Download Cancer Care Center Annual Report - St. Anthony's ...
Download Cancer Care Center Annual Report - St. Anthony's ...
Download Cancer Care Center Annual Report - St. Anthony's ...
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Cancer</strong> committee membersCommittee LeadershipSarah Beth Snell, M.D., Breast Surgery (Chairman)John Bechtel M.D., Radiation Oncology(Physician Liaison)William Morris M.D., Medical Oncology(Medical Director Oncology Services)Brian Pence, Director of <strong>Cancer</strong> <strong>Care</strong>(<strong>Cancer</strong> Program Administrator)Eric Appelgren, M.D., Executive Vice President,Ambulatory Services, <strong>St</strong>. Anthony’s Medical<strong>Center</strong>Physician Committee MembersMazen AbuAwad M.D., Interventional RadiologyJohn Bechtel M.D., Radiation OncologyRobert Beckman, M.D., General SurgeryEdward Burns, M.D., Palliative <strong>Care</strong>Rama Devabhaktuni, M.D., Family PracticePeter Fonseca, M.D., PhD., Thoracic SurgeryEddy Hsueh, M.D., Surgical OncologyLawrence Kriegshauser, M.D., Orthopedic SurgeryJose Lima, M.D., OtolaryngologyRonna F. Lodato, M.D., PathologyKaruna Murray, M.D., Gyn/OncologyPaul Oberle, M.D., Diagnostic RadiologyJayprakash Patel, M.D., UrologyDavid Schuval, M.D., Colorectal SurgeryEric Sutphen, M.D., Radiation OncologyPaul Young, M.D., Neuro SurgeryNon-Physician Committee MembersGail Behling, Oncology Data Services, QA ofRegistry DataLaura Bub,Education/Community OutreachCoordinatorKevin Dobson, Oncology Data Services, <strong>Cancer</strong>Conference CoordinatorLizzie Huger, Pastoral <strong>Care</strong><strong>St</strong>ephanie Jacobsmeyer, Quality ManagementMichelle Jost, Oncology InpatientJanet Lesko, Oncology ResearchLynn <strong>St</strong>ephan, American <strong>Cancer</strong> SocietyRepresentativeElaine Sharamitaro, OCN, RN, Infusion ServicesRuth Southards, Director HospiceTerri Thompson, Nutrition ServicesRebecca Zickler, Social Worker<strong>Cancer</strong> Oncology Program AdministrationTina Crossland4
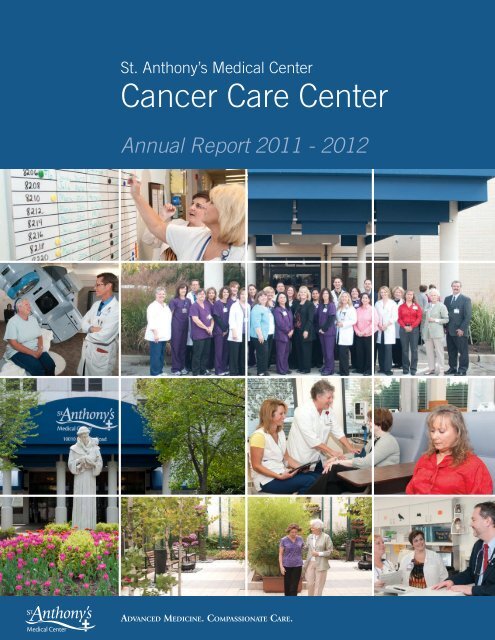
A message from leadership<strong>St</strong>. Anthony’s Medical <strong>Center</strong> became an accredited communitycancer program in 2010 from the Commission on <strong>Cancer</strong> of theAmerican College of Surgeons. We area now eagerly approachingour first re-certification visit in August 2013. This will allow us toshowcase the quality community cancer care we offer at <strong>St</strong>. Anthony’s<strong>Cancer</strong> <strong>Care</strong> <strong>Center</strong>.<strong>Cancer</strong> care at <strong>St</strong>. Anthony’s involves multiple specialties. Thisis a true team approach from all aspects. This involves not onlysurgery, medical oncology, and radiation oncology; but many otherspecialized disciplines of medicine. The spotlight cancer this yearchosen by the <strong>Cancer</strong> Committee was colorectal cancer and involvedthe goal/use of preoperative staging of rectal cancer with rectalMRI. This is a new technology to allow for appropriate patients toreceive preoperative chemotherapy with radiation to allow for betteroutcomes. This required the radiologist to work with the surgeons toevaluate the appropriate patients and to introduce a new standard inthe preoperative work up. We also worked with pathology and surgeryto make sure that an appropriate number of lymph nodes wereremoved in colorectal cancer patients. This allows the team to provideappropriate post operative treatment and follow up and thereforebetter care.Comprehensive cancer care also involves the cancer registry thatcollects data on all patients to track outcomes. Since our accreditation,abstracting of all cancer patients has remained timely and accurate.Another benefit of an accredited cancer center involves accessto clinical trial specialists that offer patients access to the newesttreatment options close to home, as well as outreach programs thatoffer frequent health screenings and community education. Wealso provide palliative care services and both inpatient and homehospice. This is uncommon in a community cancer program andsomething that we are distinctly proud of. All these services allowpatients first class cancer care in a comfortable community setting.The accreditation also allows <strong>St</strong>. Anthony’s to compare our outcomesto other accredited facilities. We strive to provide improved survivaland quality of life and confirm this with comparing ourselves to otherfacilities of the same size.<strong>St</strong>. Anthony’s provides excellent care in a convenient, communitysetting. With this I am proud to present the annual reportspotlighting colorectal cancer.Sarah Beth Snell, M.D.Sarah Beth Snell M.D., FACSChairman, <strong>Cancer</strong> Committee314-525-15455
