19SUBPART I: SPECIAL PROGRAMSSection120.500 Health Benefits for Persons with Breast or Cervical Cancer120.510 Health Benefits for Workers with Disabilities120.520 SeniorCare (Repealed)120.530 Home and Community Based Services Waivers for Medic<strong>all</strong>y Fragile,Technology Dependent, Disabled Persons Under Age 21120.540 Illinois Healthy Women Program120.550 Asylum Applicants and Torture Victims120.TABLE A Value of a Life Estate and Remainder Interest120.TABLE B Life Expectancy (Repealed)AUTHORITY: Implementing Articles III, IV, V and VI and authorized by Section 12-13 of theIllinois Public Aid Code [305 ILCS 5/Arts. III, IV, V and VI and 12-13] and implementing thefederal Deficit Reduction Act of 2005.SOURCE: Filed effective December 30, 1977; peremptory amendment at 2 Ill. Reg. 17, p. 117,effective February 1, 1978; amended at 2 Ill. Reg. 31, p. 134, effective August 5, 1978;emergency amendment at 2 Ill. Reg. 37, p. 4, effective August 30, 1978, for a maximum of 150days; peremptory amendment at 2 Ill. Reg. 46, p. 44, effective November 1, 1978; peremptoryamendment at 2 Ill. Reg. 46, p. 56, effective November 1, 1978; emergency amendment at 3 Ill.Reg. 16, p. 41, effective April 9, 1979, for a maximum of 150 days; emergency amendment at 3
<strong>JCAR890120</strong>-<strong>1011664r08</strong>215216217218219220221222223224225226227228229230231232233234235236237238239240241242243244245246247248249250251252253254255256257Ill. Reg. 28, p. 182, effective July 1, 1979, for a maximum of 150 days; amended at 3 Ill. Reg.33, p. 399, effective August 18, 1979; amended at 3 Ill. Reg. 33, p. 415, effective August 18,1979; amended at 3 Ill. Reg. 38, p. 243, effective September 21, 1979; peremptory amendment at3 Ill. Reg. 38, p. 321, effective September 7, 1979; amended at 3 Ill. Reg. 40, p. 140, effectiveOctober 6, 1979; amended at 3 Ill. Reg. 46, p. 36, effective November 2, 1979; amended at 3 Ill.Reg. 47, p. 96, effective November 13, 1979; amended at 3 Ill. Reg. 48, p. 1, effective November15, 1979; peremptory amendment at 4 Ill. Reg. 9, p. 259, effective February 22, 1980; amendedat 4 Ill. Reg. 10, p. 258, effective February 25, 1980; amended at 4 Ill. Reg. 12, p. 551, effectiveMarch 10, 1980; amended at 4 Ill. Reg. 27, p. 387, effective June 24, 1980; emergencyamendment at 4 Ill. Reg. 29, p. 294, effective July 8, 1980, for a maximum of 150 days;amended at 4 Ill. Reg. 37, p. 797, effective September 2, 1980; amended at 4 Ill. Reg. 37, p. 800,effective September 2, 1980; amended at 4 Ill. Reg. 45, p. 134, effective October 27, 1980;amended at 5 Ill. Reg. 766, effective January 2, 1981; amended at 5 Ill. Reg. 1134, effectiveJanuary 26, 1981; peremptory amendment at 5 Ill. Reg. 5722, effective June 1, 1981; amended at5 Ill. Reg. 7071, effective June 23, 1981; amended at 5 Ill. Reg. 7104, effective June 23, 1981;amended at 5 Ill. Reg. 8041, effective July 27, 1981; amended at 5 Ill. Reg. 8052, effective July24, 1981; peremptory amendment at 5 Ill. Reg. 8106, effective August 1, 1981; peremptoryamendment at 5 Ill. Reg. 10062, effective October 1, 1981; peremptory amendment at 5 Ill. Reg.10079, effective October 1, 1981; peremptory amendment at 5 Ill. Reg. 10095, effective October1, 1981; peremptory amendment at 5 Ill. Reg. 10113, effective October 1, 1981; peremptoryamendment at 5 Ill. Reg. 10124, effective October 1, 1981; peremptory amendment at 5 Ill. Reg.10131, effective October 1, 1981; amended at 5 Ill. Reg. 10730, effective October 1, 1981;amended at 5 Ill. Reg. 10733, effective October 1, 1981; amended at 5 Ill. Reg. 10760, effectiveOctober 1, 1981; amended at 5 Ill. Reg. 10767, effective October 1, 1981; peremptoryamendment at 5 Ill. Reg. 11647, effective October 16, 1981; peremptory amendment at 6 Ill.Reg. 611, effective January 1, 1982; amended at 6 Ill. Reg. 1216, effective January 14, 1982;emergency amendment at 6 Ill. Reg. 2447, effective March 1, 1982, for a maximum of 150 days;peremptory amendment at 6 Ill. Reg. 2452, effective February 11, 1982; peremptory amendmentat 6 Ill. Reg. 6475, effective May 18, 1982; peremptory amendment at 6 Ill. Reg. 6912, effectiveMay 20, 1982; emergency amendment at 6 Ill. Reg. 7299, effective June 2, 1982, for a maximumof 150 days; amended at 6 Ill. Reg. 8115, effective July 1, 1982; amended at 6 Ill. Reg. 8142,effective July 1, 1982; amended at 6 Ill. Reg. 8159, effective July 1, 1982; amended at 6 Ill. Reg.10970, effective August 26, 1982; amended at 6 Ill. Reg. 11921, effective September 21, 1982;amended at 6 Ill. Reg. 12293, effective October 1, 1982; amended at 6 Ill. Reg. 12318, effectiveOctober 1, 1982; amended at 6 Ill. Reg. 13754, effective November 1, 1982; amended at 7 Ill.Reg. 394, effective January 1, 1983; codified at 7 Ill. Reg. 6082; amended at 7 Ill. Reg. 8256,effective July 1, l983; amended at 7 Ill. Reg. 8264, effective July 5, l983; amended (by addingSection being codified with no substantive change) at 7 Ill. Reg. 14747; amended (by addingSections being codified with no substantive change) at 7 Ill. Reg. 16108; amended at 8 Ill. Reg.5253, effective April 9, 1984; amended at 8 Ill. Reg. 6770, effective April 27, 1984; amended at8 Ill. Reg. 13328, effective July 16, 1984; amended (by adding Sections being codified with nosubstantive change) at 8 Ill. Reg. 17897; amended at 8 Ill. Reg. 18903, effective September 26,1984; peremptory amendment at 8 Ill. Reg. 20706, effective October 3, 1984; amended at 8 Ill.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>258259260261262263264265266267268269270271272273274275276277278279280281282283284285286287288289290291292293294295296297298299300Reg. 25053, effective December 12, 1984; emergency amendment at 9 Ill. Reg. 830, effectiveJanuary 3, 1985, for a maximum of 150 days; amended at 9 Ill. Reg. 4515, effective March 25,1985; amended at 9 Ill. Reg. 5346, effective April 11, 1985; amended at 9 Ill. Reg. 7153,effective May 6, 1985; amended at 9 Ill. Reg. 11346, effective July 8, 1985; amended at 9 Ill.Reg. 12298, effective July 25, 1985; amended at 9 Ill. Reg. 12823, effective August 9, 1985;amended at 9 Ill. Reg. 15903, effective October 4, 1985; amended at 9 Ill. Reg. 16300, effectiveOctober 10, 1985; amended at 9 Ill. Reg. 16906, effective October 18, 1985; amended at 10 Ill.Reg. 1192, effective January 10, 1986; amended at 10 Ill. Reg. 3033, effective January 23, 1986;amended at 10 Ill. Reg. 4907, effective March 7, 1986; amended at 10 Ill. Reg. 6966, effectiveApril 16, 1986; amended at 10 Ill. Reg. 10688, effective June 3, 1986; amended at 10 Ill. Reg.12672, effective July 14, 1986; amended at 10 Ill. Reg. 15649, effective September 19, 1986;amended at 11 Ill. Reg. 3992, effective February 23, 1987; amended at 11 Ill. Reg. 7652,effective April 15, 1987; amended at 11 Ill. Reg. 8735, effective April 20, 1987; emergencyamendment at 11 Ill. Reg. 12458, effective July 10, 1987, for a maximum of 150 days; amendedat 11 Ill. Reg. 14034, effective August 14, 1987; amended at 11 Ill. Reg. 14763, effective August26, 1987; amended at 11 Ill. Reg. 20142, effective January 1, 1988; amended at 11 Ill. Reg.20898, effective December 14, 1987; amended at 12 Ill. Reg. 904, effective January 1, 1988;amended at 12 Ill. Reg. 3516, effective January 22, 1988; amended at 12 Ill. Reg. 6234, effectiveMarch 22, 1988; amended at 12 Ill. Reg. 8672, effective May 13, 1988; amended at 12 Ill. Reg.9132, effective May 20, 1988; amended at 12 Ill. Reg. 11483, effective June 30, 1988;emergency amendment at 12 Ill. Reg. 11632, effective July 1, 1988, for a maximum of 150 days;emergency amendment at 12 Ill. Reg. 11839, effective July 1, 1988, for a maximum of 150 days;amended at 12 Ill. Reg. 12835, effective July 22, 1988; emergency amendment at 12 Ill. Reg.13243, effective July 29, 1988, for a maximum of 150 days; amended at 12 Ill. Reg. 17867,effective October 30, 1988; amended at 12 Ill. Reg. 19704, effective November 15, 1988;amended at 12 Ill. Reg. 20188, effective November 23, 1988; amended at 13 Ill. Reg. 116,effective January 1, 1989; amended at 13 Ill. Reg. 2081, effective February 3, 1989; amended at13 Ill. Reg. 3908, effective March 10, 1989; emergency amendment at 13 Ill. Reg. 11929,effective June 27, 1989, for a maximum of 150 days; emergency expired November 25, 1989;emergency amendment at 13 Ill. Reg. 12137, effective July 1, 1989, for a maximum of 150 days;amended at 13 Ill. Reg. 15404, effective October 6, 1989; emergency amendment at 13 Ill. Reg.16586, effective October 2, 1989, for a maximum of 150 days; emergency expired March 1,1990; amended at 13 Ill. Reg. 17483, effective October 31, 1989; amended at 13 Ill. Reg. 17838,effective November 8, 1989; amended at 13 Ill. Reg. 18872, effective November 17, 1989;amended at 14 Ill. Reg. 760, effective January 1, 1990; emergency amendment at 14 Ill. Reg.1494, effective January 2, 1990, for a maximum of 150 days; amended at 14 Ill. Reg. 4233,effective March 5, 1990; emergency amendment at 14 Ill. Reg. 5839, effective April 3, 1990, fora maximum of 150 days; amended at 14 Ill. Reg. 6372, effective April 16, 1990; amended at 14Ill. Reg. 7637, effective May 10, 1990; amended at 14 Ill. Reg. 10396, effective June 20, 1990;amended at 14 Ill. Reg. 13227, effective August 6, 1990; amended at 14 Ill. Reg. 14814,effective September 3, 1990; amended at 14 Ill. Reg. 17004, effective September 30, 1990;emergency amendment at 15 Ill. Reg. 348, effective January 1, 1991, for a maximum of 150days; amended at 15 Ill. Reg. 5302, effective April 1, 1991; amended at 15 Ill. Reg. 10101,
<strong>JCAR890120</strong>-<strong>1011664r08</strong>301302303304305306307308309310311312313314315316317318319320321322323324325326327328329330331332333334335336337338339340341342343effective June 24, 1991; amended at 15 Ill. Reg. 11973, effective August 12, 1991; amended at15 Ill. Reg. 12747, effective August 16, 1991; amended at 15 Ill. Reg. 14105, effectiveSeptember 11, 1991; amended at 15 Ill. Reg. 14240, effective September 23, 1991; amended at16 Ill. Reg. 139, effective December 24, 1991; amended at 16 Ill. Reg. 1862, effective January20, 1992; amended at 16 Ill. Reg. 10034, effective June 15, 1992; amended at 16 Ill. Reg. 11582,effective July 15, 1992; amended at 16 Ill. Reg. 17290, effective November 3, 1992; amended at17 Ill. Reg. 1102, effective January 15, 1993; amended at 17 Ill. Reg. 6827, effective April 21,1993; amended at 17 Ill. Reg. 10402, effective June 28, 1993; amended at 18 Ill. Reg. 2051,effective January 21, 1994; amended at 18 Ill. Reg. 5934, effective April 1, 1994; amended at 18Ill. Reg. 8718, effective June 1, 1994; amended at 18 Ill. Reg. 11231, effective July 1, 1994;amended at 19 Ill. Reg. 2905, effective February 27, 1995; emergency amendment at 19 Ill. Reg.9280, effective July 1, 1995, for a maximum of 150 days; amended at 19 Ill. Reg. 11931,effective August 11, 1995; amended at 19 Ill. Reg. 15079, effective October 17, 1995; amendedat 20 Ill. Reg. 5068, effective March 20, 1996; amended at 20 Ill. Reg. 15993, effectiveDecember 9, 1996; emergency amendment at 21 Ill. Reg. 692, effective January 1, 1997, for amaximum of 150 days; amended at 21 Ill. Reg. 7423, effective May 31, 1997; amended at 21 Ill.Reg. 7748, effective June 9, 1997; amended at 21 Ill. Reg. 11555, effective August 1, 1997;amended at 21 Ill. Reg. 13638, effective October 1, 1997; emergency amendment at 22 Ill. Reg.1576, effective January 5, 1998, for a maximum of 150 days; amended at 22 Ill. Reg. 7003,effective April 1, 1998; amended at 22 Ill. Reg. 8503, effective May 1, 1998; amended at 22 Ill.Reg. 16291, effective August 28, 1998; emergency amendment at 22 Ill. Reg. 16640, effectiveSeptember 1, 1998, for a maximum of 150 days; amended at 22 Ill. Reg. 19875, effectiveOctober 30, 1998; amended at 23 Ill. Reg. 2381, effective January 22, 1999; amended at 23 Ill.Reg. 11301, effective August 27, 1999; amended at 24 Ill. Reg. 7361, effective May 1, 2000;emergency amendment at 24 Ill. Reg. 10425, effective July 1, 2000, for a maximum of 150 days;amended at 24 Ill. Reg. 15075, effective October 1, 2000; amended at 24 Ill. Reg. 18309,effective December 1, 2000; amended at 25 Ill. Reg. 8783, effective July 1, 2001; emergencyamendment at 25 Ill. Reg. 10533, effective August 1, 2001, for a maximum of 150 days;amended at 25 Ill. Reg. 16098, effective December 1, 2001; amended at 26 Ill. Reg. 409,effective December 28, 2001; emergency amendment at 26 Ill. Reg. 8583, effective June 1, 2002,for a maximum of 150 days; amended at 26 Ill. Reg. 9843, effective June 26, 2002; emergencyamendment at 26 Ill. Reg. 11029, effective July 1, 2002, for a maximum of 150 days; emergencyamendment at 26 Ill. Reg. 15051, effective October 1, 2002, for a maximum of 150 days;amended at 26 Ill. Reg. 16288, effective October 25, 2002; amended at 27 Ill. Reg. 4708,effective February 25, 2003; emergency amendment at 27 Ill. Reg. 10793, effective July 1, 2003,for a maximum of 150 days; amended at 27 Ill. Reg. 18609, effective November 26, 2003;amended at 28 Ill. Reg. 4701, effective March 3, 2004; amended at 28 Ill. Reg. 6139, effectiveApril 1, 2004; emergency amendment at 28 Ill. Reg. 6610, effective April 19, 2004, for amaximum of 150 days; emergency amendment at 28 Ill. Reg. 7152, effective May 3, 2004, for amaximum of 150 days; amended at 28 Ill. Reg. 11149, effective August 1, 2004; emergencyamendment at 28 Ill. Reg. 12921, effective September 1, 2004, for a maximum of 150 days;amended at 28 Ill. Reg. 13621, effective September 28, 2004; amended at 28 Ill. Reg. 13760,effective October 1, 2004; amended at 28 Ill. Reg. 14541, effective November 1, 2004; amended
<strong>JCAR890120</strong>-<strong>1011664r08</strong>344345346347348349350351352353354355356357358359360361362363364365366367368369370371372373374375376377378379380381382383384385386at 29 Ill. Reg. 820, effective January 1, 2005; amended at 29 Ill. Reg. 10195, effective June 30,2005; amended at 29 Ill. Reg. 14939, effective September 30, 2005; emergency amendment at 30Ill. Reg. 521, effective January 1, 2006, for a maximum of 150 days; amended at 30 Ill. Reg.10314, effective May 26, 2006; emergency amendment at 30 Ill. Reg. 15029, effectiveSeptember 1, 2006, for a maximum of 150 days; amended at 31 Ill. Reg. 2629, effective January28, 2007; emergency amendment at 31 Ill. Reg. 7323, effective May 1, 2007, for a maximum of150 days; amended at 31 Ill. Reg. 11667, effective August 1, 2007; amended at 31 Ill. Reg.12756, effective August 27, 2007; emergency amendment at 31 Ill. Reg. 15854, effectiveNovember 7, 2007, for a maximum of 150 days; emergency rule suspended at 31 Ill. Reg. 16060,effective November 13, 2007; emergency rule repealed, effective May 10, 2008; peremptoryamendment at 32 Ill. Reg. 7212, effective April 21, 2008; peremptory amendment suspended at32 Ill. Reg. 8450, effective May 20, 2008; peremptory amendment repealed under Section 5-125of the Illinois Administrative Procedure Act, effective November 16, 2008; amended at 32 Ill.Reg. 17428, effective November 1, 2008; peremptory amendment at 32 Ill. Reg. 18889, effectiveNovember 18, 2008; peremptory amendment suspended at 32 Ill. Reg. 18906, effectiveNovember 19, 2008; suspension withdrawn by the Joint Committee on Administrative Rules at33 Ill. Reg. 6551, effective April 28, 2009; peremptory amendment repealed by emergencyrulemaking at 33 Ill. Reg. 6712, effective April 28, 2009, for a maximum of 150 days; amendedat 33 Ill. Reg. 1681, effective February 1, 2009; amended at 33 Ill. Reg. 2289, effective March 1,2009; emergency amendment at 33 Ill. Reg. 5802, effective April 2, 2009, for a maximum of 150days; emergency expired August 29, 2009; emergency amendment at 33 Ill. Reg. 10785,effective June 30, 2009, for a maximum of 150 days; amended at 33 Ill. Reg. 12703, effectiveSeptember 7, 2009; amended at 33 Ill. Reg. 15707, effective November 2, 2009; amended at 33Ill. Reg. 17070, effective December 2, 2009; amended at 34 Ill. Reg. 889, effective December30, 2009; emergency rulemaking at 34 Ill. Reg. 13538, effective September 1, 2010, for amaximum of 150 days; amended at 35 Ill. Reg. 379, effective December 27, 2010; amended at35 Ill. Reg. 979, effective January 1, 2011; amended at 35 Ill. Reg. ______, effective____________.SUBPART B: ASSISTANCE STANDARDSSection 120.10 Eligibility forFor Medical Assistancea) Eligibility for medical assistance exists when a personclient meets the nonfinancialrequirements of the program and the person'sclient's countablenonexempt income (Sections 120.330 and 120.360) is equal to or less than theapplicable Medical Assistance − No Grant (MANG) standard and, for AABDMANG, countable nonexempt resourcesassets are not in excess of the applicableresourceasset disregards (Section 120.382120.380). Persons receiving basicmaintenance grants under Article III or IV of the Public Aid Code are eligible formedical assistance. Financial eligibility for medical assistance for other personsliving in the community is determined according to Section 120.60 of this Part,unless otherwise specified. Financial eligibility for medical assistance for persons
<strong>JCAR890120</strong>-<strong>1011664r08</strong>387388389390391392393394395396397398399400401402403404405406407408409410411412413414415416417418419420421422423424425426427428429receiving long-term care services, as defined in Section 120.61(a) of this Part, isdetermined according to that Section, unless otherwise specified.b) For AABD MANG, a person'sthe client's countable income and resourcesassetsinclude the person's countableclient's nonexempt income and resourcesassets andthe countablenonexempt income and resourcesassets of <strong>all</strong> persons included in theMedical Assistance standard. The person'sclient's responsible relativesrelative(s)living with the child must be included in the standard. The personclient has theoption to request that a dependent child under age 18 in the home who is notincluded in the MANG unit be included in the MANG standard.c) For TANF (Temporary Assistance for Needy Families) MANG, a person'stheclient's countable income <strong>includes</strong> the person'sclient's nonexempt income and thenonexempt income of <strong>all</strong> persons included in the Medical Assistance standard.The person'sclient's responsible relativesrelative(s) living with the child must beincluded in the standard. The personclient has the option to request that adependent child under age 18 in the home who is not included in the MANG unitbe included in the MANG standard.d) For AABD MANG, if a person'sthe client's countable nonexempt income isgreater than the applicable MANG standard and/or countable nonexemptresourcesassets are over the applicable resourceasset disregard, the personclientmust meet the spenddown obligation determined for the applicable time periodbefore becoming eligible to receive medical assistance.e) For TANF MANG, if a person'sthe client's countable nonexempt income isgreater than the applicable MANG standard, the personclient must meet thespenddown obligation determined for the applicable time period before becomingeligible to receive medical assistance.f) A one month eligibility period is used for personsclients receiving long-term careservices (as defined in Section 120.61(a) of this Part)in an intermediate carefacility (ICF) or skilled nursing facility (SNF) or in a Department of HumanServices facility. Nonexempt income and nonexempt resourcesassets over theresourceasset disregard are applied toward the cost of care on a monthly basis, asprovided in Section 120.61 of this Part.g) Newborns1) When the Department becomes aware of the birth of a child to a recipientof a TANF or AABD grant or related medical assistance or medicalassistance due to the mother's pregnancy, the child sh<strong>all</strong> be deemed tohave applied for medical assistance only, without written request, if the
<strong>JCAR890120</strong>-<strong>1011664r08</strong>430431432433434435436437438439440441442443444445446447448449450451452453454455456457458459460461462463464465466467468469470471472mother had been receiving TANF or AABD related medical assistance ormedical assistance due to her pregnancy on the date of birth of the child.2) The newborn sh<strong>all</strong> be eligible to receive medical assistance for a period oftime as determined in Section 120.400.(Source: Amended at 35 Ill. Reg. ______, effective ____________)Section 120.20 MANG(AABD) Income Standarda)The monthly countable income standard is 100 percent of the Federal Poverty Level IncomeGuidelines, as published annu<strong>all</strong>y in the Federal Register, for the appropriate family size.b) A client receiving care in a public tuberculosis hospital is not considered to bereceiving long term care. Such a client's financial eligibility for MANG isdetermined by use of the Aid to the Aged, Blind or Disabled MANG(AABD)Income Standard.c) The MANG(AABD) Income Standard is used in the determination of financialeligibility for MANG of a client living in a residential home or facility which isnot licensed as a medical care facility or as a sheltered care facility. The cost ofmaintenance and/or care in such a facility is not an <strong>all</strong>owable medical expense.Regardless of the amount the client may be paying for care and/or maintenance inthe facility, the client's nonexempt income and assets in excess of theMANG(AABD) Standard are considered available for payment for medical carenot provided in the facility.d) MANG1) A recipient residing in a Department of Human Services (DHS) Statepsychiatric hospital or developmental center is <strong>all</strong>owed $30 per month inlieu of any other MANG standard.2) As soon as MANG(AABD) clients become residents of a DHS facility(see subsection (d)(1) of this Section), a skilled nursing facility, anintermediate care facility, or other facility, their eligibility for MANG isdetermined separately from persons remaining in the home.3) When eligibility is based on being temporarily discharged from a DHSfacility (see subsection (d)(1) of this Section) for the purpose of obtainingmedical care in a general hospital, the amount which the recipient isobligated to pay DHS for care and maintenance is to be <strong>all</strong>owed inaddition to the $30.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>4734744754764774784794804814824834844854864874884894904914924934944954964974984995005015025035045055065075085095105115125135145154) Clients in a long term facility are <strong>all</strong>owed deductions from their non-SSIincome to meet the needs of their community spouse, dependent familymembers and dependent children under the age of 21 years who do notreside with the community spouse. Family members include dependentchildren under the age of 21 years, dependent adult children, dependentparents or dependent siblings of either spouse who reside with the spousein the community. To calculate the amount of non-SSI income to bededucted, use the:A) Community Spouse Maintenance Needs Allowance (as describedat Ill. Adm. Code 120.61) if the deduction is for a spouse in thecommunity;B) Family Maintenance Needs Allowance (as described in Ill. Adm.Code 120.61), if the deduction is for dependent family membersresiding with the community spouse; andC) Temporary Assistance for Needy Families (TANF) cash grantstandard if the deduction is for dependent children under the age of21 years who do not reside with the community spouse.(Source: Amended at 35 Ill. Reg. ______, effective ____________)Section 120.40 Exceptions To Use Of MANG Income Standard MANG(AABD) (Repealed)a) An individual receiving long-term care in a licensed group care facility is <strong>all</strong>owed$30 per month in lieu of the MANG standard.b) Spouses sharing a room in a long term care facility, including a DMHDD facilityor other medical care facility are considered residing together, if it is to theiradvantage when determining eligibility. For spouses considered residing together<strong>all</strong>ow sixty dollars ($60) per month for each individual in lieu of the MANGstandard.c) A client 65 years of age and over receiving care in a State mental hospital isconsidered to be receiving long-term care.d) Children under age 21 are considered to be receiving long-term care if they areresiding in one of the following settings:1) Skilled nursing and intermediate care facilities approved for participation.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>5165175185195205215225235245255265275285295305315325335345355365375385395405415425435445455465475485495505515525535545555565575582) Psychiatric hospitals approved for participation.(Source: Repealed at 35 Ill. Reg. ______, effective ____________)SUBPART C: FINANCIAL ELIGIBILITY DETERMINATIONSection 120.60 Community Cases Other Than Long Term Care, Pregnant Women andCertain ChildrenThe following subsections apply to persons or family units who reside in the community orcommunity-based residential facilities or settings (such as a Community Living Facility, SpecialHome Placement, Home Individual Program or Community and Residential Alternatives (59 Ill.Adm. Code 120.10) <strong>all</strong> cases other than those receiving care in licensed intermediate carefacilities, licensed skilled nursing facilities, Department of Human Services (DHS) facilities, orDHS approved community based residential settings under 89 Ill. Adm. Code 140.643, orpregnant women and children under age 19 who do not qualify as mandatory categoric<strong>all</strong>yneedy.a) The eligibility period sh<strong>all</strong> begin with:1) the first day of the month of application;2) the first day of any month, prior to the month of application, in which thepersonclient meets financial and non-financial eligibility requirements upto three months prior to the month of application, if the personclient sodesires; or3) the first day of a month, after the month of application, in which thepersonclient meets non-financial eligibility requirements.b) Eligibility Without Spenddown for MANG1) For MANG AABD MANG, if the person's countableclient's nonexemptincome available during the eligibility period is equal to or below theapplicable MANG AABD income standard (SectionSections 120.20 and120.30) and nonexempt resourcesassets are not in excess of the applicableresourceasset disregard (Section 120.382), the personclient is eligible formedical assistance from the first day of the eligibility period. TheDepartment will pay for covered services received during the entireeligibility period.2) For TANF MANG, if the person's countableclient's nonexempt incomeavailable during the eligibility period is equal to or below the applicable
