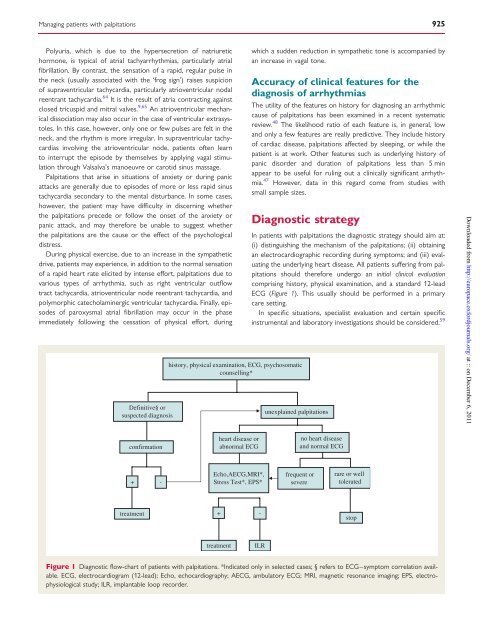
Managing <strong>patients</strong> <strong>with</strong> <strong>palpitations</strong> 925Polyuria, which is due to <strong>the</strong> hypersecretion <strong>of</strong> natriuretichormone, is typical <strong>of</strong> atrial tachyarrhythmias, particularly atrialfibrillation. By contrast, <strong>the</strong> sensation <strong>of</strong> a rapid, regular pulse in<strong>the</strong> neck (usually associated <strong>with</strong> <strong>the</strong> ‘frog sign’) raises suspicion<strong>of</strong> supraventricular tachycardia, particularly atrioventricular nodalreentrant tachycardia. 64 It is <strong>the</strong> result <strong>of</strong> atria contracting againstclosed tricuspid and mitral valves. 9,65 An atrioventricular mechanicaldissociation may also occur in <strong>the</strong> case <strong>of</strong> ventricular extrasystoles.In this case, however, only one or few pulses are felt in <strong>the</strong>neck, and <strong>the</strong> rhythm is more irregular. In supraventricular tachycardiasinvolving <strong>the</strong> atrioventricular node, <strong>patients</strong> <strong>of</strong>ten learnto interrupt <strong>the</strong> episode by <strong>the</strong>mselves by applying vagal stimulationthrough Valsalva’s manoeuvre or carotid sinus massage.Palpitations that arise in situations <strong>of</strong> anxiety or during panicattacks are generally due to episodes <strong>of</strong> more or less rapid sinustachycardia secondary to <strong>the</strong> mental disturbance. In some cases,however, <strong>the</strong> patient may have difficulty in discerning whe<strong>the</strong>r<strong>the</strong> <strong>palpitations</strong> precede or follow <strong>the</strong> onset <strong>of</strong> <strong>the</strong> anxiety orpanic attack, and may <strong>the</strong>refore be unable to suggest whe<strong>the</strong>r<strong>the</strong> <strong>palpitations</strong> are <strong>the</strong> cause or <strong>the</strong> effect <strong>of</strong> <strong>the</strong> psychologicaldistress.During physical exercise, due to an increase in <strong>the</strong> sympa<strong>the</strong>ticdrive, <strong>patients</strong> may experience, in addition to <strong>the</strong> normal sensation<strong>of</strong> a rapid heart rate elicited by intense effort, <strong>palpitations</strong> due tovarious types <strong>of</strong> arrhythmia, such as right ventricular outflowtract tachycardia, atrioventricular node reentrant tachycardia, andpolymorphic catecholaminergic ventricular tachycardia. Finally, episodes<strong>of</strong> paroxysmal atrial fibrillation may occur in <strong>the</strong> phaseimmediately following <strong>the</strong> cessation <strong>of</strong> physical effort, duringDefinitive§ orsuspected diagnosishistory, physical examination, ECG, psychosomaticcounselling*which a sudden reduction in sympa<strong>the</strong>tic tone is accompanied byan increase in vagal tone.Accuracy <strong>of</strong> clinical features for <strong>the</strong>diagnosis <strong>of</strong> arrhythmiasThe utility <strong>of</strong> <strong>the</strong> features on history for diagnosing an arrhythmiccause <strong>of</strong> <strong>palpitations</strong> has been examined in a recent systematicreview. 48 The likelihood ratio <strong>of</strong> each feature is, in general, lowand only a few features are really predictive. They include history<strong>of</strong> cardiac disease, <strong>palpitations</strong> affected by sleeping, or while <strong>the</strong>patient is at work. O<strong>the</strong>r features such as underlying history <strong>of</strong>panic disorder and duration <strong>of</strong> <strong>palpitations</strong> less than 5 minappear to be useful for ruling out a clinically significant arrhythmia.47 However, data in this regard come <strong>from</strong> studies <strong>with</strong>small sample sizes.Diagnostic strategyIn <strong>patients</strong> <strong>with</strong> <strong>palpitations</strong> <strong>the</strong> diagnostic strategy should aim at:(i) distinguishing <strong>the</strong> mechanism <strong>of</strong> <strong>the</strong> <strong>palpitations</strong>; (ii) obtainingan electrocardiographic recording during symptoms; and (iii) evaluating<strong>the</strong> underlying heart disease. All <strong>patients</strong> suffering <strong>from</strong> <strong>palpitations</strong>should <strong>the</strong>refore undergo an initial clinical evaluationcomprising history, physical examination, and a standard 12-leadECG (Figure 1). This usually should be performed in a primarycare setting.In specific situations, specialist evaluation and certain specificinstrumental and laboratory investigations should be considered. 