A Challenging and Rewarding YearBrian PenceThis has been my third year as Executive Director of Oncology Servicesat <strong>St</strong>. Anthony’s Medical <strong>Center</strong>. I have had the privilege to work for athird year with a terrific group of physicians, nurses, therapists and manyother cancer care professionals as we work together to grow the program.This year we have been involved in a strategic process improvementfor <strong>St</strong>. Anthony’s. The tasks forces associated have successfully met thetargeted cost savings and financial improvements for the organization.This will place us in solid financial grown for future initiatives for thecancer program. An example of new initiatives has been the use of ournew High Dose Rate Brachy-Therapy (HDR) unit for the treatmentof lung cancers in the bronchus as well as certain esophagus tumors. Inboth situations we have an interdisciplinary team of physicians and staffcaring for the patient with quality and efficiency. Pulmonologists andGI doctors come directly to the cancer center to work with our radiationoncologists so we do not need to transport the patient from one clinic toanother. It is a terrific example of interdisciplinary care.The outpatient infusion center cares for more and more patients eachyear, delivering treatments for not just cancer but many other diseasesas well. Approximately 60 percent of our patients cared for in OPinfusion have a cancer diagnosis. The other 40 percent have other healthconcerns.Approximately 1,317 new cancers were diagnosed at <strong>St</strong>. Anthony’sMedical <strong>Center</strong> in 2011. This was a smaller number of patientsdiagnosed in 2012, which was 1,486. While the number of patientsdiagnosed declined, the number of patients who received treatmentfor cancer at <strong>St</strong>. Anthony’s increased. Our interdisciplinary care offersthe opportunity for patients to have a streamlined and efficient accessto all of the oncology therapies in order to tailor treatment to theirindividualized needs. The cancer center met all of its quality goals for2011 including excellent patient satisfaction and employee satisfactionscores.We look forward to working with our medical oncologists in 2013to create and implement clinical pathways for the <strong>Cancer</strong> <strong>Care</strong> <strong>Center</strong>.Clinical pathways are the stepping stone for outcomes-based medicineand our team of physicians will continue to be engaged in the creationof pathways for all of the primary cancers diagnosed in our community.This approach assures not just the success of treatment delivery butmeasures the positive effect of an inter-disciplinary approach to cancercare. The goal will be to provide patients and the community withmeasured results of the quality care this is provided.We look forward to meeting the oncology needs of our community.We are here to provide quality care in a compassionate and comfortablesetting. Warmest regards.Brian PenceExecutive Director, <strong>Cancer</strong> <strong>Care</strong> <strong>Center</strong>314-525-40636
A message from leadershipThe <strong>St</strong>. Anthony’s Colorectal <strong>Cancer</strong> <strong>Care</strong> Team is comprised ofa group of premier oncologic specialists with research-based expertisein colorectal cancer. Colorectal cancer is the second most commoncause of death from cancer in the U.S. today. Cure rates are increasingyearly with improvements in treatment, but more Americans need tohave their colonoscopies performed on a regular basis to exert a biggerimpact on this disease.90 percent of colon cancers occur after the age of 50. Most of thesecancers evolve from benign polyps, which grow into benign adenomas(or gland tumors). Over time (usually 10 years or