<strong>JCAR890120</strong>-<strong>1011664r08</strong>559560561562563564565566567568569570571572573574575576577578579580581582583584585586587588589590591592593594595596597598599600601MANG standard (Sections 120.20 and 120.30), the personclient is eligiblefor medical assistance from the first day of the eligibility period. TheDepartment will pay for covered services received during the entireeligibility period.3) The personclient is responsible for reporting any changes that occur duringthe eligibility period thatwhich might affect eligibility for medicalassistance. If changes occur, appropriate action sh<strong>all</strong> be taken by theDepartment, including termination of eligibility for medical assistance. Ifchanges in income, resourcesassets or family composition occur thatwould make the personclient a spenddown case, a spenddown obligationwill be determined and subsection (c) of this Section will apply.4) A redetermination of eligibility will be made at least every 12 months.c) Eligibility with Spenddown for MANG1) For AABD MANG AABD community cases, if the person'scountableclient's nonexempt income available during the applicableeligibility period is greater than the applicable MANG AABD incomestandard and/or nonexempt resourcesassets are over the applicableresourceasset disregard, the personclient must meet the spenddownobligation determined for the eligibility period before becoming eligible toreceive medical assistance. The spenddown obligation is the sum of theamount by which the person's countableclient's nonexempt incomeexceeds the MANG AABD income standard and/orand the amount ofnonexempt resourcesassets in excess of the applicable resourceassetdisregard (see Section 120.384).2) For TANF MANG, if a person's countablethe client's nonexempt incomeavailable during the applicable eligibility period is greater than theapplicable MANG standard (see Sections 120.20 and 120.30 of this Part),the personclient must meet the spenddown obligation determined for theeligibility period before becoming eligible to receive medical assistance.The spenddown obligation is the amount by which the person'scountableclient's nonexempt income exceeds the MANG standard.3) A personThe client meets the spenddown obligation by incurring orpaying for medical expenses in an amount equal to the spenddownobligation. PersonsAABD MANG clients also have the option of meetingtheir income or resource spenddown by paying or having a third-party paythe amount of their spenddown obligation to the Department.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>602603604605606607608609610611612613614615616617618619620621622623624625626627628629630631632633634635636637638639640641642643644A) Incurred expenses are expenses for medical or remedial services:i) recognized under State law;ii) rendered to the person, the person's family, or a financi<strong>all</strong>yresponsible relative;iii) for which the person is liable in the current month forwhich eligibility is being sought or was liable in any of the3-month retroactive eligibility period described insubsection (a) of this Section; andiv) for which no third party is liable in whole or in part unlessthe third party is a State program.B)A) Incurred medicalMedical expenses sh<strong>all</strong> be applied to thespenddown obligation in the following order:i) Expenses for necessary medical or remedial services, asfunded by DHS or the Department on Aging from sourcesother than federal funds. TheSuch expenses sh<strong>all</strong> be basedon the service provider's usual and customary charges tothe public. TheSuch expenses sh<strong>all</strong> not be based on anynominal amount the provider may assess the personclient.These charges are considered incurred the first day of themonth, regardless of the day the services are actu<strong>all</strong>yprovided.ii) Payments made for medical expenses within the previoussix months. Payments are considered incurred the first dayof the month of payment.iii) Unpaid medical expenses. These are considered as of thedate of service and are applied in chronological order.C)B) If multiple medical expenses are incurred on the same day, theexpenses sh<strong>all</strong> be applied in the following order:i) Health insurance deductibles (including Medicare and otherco-insurance charges).ii) All copayment charges incurred or paid on spenddown metday.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>645646647648649650651652653654655656657658659660661662663664665666667668669670671672673674675676677678679680681682683684685686687iii) Expenses for medical services and/or items not covered bythe Department's Medical Assistance Program.iv) Cost share amounts incurred for in-home care services byindividuals receiving services through the Department onAging (DonA).v) Expenses incurred for in-home care services by individualsreceiving or purchasing services from private providers.vi) Expenses incurred for medical services or items covered bythe Department's Medical Assistance Program. If morethan one covered service is received on the day, the chargeswill be considered in order of amount. The bill for thesm<strong>all</strong>est amount will be considered first.D)C) If a service is provided during the eligibility period but paymentmay be made by a third party, such as an insurance company, themedical expense will not be considered towards spenddown untilthe bill is adjudicated. When adjudicated, that part determined tobe the responsibility of the personclient sh<strong>all</strong> be considered asincurred on the date of service.E)D) AABD MANG spenddown personsclients may choose to pay or tohave a third-party pay the amount of their spenddown obligation tothe Department to meet spenddown. The following rules willgovern when personsclients or third parties choose to pay thespenddown:i) Payments to the Department will be applied to thespenddown obligation after <strong>all</strong> other medical expenses havebeen applied per subsections (c)(3)(A), and (B) and (C) ofthis Section.ii) Excess payments will be credited forward to meet thespenddown obligation of a subsequent month for which thepersonclient chooses to meet spenddown.iii) The spenddown obligation may be met using a combinationof medical expenses and amounts paid.4) After application for medical assistance for cases eligible with a
<strong>JCAR890120</strong>-<strong>1011664r08</strong>688689690691692693694695696697698699700701702703704705706707708709710711712713714715716717718719720721722723724725726727728729730spenddown obligation thatwho do not have a QMB or MANG(P) member,an additional eligibility determination will be made.A) For TANF MANG, if countable income is greater than the incomestandard (Section 120.30), and for AABD MANG, if countableincome is greater than the income standard or countableresourcesassets are greater than the resourceasset disregard(Section 120.382(d)), a person will not be enrolled in spenddownunless:i) the person does not have a spenddown obligation for anymonth of the 12-month enrollment period;ii) medical expenses equal the spenddown obligation for atleast one month of the 12-month enrollment period; oriii) the person is on a waiting list or would be on a waiting listto receive a transplant if he or she had a source of payment.B) Cases that meet any of these conditions will be notified, in writing,of the spenddown obligation. The personclient will also benotified that his or her case will be reviewed beginning in the sixthmonth of the 12-month enrollment period. If the personclient hasnot had medical eligibility in one of the last three months at thetime of review (including the month of review), the case willterminate unless the case contains a person who is on a waiting listor who would be on a waiting list to receive a transplant if he orshe had a source of payment. A new application will be required ifthe personclient wishes continued medical assistance.C) When proof of incurred medical expenses equal to the spenddownobligation is provided to the local office, eligibility for medicalassistance sh<strong>all</strong> begin effective the first day that the spenddownobligation is met. The Department will pay for covered servicesreceived from that date until the end of the eligibility period. Thepersonclient sh<strong>all</strong> be responsible, directly to the provider, forpayment for services provided prior to the time the personclientmeets the spenddown obligation.5) Cases with a spenddown obligation that do not have a QMB, a MANG(P)member or a person on a waiting list or who would be on a waiting list toreceive a transplant if he or she had a source of payment, will be reviewedbeginning in the sixth month of enrollment to determine if they have had
<strong>JCAR890120</strong>-<strong>1011664r08</strong>731732733734735736737738739740741742743744745746747748749750751752753754755756757758759760761762763764765766767768769770771772773medical eligibility within the last three months, including the month ofreview. If so, enrollment will continue. If not, enrollment will beterminated and the personclient will be advised that if he or she wishescontinued medical assistance, a reapplication must be filed. Uponreapplication, a new 12-month enrollment period will be established(assuming non-financial factors of eligibility are met). If appropriate, anew spenddown obligation will be created.A) If the personclient files a reapplication prior to four months afterthe end of the period of enrollment, the personclient will be sentthrough a special abbreviated intake procedure making use ofcurrent case record material to verify factors of eligibility notsubject to change.B) Cases that remain eligible in the tenth month of the enrollmentperiod or that have a QMB, a MANG(P) member or a person on awaiting list or who would be on a waiting list to receive atransplant if he or she had a source of payment, will remainenrolled and will be redetermined once every 12 months.6) The personclient is responsible for reporting any changes that occur duringthe enrollment period that might affect eligibility for medical assistance.If changes occur, appropriate action sh<strong>all</strong> be taken by the Department,including termination of eligibility for medical assistance.7) For AABD MANG AABD, if changes in income, resourcesassets orfamily composition occur, appropriate adjustments to the spenddownobligation and date of eligibility for medical assistance sh<strong>all</strong> be made bythe Department. The personclient will be notified, in writing, of the newspenddown obligation.A) If income decreases, or resourcesassets f<strong>all</strong> below the applicableresourceasset disregard and, as a result, the personclient hasalready met the new spenddown obligation, eligibility for medicalassistance sh<strong>all</strong> be backdated to the appropriate date.B) If income or resourcesassets increase and, as a result, thepersonclient has not produced proof of incurred medical expensesequal to the new spenddown obligation, the written notification ofthe new spenddown amount will also inform the personclient thateligibility for medical assistance will be interrupted until proof ofmedical expenses equal to the new spenddown obligation isproduced.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>7747757767777787797807817827837847857867877887897907917927937947957967977987998008018028038048058068078088098108118128138148158168) For TANF MANG, if changes in income or family composition occur,appropriate adjustments to the spenddown obligation and date ofeligibility for medical assistance sh<strong>all</strong> be made by the Department. Thepersonclient will be notified, in writing, of the new spenddown obligation.A) If income decreases and, as a result, the personclient has alreadymet the new spenddown obligation, eligibility for medicalassistance sh<strong>all</strong> be backdated to the appropriate date.B) If income increases and, as a result, the personclient has notproduced proof of incurred medical expenses equal to the newspenddown obligation, the written notification of the newspenddown amount will also inform the personclient that eligibilityfor medical assistance will be interrupted until proof of medicalexpenses equal to the new spenddown obligation is produced.9) Reconciliation of Amounts Paid-in to Meet SpenddownA) The Department will reconcile payments received to meet anincome spenddown obligation for a given month against theamount of claims paid for services received in that month andrefund any excess spenddown paid to the personclient. Excessamounts paid for a calendar month will be determined andrefunded to the personclient six calendar quarters later. Refundpayments will be made once per quarter.B) The Department will reconcile payments received to meet aresourcean asset spenddown obligation against the amount of <strong>all</strong>claims paid during the individual's period of enrollment formedical assistance. Excess amounts paid will be determined andrefunded to the individual six calendar quarters after theindividual's enrollment for medical assistance ends.C) When payments are received to meet both a resourcean asset andan income spenddown obligation, the Department will firstreconcile the amount of claims paid to amounts paid toward theresourceasset spenddown. If the total amount of claims paid havenot met or exceeded the amount paid to meet the resourceassetspenddown by the time the individual's enrollment ends, the excessresourceasset payments sh<strong>all</strong> be handled per subsection(c)(3)(C)(B) of this Section. Once the amount of claims paidequals or exceeds the amount paid toward the resourceasset
<strong>JCAR890120</strong>-<strong>1011664r08</strong>817818819820821822823824825826827828829830831832833834835836837838839840841842843844845846847848849850851852853854855856857858859spenddown, the remaining amount of claims paid will be comparedagainst the amount paid to meet the income spenddown persubsection (c)(3)(B)(A) of this Section.10) The Department will refund payment amounts received for any months inwhich the personclient is no longer in spenddown status and the paymentcannot be used to meet a spenddown obligation. These payment amountssh<strong>all</strong> not be subject to reconciliation under subsection (c)(9) of thisSection. Refunds sh<strong>all</strong> be processed within six months after the casestatus changed.(Source: Amended at 35 Ill. Reg. ______, effective ____________)Section 120.61 Long Term CareCases in Intermediate Care, Skilled Nursing Care andDMHDD-MANG (AABD) and All Other Licensed Medical Facilities<strong>This</strong> Section applies to persons residing in long term care facilities or State-certified, Statelicensed,or State-contracted residential care programs who, as a condition of eligibility formedical assistance, are required to pay <strong>all</strong> of their income, less certain protected amounts, for thecost of their own care.a) The term "long term care facility" refers to:1) an institution (or a distinct part of an institution) that meets the definitionof a "nursing facility" as that term is defined in 42 USC 1396r;2) licensed Intermediate Care Facilities (ICF and ICF/DD), licensed SkilledNursing Facilities (SNF and SNF/Ped) and licensed hospital-based longterm care facilities (see 89 Ill. Adm. Code 148.50(c)); and3) Supportive Living Facilities (SLF) and Community Integrated LivingFacilities (CILA).The policy set forth in subsections (b), (c), (d) and (e)below applies to cases receiving care in Licensed Intermediate CareFacilities, Licensed Skilled Nursing Facilities, or Department of MentalHealth and Developmental Disabilities (DMHDD) Facilities. The policyset forth in subsection (f) below applies to cases receiving care in LicensedIntermediate Care Facilities, Licensed Skilled Nursing Facilities, DMHDDFacilities and <strong>all</strong> other Licensed Medical Facilities (see 89 Ill. Adm. Code140.642).b) The eligibility period sh<strong>all</strong> begin with:Treatment of Resources1) the first day of the month of application;
<strong>JCAR890120</strong>-<strong>1011664r08</strong>8608618628638648658668678688698708718728738748758768778788798808818828838848858868878888898908918928938948958968978988999009019022) up to three months prior to the month of application for any month inwhich the person meets both financial and non-financial eligibilityrequirements. Eligibility will be effective the first day of a retroactivemonth if the person meets eligibility requirements at any time during thatmonth; or3) the first day of a month, after the month of application, in which theperson meets non-financial and financial eligibility requirements.c) Eligibility Without Spenddown1) A one-month eligibility period will be used. If a person's nonexemptincome available during the eligibility period is equal to or below theapplicable income standard and nonexempt resources are not in excess ofthe applicable resource disregard (see Section 120.382 of this Part), theperson is eligible for medical assistance from the first day of the eligibilityperiod without a spenddown. All nonexempt income and non-exemptassets over the applicable asset disregard (Section 120.382) sh<strong>all</strong> beapplied towards the cost of care on a monthly basis. Non-exempt income(see Section 120.360) and assets (see 120.381) are applied towards thecost of care beginning with the first full calendar month of anticipated stayin the facility. Non-exempt income sh<strong>all</strong> be applied toward the cost of carefirst. If insufficient to meet the cost of care at the private pay rate, thennon-exempt assets over the applicable asset disregard sh<strong>all</strong> be used.2) A person eligible under this subsection (c) is responsible for reporting anychanges that occur during the eligibility period that might affect eligibilityfor medical assistance. If changes occur, appropriate action sh<strong>all</strong> be takenby the Department, including termination of eligibility for medicalassistance. If changes in income, resources or family composition occurthat would make the person a spenddown case, a spenddown obligationwill be determined and subsection (d) of this Section will apply. When aclient transfers between non-DMHDD facilities or transfers to a DMHDDfacility, non-exempt income and/or excess assets are applied first towardthe cost of care at the first facility and any balance is applied toward thecost of care at the second facility. If the client transfers from a DMHDDfacility to a non-DMHDD facility, non-exempt income and/or excessassets are not applied toward the cost of care at the non-DMHDD facilityfor the month the transfer occurs. If the client is discharged from aDMHDD facility or non-DMHDD facility to his/her residence in thecommunity or to a community based residential setting (such asCommunity Living Facility, Special Home Placement, Supported Living
903904905906907908909910911912913914915916917918919920921922923924925926927928929930931932933934935936937938939940941942943944945d)c)<strong>JCAR890120</strong>-<strong>1011664r08</strong>Arrangement, Home Individual Program, Community ResidentialAlternatives as defined at 59 Ill. Adm. Code 120.10), the MANGCommunity Income Standard is used (see Section 120.20) beginning withthe month of discharge from the DMHDD facility or non-DMHDD. 3)Ifnon-exempt income and non-exempt assets over the applicable assetdisregard are greater than the Department's rate for cost of care, nopayment will be made to the facility. However, the client may becomeeligible for Medical Assistance for other medical expenses by incurringmedical expenses equal to the spend-down obligation. The private rate ofthe facility may be applied to the spend-down obligation in this instance.A full redetermination of eligibility sh<strong>all</strong> be made at least every 12twelve(12) months.Eligibility with SpenddownAllow a deduction from the MANG client's income tomeet the needs of dependent children under age 21 who do not reside with thecommunity spouse, who do not have enough income to meet their needs andwhose assets do not exceed the asset limit. To determine needs and asset limits:1) If countable income available during the eligibility period exceeds theapplicable income standard and/or nonexempt resources exceed theapplicable resource disregard, a person has a spenddown obligation thatmust be met before financial eligibility for medical assistance can beestablished. The spenddown obligation is the amount by which theperson's countable income exceeds the applicable income standard ornonexempt resources exceed the applicable resource disregard. fordependent children, use AFDC MAG standard and asset disregard (seeSections 120.30 and 120.382).2) A person meets the spenddown obligation by incurring or paying formedical expenses in an amount equal to the spenddown obligation.Medical expenses sh<strong>all</strong> be applied to the spenddown obligation asprovided in Section 120.60(c) of this Part.<strong>all</strong>ow any payments made onmedical bills for the children.3) Projected expenses for services provided by a long term care facility thathave not yet been incurred, but are reasonably expected to be, may also beused to meet a spenddown obligation. The amount of the projectedexpenses is based on the private pay rate of the long term care facility atwhich the person resides or is seeking admission.4) A person who has both an income spenddown and a resource spenddowncannot apply the same incurred medical benefits to both. Incurred medicalexpenses are first applied to an income spenddown.