59unexplained <strong>palpitations</strong>Downloaded <strong>from</strong> http://europace.oxfordjournals.org/ at :: on December 6, 2011confirmationheart disease orabnormal ECGno heart diseaseand normal ECG+ -Echo,AECG,MRI*,Stress Test*, EPS*frequent orsevererare or welltoleratedtreatment+-stoptreatmentILRFigure 1 Diagnostic flow-chart <strong>of</strong> <strong>patients</strong> <strong>with</strong> <strong>palpitations</strong>. *Indicated only in selected cases; § refers to ECG–symptom correlation available.ECG, electrocardiogram (12-lead); Echo, echocardiography; AECG, ambulatory ECG; MRI, magnetic resonance imaging; EPS, electrophysiologicalstudy; ILR, implantable loop recorder.
926A. Raviele et al.Stress testing is indicated if <strong>the</strong> <strong>palpitations</strong> are associated <strong>with</strong>physical exertion (e.g. right ventricular outflow tract extrasystoles),in athletes and when coronary heart disease is suspected. The role<strong>of</strong> echocardiography is <strong>of</strong> paramount importance to evaluate <strong>the</strong>presence <strong>of</strong> structural heart disease. The need to conductfur<strong>the</strong>r non-invasive cardiologic investigations (particularlycardiac magnetic resonance imaging to evaluate <strong>patients</strong> <strong>with</strong>structural normal heart, <strong>palpitations</strong>, and frequent ventriculararrhythmias) or invasive investigations (coronary angiography,etc.) will depend on <strong>the</strong> nature <strong>of</strong> <strong>the</strong> heart disease suspectedor ascertained. Comparable to exercise-induced syncope,exercise-induced <strong>palpitations</strong> should raise suspicion for ischaemic,valvular, or o<strong>the</strong>r structural heart disease <strong>with</strong> <strong>the</strong> correspondingwork-up. Whenever a systemic or pharmacological cause <strong>of</strong> <strong>palpitations</strong>is suspected, specific laboratory tests should be performedon <strong>the</strong> basis <strong>of</strong> <strong>the</strong> clinical presentation <strong>of</strong> <strong>the</strong> symptom and <strong>the</strong>patient’s clinical characteristics (e.g. haemochrome, electrolytes,glycaemia, thyroid function, urinary catecholamines, detection <strong>of</strong>illicit substances in <strong>the</strong> blood or urine). If, on <strong>the</strong> contrary, a psychosomaticcause is suspected, <strong>the</strong> patient’s mental state must beassessed ei<strong>the</strong>r by means <strong>of</strong> specific questionnaires or through7,8,20 – 23referral for specialist examination.The initial clinical evaluation leads to a definitive or probablediagnosis <strong>of</strong> <strong>the</strong> cause <strong>of</strong> <strong>the</strong> <strong>palpitations</strong> in about half <strong>of</strong> <strong>patients</strong>,and excludes <strong>with</strong> reasonable certainty <strong>the</strong> presence <strong>of</strong> causes thathave an unfavourable prognosis. 47 Moreover, a thorough initialclinical evaluation will indicate which specific investigations, if any,are necessary.If <strong>the</strong> initial clinical evaluation proves completely unremarkable—which is more frequent in paroxysmal, short-lasting<strong>palpitations</strong>—<strong>the</strong> <strong>palpitations</strong> are deemed to be <strong>of</strong> unknownorigin. In subjects <strong>with</strong> <strong>palpitations</strong> <strong>of</strong> unknown origin who have alow probability <strong>of</strong> an arrhythmic cause (i.e. <strong>patients</strong> <strong>with</strong> gradualonset <strong>of</strong> <strong>palpitations</strong> and <strong>with</strong>out significant heart disease and those<strong>with</strong> anxiety-related or extrasystolic <strong>palpitations</strong>), fur<strong>the</strong>r investigationsare <strong>of</strong>ten not required. The