so), both raised andflat adenomas can turn into cancer. Early detection and removal ofthese pre-malignant tumors can prevent colon cancer and save manylives.Risk factors for colorectal cancers include smoking, eating redmeat, refined grains and sugar, plus alcohol and obesity. Avoidanceof these lifestyle choices, plus the intake of Vitamin D, folate, andVitamin B6 and aspirin can help prevent this cancer from occurring.The genetic risk for colorectal cancer is relatively low. However,persons with a family history of this disease should inform theirprimary care physician. If a colon cancer is diagnosed by colonoscopy,surgical resection is usually performed first. Surgery includes completeremoval of the involved colon segment along with the local bloodsupply and lymph nodes. Laparoscopic (minor fiberoptic) surgery forcolon cancer is frequently performed at <strong>St</strong>. Anthony’s Medical <strong>Center</strong>.Compared to open abdominal surgery, laparoscopic surgery is just aseffective and often provides a shorter hospital stay with less pain andsimilar cure rates. Laparoscopic procedures at <strong>St</strong>. Anthony’s can beperformed with the da Vinci® Surgical System.Colorectal cancer patients at <strong>St</strong>. Anthony’s are usually seen by amulti-disciplinary care team including specialists in surgical, medical,and radiation oncology. X-rays, scans, pathology and other data areoften reviewed and evaluated at a colorectal cancer conference, wherea “personalized treatment plan” is created by consensus. National<strong>Cancer</strong> Institute clinical trials are sometimes available for therapyin qualifying cases. Early colorectal cancer at <strong>St</strong>. Anthony’s canoften be managed with the Oncotype DX Colon <strong>Cancer</strong> (Gene)Assay, which can help predict the value of adjuvant (or preventive)chemotherapy after surgery. The K-RAS gene mutation study can alsobe exceptionally useful in colon cancer cases with advanced disease todetermine treatment eligibility for cetuximab, a monoclonal antibodyand EGFR inhibitor.Treatment for colorectal cancer at <strong>St</strong>. Anthony’s is designedby stage, according to National Comprehensive <strong>Cancer</strong> Network(NCCN) guidelines:<strong>St</strong>age I: Usually treated by surgery without adjuvantchemotherapy.R. William Morris, M.D., M.B.A.7
<strong>St</strong>age II: Treated by surgical resection, plus adjuvant chemotherapyin cases eligible by the Oncotype DX Colon <strong>Cancer</strong> (Gene) Assay,plus other criteria.<strong>St</strong>age III: <strong>Cancer</strong>s with positive metastatic lymph nodes areusually treated with adjuvant chemotherapy regimens, including 6months of FOLFOX-6 or CAPEOX, in the out-patient setting.<strong>St</strong>age IV: (Including cancers metastatic to the liver, lung andlymph nodes) Is treated with multiple chemotherapy protocols,plus either Avastin or Zaltrap (monoclonal antibodies which inhibitvascular endothelial growth factor, known as VEGF ) or cetuximab(noted above).Patients with a significant response to metastatic disease, (>50percent tumor shrinkage from chemotherapy) can often becomecandidates for surgical resection of small residual tumors by ourliver oncologic surgeon or for Radio-Frequency Ablation (RFA),specifically, high energy thermal treatment. Some patients whoachieve a complete remission status can often enjoy long-term survivaland even cure.<strong>St</strong>age II and III rectal cancers are treated more often withneoadjuvant (pre-surgical) combined chemo-therapy, plus radiationtherapy which offers a distinct therapeutic advantage. High cure ratesare expected after surgery and additional chemotherapy.Metastatic or advanced colorectal cancer patients that do notachieve a complete remission with treatment can frequently bestabilized (in a palliative mode) for two to three or more yearswhile enjoying good quality of life and minimal side effects fromchemotherapy.The <strong>St</strong>. Anthony’s Colorectal <strong>Cancer</strong> <strong>Care</strong> Team, including boardcertifiedoncologic specialists is currently available for “Personalized<strong>Care</strong> Prescriptions” (“PCRx“ ) plans with an opportunity for superioroutcomes and survivals.<strong>St</strong>. Anthony’s Colorectal <strong>Cancer</strong> <strong>Care</strong> is proud of its team and itsachievements and is seeking early stage and advanced colorectal cancerpatients for first and second treatment opinions.R. William Morris, M.D., M.B.A.Medical Director, Oncology Services314-849-60668