946947948949950951952953954955956957958959960961962963964965966967968969970971972973974975976977978979980981982983984985986987e)d)f)e)<strong>JCAR890120</strong>-<strong>1011664r08</strong>Post-eligibility Treatment of Income. If non-financial and financial eligibility isestablished, a person's total income, including income exempt and disregarded indetermining eligibility, must be applied to the cost of the person's care, minus anyapplicable deductions provided under subsection (f) of this Section. Allowdeductions from the MANG clients non-SSI income for a Community SpouseMaintenance Needs Allowance and a Family Maintenance Needs Allowance foreach dependent family member who does not have enough income to meet his/herneeds. Family members include dependent children under age 21, dependentadult children, dependent parents or dependent siblings of either spouse who areliving with the community spouse. To determine the amount of the deduction:1) The deduction for the Community Spouse Maintenance Needs Allowance,as of October 1, 1989, is equal to the community spouse maintenanceneeds standard ($1,500) less any non-exempt monthly income of thecommunity spouse. The amount established as the community spousemaintenance needs standard sh<strong>all</strong> be increased for calendar years after1989 by the same percentage as the percentage increase in the consumerprice index for <strong>all</strong> urban consumers. The deduction is <strong>all</strong>owed only to theextent income of the institutionalized spouse is contributed to thecommunity spouse. However, the deduction for the Community SpouseMaintenance Needs Allowance sh<strong>all</strong> not be less than the amount orderedby the court for support of the community spouse or the amountdetermined as the result of the fair hearing.2) The deduction for the Family Maintenance Needs Allowance for eachdependent family member is equal to one-third of the difference betweenthe family maintenance needs standard (122% of the Federal PovertyLevel for two persons as of September 30, 1989, 133% as of July 1, 1991,and 150% as of July 1, 1992) and any non-exempt income of the familymember.Post-eligibility Income Deductions. From a person's total income that is payablefor a person's care, certain deductions are <strong>all</strong>owed. Allowed deductions sh<strong>all</strong>increase the amount paid by the Department for residential services on behalf ofthe person, up to the Department's payment rate for the facility. Deductions sh<strong>all</strong>be <strong>all</strong>owed for the following amounts in the following order:1) SSI benefits paid under 42 USC 1382(e)(1)(E) or (G) and, for residents ofSupportive Living Facilities, the minimum current SSI payment standardfor an individual (or a couple, if spouses reside together), less the personalneeds <strong>all</strong>owance specified in subsection (f)(2)(C) of this Section, sh<strong>all</strong> be
<strong>JCAR890120</strong>-<strong>1011664r08</strong>9889899909919929939949959969979989991000100110021003100410051006100710081009101010111012101310141015101610171018101910201021102210231024102510261027102810291030deducted for room and board charges (see 89 Ill. Adm. Code 146.225(c)and (d));2) a personal needs <strong>all</strong>owance:A) for persons other than those specified in subsections (f)(2)(B)through (E), $30 per month;B) for spouses residing together, $60 per couple per month ($30 perspouse);C) for persons or spouses residing in Supportive Living Facilities,$90;D) for persons residing in Community Integrated LivingArrangements (see 59 Ill. Adm. Code 115), $50; orE) for veterans who have neither a spouse nor dependent child, orsurviving spouses of veterans who do not have a dependent child,and whose monthly veterans' benefits are reduced to $90, a $90income disregard is <strong>all</strong>owed in lieu of a personal <strong>all</strong>owancededuction. Persons <strong>all</strong>owed the $90 per month income disregardare not also permitted the $30 per month personal <strong>all</strong>owance;3) a community spouse income <strong>all</strong>owance pursuant to Section 120.379(e) ofthis Part;4) a family <strong>all</strong>owance pursuant to Section 120.379(e)(2) of this Part;5) an amount to meet the needs of qualifying children (as defined in 26 USC152) under age 21 who do not reside with either parent, who do not haveenough income to meet their needs and whose resources do not exceed theresource limit. To determine needs and resource limits:A) the MANG(C) and applicable resource disregard are used (seeSections 120.30 and 120.382 of this Part); andB) any payments made on medical bills for the children can bededucted from the person's income;6) amounts for incurred expenses for certain Medicare and health insurancecost sharing that are not subject to payment by a third party, limited to:
<strong>JCAR890120</strong>-<strong>1011664r08</strong>1031103210331034103510361037103810391040104110421043104410451046104710481049105010511052105310541055105610571058105910601061106210631064106510661067106810691070107110721073A) Medicare premiums, deductibles, or coinsurance charges not paidby Medicaid or another third party payor;B) Other health insurance premiums, deductibles or coinsurance (costsharing) charges provided the insurance meets the definition of a"health benefit plan" and is approved for providing that insurancein Illinois by the Illinois Department of Insurance.i) "Health benefit plan" means any accident and healthinsurance policy or certificate, health services plancontract, health maintenance organization subscribercontract, plan provided by a MEWA (Multiple EmployerWelfare Arrangement) or plan provided by another benefitarrangement.ii) Health benefit plan does not mean accident only, credit, ordisability insurance; long-term care insurance (except forthe month of admission to a long term care facility); dentalonly or vision only insurance; specified disease insurance;hospital confinement indemnity coverage; limited benefithealth coverage; coverage issued as a supplement toliability insurance; insurance arising out of a workers'compensation or similar law; automobile medical paymentinsurance; or insurance under which benefits are payablewith or without regard to fault and that is statutorilyrequired to be contained in any liability insurance policy orequivalent self-insurance;7) Expenses Not Subject to Third Party Payment for Necessary Medical CareRecognized under State Law, but Not a Covered Service under theMedical Assistance Program. "Necessary medical care" has the meaningdescribed in 215 ILCS 105/2 and must be proved as such by aprescription, referral or statement from the patient's doctor or dentist. Thefollowing are <strong>all</strong>owable deductions from a person's post-eligibility incomefor medic<strong>all</strong>y necessary services:A) expenses incurred within the six months prior to the month of anapplication, provided those expenses remain a current liability tothe person and were not used to meet a spenddown. Medicalexpenses incurred during a period of ineligibility resulting from apenalty imposed under Section 120.387 or 120.388 of this Part arenot an <strong>all</strong>owable deduction;
<strong>JCAR890120</strong>-<strong>1011664r08</strong>1074107510761077107810791080108110821083108410851086108710881089109010911092109310941095109610971098109911001101110211031104110511061107110811091110111111121113111411151116B) expenses incurred for necessary medical services from a medicalprovider (subject to reasonable dollar limits on specific services)so long as the provider was not terminated, barred or suspendedfrom participation in the Medical Assistance Program (pursuant to89 Ill. Adm. Code 140.16, 140.17 or 140.18) at the time themedical services were provided; andC) expenses for long term care services, subject to the limitations ofthis subsection (f)(7) and provided that the services were notprovided by a facility to a person admitted during a time thefacility was subject to the sanction of non-payment for newadmissions (see 305 ILCS 5/12-4.25(I)(3));8) Amounts to maintain a residence in the community for up to six monthswhen:A) the person does not have a spouse and/or dependent children in thehome;B) a physician has certified that the stay in the facility is temporaryand the individual is expected to return home within six months;C) the amount of the deduction is based on:i) the rent or property expense <strong>all</strong>owed under the AABDMAG standard if the person was at home (see 89 Ill. Adm.Code 113.248); andii) the utility expenses that would be <strong>all</strong>owed under the AABDMAG standard if the person was at home (see 89 Ill. Adm.Code 113.249).Allow a $90.00 per month income disregard for veterans, who have neitherspouse nor dependent child, or surviving spouses, who do not have a dependentchild, who reside in long term care facilities who receive reduced monthlyveterans benefits in the amount of $90.00. Persons <strong>all</strong>owed the $90.00 per monthincome disregard are not also permitted the $30.00 per month personal <strong>all</strong>owance(see Section 120.40).f) Deduction from MANG program1) A deduction from the MANG program participant's income sh<strong>all</strong> bepermitted for up to six months to maintain a residence in the community
<strong>JCAR890120</strong>-<strong>1011664r08</strong>1117111811191120112111221123112411251126112711281129113011311132113311341135113611371138113911401141114211431144114511461147114811491150115111521153115411551156115711581159when:A) the individual does not have a spouse and/or dependent children inthe home; andB) a physician has certified that the stay in the facility is temporaryand the individual is expected to return home within six months.2) To determine the amount of the deduction include:A) rent or property expense that would be <strong>all</strong>owed in the AABDMAG standard if the individual was at home; andB) utility expenses that would be <strong>all</strong>owed in the AABD MAGstandard if the individual was at home.(Source: Amended at 35 Ill. Reg. ______, effective ____________)Section l20.62 Department of Mental Health and Developmental Disabilities (DMHDD)Approved Home and Community Based Residential Settings Under 89 Ill. Adm. Code140.643 (Repealed)a) Community-based Residential Settings1) The following rule applies to individuals receiving in-home care servicesthrough the Department of Mental Health and Developmental Disabilities(DMHDD) in accord with 89 Ill. Adm. Code 140.643. The in-home careservices are provided in the following community based residentialsettings.A) Community Living Facilities (CLF)B) Special Home Placements (SHP)C) Supported Living Arrangement (SLA)D) Home Individual Program (HIP)E) Community Residential Alternatives (CRA)2) A definition of the above quoted Home and Community based residentialsettings as well as a description of the Title XIX waiver services can befound at 59 Ill. Adm. Code 120.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>1160116111621163116411651166116711681169117011711172117311741175117611771178117911801181118211831184118511861187118811891190119111921193119411951196119711981199120012011202b) A one-month eligibility period will be used. Eligibility begins the first day of theeligibility period or the day during the month that spend-down is met.c) A one-person MANG Community Income Standard will be used (see Section120.20).d) The client sh<strong>all</strong> be <strong>all</strong>owed an asset disregard in the amount for one client inaccord with Section 120.382. Assets are considered in accord with 89 Ill. Adm.Code 113.140, 113.141, 113.142 and 113.154.e) If the client has SSI income, the SSI income will be applied by DMHDD towardthe cost of room and board. However, no payment will be made by theDepartment for the cost of room and board. The client sh<strong>all</strong> be responsibledirectly to DMHDD for payment of room and board costs.f) If the client's non-exempt income is greater than the MANG standard and/or nonexemptassets are over the applicable asset disregard, the client must meet thespend-down obligation determined for the eligibility period before becomingeligible to receive Medical Assistance. The spend-down obligation is the sum ofthe amount by which the client's non-exempt income exceeds the MANG standardand the amount of non-exempt assets in excess of the applicable asset disregard.g) The client may meet the spend-down by incurring Title XIX waiver (in-homecare) services. Waiver services are considered incurred in total for the month onthe first day of the month or the first day of stay for a month that the client residesin the approved residential setting if for less than an entire month. If the cost ofwaiver services equals or exceeds the spend-down amount, the spend-downobligation is met. DMHDD will provide the local office a statement of expectedmonthly charges for waiver services to ensure that the spend-down obligation ismet.h) If the client's non-exempt income is equal to or less than the MANG Standard andnon-exempt assets are not in excess of the applicable asset disregard, the client iseligible for medical assistance from the first day of the eligibility period.i) If the client's non-exempt income exceeds the MANG Standard and/or nonexemptassets are over the applicable asset disregard, eligibility for medicalassistance sh<strong>all</strong> begin effective the first day that the spend-down obligation is met.The Department will pay for covered services less the client's liability (excludingTitle XIX waiver services) received from the date the spend-down obligation ismet date until the end of the eligibility period. The client sh<strong>all</strong> be responsibledirectly to the provider for payment for services provided prior to the time client
<strong>JCAR890120</strong>-<strong>1011664r08</strong>1203120412051206120712081209121012111212121312141215121612171218121912201221122212231224122512261227122812291230123112321233123412351236123712381239124012411242124312441245meets the spend-down obligation.j) A new application and/or a redetermination of eligibility will not be required foreligible clients who move from an institutional setting to an approved Home andCommunity based residential setting.k) A case review is required for eligible cases placed in an approved residentialsetting.l) A full redetermination of eligibility sh<strong>all</strong> be made every twelve months.(Source: Repealed at 35 Ill. Reg. ______, effective ____________)Section 120.63 Department of Mental Health and Developmental Disabilities (DMHDD)Approved Home and Community Based Residential Settings (Repealed)a) In-Home Care Services1) <strong>This</strong> Section applies to individuals receiving remedial care servicesthrough the Department of Mental Health and Developmental Disabilities(DMHDD) in Home and Community Based Residential Settings approvedby DMHDD. Remedial care services are those services (except for roomand board) provided by DMHDD that are directed toward meeting theneeds of disabled clients who are not receiving services through theDepartment's In-Home Care Program (see Section 120.62). The remedialcare services are provided in the following Home and Community BasedResidential Settings:A) Community Living Facilities (CLF)B) Special Home Placements (SHP)C) Supported Living Arrangement (SLA)D) Home Individual Program (HIP)E) Community Residential Alternatives (CRA)2) A definition of the Home and Community Based Residential Settings canbe found at 59 Ill. Adm. Code 120.b) A one-month eligibility period will be used. Eligibility begins the first day of theeligibility period or the day during the month that spend-down is met.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>1246124712481249125012511252125312541255125612571258125912601261126212631264126512661267126812691270127112721273127412751276127712781279128012811282128312841285128612871288c) A one-person MANG Community Income Standard will be used (see Section120.20).d) The client sh<strong>all</strong> be <strong>all</strong>owed an asset disregard in the amount for one client inaccord with Section 120.382. Assets are considered in accord with 89 Ill. Adm.Code 113.140, 113.141, 113.142 and 113.154.e) If the client has SSI income, the SSI income will be applied by DMHDD towardthe cost of room and board. The client sh<strong>all</strong> be responsible directly to DMHDDfor payment of room and board costs. No payment will be made by theDepartment for the cost of room and board.f) If the client's non-exempt income is greater than the MANG Standard and/or nonexemptassets are over the applicable asset disregard, the client must meet thespend-down obligation determined for the eligibility period before becomingeligible to receive medical assistance. The spend-down obligation is the sum ofamount by which the client's non-exempt income exceeds the MANG Standardand the amount on non-exempt assets in excess of the applicable asset disregard.g) The client may meet the spend-down by incurring costs for remedial careservices. Remedial care costs are the cost of <strong>all</strong> services reported by DMHDDthat exceed the MANG Community Income Standard and the Income Disregardamount. Remedial care services are considered incurred in total for the month onthe first day of the month or the first day of stay for a month that the client residesin the approved residential setting if for less than an entire month. If the cost ofremedial care services equal or exceeds the spend-down amount, the spend-downobligation is met. DMHDD will provide the local office a statement of expectedmonthly charges for remedial care services to ensure that the spend-downobligation is met.h) If the client's non-exempt income is equal to or less than the MANG Standard andnon-exempt assets are not in excess of the applicable asset disregard, the client iseligible for medical assistance from the first day of the eligibility period.i) If the client's non-exempt income exceeds the MANG Standard and/or nonexemptassets are over the applicable asset disregard, eligibility for medicalassistance sh<strong>all</strong> begin effective the first day that the spend-down obligation is met.Covered services, less the client's liability, received from the spend-down metdate until the end of the eligibility period will be paid for by the Department. Theclient sh<strong>all</strong> be responsible directly to the provider for payment for servicesprovided prior to the time client meets the spend-down obligation.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>1289129012911292129312941295129612971298129913001301130213031304130513061307130813091310131113121313131413151316131713181319132013211322132313241325132613271328132913301331j) A new application and/or a redetermination of eligibility will not be required foreligible clients who move from an institutional setting to an approved Home andCommunity Based Residential Setting.k) A case review is required for eligible cases placed in an approved Home andCommunity Based Residential Setting.l) A full redetermination of eligibility sh<strong>all</strong> be made every twelve months.(Source: Repealed at 35 Ill. Reg. ______, effective ____________)Section 120.65 Department of Mental Health and Developmental Disabilities (DMHDD)Licensed Community-Integrated Living Arrangements (Repealed)a) Community-Integrated Living Arrangement (CILA) Services1) <strong>This</strong> Section applies to individuals receiving CILA services through anagency licensed by DMHDD. CILA services are provided in approvedsettings where eight or fewer individuals with mental retardation (MR) ormental illness (MI) reside under the supervision of the agency licensed byDMHDD. Individuals actively participate in choosing services designedto provide treatment, habilitation, training, rehabilitation and othercommunity integrative supports and in choosing a home from among thoseliving arrangements available to the general public and/or housing ownedor leased by an agency licensed by DMHDD.2) The standards and licensure requirements for community-integrated livingarrangements are found at 59 Ill. Adm. Code 115.b) A one-month eligibility period will be used. Eligibility begins the first day of theeligibility period or the day during the month that spend-down is met.c) The appropriate MANG Community Income Standard will be used (see Section120.20).d) The individual sh<strong>all</strong> be <strong>all</strong>owed an asset disregard in accordance with Section120.382. Assets are considered in accordance with 89 Ill. Adm. Code 113.140,113.141 and 113.142.e) No payment will be made by the Department for the cost of room and board. Theindividual sh<strong>all</strong> be responsible directly to the agency licensed by DMHDD forpayment of any room and board costs.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>1332133313341335133613371338133913401341134213431344134513461347134813491350135113521353135413551356135713581359136013611362136313641365136613671368136913701371137213731374f) If non-exempt income is greater than the MANG Standard and/or non-exemptassets are over the applicable asset disregard, the client must meet the spenddowndetermined for the eligibility period before becoming eligible to receivemedical assistance. The spend-down is the sum of the amount by which theclient's non-exempt income exceeds the MANG standard and the amount of nonexemptassets in excess of the applicable asset disregard.g) The client may meet the spend-down by incurring costs for CILA services. CILAservices are considered incurred in total for the month on the first day of themonth or the first day services are received if for less than an entire month. If thecost of CILA services equals or exceeds the spend-down amount, the spend-downis met. DMHDD will provide the local office with a statement of expectedmonthly charges for CILA services to ensure that the spend-down obligation ismet.h) If non-exempt income is equal to or less than the MANG Standard and nonexemptassets are not in excess of the applicable asset disregard, the client iseligible for medical assistance from the first day of the eligibility period.i) If non-exempt income exceeds the MANG Standard and/or non-exempt assets areover the applicable asset disregard, eligibility for medical assistance sh<strong>all</strong> begineffective the first day that the spend-down obligation is met. Covered services,less the client's liability, received from the spend-down met date until the end ofthe eligibility period will be paid for by the Department. The client sh<strong>all</strong> beresponsible directly to the provider for payment for services provided prior to thetime the client meets spend-down.j) A new application and/or a redetermination of eligibility will not be required foreligible clients who move from an institutional setting to an approved setting inwhich CILA services are received.k) A full redetermination of eligibility sh<strong>all</strong> be made every twelve months.(Source: Repealed at 35 Ill. Reg. ______, effective ____________)SUBPART H: MEDICAL ASSISTANCE – NO GRANT (MANG) ELIGIBILITY FACTORSSection 120.308 Client Cooperationa) As a condition of eligibility, clients must cooperate:1) in the determination of eligibility;