patient should be reassured and afollow-up clinical examination may be scheduled. It should be underlined,however, that, in <strong>the</strong> absence <strong>of</strong> electrocardiographic recordingduring an episode <strong>of</strong> <strong>palpitations</strong>, only a presumed or probablediagnosis can be made. 30 By contrast, in instances <strong>of</strong> subjects <strong>with</strong><strong>palpitations</strong> <strong>of</strong> unknown origin presenting <strong>with</strong> clinical features suggestive<strong>of</strong> an arrhythmic cause 66 (Table 4), or when <strong>palpitations</strong> aresuspected to be related to atrial fibrillation in individuals <strong>with</strong> riskfactors for thromboembolism, 14,67 <strong>patients</strong> should be referred toTable 4 Clinical features suggestive <strong>of</strong> <strong>palpitations</strong> <strong>of</strong>arrhythmic originStructural heart diseasePrimary electrical heart diseaseAbnormal ECGFamily history <strong>of</strong> sudden deathAdvanced ageTachycardiac <strong>palpitations</strong>Palpitations associated <strong>with</strong> haemodynamic impairmentan arrhythmia centre, and second-level investigations should be considered;<strong>the</strong>se include ambulatory ECG monitoring and electrophysiologicalstudy (EPS) (Figure 1). Finally, second-levelinvestigations should also be carried out in <strong>patients</strong> <strong>with</strong> <strong>palpitations</strong><strong>of</strong> unknown origin whose symptoms are frequent or associated <strong>with</strong>impaired haemodynamic function or impaired quality <strong>of</strong> life or states <strong>of</strong>anxiety. 9Initial clinical evaluationHistoryIt represents a major part <strong>of</strong> <strong>the</strong> initial examination as most<strong>patients</strong> at <strong>the</strong> time <strong>the</strong>y visit a physician have no <strong>palpitations</strong>and <strong>the</strong> diagnosis has to be performed retrospectively. 5 – 9,48 Thefirst step is to establish that symptoms described by <strong>the</strong> patientmatch to <strong>palpitations</strong> and are not confused <strong>with</strong> chest pain oro<strong>the</strong>r manifestations arising in <strong>the</strong> chest, but that do not correspondto <strong>the</strong> definition <strong>of</strong> <strong>palpitations</strong> described in this article.When this first step has been achieved several important questionshave to be asked, <strong>the</strong> most important <strong>of</strong> which are summarizedin Table 5. Answers to some <strong>of</strong> <strong>the</strong>se questions may requireTable 5 Main questions to ask a patient <strong>with</strong><strong>palpitations</strong>Circumstances prior to <strong>the</strong> beginning <strong>of</strong> <strong>palpitations</strong>Activity (rest, sleeping, during sport or normal exercise, change inposture, after exercise)Position (supine or standing)Predisposing factors (emotional stress, exercise, squatting orbending)Onset <strong>of</strong> <strong>palpitations</strong>Abrupt or slowly arisingPreceded by o<strong>the</strong>r symptoms (chest pain, dyspnoea, vertigo, fatigue,etc.)Episode <strong>of</strong> <strong>palpitations</strong>Type <strong>of</strong> <strong>palpitations</strong> (regular or not, rapid or not, permanent or not)Associated symptoms (chest pain, syncope or near syncope,sweating, pulmonary oedema, anxiety, nausea, vomiting, etc.)End <strong>of</strong> <strong>the</strong> episodeAbrupt or slowly decreasing, end or perpetuation <strong>of</strong> accompanyingsymptoms, duration, urinationSpontaneously or <strong>with</strong> vagal manoeuvres or drug administrationBackgroundAge at <strong>the</strong> first episode, number <strong>of</strong> previous episodes, frequencyduring <strong>the</strong> last year or monthPrevious cardiac diseasePrevious psychosomatic disordersPrevious systemic diseasesPrevious thyroid dysfunctionFamily history <strong>of</strong> cardiac disease, tachycardia or sudden cardiacdeathMedications at <strong>the</strong> time <strong>of</strong> <strong>palpitations</strong>Drug abuse (alcohol and/or o<strong>the</strong>rs)Electrolytes imbalanceDownloaded <strong>from</strong> http://europace.oxfordjournals.org/ at :: on December 6, 2011