Treatment of colorectal cancerColon <strong>Cancer</strong>: Preventable • Treatable • BeatableColorectal cancer is the third most common cancer and the secondmost common cancer killer in the United <strong>St</strong>ates, which, in 2012,is an estimated 143,000 new colorectal cancers and 52,000 deaths.The risk of developing colorectal cancer increases with age. All menand women age 50 and older are at risk of developing colorectalcancer, and should be screened. Those with a personal history ofinflammatory bowel disease or family history of colorectal cancer orpolyps should be screened before age 50.At <strong>St</strong>. Anthony’s Medical <strong>Center</strong>, rectal cancers are treated with ateam approach which includes the colon and rectal surgeon, medicaloncologist and radiation therapist. Radiation therapy is used in mostrectal cancer cases, and in the few instances of colon cancer when it isnot possible, or safe, to surgically remove all of the cancer. Surgeonsworking with the radiation therapists utilize different techniques toallow for the delivery of the maximum appropriate dose of radiationtherapy while minimizing the adverse effects to the surroundingtissues.Current screening methods include one or more of the following:fecal occult blood testing, flexible sigmoidoscopy, double contrastbarium enema and the gold standard - colonoscopy. Colorectal cancerscreening costs, including colonoscopies, are covered by Medicare andnearly all commercial health plans.Colorectal cancer can be cured in up to 90 percent of patientswhen discovered in its early stages. Approximately 40,000 lives ayear could be saved through widespread adoption of colon cancerscreening and early treatment in men and women.Symptoms from colorectal cancer may include any or all of thefollowing: bleeding per rectum, dark black stools, change in stoolcaliber, tenesmus, lower abdominal pain, recent change in bowelhabits towards diarrhea or constipation, and unintentional weightloss. However, most patients identified to have colorectal cancer haveno symptoms. This is why screening is so important.Ten percent of all colorectal cancers are identified in patientsyounger than age 50; therefore, when these patients do present withthe symptoms associated with colorectal cancer, they should beinvestigated thoroughly.Colorectal cancer, like most cancers, is staged at four differentlevels. Each stage carries different treatment recommendations andprognoses. Although staged the same, treatment recommendationsfor colon cancer and rectal cancer are different.<strong>St</strong>age I colorectal cancers are those where the cancer penetratesonly a portion of the bowel wall. Colon resection is the main stay,without any additional therapy, and yields a five-year survival rate of74- 93 percent. <strong>St</strong>age II colorectal cancers invade through most, ifnot all, of the bowel wall or directly invade an adjacent organ. Colonresection provides a significant cure rate with five-year survivalDavid Schuval, M.D.9
etween 59 and 85 percent. However, there is a subset of patientswith stage II cancers who do benefit from adjuvant chemotherapy.<strong>St</strong>age III colorectal cancers exist when cancer is present in one ormore lymph nodes with any level of bowel wall penetration. Colonresection and, in most cases, postoperative chemotherapy yield a fiveyearsurvival rate between 44 and 84 percent depending on the subsetwithin stage III cancers.<strong>St</strong>age IV colorectal cancers are present when cancer hasmetastasized to other locations in the body and has a five-year survivalof 10 percent or less. Surgical resection of the primary cancer site isappropriate in almost all cases. When surgical or radiation therapytreatment can be used to eliminate all metastatic disease, the patient’sfive-year survival may approach 25 percent. Radiation therapy is usedin select cases and chemotherapy is recommended for all.With rectal cancer, preoperative radiographic testing is critical todetermine the proper treatment recommendations. Rectal ultrasoundand, more recently, rectal MRI (which is available at <strong>St</strong>. Anthony’s) areused to identify whether the cancer is stage I, II or III before surgery.