<strong>JCAR890120</strong>-<strong>1011664r08</strong>13751376137713781379138013811382138313841385138613871388138913901391139213931394139513961397139813991400140114021403140414051406140714081409141014111412141314141415141614172) with Department programs conducted for the purposes of acquisition orverification of information upon which eligibility may depend; and3) in applying for <strong>all</strong> financial benefits for which they may qualify and toavail themselves of thosesuch benefits at the earliest possible date.b) Clients are required to avail themselves of <strong>all</strong> potential income and resources andto take appropriate action to receive such resources, including those describedunder Section 120.388(d)(2) of this Part.c) When eligibility cannot be conclusively determined because the individual isunwilling or fails to provide essential information or to consent to verification, theclient is ineligible.d) At screening, applicants sh<strong>all</strong> be informed, in writing, of any information they areto provide at the eligibility interview.e) At the eligibility interview or at any time during the application process, when theapplicant is requested to provide information in his or her possession, theDepartment will <strong>all</strong>ow 10ten (10) days for the return of the requested information.The first day of the 10ten (10) day period is the calendar day following the datethe information request form is sent or given to the applicant. The last day of the10ten (10) day period sh<strong>all</strong> be a work day and is to be indicated on theinformation request form. If the applicant does not provide the information by thedate on the information request form, the application sh<strong>all</strong> be denied on thefollowing work day.f) At the eligibility interview or at any time during the application process, when theapplicant is requested to provide third party information, the Department sh<strong>all</strong><strong>all</strong>ow 10 calendarten (10) days for the return of the requested information or forverification that the third party information has been requested. The first day ofthe 10ten (10) day period is the calendar day following the date the informationrequest form is sent or given to the applicant. The last day of the 10ten (10) dayperiod sh<strong>all</strong> be a work day and willis to be indicated on the information requestform. It is to be indicated on the information request form that the applicant sh<strong>all</strong>provide written verification of the request for the third party information. If theapplicant does not provide the information or the verification that the informationwas requested by the date on the information request form, the application sh<strong>all</strong>be denied on the following work day.1) Third party information is defined as information thatwhich must beprovided by someone other than the applicant. An authorizedrepresentative or person applying on another's behalf is not a third party,
<strong>JCAR890120</strong>-<strong>1011664r08</strong>1418141914201421142214231424142514261427142814291430143114321433143414351436143714381439144014411442144314441445144614471448144914501451145214531454145514561457145814591460but is treated as if he or she were the applicant.2) The Department sh<strong>all</strong> advise clients of the need to provide writtenverification of third party information requests and the consequences offailing to provide thatsuch verification.3) If the applicant requests an extension either verb<strong>all</strong>y or in writing in orderto obtain third party information and provides written verification of therequest for the third party information, such as a copy of the request thatwas sent to the third party, an extension of forty-five (45) days from thedate of application sh<strong>all</strong> be granted. The first day of the forty-five (45) dayperiod is the calendar day following the date of application. The 45 th daymust be a work day.4) If an applicant's attempt to obtain third party information is unsuccessful,upon the applicant's request, the Department will assist in securingevidence to support the client's eligibility for assistance.g) Any information or verifications requested under this Section must be returned tothe Department's or its agent's office in the manner indicated on the informationrequest form. Information mailed or otherwise delivered to an address notindicated on the form will not toll the timeframes for providing information underthis Section.h) Failure to cooperate in the determination of eligibility under this Section,including failure to provide requested information or verifications, is a basis forthe denial of an application for benefits. A person has the right to appeal such adenial under 89 Ill. Adm. Code 102.80. The Department sh<strong>all</strong> not deny anapplication if third party information cannot be timely obtained when the delay isbeyond the control of the person and a timely request was made to the third partyfor the information. The Department sh<strong>all</strong> not deny an application for failure totimely provide information in the applicant's possession if the person has made agood faith attempt to retrieve the information and is unable, due to incapacity,illness, family emergency or other just cause, to do so.(Source: Amended at 35 Ill. Reg. ______, effective ____________)Section 120.347 Treatment of Trusts and Annuitiesa) <strong>This</strong> Section applies to trusts established on or after August 11, 1993.b) A trust is any arrangement in which a grantor transfers property to a trustee ortrustees with the intention that it be held, managed or administered by the trustee
<strong>JCAR890120</strong>-<strong>1011664r08</strong>1461146214631464146514661467146814691470147114721473147414751476147714781479148014811482148314841485148614871488148914901491149214931494149514961497149814991500150115021503or trustees for the benefit of the grantor or designated beneficiaries. A trust also<strong>includes</strong> any legal instrument or device that is similar to a trust, including anannuity.c) A person sh<strong>all</strong> be considered to have established a trust if resourcesassets of theperson were used to form <strong>all</strong> or part of the principal of the trust and the trust isestablished (other than by will) by any of the following:1) the person;2) the person's spouse; or3) any other person, including a court or administrative body, with legalauthority to act on behalf of or at the direction of the person or the person'sspouse.d) <strong>This</strong> Section does not apply to the following trusts:1) an irrevocable trust containing the resourcesassets of a disabled personwho is determined disabled (as provideddescribed in Section 120.314) andunder age 65 that is established by a parent, grandparent, legal guardian orcourt for the sole benefit (as defined in Section 120.388(m)(2)) of thedisabled person, if language contained in the trust stipulates that anyamount remaining in the trust (up to the amount expended by theDepartment on medical assistance) sh<strong>all</strong> be paid to the Department uponthe death of the person. <strong>This</strong> exclusion continues after the person reachesage 65 as long as the person continues to be disabled but any additionsmade by the person to the trust after age 65 will be treated as a transfer ofassets under SectionsSection 120.387 and 120.388. If the trust containsproceeds from a personal injury settlement, any Department charge (asdescribed at 89 Ill. Adm. Code 102.260) must be satisfied in order for thetrust to be excluded under this subsection; or2) an irrevocable trust containing the resourcesassets of a disabled personwho is determined disabled (as provideddescribed in Section 120.314) thatis established and managed by a non-profit association that pools fundsbut maintains a separate account for each beneficiary that is established bythe disabled person, a parent, grandparent, legal guardian or court for thesole benefit of the disabled person, if language contained in the truststipulates that any amount remaining in the trust (up to the amountexpended by the Department on medical assistance) that is not retained bythe trust for reasonable administrative costs related to wrapping up theaffairs of the subaccount sh<strong>all</strong> be paid to the Department upon the death of
<strong>JCAR890120</strong>-<strong>1011664r08</strong>1504150515061507150815091510151115121513151415151516151715181519152015211522152315241525152615271528152915301531153215331534153515361537153815391540154115421543154415451546the person. <strong>This</strong> exclusion continues after the person reaches age 65 aslong as the person continues to meet the definition of disabled (to theextent permitted under federal law). Any funding of a subaccount in apooled trust by a person over age 64 will be treated as a transfer for fairmarket value under Section 120.388 so long as the person meets thedefinition of disabled. If the trust contains proceeds from a personalinjury settlement, any Department charge (as described at 89 Ill. Adm.Code 102.260) must be satisfied in order for the trust to be excluded underthis subsection (d).e) Subsections (f) and (g) of this Section apply to the portion of the trust attributableto the person and without regard to:1) the purpose for establishment of the trust;2) whether the trustee has or exercises any discretion under the trust; or3) whether there are any restrictions on distributions or use of distributionsfrom the trust.f) For revocable trusts, the Department sh<strong>all</strong>:1) treat the principal as an available resourceasset;2) treat as income payments from the trust that are made to or for the benefitof the person; and3) treat any other payments from the trust as transfers of assets by the person(subject to the provisions of, and depending on the date of the payment,Section 120.387 or 120.388).g) For irrevocable trusts, the Department sh<strong>all</strong>:1) treat as an available resourceasset the amount of the trust from whichpayment to or for the benefit of the person could be made;2) treat as income payments from the trust that are made to or for the benefitof the person;3) treat any other payments from the trust as transfers of assets by the person(subject to the provisions of Section 120.387 or 120.388, as applicable);and
<strong>JCAR890120</strong>-<strong>1011664r08</strong>15471548154915501551155215531554155515561557155815591560156115621563156415651566156715681569157015711572157315741575157615771578157915801581158215831584158515861587158815894) treat as a transfer of assets by the person the amount of the trust fromwhich no payment could be made to the person under any circumstances(subject to the provisions of Section 120.387 or 120.388, as applicable).The date of the transfer is the date the trust was established or, if later, thedate that payment to the person was foreclosed. The amount of the trust isdetermined by including any payments made from the trust after the datethat payment to the person was foreclosed.h) Trust Income. For married couples, income from trusts sh<strong>all</strong> be attributed to eachspouse as provided in the trust, unless:1) payment of income is made solely to one spouse, in which case the incomesh<strong>all</strong> be attributed to that spouse;2) payment of income is made to both spouses, in which case one-half of theincome sh<strong>all</strong> be attributed to each spouse; or3) payment of income is made to either spouse, or both, and to anotherperson or persons, in which case the income sh<strong>all</strong> be attributed to eachspouse in proportion to the spouse's interest, or, if payment is made to bothspouses and no such interest is specified, one-half of the joint interest sh<strong>all</strong>be attributed to each spouse.i) Annuities are treated similar to trusts.1) Revocable and assignable annuities are considered available resources.2) Any portion of an annuity from which payment to or for the benefit of theperson or the person's spouse could be made is an available resource. Anannuity that may be surrendered to its issuing entity for a refund orpayment of a specified amount or provides a lump-sum settlement optionis an available resource valued at the amount of any such refund, surrenderor settlement.3) Income received from an annuity by an institutionalized person isconsidered non-exempt income. Income received by the communityspouse of an institutionalized person is treated as available to thecommunity spouse for the purpose of determining the community spouseincome <strong>all</strong>owance under Section 120.379(e).4) An annuity that fails to name the State of Illinois as a remainderbeneficiary as required under Section 120.385(b) sh<strong>all</strong> result in denial ortermination of eligibility for long term care services.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>1590159115921593159415951596159715981599160016011602160316041605160616071608160916101611161216131614161516161617161816191620162116221623162416251626162716281629163016311632j) The principal of a trust fund established under the Self Sufficiency Trust FundProgram (see 20 ILCS 1705/21.1) is an exempt resource.(Source: Amended at 35 Ill. Reg. ______, effective ____________)Section 120.379 Provisions for the Prevention of Spousal Impoverishmenta) The provisions for the prevention of spousal impoverishment apply only to aninstitutionalized person (as defined in Section 120.388(c)) whose spouse residesin the community. For purposes of this Section, those persons sh<strong>all</strong> be referred toas the institutionalized spouse and the community spouse.a resident of a long termcare facility whose spouse resides in the community and to a person who but forthe provision of home and community-based services under Section 4.02 of theIllinois Act on the Aging would require the level of care provided in a long termcare facility and whose spouse resides in the community.b) Income. In determining the financial eligibility of an institutionalized spouse,only non-exempt income attributed to the institutionalized spouse sh<strong>all</strong> beconsidered available. The following rebuttable presumptions sh<strong>all</strong> apply indetermining the income attributed to each spouseAn assessment is completed todetermine the total combined amount of nonexempt assets of the individual andhis or her community spouse:1) if payment of income is made solely in the name of one spouse, theincome will be considered available only to that spouse; when residencebegins in a long term care facility or when home and community-basedservices begin; and2) if payment of income is made in the names of both spouses, one-half ofthe income sh<strong>all</strong> be considered available to each spouse;when requestedby either spouse or a representative acting on behalf of either spouse, evenif an application for assistance has not been filed.3) if payment of income is made in the names of either spouse, or both, andto another person or persons, the income sh<strong>all</strong> be considered available toeach spouse in proportion to the spouse's interest (or, if payment is madeto both spouses and no other interest is specified, one-half of the jointinterest sh<strong>all</strong> be considered available to each spouse);4) if payment of income is made from a trust, the income sh<strong>all</strong> be consideredavailable to each spouse as provided under Section 120.347(h); and
<strong>JCAR890120</strong>-<strong>1011664r08</strong>16331634163516361637163816391640164116421643164416451646164716481649165016511652165316541655165616571658165916601661166216631664166516661667166816691670167116721673167416755) if there is no trust or instrument establishing ownership, one-half of theincome sh<strong>all</strong> be considered available to the institutionalized spouse andone-half to the community spouse.c) Resources. In determining the financial eligibility of an institutionalized spouse,the following sh<strong>all</strong> applyA re-assessment is not required if:1) At the beginning of a continuous period of institutionalization, the totalvalue of resources owned by either or both spouses sh<strong>all</strong> be computed. aresident of a long term care facility is discharged for a period of less than30 days and then reenters the facility;2) Assessment. Upon the request of an institutionalized spouse, communityspouse, or a representative of either, at the beginning of a continuousperiod of institutionalization, the Department sh<strong>all</strong> conduct an assessmentof the couple's resources for the purpose of determining the combinedamount of nonexempt resources in which either spouse has an ownershipinterest. The person requesting the assessment sh<strong>all</strong> be responsible forproviding documentation and verification necessary for the Department tocomplete the assessment. a resident of a long term care facility enters ahospital and then returns to the facility from the hospital;3) For purposes of this subsection (c), a continuous period ofinstitutionalization is defined as at least 30 days of continuous institutionalcare. An initial assessment remains effective during that period if: anindividual discontinues receiving home and community-based services fora period of less than 30 days; orA) a resident of a long term care facility is discharged for a period ofless than 30 days and then reenters the facility;B) a resident of a long term care facility enters a hospital and thenreturns to the facility from the hospital;C) a person discontinues receiving home and community-basedservices for a period of less than 30 days; orD) a person discontinues receiving home and community-basedservices due to hospitalization and then is discharged and begins toreceive home and community-based services.4) At the time of an institutionalized spouse's application for medicalassistance, <strong>all</strong> nonexempt resources held by either the institutionalized
<strong>JCAR890120</strong>-<strong>1011664r08</strong>167616771678167916801681168216831684168516861687168816891690169116921693169416951696169716981699170017011702170317041705170617071708170917101711171217131714171517161717person, the community spouse, or both sh<strong>all</strong> be considered available to theinstitutionalized spouse. From this amount may be deducted andtransferred to the community spouse the Community Spouse ResourceAllowance (CSRA), as provided under subsection (d) of this Section. Theremaining amount sh<strong>all</strong> be the total amount of resources consideredavailable to the institutionalized spouse.an individual discontinuesreceiving home and community-based services due to hospitalization andthen is discharged and begins to receive home and community-basedservices.d) Transfer of Resources to the Community Spouse. From the amount of nonexemptresources considered available to the institutionalized spouse, as described insubsection (c)(4) of this Section, a The transfer of resourcesproperty is <strong>all</strong>owed, asdetermined in subsection (b) of this Section, by the institutionalized spouseclientto the community spouse or to another individual for the sole benefit (as definedin Section 120.388(m)(2)(D)) of the community spouse in an amount that doesnot exceed the CSRACommunity Spouse Asset Allowance (CSAA). The CSRAis the difference between the amount of resources otherwise available to thecommunity spouse and the greatest of:CSAA, as of October 1, 1989, is an amountup to but not greater than $60,000 that the individual may transfer, withoutaffecting eligibility, to the community spouse or to another individual for the solebenefit of the community spouse. As of October 1, 1989, the amount of assets anindividual may transfer to his or her community spouse is $60,000 minus anynonexempt assets of the community spouse. The amount established as theCSAA sh<strong>all</strong> be provided for calendar years after 1989 by the Department ofHealth and Human Services. The CSAA may exceed the standard annual figureestablished by the U.S. Department of Health and Human Services only in one ofthe following circumstances:1) the amount established annu<strong>all</strong>y by the US Department of Health andHuman Services (DHHS) (as of January 1, 2011, $109,560); in a legalproceeding, a court approves the transfer of income-producing assets tothe community spouse in an amount greater than the standard CSAA; or2) the amount established through a fair hearing under subsection (f)(3) ofthis Section; oras the result of an appeal hearing (described in 89 Ill. Adm.Code 104.1), the Department determines that the transfer of incomeproducingassets to the community spouse in an amount greater than thestandard CSAA is necessary to raise the community spouse's income to,but not more than, the Community Spouse Maintenance Needs Allowance(described in subsection (f) of this Section).
<strong>JCAR890120</strong>-<strong>1011664r08</strong>17181719172017211722172317241725172617271728172917301731173217331734173517361737173817391740174117421743174417451746174717481749175017511752175317541755175617571758175917603) the amount transferred under a court order against an institutionalizedspouse for the support of the community spouse.A) The Department will measure the amount of an <strong>all</strong>owable increasein the CSAA by the cost to purchase an actuari<strong>all</strong>y sound singlepremium life annuity producing monthly payments that, whenadded to the community spouse's income, will be sufficient to raisethe community spouse's income to, but not more than, theCommunity Spouse Maintenance Needs Allowance. If assets areinsufficient to purchase such an annuity, the Department willmeasure the amount of an <strong>all</strong>owable increase in the CSAA by thecost to purchase an actuari<strong>all</strong>y sound single premium life annuityproducing monthly payments using available assets.B) It is the appellant's responsibility to provide the Department withan estimate from a reputable company of the cost to purchase theannuity.C) The Department may compare the estimate with availableinformation on the cost of other single premium life annuities.D) In calculating the amount of the community spouse's income afterapproval of an increased CSAA, the Department sh<strong>all</strong> deem theamount of the annuity payments as being available to thecommunity spouse, although it will not require the actual purchaseof an annuity.e) The appeal hearing, described in subsection (d)(2) of this Section, sh<strong>all</strong> be heldwithin 30 days after the date the appeal is filed.e)f) Deductions are <strong>all</strong>owed from an institutionalized spouse's post-eligibility theMANG client's non-SSI income (pursuant to Section 120.61(d) and (e)) for acommunity spouse income <strong>all</strong>owance and a family <strong>all</strong>owancefor a CommunitySpouse Maintenance Needs Allowance and a Family Maintenance NeedsAllowance for each dependent family member who is living with the communityspouse and who does not have enough income to meet his or her needs. Familymembers include dependent children under age 21, dependent adult children,dependent parents or dependent siblings of either spouse. The deductionsareamount of the deduction is determined as follows:1) The deduction for the Community Spouse Maintenance Allowance.SpouseMaintenance Needs Allowance, as of October 1, 1989, is equal to thecommunity spouse maintenance needs standard ($1,500) less any
<strong>JCAR890120</strong>-<strong>1011664r08</strong>1761176217631764176517661767176817691770177117721773177417751776177717781779178017811782178317841785178617871788178917901791179217931794179517961797179817991800180118021803nonexempt monthly income of the community spouse.A) The amount of monthly income that may be deducted from theinstitutionalized spouse's post-eligibility income for the benefit ofthe community spouse is equal to the minimum monthlymaintenance needs <strong>all</strong>owance (MMMNA) less the amount ofmonthly income otherwise available to the community spouse (asdetermined under subsection (b) of this Section.The amountestablished as the MMMNA (as of January 1, 2011, $2,739 permonth)community spouse maintenance needs standard sh<strong>all</strong> beprovided for calendar years after 20111989 by DHHStheDepartment of Health and Human Services.B) The deduction is <strong>all</strong>owed only to the extent the income of thepersonindividual is in fact contributed to the community spouse.However, the deduction for the community spouse income<strong>all</strong>owanceCommunity Spouse Maintenance Needs Allowance sh<strong>all</strong>not be less than the amount ordered by athe court for support of thecommunity spouse or the amount determined as the result of athefair hearing provided for under subsection (f) of this Section.C) For purposes of this Section, <strong>all</strong> income of the institutionalizedspouse that can be made available to the community spouse sh<strong>all</strong>be made available before resources may be transferred in excess ofthe CSRA specified under subsection (d)(1) of this Section thatwill generate income to make up the difference between theMMMNA and the amount of income available to the communityspouse.2) Family Allowance. The amount of monthly income that may be deductedfrom the institutionalized spouse's post-eligibility income for the benefit ofThe deduction for the Family Maintenance Needs Allowance for eachdependent family member is equal to one-third of the difference betweenthe family maintenance needs standard (150%122% of the annual FederalPoverty Level for two persons as of September 30, 1989, 133% as of July1, 1991 and 150% as of July 1, 1992) and any nonexempt income of thefamily member. Family members only include dependent children underage 21, dependent adult children, dependent parents or dependent siblingsof either spouse who reside with the community spouse.3) A deduction is also <strong>all</strong>owed from the institutionalized spouse's posteligibilityincome for dependent children under age 21 who do not residewith the community spouse pursuant to Section 120.61(e)(5).
<strong>JCAR890120</strong>-<strong>1011664r08</strong>18041805180618071808180918101811181218131814181518161817181818191820182118221823182418251826182718281829183018311832183318341835183618371838183918401841184218431844184518464) The term "dependent" has the meaning ascribed to a "qualified" personunder 26 USC 152.f) Fair Hearings. Either the institutionalized spouse or the community spouse mayrequest a hearing (as described in 89 Ill. Adm. Code 104.1) under this Section forthe following reasons:1) either spouse is dissatisfied with a determination of:A) the community spouse income <strong>all</strong>owance under subsection (e)(1)of this Section;B) the amount of the monthly income treated as otherwise available tothe community spouse (as applied under subsection (e)(1) of thisSection);C) the attribution of resources under subsection (c)(4) of this Section;orD) the determination of the CSRA under subsection (d) of thisSection.2) Either spouse may request an increase in the MMMNA under subsection(e)(1). If either spouse establishes that, due to exceptional circumstancesresulting in significant financial duress, the community spouse needsincome above the level provided by the MMMNA, an amount adequate toprovide that additional income sh<strong>all</strong> be substituted. For purposes of thissubsection (f)(2), significant financial distress means expenses that thecommunity spouse incurs in excess of the income standard, including:A) recurring or extraordinary medical expenses of the communityspouse that are not covered by any third party resource, includinginsurance or the Medical Assistance Program;B) amounts necessary to preserve, maintain or make major repairs tohomestead property; orC) amounts necessary to preserve an income producing resource,subject to the limitations on that property under Section120.381(a)(3) and as long as the expense is reasonable in relationto the income produced by the resource.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>18471848184918501851185218531854185518561857185818591860186118621863186418651866186718681869187018711872187318741875187618771878187918801881188218831884188518861887188818893) Either spouse may request that an alternative CSRA be substituted for thestandard CSRA calculated under subsection (d) of this Section if it can beestablished that the standard CSRA (in relation to the amount of income itgenerates) is inadequate to raise the community spouse's income to theMMMNA.A) Before a substitute CSRA may be <strong>all</strong>ocated under this subsection(f)(3), the amount of income attributed to the institutionalizedspouse that may be transferred to the community spouse undersubsection (e) of this Section sh<strong>all</strong> first be considered available toraise the community spouse's income to the MMMNA.B) If the sum of income otherwise available to the community spouseand income that may be transferred from the institutionalizedspouse is insufficient to raise the community spouse's income tothe MMMNA, then a substitute CSRA may be <strong>all</strong>owed. Theamount the substitute CSRA may exceed the CSRA provided forunder subsection (d) of this Section is limited to the amount ofresources necessary to generate income to raise the communityspouse's total income to the MMMNA.C) In determining the amount of income that a substitute CSRA underthis subsection (f)(3) may generate, the Department will use, forpurposes of comparison, the cost to purchase an actuari<strong>all</strong>y soundsingle premium life annuity producing monthly payments that,when added to the community spouse's total income, will besufficient to raise the community spouse's income to, but not morethan, the MMMNA. If resources are insufficient to purchase anannuity that will raise the community spouse's income to theMMMNA, the Department will measure the amount of an<strong>all</strong>owable increase in the CSRA by the cost to purchase anactuari<strong>all</strong>y sound single premium life annuity producing monthlypayments using available resources.D) It is the requesting person's responsibility to provide theDepartment with an estimate from a reputable company of the costto purchase the annuity described in subsection (f)(3)(C).E) The Department may compare the estimate with availableinformation on the cost of other single premium life annuities.F) In calculating the amount of the community spouse's income afterapproval of a substitute CSRA, the Department sh<strong>all</strong> deem the
<strong>JCAR890120</strong>-<strong>1011664r08</strong>1890189118921893189418951896189718981899190019011902190319041905190619071908190919101911191219131914191519161917191819191920192119221923192419251926192719281929193019311932amount of the monthly annuity payments as being available to thecommunity spouse, although it will not require the actual purchaseof an annuity.g) The appeal hearing described in subsection (d)(2) of this Section sh<strong>all</strong> be heldwithin 30 days after the date the appeal is filed.h) A transfer of resources under subsection (d) of this Section from theinstitutionalized spouse to the community spouse sh<strong>all</strong> be made as soon aspracticable after the date of initial determination of eligibility and before the firstregularly scheduled redetermination of eligibility, taking into account such timeas may be necessary to obtain a court order under subsection (d)(3) of thisSection. If a transfer of resources to a community spouse has not been made bythe first scheduled redetermination and no petition for an order of spousal supportis pending judicial review, the resources sh<strong>all</strong> be considered available to theinstitutionalized spouse.i) Assignment of Support Rights. The institutionalized spouse sh<strong>all</strong> not be ineligibleby reason of resources determined under subsection (c)(4) to be available for thecost of care when:1) the institutionalized spouse has assigned to the State any rights tosupport from the community spouse (see Section 120.319);2) the institutionalized spouse lacks the ability to execute anassignment due to physical or mental impairment, but the State has theright to bring a support proceeding against a community spouse withoutthat assignment; or3) the State determines that denial of eligibility would work an unduehardship (see Section 120.388(r)(1)).j) The Department may pursue any available legal process to enforce its right ofassignment to support against the community spouse or any other responsibleperson pursuant to Section 120.319. These processes may include, but sh<strong>all</strong> notbe limited to, the administrative support procedures provided under 89 Ill. Adm.Code 103.(Source: Amended at 35 Ill. Reg. ______, effective ____________)Section 120.380 ResourcesAssetsa) Unless otherwise specified and for purposes of this Part, the term "resource" (as
<strong>JCAR890120</strong>-<strong>1011664r08</strong>1933193419351936193719381939194019411942194319441945194619471948194919501951195219531954195519561957195819591960196119621963196419651966196719681969197019711972197319741975defined in 42 USC 1382b, except subsection (a)(1) of that section, which excludesthe home as a resource) means cash or any other personal or real property that aperson owns and has the right, authority or power to liquidate. The value ofnonexempt assets sh<strong>all</strong> be considered in determining eligibility for AABDMANG. Assets do not affect eligibility for TANF MANG.b) A resource is considered available to pay for a person's own care when at thedisposal of that person; when the person has a legal interest in a liquidated sumand has the legal ability to make the sum available for support, maintenance ormedical care; or when the person has the lawful power to make the resourceavailable or to cause the resource to be made availableJointly held assets forAABD MANG sh<strong>all</strong> be treated in the same manner as described in 89 Ill. Adm.Code 113.140.c) The value of nonexempt resources sh<strong>all</strong> be considered in determining eligibilityfor any means-tested public benefit program administered by the Department, theDepartment of Human Services or the Department on Aging if eligibility isdetermined, in part, on the basis of resources as provided under thisSectionPotential payments from a Medicaid qualifying trust for AABD MANGand MANG(C) sh<strong>all</strong> be treated in the same manner as described in Section120.346.d) Determination of Resources. Trusts established on or after August 11, 1993, sh<strong>all</strong>be treated in the manner described in Section 120.347.1) In determining initial financial eligibility for medical assistance, theDepartment considers nonexempt verified resources available to a personas of the date of decision on the application for medical assistance. Thedate of verification (see Section 120.308(f)) may be prior to the date ofdecision. Money considered as income for a month is not considered aresource for that same month. If income for a month is added to a bankaccount that month, the Department will subtract the amount of incomefrom the bank balance to determine the resource level. Any incomeremaining in the following months is considered a resource.2) In determining financial eligibility for retroactive months (see Section120.61(b)), the Department will consider the amount of income andresources available to a person as of the first day of each of the backdatedmonths for which eligibility is sought.3) In determining a person's spenddown obligation (see Section 120.384), theDepartment considers the amount of nonexempt resources available as ofthe date of decision, in the case of initial eligibility, and the first day of the
<strong>JCAR890120</strong>-<strong>1011664r08</strong>1976197719781979198019811982198319841985198619871988198919901991199219931994199519961997199819992000200120022003200420052006200720082009201020112012201320142015201620172018month, in the case of retroactive eligibility, that are in excess of theapplicable resource disregard (see Section 120.382).e) Subject to subsection (c) of this Section and 89 Ill. Adm. Code 113.140, the entireequity value of jointly held resources sh<strong>all</strong> be considered available in determininga person's eligibility for assistance, unless:1) The resource is a joint income tax refund, in which case one-half of therefund is considered owned by each person; or2) The person documents that he or she does not have access to the resource.Appropriate documents may include, but are not limited to, bankdocuments, signature cards, trust documents, divorce papers, and papersfrom court proceedings that show the person is leg<strong>all</strong>y unable to access theresource; or3) The resource is held jointly with an individual eligible under any meanstestedpublic health benefit program (other than the SupplementalNutrition Assistance Program) administered by the Department, theDepartment of Human Services, or the Department on Aging; or4) The person can document the amount of his or her legal interest in theresource and that such amount is less than the entire value of the resource,then the documented amount sh<strong>all</strong> be considered. Appropriatedocumentation may include, but is not limited to, bank documents, trustdocuments, signature cards, divorce papers, or court orders that show theperson's legal interest is less than the entire value of the resource; or5) The person documents that the resource or a portion of the resource is notowned by the person and the person's accessibility to the resource ischanged (see subsections (b)(2) and (4) of this Section for documentationexamples).f) In determining the eligibility of a person for long term care services whose spouseresides in the community, <strong>all</strong> nonexempt resources owned by the institutionalizedspouse, the community spouse, or both sh<strong>all</strong> be considered available to theinstitutionalized spouse in determining his or her eligibility for medicalassistance. From the total amount of such resources may be deducted aCommunity Spouse Resource Allowance as provided under Section 120.379.g) Trusts established prior to August 11, 1993 sh<strong>all</strong> be treated in the mannerdescribed in Section 120.346.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>2019202020212022202320242025202620272028202920302031203220332034203520362037203820392040204120422043204420452046204720482049205020512052205320542055205620572058205920602061h) Trusts established on or after August 11, 1993 sh<strong>all</strong> be treated in the mannerdescribed in Section 120.347.i) The value of a life estate sh<strong>all</strong> be determined at the time the life estate in theproperty is established and at the time the property (for example, resoucesassets)is liquidated. In determining the value of a life estate and remainder interestbased on the value of the property at the time the life estate is established or of theamount received when the property is liquidated, the Department sh<strong>all</strong> apply thevalues described in Section 120.Table A. The life estate and remainder interestare based on the age of the person at the time the life estate in the property isestablished and at the time the property is liquidated and the corresponding valuesdescribed in Section 120.Table A.j) A person's entrance fee in a continuing care retirement community or life carecommunity (as those entities are described in 42 USC 1396r(c)(5)(B)) sh<strong>all</strong> beconsidered an available resource to the extent that:1) the person has the ability to use the entrance fee, or the contract providesthat the entrance fee may be used to pay for care should other resources orincome of the person be insufficient to pay for the care;2) the person is eligible for a refund of any remaining entrance fee when theperson dies or terminates the continuing care retirement community or lifecare community contract and leaves the community; and3) the entrance fee does not confer an ownership interest in the continuingcare retirement community or life care community.k) Non-homestead real property, including homestead property that is no longerexempt (see Section 120.381(a)(1)), is considered an available resource unless:1) the property is exempted as income-producing to the extent permittedunder Section 120.381(a)(3);2) ownership of the property consists of a fractional interest of such a sm<strong>all</strong>value that a substantial loss to the person would occur if the property weresold; or3) the property has been listed for sale, in which case the propertywill not be counted as available for at least six months as long as theperson continues to make a good faith effort to sell the property. <strong>This</strong>effort can be verified by evidence, including advertisements ordocumentation of the listing of the property with licensed real estate
<strong>JCAR890120</strong>-<strong>1011664r08</strong>2062206320642065206620672068206920702071207220732074207520762077207820792080208120822083208420852086208720882089209020912092209320942095209620972098209921002101210221032104agents or brokers that <strong>includes</strong> a report of any offer from prospectivebuyers. The Department will review cases in which the property has notbeen sold after six months and will consider the following factors indetermining if extensions of the initial six months are warranted:A) the asking price is less than the fair market value of the property;B) the property is marketed through a qualified realtor who isacting in good faith;C) there is not a substantial market for the type of propertybeing sold; andD) the person has not rejected any reasonable offer to buy theproperty.(Source: Amended at 35 Ill. Reg. ______, effective ____________)Section 120.381 Exempt ResourcesAssetsAABD MANG-assets exempt from consideration for AABD MANG sh<strong>all</strong> be as follows:a) The following resourcesassets are exempt from consideration in determiningeligibility for medical assistance and the amount of the assistance payment:1) Homestead Property.propertyA) Homestead property is any property in which a person (and spouse,if any) has an ownership interest and that serves as the person'sprincipal place of residence. <strong>This</strong> property <strong>includes</strong> the shelter inwhich a person resides, the adjoining land on which the shelter islocated and related outbuildings.B) If a person (and spouse, if any) moves out of his or her homewithout the intent to return, the home is no longer exempt becauseit is no longer the person's principal place of residence. If a personleaves his or her home to live in a long term care facility, theproperty is considered exempt, irrespective of the person's intent toreturn, as long as a spouse or dependent relative of the eligibleperson continues to live there. The person's equity in the formerhome is treated as an available resource effective with the first dayof the month following the month it is no longer his or herprincipal place of residence.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>21052106210721082109211021112112211321142115211621172118211921202121212221232124212521262127212821292130213121322133213421352136213721382139214021412142214321442145214621472) Personal effects and household goods are exempt to the extent they areexcluded under 20 CFR 416.1216.PropertyA) Personal effects and household goods of reasonable value(reasonable value means the client's equity value in such propertydoes not exceed $2,000). Wedding and engagement rings anditems required due to medical or physical condition.B) Regardless of the value, personal effects and household goods areexempt in determining the amount <strong>all</strong>owed as the CommunitySpouse Asset Allowance (as described in Section 120.386).3) Resources (for example, land, buildings, equipment and supplies or tools)necessary for self-support up to $6,000 of the person'sindividual's equityin the income producing property provided the property produces a netannual income of at least six percent of the excluded equity value of theproperty. The equity value in excess of $6,000 is not excludedappliedtoward the asset disregard. If the activity produces income that is less thansix percent of the exempt equity due to reasons beyond theperson'sindividual's control (for example, the person'sindividual's illnessor crop failure) and there is a reasonable expectation that the property willagainindividual's activity will increase to produce income equal to sixpercent of the equity value (for example, a medical prognosis that thepersonindividual is expected to respond to treatment or that droughtresistant corn will be planted), the equity value in the property up to$6,000 is exempt. If the personindividual owns more than one piece ofproperty and each produces income, each is looked at to determine if thesix percent rule is met and then the amounts of the person'sindividual'sequity in <strong>all</strong> of those properties are totaled to see if the total equity is$6,000 or less. The total equity value of <strong>all</strong> properties that is exemptunder this subsection is limited to $6,000.4) Automobile.A) Exclude one automobile, regardless of value, used by the client,spouse or other dependent if:i) it is necessary for employment;ii) it is necessary for the medical treatment of a specific orregular medical problem;