<strong>St</strong>age I rectal cancers are treated with surgery alone and yield afive-year survival rate of 70-80 percent. Both stage II and stage IIIrectal cancers are treated most often with preoperative radiation andchemotherapy followed by an appropriate rest period before surgicalresection. In nearly all cases, these patients should receive furtherchemotherapy after healing from their surgery. Five-year survival ratesfor stage II is 50-60 percent and stage III is 30-40 percent.<strong>St</strong>age IV rectal cancers are treated similarly to stage IV coloncancers.All of the latest treatments for colorectal cancer are available at<strong>St</strong>. Anthony’s Medical <strong>Center</strong>. <strong>St</strong>ate-of-the-art surgical treatmentsinclude laparoscopic colectomy and other minimally invasive surgicaltechniques to remove the cancer. Transanal endoscopic microsurgeryis available for select early rectal cancers. This outpatient procedureallows the patient to return to work and a normal lifestyle within afew days. Today, with rare exception, if patients have a rectal cancerthat does not directly invade the anal canal, they can be reassured apermanent colostomy will not be necessary.As described, even when colon and rectal cancers are treatedwith the latest and most sophisticated techniques, some patientswill develop a cancer recurrence. <strong>Care</strong>ful monitoring is critical aftertreatment for a minimum of five years with an appropriate history,physical examination, laboratory evaluations and radiographic testing.When patients have their recurrent cancer detected early, and treatedwith the selective use of surgery, radiation and/or chemotherapy,there is a greater probability for improved quality of life and, in someinstances, cure.10David Schuval M.D. FACS FASCRS
The Pathologist’s Role in the Diagnosis, <strong>St</strong>aging andTreatment of Colorectal <strong>Cancer</strong>Colon and rectal cancers are amongst the most frequent cancersdiagnosed in Americans. These cancers, often considered togetheras colorectal cancer, are one of the most frequent causes of cancerdeaths. Colorectal cancer rates can be decreased, and deaths frommany of these cancers prevented, by screening and surveillanceprograms for early detection and removal of colorectal polyps. Polypsare collections of precancerous cells which represent an overgrowthin abnormal colorectal lining cells. They may be flat or raised abovethe surrounding tissue, and are usually visible via colonoscopy. Smallpolyps may be removed via colonoscopy; larger polyps may requiresurgery for removal. If not removed, over time colorectal polyps mayundergo further changes, including genetic mutations, and becomecancer (carcinoma). Colorectal carcinomas may also be detected bycolonoscopy, and are usually removed (resected) by surgery.Pathologists are physicians who specialize in the diagnosis ofhuman diseases (pathology) by examination of tissue. Pathologistsencounter colorectal polyps and cancers in both endoscopic biopsiesand surgically removed segments of colon and rectum. These tissuesare placed in formalin, a fixative which helps preserve cellular detail,and then examined by the pathologist.Small biopsy specimens are used in their entirety to produce slidesfor microscopic examination. Larger specimens, including colon andrectum removed surgically, are grossly (with the naked eye) examinedand dissected by the pathologist to select the areas of most significancefor microscopic examination. These areas include the tumor or polypitself and its relationship to the edges of surgical resection (margins ofthe specimen). For the polyp or cancer, size, shape, color, consistency,and distance from the margins are noted and documented in thepathology report. The presence or absence of invasion into the bowelwall is also noted. Additional characteristics of any invasion and thestatus of the margins are further classified upon microscopic exam (seebelow).An important feature in the staging of