<strong>JCAR890120</strong>-<strong>1011664r08</strong>2148214921502151215221532154215521562157215821592160216121622163216421652166216721682169217021712172217321742175217621772178217921802181218221832184218521862187218821892190iii) it is modified for operation by, or transportation of, ahandicapped person;iv) it is necessary because of factors such as climate, terrain ordistance to provide necessary transportation to performessential daily activities; orv) one vehicle for each spouse is exempt in determining theamount <strong>all</strong>owed as the Community Spouse ResourceAssetAllowance (as described in Section 120.379(d)120.386).B) If not excluded in subsection (a)(4)(A) of this Section, exclude oneautomobile is excluded to the extent its equity valuethe fair marketvalue does not exceed $4500. AnyApply the excess equity value isappliedfair market value toward the applicable resourceassetdisregard (see Section 120.38289 Ill. Adm. Code 113.142). TheDepartment will determine fair market value in accordance with 89Ill. Adm. Code 121.57(b)(2)(D)(iv).C) For <strong>all</strong> other automobiles, apply the equity value (fair market valueminus any encumbrance) toward the resourceasset disregard (see89 Ill. Adm. Code 113.142).5) Life insurance policies with a total face value of $1,500 or less and <strong>all</strong>term life insurance policies. If the total face value exceeds $1,500, thecash surrender value must be counted as a resource.6) For purposes of this Section, the term "equity value" refers to:A) in the case of real property, the value described in Section120.385(c); andB) in the case of personal property, the price that an item canreasonably be expected to sell for on the open market in theparticular geographic area involved, minus any encumbrances (asdescribed in Section 120.385(c)(1)(C)).b) Burial spaces and funds are exempt as follows:1)Burial spaces that are intendedfor the use of the personindividual, his or her spouse, or any other member of hisor her immediate family are exempt. Immediate family is defined as a person'sanindividual's minor and adult children, including adopted children andstepchildren, a person'san individual's brothers, sisters, parents and, adoptiveparents, and the spouses of these individuals.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>21912192219321942195219621972198219922002201220222032204220522062207220822092210221122122213221422152216221722182219222022212222222322242225222622272228222922302231223222332) Funds set aside for the burial expenses of the individual and his or herspouse, subject to a limit of $1,500 each. <strong>This</strong> limit will be reduced by theface value of any excluded life insurance policy and the amount of anyfunds held in an irrevocable trust or other irrevocable arrangement that isavailable for burial expenses.3) Interest earned on excluded burial funds and appreciation in the value ofexcluded burial arrangements which occurred the earlier of the date of firstSSI eligibility or the date of AABD eligibility, but no earlier thanNovember 1, 1982 (see 20 CFR 416.1231(b)(5) (1992)).4) Funds specific<strong>all</strong>y and irrevocably set aside for the professional funeralservices and burial expenses of the individual and his or her spouse,subject to a limit of $4,000 each, including prepaid funeral and burialplans. <strong>This</strong> limit will be increased annu<strong>all</strong>y by three percent.c) Funds that are set aside for the burial expenses of a person and his or her spousein a bank account owned by the person that is clearly identified as a burial fund isexempt up to $1500. <strong>This</strong> amount is reduced by the face value of any excludedlife insurance on the person and the amount of any funds held in an irrevocabletrust or other irrevocable arrangement that is available for burial expenses perperson.d) Prepaid Funeral/Burial Contracts. Prepaid funeral/burial contracts that complywith the provisions of the Illinois Funeral or Burial Funds Act [225 ILCS 45] areexempt to the following extent:1) Funds in a revocable prepaid funeral/burial contract are exempt up to$1500.2) Effective September 1, 2009, funds in an irrevocable prepaidfuneral/burial contract are exempt up to $5,537. <strong>This</strong> amount sh<strong>all</strong> beincreased annu<strong>all</strong>y each September 1 by 3%.3) A prepaid, guaranteed price funeral/burial contract funded by anirrevocable assignment of a person's life insurance policy to a trust, asprovided under 225 ILCS 45/2a(c), is exempt. The trust is responsible forensuring that the provider of funeral services under contract receives theproceeds of the policy when it provides the funeral goods and servicesspecified under the contract (see 225 ILCS 45/1a-1(a). The irrevocableassignment of ownership of the insurance policy must be acknowledgedby the insurance company.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>2234223522362237223822392240224122422243224422452246224722482249225022512252225322542255225622572258225922602261226222632264226522662267226822692270227122722273227422752276e)c) ResourcesAssets necessary for fulfillment of an approved plan for achieving selfsupportunder 42 CFR 416.1220.d) Trust funds are exempt as follows:1) The principal of a trust fund only when the instrument establishing thetrust specific<strong>all</strong>y states the principal cannot be impaired.2) The principal of a trust fund established under the Self Sufficiency TrustFund Program [20 ILCS 1705/21.1].f)e) ResourcesAssets excluded by express provision of 20 CFR 416.1236 (20091997).g)f)h)g)i)h)j)i)k)j)l)k)Donations or benefits from fund raisers held for a seriously ill client provided theclient or a responsible relative of the client does not have control (for example,not available to the client or the responsible relative) over the donations orbenefits or the disbursement of donations or benefits [305 ILCS 5/5-2].Payments made to veterans who receive an annual disability payment or to thesurvivors of deceased veterans who receive a one-time lump sum payment fromthe Agent Orange Settlement Fund or any other fund referencing Agent Orangeproduct liability under Public Law 101-201.Money received from the Social Security Administration under a Plan to AchieveSelf-Support (PASS) and held in a separate account.Disaster relief payments provided by federal, State or local government or adisaster assistance organization.The amount of earned income tax credit that the client receives as advancepayment or as a refund of federal income tax.For disabled persons who have lost eligibility under Section 120.510 and who areonly requesting services other than those described in Section89 Ill. Adm. Code120.61(a) (except that subsection's reference to services provided through aCommunity Integrated Living Facility (CILA)), the following additionalexemptions sh<strong>all</strong> apply:1) Retirement accounts that a person with a disability cannot access withoutpenalty before the age of 59½ and medical savings accounts establishedpursuant to 26 USC 220; and
<strong>JCAR890120</strong>-<strong>1011664r08</strong>22772278227922802281228222832284228522862287228822892290229122922293229422952296229722982299230023012302230323042305230623072308230923102311231223132314231523162317231823192) Up to $25,000 if the person owned assets of equal value when his or hereligibility under Section 120.510 ended.m) The amount of damages recovered by a resident of a nursing home for any act thatinjures the resident pursuant to 210 ILCS 45/3-605.n)l)o)m)p)n)Certain payments received under the American Recovery and Reinvestment Actof 2009.1) Payments to World War II veterans who served in the Philippines andspouses of those veterans under Div. A, Title X, Sec. 1002 of P.L. 111-5.2) Payments or reimbursements for Premium Assistance for COBRAContinuous Coverage under Div. B, Title III, Sec. 3001 of P.L. 111-5.Certain payments received under the American Recovery and Reinvestment Actof 2009 are exempt as an asset the month of receipt and two months thereafter.1) Making Work Pay Credit under Div. B, Title I, Sec. 1001 of P.L. 111-5.2) Tax Credit for Certain Government Retirees under Div. B, Title II, Sec.2202 of P.L. 111-5.Economic Recovery Payments under the American Recovery and ReinvestmentAct of 2009 under Div B, Title II, Sec. 2201 of P.L. 111-5 are exempt as an assetthe month of receipt and nine months thereafter.(Source: Amended at 35 Ill. Reg. ______, effective ____________)Section 120.382 ResourceAsset DisregardIn addition to the exempt resourcesassets listed in Section 120.381, the cash value ofresourcesassets sh<strong>all</strong> be disregarded for AABD MANG as follows:a) $2,000 for a personclient and $3,000 for a personclient and one dependentresiding together. A dependent means a "qualifying" person as that term isdescribed in 26 USC 152.b) $50 for each additional dependent residing in the same household.c) Resources equal in amount to the benefits paid on behalf of a person under aqualified long term care insurance policy as provided under 42 USC1396p(b)(1)(C) and (b)(5). Policies written in Illinois are approved by the
<strong>JCAR890120</strong>-<strong>1011664r08</strong>232023212322232323242325232623272328232923302331233223332334233523362337233823392340234123422343234423452346234723482349235023512352235323542355235623572358235923602361Director of the Illinois Department of Insurance under the Qualified Long TermCare Insurance Partnership (QLTCIP) program (50 Ill. Adm. Code 2012). Thedollar value of the amount paid for QLTCIP benefits is disregarded; the extent towhich the disregard is applied to a resource will depend and may vary with theunderlying equity value (see Section 120.381(a)(6)) the person holds in theresource. The amount equal to the sum of qualifying insurance benefit paymentsmade as a result of coverage under a Long Term Care Partnership InsurancePolicy, as described in 50 Ill. Adm. Code 2018, provided that the person hasreceived <strong>all</strong> of the qualifying insurance benefit payments that are payable underthe policy.d) All assets of a person who purchases a Long Term Care Partnership InsurancePolicy, as described in 50 Ill. Adm. Code 2018, with coverage equal to theaverage cost of four years of long term care services in a nursing facility,provided that the person has received <strong>all</strong> of the qualifying insurance benefitpayments that are payable under the policy.d)e) Eligibility for medical assistance or the benefits described in Sections 120.72 and120.73AABD MANG does not exist when nonexempt resourcesassets exceed<strong>all</strong>owable disregardsthe above disregard.ef) For Qualified Medicare BeneficiariesBeneficiary (QMB)1) $4,000 for a single person and $6,000 for a person with one or moredependents.2) Eligibility for QMB status does not exist when resources exceed thedisregard amounts described in this subsection (e)countable assets exceedthe above disregard.(Source: Amended at 35 Ill. Reg. ______, effective ____________)Section 120.384 Spenddown of ResourcesAssets (AABD MANG)In determining a person's resource spenddown obligation, the Department compares nonexemptresources available to the person to the appropriate resource disregard. The amount of resourcesin excess of the disregard determines the amount of the spenddown.a) If a person presents verification that excess resources are no longer available, theDepartment will make the appropriate changes the month following the month theperson disposed of the resources.Determination of Assets
<strong>JCAR890120</strong>-<strong>1011664r08</strong>2362236323642365236623672368236923702371237223732374237523762377237823792380238123822383238423852386238723882389239023912392239323942395239623972398239924002401240224032404b) Persons enrolled in spenddown are not eligible for payment of covered medicalservices until spenddown is met. A resource spenddown is met by presenting<strong>all</strong>owable medical bills or receipts to the Department that equal the amount of theperson's nonexempt excess resources. See Sections 120.60(c) and 120.61(c) forspecific requirements related to spenddown, including the option to pay inspenddown to the Department by enrolling in the Pay-in Spenddown Program.c) Once an excess resource has been used to meet spenddown, whether or not theexcess amount has actu<strong>all</strong>y been reduced, it is no longer considered. However, atreapplication/redetermination, the Department will consider any excessnonexempt resources remaining as currently available. A spenddown cannot beeliminated by a non-<strong>all</strong>owable transfer made to qualify for or increase the needfor medical assistance.1) For individuals residing in the community, the Department determines theamount of non-exempt assets using the verified amount on the date ofdecision on the application for medical assistance. The date of verificationmay be prior to the date of decision. Money considered as income for amonth is not considered as an asset for that same month. If income for amonth is added to a bank account that month, the Department will subtractthe amount of income from the bank balance to determine the asset level.Any income remaining the following months is considered as an asset.2) The amount of non-exempt assets verified during the application processis used on the date of decision. If medical eligibility <strong>includes</strong> backdatedmonths, for the backdated months the Department will consider theamount of assets available to apply to the cost of medical care. TheDepartment will not determine the value of assets for backdated months ofeligibility. However, the amount of the excess assets verified during theapplication process is used to determine spenddown status in eachbackdated month of eligibility.3) Once the excess asset has been used to meet spenddown, whether or notthe excess amount has actu<strong>all</strong>y been reduced, it is no longer considered.However, at reapplication/redetermination, the Department will considerany excess non-exempt assets remaining as currently available.b) Community Cases (AABD MANG)For AABD MANG, to determine the spenddown obligation for clients in thecommunity, the Department will compare monthly countable income to theappropriate MANG standard and add any non-exempt assets in excess of theappropriate asset disregard to non-exempt monthly income in excess of theappropriate MANG Standard.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>24052406240724082409241024112412241324142415241624172418241924202421242224232424242524262427242824292430243124322433243424352436243724382439244024412442244324442445244624471) Regular AABD MANG – Community ResidentsWhen an individual residing in the community, has countable monthlyincome of not more than 99 cents over the appropriate MANG Standardand has non-exempt excess assets of not more than 99 cents over theappropriate asset disregard, the case is referred to as a Regular MANGcase. Payment for covered services is made for each month eligibilityexists.2) Spenddown AABD MANGA) When an individual resides in the community and has countablemonthly income of at least $1.00 over the MANG Standard and/ornon-exempt assets of at least $1.00 in excess of the asset disregardfor the appropriate size household, the case is referred to as acommunity spenddown case. The spenddown amount is the sumof the amount of income in excess of the MANG Standard plusnon-exempt assets in excess of the appropriate asset disregard.The Department will disregard any excess income and/or assetamounts that are not at least $1.00 over the appropriate standard ordisregard.B) If the individual presents verification that the excess amount is nolonger available, the Department will make the appropriatechanges the month following the month the assets were transferred.C) Individuals enrolled in spenddown are not eligible for payment ofcovered medical services until spenddown is met. Spenddown ismet by presenting <strong>all</strong>owable medical bills or receipts to theDepartment that equal the amount of the individual's excesscountable income and/or non-exempt excess assets. Individualsmay also pay-in the amount of the income or asset spenddown tothe Department by enrolling in the Pay-in Spenddown Program(see Section 120.60). Excess assets do not have to be reducedprior to the authorization of medical assistance.c) Group Care CasesTo determine the spenddown obligation for AABD MANG clients in group care,the Department will compare monthly countable income and non-exempt assets inexcess of the appropriate asset disregard to the cost of long term care at theprivate pay rate or the Department rate, whichever is greater. When an individualhas non-exempt excess assets, the excess amount is applied to the monthly longterm care charges after the monthly countable income has been applied.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>24482449245024512452245324542455245624572458245924602461246224632464246524662467246824692470247124722473247424752476247724782479248024812482248324842485248624872488248924901) Regular Group CareWhen an individual in group care has countable monthly income plus nonexemptassets in excess of the applicable asset disregard of not more than99 cents over the private pay rate or the Department rate, whichever isgreater, the case is referred to as a Regular Group Care case. If monthlycountable income plus excess non-exempt assets are less than the longterm care charges at the Department rate, the Department will pay thedifference.2) Group Care SpenddownA) When an individual in group care has countable monthly incomeplus non-exempt assets in excess of the applicable asset disregardof at least $1.00 over the cost of long term care at the private payrate or the Department rate, whichever is greater, the case isreferred to as a Group Care Spenddown case. The spenddownamount is the sum of the monthly countable income plus nonexemptassets over the applicable asset disregard.B) The transfer of asset policy set forth in Section 120.385 stillapplies. Once the client has been determined to have a resourcespenddown because of excess non-exempt assets, the spenddowncannot be eliminated by a non-<strong>all</strong>owable transfer made to qualifyfor or increase the need for medical assistance.C) If the individual presents verification that the excess amount is nolonger available and the transfer of assets is <strong>all</strong>owable according toSection 120.385, the Department will make the appropriatechanges the month following the month the assets were transferred.If spenddown has been met, the policy set forth in Section 120.385regarding transfer of assets does not apply. The client may disposeof the asset as he/she wishes as it has been applied to a metspenddown.D) Individuals enrolled in spenddown are not eligible for payment ofcovered medical services until spenddown is met. Spenddown ismet by presenting <strong>all</strong>owable medical bills or receipts to theDepartment that equal the amount of the individual's excesscountable income and/or non-exempt assets. Excess assets do nothave to be reduced prior to the authorization of medical assistance.(Source: Amended at 35 Ill. Reg. ______, effective ____________)
<strong>JCAR890120</strong>-<strong>1011664r08</strong>2491249224932494249524962497249824992500250125022503250425052506250725082509251025112512251325142515251625172518251925202521252225232524252525262527252825292530253125322533Section 120.385 Factors Affecting Eligibility for Long Term Care ServicesPropertyTransfer for Applications Filed Prior to October 1, 1989 (Repealed)a) For purposes of this Section, the terms "institutionalized persons" and "long termcare services" sh<strong>all</strong> have the meanings described in Section 120.388 of this Part.The terms "institutionalized spouse" and "community spouse" sh<strong>all</strong> have themeanings described in Section 120.379(a) of this Part.b) Disclosure of annuity and naming the State as remainder beneficiary:1) Effective November 1, 2011, an application (or redetermination related toan application) for long term care services sh<strong>all</strong> include a disclosure by aninstitutionalized person or his or her community spouse of any interesteither or both may have in any annuity or similar financial instrumentpurchased, regardless of whether the annuity is irrevocable or is treated asan asset. The application or recertification form sh<strong>all</strong> also include astatement that the State of Illinois becomes a remainder beneficiary undersuch an annuity or similar financial instrument to the extent that the Statehas provided medical assistance to the institutionalized person.2) Failure of an institutionalized person, his or her community spouse, or hisor her representative to disclose information or to name the State as aremainder beneficiary as provided for in subsection (b)(1) of this Section,or to disclose sufficient information regarding an annuity in order toestablish eligibility for long term care services, sh<strong>all</strong> result in denial ortermination of the eligibility. Failure of an institutionalized person, his orher community spouse or his or her representative to disclose theinformation provided for in subsection (b)(1) of this Section, or to disclosesufficient information regarding an annuity in order to establish eligibilityfor medical assistance, may also result in denial or termination ofeligibility for failure to cooperate under Section 120.308.c) Home Equity Interest.1) Effective November 1, 2011, a person sh<strong>all</strong> not be eligible for long termcare services if the person's equity interest in his or her homestead exceeds$750,000. <strong>This</strong> amount sh<strong>all</strong> be increased, beginning with 2011, fromyear to year based on the percentage increase in the consumer price indexfor <strong>all</strong> urban consumers (<strong>all</strong> items: United States city average), rounded tothe nearest $1000. A person's equity interest in his or her homestead sh<strong>all</strong>be determined as follows:
<strong>JCAR890120</strong>-<strong>1011664r08</strong>2534253525362537253825392540254125422543254425452546254725482549255025512552255325542555255625572558255925602561256225632564256525662567256825692570257125722573257425752576The is A) The current market value (CMV) of the property is thegoing price for which it can reasonably be expected to sell on theopen market in the particular geographic area involved. The CMVof the property may be established by:i) an appraisal report, no more than six months old at the timeof the application for long term care services, completed byan appraiser who is licensed or otherwise meets therequirements under the Real Estate Appraiser LicensingAct [225 ILCS 458]; orii) a county real estate assessor's current estimate of themarket value or fair cash value of the property used indetermining the assessed value of a property; oriii) any other reliable and verifiable indicia of the price that aproperty would bring in a sale between a willing buyer andseller under arms-length conditions unaffected by unduepressures;B) Equity value (EV) is the CMV of the property minus anyencumbrance on it;C) An encumbrance is a leg<strong>all</strong>y binding debt against a specificproperty. Such a debt reduces the value of the encumberedproperty but does not necessarily prevent the property owner fromtransferring ownership (selling) to a third party. However, if theowner of encumbered property does sell, the creditor will nearlyalways require debt satisfaction from the proceeds of sale.Examples of encumbrances include mortgages, reverse mortgages,home equity loans or other debt that is secured by the property;D) If property is held in any form of shared ownership (e.g., jointtenancy, tenancy in common or other similar arrangement) only thefractional interest in the property sh<strong>all</strong> be considered indetermining the person's equity in that property.2) The eligibility of a person for long term care services sh<strong>all</strong> not be affectedunder this subsection (c)(2) if any of the following are lawfully residing inthe person's home:A) the person's spouse;
<strong>JCAR890120</strong>-<strong>1011664r08</strong>2577257825792580258125822583258425852586258725882589259025912592259325942595259625972598259926002601260226032604260526062607260826092610261126122613261426152616261726182619B) the person's child who is under age 21; orC) the person's adult child who is blind (as described in Section120.313 of this Part) or disabled (as described in Section 120.314of this Part).3) A person whose eligibility for long term care services is affected underthis subsection (c) may request a hardship waiver. The process and basisfor requesting such a waiver sh<strong>all</strong> be the same as described in Section120.388(r) of this Part. In determining whether a waiver should begranted, the Department sh<strong>all</strong> also take into account:A) the amount of time the person has resided in and owned the home;B) whether a substantial increase in property values in the home'sgeographic area occurred after the person purchased the home;C) whether the home comprises a substantial portion of the person'sassets (as defined in Section 120.388(d)); andD) whether the person intends to return to the home after a period ofinstitutionalization or, if the person does not intend to return,whether the home can be sold after being listed for sale or, if itcannot be sold, can produce income commensurate with similarincome producing properties in the geographic area.4) For purposes of this Section the words, "homestead" and "home" have thesame meaning as the term "homestead" in Section 120.381(a)(1)(A) of thisPart.(Source: Amended at 35 Ill. Reg. ______, effective ____________)Section 120.387 Property Transfers Occurring On or After August 11, 1993 and BeforeNovember 1, 2006a) The provisions for the transfer of property (for example, assets) listed insubsection (e)below only apply to institutionalized persons when the transferoccurs on or after August 11, 1993 and before November 1, 2006 or to personswho applied for or whose application for long term care assistance was filed orapproved prior to November 1, 2011. An institutionalized person is defined as aresident of a long term care facility, including a resident who was living in thecommunity at the time of the transfer, and to individuals who but for theprovisionprovisions of home and community-based services under Section 4.02