colorectal cancers isthe status of the lymph nodes. These are normal structures in thefat surrounding the colon and rectum, where lymphocytes andinflammatory cells cluster, and where lymphatic channels drain. Theseare typically the sites where colorectal cancers first metastasize, andare therefore important to examine to assess for metastatic colorectalcancer. These lymph nodes must be dissected, or teased out of theirsurrounding fat, by the pathologist. Often lymph nodes are quiteobvious, and may even be enlarged, up to several centimeters (1-2inches), due to inflammation or metastatic cancer. However theselymph nodes may also be quite small or few in number in somecases (eg, smaller specimens, after radiation or chemotherapy, elderly11
Ronna F. Lodato, M.D.patients, rectal site). Tiny nodes may measure only 1-2 millimeters,and these pinpoint structures are challenging for the pathologist to seeand feel in what may be an abundance of fat attached to the colorectalspecimen. It’s important to find all of the lymph nodes and examinethem microscopically for the presence of absence of metastatic cancer.The goal for the surgeon and pathologist for accurate staging is toretrieve at least 12 lymph nodes from all colorectal surgical resections.Once the areas of interest of the colorectal polyp or tumor areselected during gross examination and dissection by the pathologist,the tissue is processed overnight by progressive dehydration, and thenembedded in paraffin wax by histotechnologists in our laboratory.These formalin-fixed, paraffin-embedded tissues are then cut inapproximately 4-5 micron slices and mounted on slides which arethen stained, and examined by the pathologist using a microscope.Polyps are of many types, the two most common of whichare completely benign hyperplastic polyps, and precancerousadenomatous polyps. All are examined carefully to exclude thepresence of carcinoma. Biopsies of carcinomas are also performedendoscopically, and are likewise carefully examined to confirm theendoscopist’s impression of cancer and provide details about themicroscopic appearance in the pathology report.Microscopic examination of the resected colorectal cancerspecimen is a detailed process, and includes creating a report whichclarifies the characteristics of the cancer. These include:• type of cancer (the vast majority of colorectal cancers areadenocarcinomas)• grade or degree of differentiation (how closely the tumorresembles normal colorectal glands)• depth of invasion by the cancer into the colorectal wall (the “T”stage)• presence or absence of lymphatic or vascular invasion• presence or absence of lymph node metastases, their number andsize (the “N” stage)• status of the margins (whether the cancer was completelyremoved)• any other polyps or abnormalities in the specimenIn addition, in patients who have undergone pre-operativechemotherapy and /or radiation therapy, the pathologist assessesfor treatment effect, which provides information on how well thetumor has responded to the treatment. If there is clinical evidenceof metastatic carcinoma beyond the colorectal lymph nodes, thosesites (the most common is the liver) are typically biopsied and thepathologist examines the tumor to ensure it is similar in microscopicappearance to the colorectal cancer. All of this detailed information isincluded in a comprehensive pathology report and to provide detailsfor the treating physicians (surgeon, oncologist, radiation oncologist)12
who use it to craft the appropriate treatment plan for a givenindividual. The pathologic stage of the cancer (I-IV) is a combinationof details about the size and depth of the tumor invasion (rangingfrom T1-4), lymph node metastases (N0-2), and any metastatic canceroutside the nodes (M0-1).Additional pathologic studies performed in our lab may includeimmunohistochemical staining of the cancer using antibodies tocertain substances found on tumor cells. This is to clarify exact tumortype in tumors that appear unusual microscopically. Genetic testingis sometimes performed on tumors to look for mutations that suggestgenetic susceptibility to cancer; these are typically performed atreference pathology laboratories on paraffin blocks from our hospital.At <strong>St</strong>. Anthony’s Medical <strong>Center</strong>, all 6 board certified pathologists,with a combined 100+ years of practice experience, are trainedto diagnose colorectal specimens. We receive about 20 colorectalspecimens a day, including about 120 colorectal cancer surgicalresections each year. We communicate with our clinical colleagueswho treat these patients via pathology reports, telephone calls, andTumor Conferences, where a multidisciplinary team includingsurgeons, medical and radiation oncologists, radiologists andpathologists discuss cancer cases and develop individualized treatmentplans. This ensures we serve our mission, to provide the best care forevery patient, every day.Dr. LodatoRadiation therapy and rectal cancerRadiation therapy has been used in rectal cancer for some time dueto the problem of local recurrences in the operative bed after surgery.The rationale is based on the anatomical considerations of where therectum lies. As opposed to the colon, which is largely intraperitonealfree floating in the abdomen, the rectum represents the transition ofthe intestinal tract out of the abdomen and to the skin surface at theanus. As such, the large colon transitions from a free floating structureto one that passes outside of the lining of the abdomen into an areathat would be considered retroperitoneal surrounded by fat in thepresacral space. The clinical implication is that cancers that invadeinto the muscular wall of the rectum can extend into the perirectal fatand into the lymph nodes nearby, making the risk for local recurrencequite a bit higher than you would see in colon cancer. This beingthe case, radiation therapy can help sterilize any microscopic diseaseremaining after surgery to help maintain control of the disease.Radiation therapy is also commonly given before surgery to decreaselocal recurrences.Early studies in the use of radiation therapy in the postoperativesetting showed an improvement in local control, but not in survival.13
find metastatic lesions. If suspicious areas are identified, CT andUS may be used to as an imaging guide to perform a needle biopsy.MRI is playing a larger role, particularly in the initial staging of rectalcancer. High resolution images of the MRI are used to determineif the cancer has invaded through the wall of the rectum into theadjacent perirectal fat and lymph nodes. This information is veryimportant for the cancer team, who will then decide if chemotherapyor radiation therapy is needed prior to any surgical procedure. All ofthe preoperative imaging and testing is to assure that the patient hasthe best odds of beating the cancer.After the initial staging and treatment, CT, PET, and ultrasoundare used to monitor the cancer. CT and PET can be used to see howwell the cancer is responding to chemotherapy and radiation therapyif metastatic lesions are present. They can also be used to periodicallyexamine the chest, abdomen and pelvis where most of the metastaticor recurrent lesions will be found if they develop. Ultrasound is usedprimarily to evaluate or follow masses in the liver. The surveillance ofthe patient allows the cancer team to diagnose and treat any problemsthat may arise.Paul Oberle, M.D.Diagnostic Radiology314-525-1145Paul Oberle, M.D.15
<strong>Cancer</strong> Treatment & ServicesThe <strong>Cancer</strong> <strong>Care</strong> <strong>Center</strong> at <strong>St</strong>. Anthony’s Medical <strong>Center</strong> providespatients with comprehensive cancer care, utilizing state-of-the-arttechnology, patient-friendly treatment areas and a full scope ofservices, including:• Breast <strong>Center</strong><strong>St</strong>. Anthony’s Breast <strong>Center</strong> is located in the Medical Plazabuilding adjacent to the main hospital campus.