<strong>JCAR890120</strong>-<strong>1011664r08</strong>2620262126222623262426252626262726282629263026312632263326342635263626372638263926402641264226432644264526462647264826492650265126522653265426552656265726582659266026612662of the Illinois Act on the Aging would require the level of care in a long term carefacility. An institutionalized person also <strong>includes</strong> an individual receiving homeand community-based services under Section 4.02 of the Illinois Act on the Agingwho was not receiving these services at the time of the transfer.b) The provisions for the transfer of property (e.g.for example, assets) listed insubsection (e)below apply to the transfer of property by the institutionalizedperson's spouse in the same manner as if the institutionalized person transferredthe property.c) Transfers of property disregarded as a result of payments made by a Long TermCare Partnership Insurance Policy (as described in 50 Ill. Adm. Code 2018) arenot subject to the provisions of this Section.d) A transfer of assets occurs when an institutionalized person or an institutionalizedperson's spouse buys, sells or gives away real or personal property or changes (forexample, change from joint tenancy to tenancy in common) the way property isheld. Changing ownership of property to a life estate interest is an asset transfer(the value of the life estate and remainder interest is determined as described atSection 120.380 and 89 Ill. Adm. Code 113.140). For assets held in jointtenancy, tenancy in common or similar arrangement, a transfer occurs when anaction by any person reduces or eliminates the person's ownership or control ofthe asset. A transfer occurs when an action or actions are taken thatwhich wouldcause an asset or assets not to be received (e.g.for example, waiving the right toreceive an inheritance).e) A transfer is <strong>all</strong>owable if:1) depending on the property transferred, the transfer occurred more thaneither 60 or 36 months before the date of application, or more than either60 or 36 months before entry into a long term care facility or more thaneither 60 or 36 months before receipt of services provided by the IllinoisDepartment on Aging under the In-Home Care Program (as described in89 Ill. Adm. CodeSection 140.643);A) the 60 month period applies to payments from a revocable trustthat are not treated as income (as described in Section 120.347)and to portions of an irrevocable trust from which no paymentscould be made (as described in Section 120.347);B) the 36 month period applies to payments from an irrevocable trustthat are not treated as income (as described in Section 120.347)and to any other property transfers not identified in this subsection;
<strong>JCAR890120</strong>-<strong>1011664r08</strong>26632664266526662667266826692670267126722673267426752676267726782679268026812682268326842685268626872688268926902691269226932694269526962697269826992700270127022703270427052) a fair market value was received. Fair market value is the price that anarticle or piece of property might be expected to bring if offered for sale ina fair market. Fair market value is determined by statements obtainedfrom institutions, community members, etc. (e.g.for example, bankers,jewelers, reputable realtors, etc.) recognized as having knowledge ofproperty values;3) homestead property was transferred to:A) a spouse;B) the person's child who is under age 21;C) the person's child who is blind (as described in Section 120.313) ordisabled (as described in Section 120.314);D) the person's brother or sister who has an equity interest in thehomestead property and who was residing in the home for at leastone year immediately prior to the date the person becameinstitutionalized; orE) the person's child who provided care for the person and who wasresiding in the homestead property for two years immediately priorto the date the person became institutionalized;4) the transfer by the institutionalized person was to the community spouseor to another person for the sole benefit of the community spouse and theamount transferred does not exceed the Community Spouse AssetAllowance (as described in Section 120.379);5) the transfer from the community spouse was to another person for the solebenefit of the community spouse;6) the transfer was to the person's child or to a trust established solely for thebenefit of the person's child who is blind (as described in Section 120.313)or disabled (as described in Section 120.314) or to another person for thesole benefit of the person's child;7) the transfer was to a trust established solely for the benefit of a personunder age 65 who is disabled (as described in Section 120.314);8) the person intended to transfer the assets for fair market value;
<strong>JCAR890120</strong>-<strong>1011664r08</strong>27062707270827092710271127122713271427152716271727182719272027212722272327242725272627272728272927302731273227332734273527362737273827392740274127422743274427452746274727489) it is determined that denial of assistance would create an undue hardship.Examples of undue hardship include, but are not limited to, situations inwhich:A) the individual is ment<strong>all</strong>y unable to explain how the assets weretransferred;B) the denial of assistance would force the resident to move from thelong term care facility; orC) the individual would be prohibited from joining a spouse in afacility or would prohibit the individual from entering a facilitythat is within close proximity to his or her family;10) the transfer was made exclusively for a reason other than to qualify forassistance. A transfer for less than fair market value is presumed to havebeen made to qualify for assistance unless a satisfactory showing is madeto the Department that the client or spouse transferred the assetexclusively for a reason other than to qualify for assistance;11) the transfer by the client was to the community spouse and was the resultof a court order;12) the assets transferred for less than fair market value have been returned tothe person; or13) the transfer was to an annuity, the expected return on the annuity iscommensurate with the estimated life expectancy of the person, and theannuity pays benefits in approximately equal periodic payments. Indetermining the estimated life expectancy of the person, the Departmentsh<strong>all</strong> use the current actuarial tables published by the Office of the ChiefActuary of the Social Security Administrationhttp://www.ssa.gov/OACT/STATS/table4c6.html.life expectancy tabledescribed in Section 120.Table B.f) If a transfer or transfers do not meet the provisions of subsection (e), the client issubject to a period of ineligibility for long term care services and for servicesprovided by the Illinois Department on Aging under the In-Home Care Program(as described in Section 140.643). The penalty period is determined inaccordance with subsection (g) of this Section. If otherwise eligible, clientsremain entitled to other covered medical services.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>274927502751275227532754275527562757275827592760276127622763276427652766276727682769277027712772277327742775277627772778277927802781278227832784278527862787278827892790g) A separate penalty period is determined for each month in which a transfer ortransfers do not meet the provisions of subsection (e) of this Section. Each penaltyperiod is the number of months equal to the total uncompensated amount of assetstransferred during a month divided by the monthly cost of long term care at theprivate rate.h) The penalty period begins with the month of the transfer or transfers unless thetransfer or transfers occurred during a previous penalty period. If so, the penaltyperiod begins with the month following the month the previous penalty periodends.i) For transfers by the community spouse that result in a penalty period as describedin subsection (g) of this Section and the community spouse becomes aninstitutionalized person and is otherwise eligible for assistance, the Departmentsh<strong>all</strong> divide any remaining penalty period equ<strong>all</strong>y between the spouses.(Source: Amended at 35 Ill. Reg. ______, effective ____________)Section 120.388 Property Transfers Occurring On or After November 1, 2006The provisions in this Section are intended to comport with federal requirements related totransfers of assets, in particular, requirements under 42 USC 1396p and guidance from the USDepartment of Health and Human Services related to those statutory requirements.Interpretation and application of this Section sh<strong>all</strong> be made in light of those requirements.a) General. A transfer of assets for less than fair market value made on or afterNovember 1, 2006 by an institutionalized person or the spouse of that personwithin 60 months before the later of applying for medical assistance ortransferring an asset sh<strong>all</strong> result in a period of ineligibility for long term careservices for that person.b) Long term care services are defined as:1) services provided in a long term care facility as that institution is definedin Section 120.61(a); and2) services provided under a home and community based waiver authorizedunder 42 USC 1396n(c) or (d) and specified in 42 CFR 441 Subpart G orH.c) Institutionalized individuals or persons are defined as:
<strong>JCAR890120</strong>-<strong>1011664r08</strong>27912792279327942795279627972798279928002801280228032804280528062807280828092810281128122813281428152816281728182819282028212822282328242825282628272828282928302831283228331) persons residing in long term care facilities, including those who wereresiding in the community at the time a transfer of assets was made; or2) persons who, but for the provision of home and community based waiverservices (42 USC 1396a(a)(10)(A)(ii)(VI)), would require the level of carein a long term care facility, including those persons receiving home andcommunity based waiver services who were not receiving the services atthe time a transfer of assets was made.d) Assets.1) For purposes of this Section, the term "assets" or "property" <strong>includes</strong> <strong>all</strong>income (as defined in 42 USC 1382a) and resources (as defined in 42 USC1382b, except subsection (a)(1) of that section, which excludes the homeas a resource) of an institutionalized person and that person's spouse,including, but not limited to: cash; savings certificates; stocks; bonds;interests in real property, including mineral rights; rights to inherited realor personal property or income; and accounts and debts receivable.2) Assets also include any income or resources that the person or the person'sspouse is entitled to but does not receive because of action or inaction by:A) the person or the person's spouse;B) a person, including a court or administrative body, with legalauthority to act in place of or on behalf of the person or theperson's spouse;C) any person, including any court or administrative body, acting atthe direction or upon the request of the person or the person'sspouse; orD) any person who acted (or failed to act) to avoid receiving assets towhich the person was entitled.3) Examples of actions that would cause assets not to be received include:A) Irrevocably waiving pension income;B) Waiving the right to receive an inheritance;C) Not accepting or accessing injury settlements;
<strong>JCAR890120</strong>-<strong>1011664r08</strong>283428352836283728382839284028412842284328442845284628472848284928502851285228532854285528562857285828592860286128622863286428652866286728682869287028712872287328742875D) Arranging for a defendant in a civil action to divert a settlementamount into a trust or similar device for the benefit of the person,who is a plaintiff in the case;E) Refusing to take legal action to obtain a court-ordered paymentthat is parti<strong>all</strong>y or wholly unpaid, such as alimony; orF) Receiving an inheritance under a will when renouncing the willand taking a statutory share (see 755 ILCS 5/2-8) is moreadvantageous. Alternately, renouncing a will and taking astatutory share when taking the inheritance is more advantageous.4) Failure to take action to receive an asset is not considered a transfer forless than fair market value when evidence is submitted showing the cost ofobtaining an asset exceeds the value of the asset.e) Transfer. A transfer of assets occurs when an institutionalized person or aninstitutionalized person's spouse buys, sells or gives away real or personalproperty or changes (e.g., a change from joint tenancy to tenancy in common) theway property is held.1) Changing ownership of property to a life estate interest is an asset transfer(the value of the life estate and remainder interest is determined asdescribed in Section 120.380(i) and 89 Ill. Adm. Code 113.140(e)).2) Transactions involving annuities, including the purchase of an annuity orany action by a person that changes the course of payments to be made bythe annuity or the treatment of income or principal of the annuity, areconsidered transfers under this Section. Such actions include, but are notlimited to, additions of principal, elective withdrawals, requests to changethe distribution of the annuity, elections to annuitize the contract and anyaction intended to make an annuity irrevocable or nonassignable.3) For property held in joint tenancy, tenancy in common or similararrangement, a transfer occurs when an action by any person reduces oreliminates the person's ownership or control of the property.4) A transfer of income in the month it is received is considered a transfer ofassets if the income would have been considered an asset in the followingmonth as provided under Section 120.380(c)(1). A transfer of theproceeds of a loan in the month received is considered a transfer of assets.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>2876287728782879288028812882288328842885288628872888288928902891289228932894289528962897289828992900290129022903290429052906290729082909291029112912291329142915291629172918f) Fair market value (FMV) is an estimate of the value of an asset if sold at theprevailing price at the time it was actu<strong>all</strong>y transferred. Prevailing price is whatproperty would sell for on the open market between a willing buyer and a willingseller, with neither being required to act and both having reasonable knowledge ofthe relevant facts.1) In determining if FMV has been received for an asset, the Departmentsh<strong>all</strong> use <strong>all</strong> reasonable means available and consider <strong>all</strong> relevant facts andcircumstances relating to the asset and the transaction, including, but notlimited to: the cost or price paid for the asset, whether the transaction wasat arm's length, comparable sales, replacement cost, and expert opinion.In determining the FMV of farmland in Illinois, the Department may takeinto account market values determined under methodologies developed bythe University of Illinois College of Agricultural, Consumer andEnvironmental Sciences.2) For an asset to be considered transferred for FMV, the compensationreceived for the asset must be in a tangible form with intrinsic value that isroughly equivalent to or greater than the value of the transferred asset.3) Transfers of assets for "love and affection" are not considered transfers forFMV. A transfer to a friend, family member or relative for care providedfor free in the past is a transfer of assets for less than FMV. TheDepartment presumes that services, care or accommodations rendered to aperson by a friend or family member are gratuitous and withoutexpectation of compensation. <strong>This</strong> presumption may be rebutted bycredible documentary evidence that preexists the delivery of the care,services or accommodations showing the type and terms of compensationand contemporaneous receipts, logs or other credible documentationshowing actual delivery of the care or services claimed. Compensationpaid in excess of prevailing rates for similar care, services oraccommodations in the community sh<strong>all</strong> be treated as a transfer for lessthan FMV.4) "Compensation received" is the amount of money or value of any propertyor services received in return for the institutionalized person's assets. Thecompensation received may be in the form of:A) Cash;B) Other assets such as promissory notes, stocks, bonds, and both realestate contracts and life estates that are evaluated over an extendedtime period;
<strong>JCAR890120</strong>-<strong>1011664r08</strong>291929202921292229232924292529262927292829292930293129322933293429352936293729382939294029412942294329442945294629472948294929502951295229532954295529562957295829592960C) Discharge of a debt;D) Prepayment of a bona fide and irrevocable contract, such as amortgage, shelter lease, loan or prepayment of taxes;E) Services; andF) Any other act, object, service or other benefit that has tangible orintrinsic economic value to the person.5) The term "uncompensated value" means the difference between the FMVof a transferred asset (less any outstanding loans, mortgages, or otherencumbrances on the asset) and the actual compensation received. Onlythe uncompensated value of a transferred asset is subject to the penaltyprovisions described in this Section.g) Look Back Period. The provisions of this Section apply to any asset transfersoccurring on or after November 1, 2006, and before the date on which the personis an institutionalized person (as defined in subsection (c) of this Section) and hasapplied for medical assistance.h) Penalty. If a person transfers assets for less than fair market value, the person issubject to a period of ineligibility for long term care services. The penalty periodis determined in accordance with subsection (j) of this Section. If otherwiseeligible, persons subject to a penalty remain eligible for <strong>all</strong> covered medicalservices except long term care services.i) Penalty Period.1) A penalty period under this Section:A) begins with the later of:i) the first day of a month during which a transfer for lessthan FMV is made; orii) the date on which the person is eligible for medicalassistance and would otherwise be receiving long term careservices (based on an approved application for thoseservices) were it not for the imposition of the penaltyperiod. A person is not considered eligible and services are
<strong>JCAR890120</strong>-<strong>1011664r08</strong>2961296229632964296529662967296829692970297129722973297429752976297729782979298029812982298329842985298629872988298929902991299229932994299529962997299829993000300130023003not considered capable of being received under thissubsection (i) until any spenddown is met; andB) does not occur during any other period of ineligibility under thisSection.2) A notice of penalty period sh<strong>all</strong> include a statement that the person mayappeal the penalty period pursuant to 89 Ill. Adm. Code 102.80.j) Penalty Calculation. A penalty period is determined based on the uncompensatedvalue of transfers. The penalty period is calculated by dividing the totaluncompensated value of assets transferred by the average monthly cost of longtermcare services at the private rate in the community in which the person isinstitutionalized at the time of application. The result is the penalty period innumber of months, days and portion of a day (e.g., $65,000/$4000 = 16.25 = 16months and 7.5 days). The Department will not round down or otherwisedisregard any period of ineligibility calculated under this subsection.k) Multiple Transfers. Multiple, non-<strong>all</strong>owable transfers made during the look-backperiod sh<strong>all</strong> be cumulated and treated as a single transfer. A single period ofineligibility sh<strong>all</strong> be calculated based on the total uncompensated value of thetransfers. Once a penalty period is imposed, it continues to run without regard towhether the person continues receiving long term care services.l) When transfers by a community spouse result in a penalty period for theinstitutionalized spouse and the community spouse subsequently becomesinstitutionalized and is otherwise eligible for medical assistance, the Departmentsh<strong>all</strong> divide any remaining penalty period equ<strong>all</strong>y between the spouses. If onespouse predeceases the other before the penalty period has ended, the remainingpenalty period will be added to the surviving spouse's penalty.m) A person sh<strong>all</strong> not be subject to a penalty period under this Section to the extentthat:1) homestead property was transferred to:A) the person's spouse;B) the person's child who is under age 21;C) the person's child who is determined blind (as described in Section120.313) or determined disabled (as described in Section 120.314);
<strong>JCAR890120</strong>-<strong>1011664r08</strong>300430053006300730083009301030113012301330143015301630173018301930203021302230233024302530263027302830293030303130323033303430353036303730383039304030413042304330443045D) the person's brother or sister who has an equity interest in thehomestead property and who was residing in the home for at leastone year immediately prior to the date the person becameinstitutionalized; orE) the person's son or daughter who provided care for the person andwho resided in the homestead property for the two yearsimmediately prior to the date the person became institutionalizedprovided credible tangible evidence is presented that:i) shows the person was in need of care that would haveotherwise required an institutional level of care. Theevidence may consist of a physician's statement or anevaluation conducted by a medical professional showingthe need for an institutional level of care. A diagnosis ofAlzheimer's or other dementia related illness sh<strong>all</strong> be primafacie evidence of a need for an institutional level of care;andii) shows the son or daughter resided with the person for twoyears immediately prior to the person's institutionalization.The evidence may consist of tax returns, driver's license,cancelled checks or other documentation demonstratingresidence in the home for at least two years prior to theparent's institutionalization; andiii) shows the son or daughter provided care to the person thatprevented institutionalization. The evidence may consist ofsworn affidavit or statement signed by the son or daughter.2) the transfer:A) by the institutionalized person was to:i) the person's spouse or to another person for the sole benefitof the person's spouse;ii) the person's child or to a trust (including a trust described inSection 120.347(d)) established solely for the benefit of theperson's child or to another person for the sole benefit ofthe institutionalized person's child. To qualify under thissubsection (m)(2)(A)(ii), the child must be determined
<strong>JCAR890120</strong>-<strong>1011664r08</strong>3046304730483049305030513052305330543055305630573058305930603061306230633064306530663067306830693070307130723073307430753076307730783079308030813082308330843085308630873088blind (as described in Section 120.313) or determineddisabled (as described in Section 120.314);iii) a trust (including trusts described in Section 120.347(d)(1)and (2)) established solely for the benefit of a person whois determined disabled (as described in Section 120.314).B) for purposes of this Section, is considered to be for the "solebenefit of" a person if:i) the transfer is arranged in such a way that no person orentity except the specified beneficiary can benefit from theproperty transferred in any way, whether at the time of thetransfer or at any time in the future.ii) the transfer to the trust (described in Section 120.347)benefits no one but the person, whether at the time the trustis established or at any time in the future.iii) the transfer instrument or document provides for thespending of the funds involved for the benefit of the personon a basis that is actuari<strong>all</strong>y sound, based on the lifeexpectancy of the person involved (as determined undercurrent actuarial tables published by the Office of the ChiefActuary of the Social Security Administrationhttp://www.ssa.go/OACT/STAT/table4c6.html). <strong>This</strong>subsection (m)(2)(B)(iii) does not apply to trusts describedin Section 120.347(d) because those trusts provide for a"payback" to the State upon the death of the beneficiary.iv) the transfer was accomplished via a written instrument oftransfer (e.g., a trust document) that leg<strong>all</strong>y binds theparties to a specified course of action and clearly sets outthe conditions under which the transfer was made, as wellas who can benefit from the transfer. A transfer withoutsuch a document may not be said to have been made for thesole benefit of the person since there is no way to establish,without the document, that only the specified person willbenefit from the transfer.3) the person intended to transfer the property for fair market value (FMV).When a transfer is made for less than FMV, a person is presumed to havedone so intention<strong>all</strong>y. <strong>This</strong> presumption may be rebutted by objective
<strong>JCAR890120</strong>-<strong>1011664r08</strong>3089309030913092309330943095309630973098309931003101310231033104310531063107310831093110311131123113311431153116311731183119312031213122312331243125312631273128312931303131tangible evidence of the following (a subjective statement of intent orclaim of ignorance of the asset transfer provision is not sufficient):A) initial and continuing reasonable, good faith efforts to sell theproperty on the open market were made and that the compensationreceived was the best value offered;B) a leg<strong>all</strong>y binding contract was executed that provided for adequatecompensation in a specified form (e.g., goods, services, cash) inexchange for the transferred asset;C) the person acted in good faith that he or she was receiving FMV orthe best price for the item or property, and the item or property wastransferred to a person other than a related party (e.g., a personrelated by blood, marriage or friendship);D) the person had other adequate means or plans for support, includingmedical care, at the time of the transfer.4) the transfer was made exclusively for a reason other than to qualify orremain eligible for medical assistance. A transfer for less than FMV ispresumed to have been made to qualify for assistance. <strong>This</strong> presumptionmay be rebutted by credible tangible evidence that the person or spousehad no reason to believe that Medicaid payment of long term care servicesmight be needed. The sudden loss of income or assets, the sudden onsetof a disabling condition, such as a stroke or Alzheimer's disease, or apersonal injury may provide convincing evidence that there was no reasonto anticipate a need for long term care assistance. A subjective statementof intent or claim of ignorance of the asset transfer provision is notsufficient. Other examples of credible evidence showing a reason fortransferring assets for reasons other than to qualify or remain eligible formedical assistance include, but are not limited to:A) police reports, other related law or regulatory enforcement reports,documentation from the Department on Aging, or like credibleevidence that assets were misappropriated as a result of elder orother abuse and cannot be recovered;B) evidence that the transfer was made by a person lacking the mentalcapacity to make the transfer and who was not represented by aguardian, family member or other legal representative at the timeof the transfer.