• Inpatient Oncology• Outpatient Infusion• Radiation Oncology• Patient Resource <strong>Center</strong>• Oncology Data Services• Pathology• Diagnositc Radiology• <strong>Cancer</strong> Research: At <strong>St</strong>. Anthony’s <strong>Cancer</strong> <strong>Care</strong> <strong>Center</strong>, ourpatients have the opportunity to be considered for cutting-edgeclinical research studies offered conveniently close to home. TheNational <strong>Cancer</strong> Institute (NCI) funds many clinical researchstudies around the nation. We participate in studies with manyNCI sponsored research groups. All research studies are reviewedby <strong>St</strong>. Anthony’s Medical <strong>Center</strong>’s Institutional Review Board(IRB) which has been granted the endorsement of the FederalOffice for Human Research Protections (OHRP), a division ofthe Department of Health and Human Services.Support ServicesAs a full service medical center, <strong>St</strong>. Anthony’s provides a full andcomprehensive scope of health care services to make the cancerjourney easier for patients and their families, including:• Palliative care• Pastoral care services• Social workers to assist families with finances, counseling,transportation, home care, emotional support and more• Educational classes and support groups for patients and families• Nutritional counseling• Lymphedema program• Hospice, in-home and on-campus hospice house• <strong>St</strong>. Anthony’s Senior Services• <strong>St</strong>. Anthony’s Wound Treatment <strong>Center</strong>.16
• Holistic therapies and complementary medicine, such as guidedimagery, massage and meditation• On-site amenities, including chapel, beautiful grounds withoutdoor seating and multiple dining options• Special programs focused on the cancer patient, includingprofessional makeup and hair-styling sessions, wigs and hats, andcertificates for dinner and ice cream treats• Access to literature that addresses all aspects of life during cancertreatment• Senior Service Home Transportation for convenient andeconomical transportation for senior citizens and people withdisabilities.<strong>St</strong>. Anthony’s Medical <strong>Center</strong> employee breastcancer survivors in front of the <strong>Cancer</strong> <strong>Care</strong><strong>Center</strong> (October, 2012).Reaching Out to the CommunityAs the leading health care provider in South <strong>St</strong>. Louis County andJefferson County, as well as <strong>St</strong>. Clair and Monroe Counties in Illinois,<strong>St</strong>. Anthony’s Medical <strong>Center</strong> provides a wide spectrum of services tohelp improve the overall health of our served communities, includingscreenings, support groups and awareness campaigns.Screenings: <strong>St</strong>. Anthony’s Medical <strong>Center</strong> provides screenings forskin cancer, prostate cancer, and head and neck cancer, as well as otherhealth tests and screenings at specially designated events throughoutthe year.Building awareness: <strong>St</strong>. Anthony’s also participates in a numberof national cancer awareness events each year, including: Colorectal<strong>Cancer</strong> Awareness Day, the Great American Smoke-Out, Breast<strong>Cancer</strong> Awareness Month, and <strong>Cancer</strong> Survivors Day.Support Groups: The <strong>Cancer</strong> <strong>Care</strong> <strong>Center</strong> provides supportgroups, co-sponsored by the American <strong>Cancer</strong> Society, including:Man to Man Prostate <strong>Cancer</strong> Support GroupLook Good…Feel Better, a free program that teaches beautytechniques to women cancer patients in active treatmentThe Breast <strong>Cancer</strong> Support Group, a survivorship program forpatients.17
<strong>Cancer</strong> data<strong>Cancer</strong> Site# of PatientsLung 241Breast 218Colorectal 159Prostate 149Melanoma 83Total 850<strong>St</strong>age# of Patients<strong>St</strong>age 0 (in situ) 2<strong>St</strong>age 1 23<strong>St</strong>age 2 32<strong>St</strong>age 3 38<strong>St</strong>age 4 14Unkown 2Total 111Treatment Type # of PatientsNo Treatment 5Surgery Only 67XRT Only 0Chemo Only 4Combo TX 35Total 111Rectal <strong>St</strong>age # of Patients<strong>St</strong>age 1 19<strong>St</strong>age 2 9<strong>St</strong>age 3 10<strong>St</strong>age 4 8Unknown 2Total 48RectalTreatment Type # of PatientsNo Treatment 1Surgery Only 20XRT Only 0Chemo Only 1Combo TX 26Total 4818
Contact us<strong>St</strong>. Anthony’s Medical <strong>Center</strong>314-525-1000Radiation Oncology314-525-1688Outpatient Infusion314-525-1625Research, Clinical Trials314.525.4928Oncology Data Services314-525-1240Pathology314-525-4928Diagnostic Radiology314-525-1145CANCER CARE CENTER10010 Kennerly Road<strong>St</strong>. Louis, MO 63128314-525-1355 • 314-525-1688www.stlouiscancer.org22