<strong>JCAR890120</strong>-<strong>1011664r08</strong>3132313331343135313631373138313931403141314231433144314531463147314831493150315131523153315431553156315731583159316031613162316331643165316631673168316931703171317231733174C) evidence that the transfers were for everyday living expenses,incidental gifts to family members, or contributions to charities orreligious organizations made on a consistent basis over a period oftime (not only in close proximity to applying for assistance).These expenses sh<strong>all</strong> be reviewed taking into account theindividual circumstances of a particular transfer and applying anobjective standard based on whether a reasonable person wouldhave made the transfer unmotivated by an intent to qualify forassistance; andD) other evidence pertinent to the person's circumstances at the timeof the transfer relating to:i) the person's physical and mental condition;ii) the person's financial situation;iii) the need for medical assistance;iv) any changes in living arrangements;v) the length of time between the transfer and application formedical assistance; orvi) whether unexpected events occurred between the transferand application.5) the person transfers property disregarded as a result of payments made bya qualified long term care insurance policy approved by the Director of theIllinois Department of Insurance under the Qualified Long Term CareInsurance Partnership (QLTCIP) program (50 Ill. Adm. Code 2012).6) the assets transferred for less than FMV have been returned to the person.A) For transfers occurring prior to November 1, 2011, if only part ofan asset is returned, a penalty period can be reduced but noteliminated. For example, if only half the value of the asset isreturned, the penalty period can be reduced by one half.B) For transfers occurring on or after November 1, 2011, <strong>all</strong> of theassets transferred for less than FMV must have been returned tothe person. Full or partial returns occurring prior to imposition of apenalty reduce the uncompensated portion of the transfer by the
<strong>JCAR890120</strong>-<strong>1011664r08</strong>3175317631773178317931803181318231833184318531863187318831893190319131923193319431953196319731983199320032013202320332043205320632073208320932103211321232133214321532163217amount returned. Once a penalty is imposed it may only beeliminated if <strong>all</strong> assets transferred for less than FMV are returned.When <strong>all</strong> transferred assets are returned, the assets are treated asreturned on the date the penalty was imposed; the penalty is erasedand the returned assets are treated as available as of the date thepenalty was imposed. For the time period between imposition ofthe penalty and return of the assets, the Department will treat theassets as available to meet the spenddown obligation for that timeperiod only (see Section 120.384). At the point in time that assetsare in fact returned, they are treated as available assets that may bereduced by a spenddown obligation or otherwise. Returned assetsthat are transferred for less than FMV may be subject to penalty.7) the Department determines that the denial of eligibility would cause anundue hardship as provided in subsection (r) of this Section.n) The purchase of an annuity by or on behalf of an institutionalized person or thespouse of that person sh<strong>all</strong> be treated as a transfer of assets for less than FMVunless:1) the annuity names the State of Illinois as the remainder beneficiary in thefirst position for at least the total amount of medical assistance paid onbehalf of the institutionalized person; or2) the annuity names the State of Illinois in the second position after thecommunity spouse or minor child or child with a disability and is namedin the first position if the spouse or a representative of the child disposesof any remainder for less than FMV.o) The purchase of an annuity by or on behalf of an institutionalized person sh<strong>all</strong> betreated as a transfer of assets for less than FMV unless:1) the annuity is considered either:A) an individual retirement annuity described in section 408(b) of theInternal Revenue Code (26 USC 408(b)); orB) a deemed individual retirement account (IRA) under a qualifiedemployer plan described in section 408(q) of the Internal RevenueCode (26 USC 408(q)); or2) the annuity is directly purchased with proceeds from one of the following:
<strong>JCAR890120</strong>-<strong>1011664r08</strong>3218321932203221322232233224322532263227322832293230323132323233323432353236323732383239324032413242324332443245324632473248324932503251325232533254325532563257325832593260A) a traditional IRA described in section 408(a) of the InternalRevenue Code (26 USC 408(a));B) certain accounts or trusts treated as traditional IRAs under section408(p) of the Internal Revenue Code (26 USC 408(p));C) a simplified employee pension described in section 408(k) of theInternal Revenue Code (26 USC 408(k)); orD) a Roth IRA described in section 408A of the Internal RevenueCode (26 USC 408A); or3) the annuity meets <strong>all</strong> the following requirements:A) was purchased from a commercial financial institution or insurancecompany authorized under federal or State law to issue annuities;B) is actuari<strong>all</strong>y sound and based on the estimated life expectancy ofthe person (as determined under current actuarial tables publishedby the Office of the Chief Actuary of the Social SecurityAdministration at http://www.ssa.gov/OACT/STATS/table4c6.html);C) is irrevocable and nonassignable; andD) pays benefits in approximately equal periodic payments no lessthan quarterly, with no deferred or b<strong>all</strong>oon payments.p) Life Estates. The purchase of a life estate interest in another person's home sh<strong>all</strong>be treated as a transfer for less than FMV unless the purchaser resided in thehome for at least 12 consecutive months after the date of the transfer. If thepurchaser resided in the home for less than 12 consecutive months, the entirepurchase amount will be considered a transfer for less than FMV.q) Promissory Notes, Loans and Mortgages. The purchase of a promissory note, loanor mortgage by a person sh<strong>all</strong> be treated as a transfer of assets for less than FMVunless the following conditions are met (a promissory note, loan, or mortgage thatdoes not satisfy these conditions sh<strong>all</strong> be valued based on the outstanding balancedue the person under the instrument as of the later of the date of application formedical assistance or the date of the transfer):1) a written instrument recording the transaction is executed, signed anddated on the effective date of the transaction;
<strong>JCAR890120</strong>-<strong>1011664r08</strong>32613262326332643265326632673268326932703271327232733274327532763277327832793280328132823283328432853286328732883289329032913292329332943295329632973298329933003301330233032) the instrument provides for a repayment term that is actuari<strong>all</strong>y sound (asdetermined under current actuarial tables published by the Office of theChief Actuary of the Social Security Administration athttp://www.ssa.gov/OACT/STATS/table4c6.html);3) the instrument provides for payments to be made in equal inst<strong>all</strong>ments (noless than monthly) during the term of the loan with no deferral and nob<strong>all</strong>oon payments;4) the instrument prohibits the cancellation of the balance upon the death ofa lender; and5) a tangible, verifiable record of consistent, timely payments in the amountsprovided under subsection (q)(2) demonstrates a good faith attempt torepay the instrument. Unpaid inst<strong>all</strong>ments delinquent three months ormore will result in the Department treating the amount remaining unpaidon the instrument as a non-<strong>all</strong>owable transfer.r) Hardship Waiver.1) The Department sh<strong>all</strong> waive a penalty period or a portion of a penaltyperiod if it determines that application of a penalty creates an unduehardship. An undue hardship exists when application of a penalty woulddeprive an institutionalized person:A) of medical care, endangering the person's health or life; orB) of food, clothing, shelter, or other necessities of life.2) The person requesting a hardship waiver sh<strong>all</strong> have the burden of proofthat actual, not just possible, hardship exists. The person may providewritten evidence to substantiate the circumstances of the transfer, attemptsto recover the uncompensated value of the transfer, reasons for the transferand the impact of a period of ineligibility for long term care services. Thefollowing criteria sh<strong>all</strong> be considered in determining whether a hardshipwaiver may be granted:A) whether credible and convincing evidence is presented that theperson, in good faith and to the best of his or her ability, has taken<strong>all</strong> equitable and legal means available to recover an asset or assetsthat have been transferred for less than fair market value. In casesinvolving <strong>all</strong>eged theft, fraud, elder abuse or other
<strong>JCAR890120</strong>-<strong>1011664r08</strong>3304330533063307330833093310331133123313331433153316331733183319332033213322332333243325332633273328332933303331333233333334333533363337333833393340334133423343334433453346misappropriation of assets, evidence of referrals to the police orother law or regulatory enforcement agencies is required. In casesin which assets have been transferred for less than FMV as a resultof legal, financial or other professional advice, evidence of legalattempts to recover the value of the assets from the professionaladviser may be required;B) the medical condition, mental capacity, financial ability and otherfactors that may have affected the person at the time of thedecision to transfer the assets for less than FMV;C) the denial of assistance would force the person to move; andD) subject to the availability of beds, the person would be prohibitedfrom joining a spouse in a facility or from entering a facility that isin close proximity to his or her family.3) Transfers Between November 1, 2006 and October 31, 2011.A) Notwithstanding the provisions of subsection (r)(2), for transfersoccurring from November 1, 2006 through October 31, 2008, ahardship waiver sh<strong>all</strong> be granted if the applicant signs anattestation form stating that the penalized transfer was made inreliance on the administrative rules in effect at the time of thetransfer and that without a waiver the person faces deprivation ofthe elements described in subsections (r)(1)(A) and (B).B) For transfers occurring from November 1, 2008 through October31, 2011, the portion of a penalty that would have been imposedfrom the date of the transfer under administrative rules existing atthe time of the transfer until October 1, 2011 sh<strong>all</strong> be waived if theapplicant signs an attestation form that the penalized transfer wasmade in reliance on the administrative rules in effect at the time ofthe transfer and that without a waiver the person faces deprivationof the elements described in subsections (r)(1)(A) and (B). Ahardship waiver of any penalty remaining after October 31, 2011sh<strong>all</strong> be determined in accordance with subsection (r)(2).4) A facility in which an institutionalized person is residing may request ahardship waiver on behalf of that person under this subsection (r) providedwritten consent has been obtained from the person if the person is leg<strong>all</strong>ycompetent to give that consent or from the person's personalrepresentative, who may include the person who signed the application for
<strong>JCAR890120</strong>-<strong>1011664r08</strong>3347334833493350335133523353335433553356335733583359336033613362336333643365336633673368336933703371337233733374337533763377337833793380medical assistance on behalf of the resident (see 89 Ill. Adm. Code110.10(c)).s) Records Production. The Department or its agent may request any and <strong>all</strong> recordsnecessary to determine the existence and extent of any transfers of property underthis Section. Persons are required to cooperate in providing requested informationand verifications in accordance with Section 120.308. The Department willprovide any needed assistance requested by a person and will use reasonablemeasures requesting records, taking into account the age, significance, relevancyand difficulty of obtaining the records, the medical condition and mental capacityof the person, and other factors that may affect the person's ability to retrieverecords.t) Notice.1) The Department sh<strong>all</strong> issue a notice to any person who is subject to apenalty period not less than 10 days prior to imposition of the penalty. Thenotice sh<strong>all</strong> inform the person of the period of ineligibility for long termcare services and include a statement that the person may appeal thedecision to impose a penalty period pursuant to 89 Ill. Adm. Code 102.80.2) A notice of imposition of a penalty period sh<strong>all</strong> inform the person that ahardship waiver under subsection (r) may be requested and that the personor facility in which the person resides may submit in writing (pursuant tosubsection (r)(2)) evidence that a hardship exists. The evidence may besubmitted to the Department, which sh<strong>all</strong> review the information and,based on the criteria under subsection (r), determine whether a hardshipwaiver should be granted. Upon completion of its review, the Departmentsh<strong>all</strong> issue a notice of decision on a request for a hardship waiver that sh<strong>all</strong>include a statement that the person may appeal the decision pursuant to 89Ill. Adm. Code 102.80.(Source: Added at 35 Ill. Reg. ______, effective ____________)
33813382Section 120.TABLE B Life Expectancy (Repealed)MALE<strong>JCAR890120</strong>-<strong>1011664r08</strong>FEMALEAge Life Expectancy Age Life Expectancy0 71.80 0 78.791 71.53 1 78.422 70.58 2 77.483 69.62 3 76.514 68.65 4 75.545 67.67 5 74.566 66.69 6 73.577 65.71 7 72.598 64.73 8 71.609 63.74 9 70.6110 62.75 10 69.6211 61.76 11 68.6312 60.78 12 67.6413 59.79 13 66.6514 58.82 14 65.6715 57.85 15 64.6816 56.91 16 63.7117 55.97 17 62.7418 55.05 18 61.7719 54.13 18 60.8020 53.21 20 59.8321 52.29 21 58.8622 51.38 22 57.8923 50.46 23 56.9224 49.55 24 55.9525 48.63 25 54.9826 47.72 26 54.0227 46.80 27 53.0528 45.88 28 52.0829 44.97 29 51.1230 44.06 30 50.1531 43.15 31 49.1932 42.24 32 48.2333 41.33 33 47.2734 40.23 34 46.3135 39.52 35 45.3536 38.62 36 44.4037 37.73 37 43.45
<strong>JCAR890120</strong>-<strong>1011664r08</strong>38 36.83 38 42.5039 35.94 39 41.5540 35.05 40 40.6041 34.15 41 39.6642 33.26 42 38.7243 32.37 43 37.7844 31.49 44 36.8545 30.61 45 35.9246 29.74 46 35.0047 28.88 47 34.0848 28.02 48 33.1749 27.17 49 32.2750 26.32 50 31.3751 25.48 51 30.4852 24.65 52 29.6053 23.82 53 28.7254 23.01 54 27.8555 22.21 55 27.0056 21.43 56 26.1557 20.66 57 25.3158 19.90 58 24.4859 19.15 59 23.6760 18.42 60 22.8661 17.70 61 22.0662 16.99 62 21.2763 16.30 63 20.4964 15.62 64 19.7265 14.96 65 18.9666 14.32 66 18.2167 13.70 67 17.4868 13.09 68 16.7669 12.50 69 16.0470 11.92 70 15.3571 11.35 71 14.6572 10.80 72 13.9973 10.27 73 13.3374 9.27 74 12.6875 9.24 75 12.0576 8.76 76 11.4377 8.29 77 10.4378 7.83 78 10.2479 7.40 79 9.6780 6.98 80 9.11
<strong>JCAR890120</strong>-<strong>1011664r08</strong>3383338481 6.59 81 8.5882 6.21 82 8.0683 5.85 83 7.5684 5.51 84 7.0885 5.19 85 6.6386 4.89 86 6.2087 4.61 87 5.7988 4.34 88 5.4189 4.09 89 5.0590 3.86 90 4.7191 3.64 91 4.4092 3.43 92 4.1193 3.24 93 3.8494 3.06 94 3.5995 2.90 95 3.3696 2.74 96 3.1697 2.60 97 2.9798 2.47 98 2.8099 2.34 99 2.64100 2.22 100 2.48101 2.11 101 2.34102 1.99 102 2.20103 1.89 103 2.06104 1.78 104 1.93105 1.68 105 1.81106 1.59 106 1.69107 1.50 107 1.58108 1.41 108 1.48109 1.33 109 1.38110 1.25 110 1.28111 1.17 111 1.19112 1.10 112 1.10113 1.02 113 1.02114 0.96 114 0.96115 0.89 115 0.89116 0.83 116 0.83117 0.77 117 0.77118 0.71 118 0.71119 0.66 119 0.66(Source: Repealed at 35 Ill. Reg. ______, effective ____________)