download as .pdf - PULSION Medical Systems SE
download as .pdf - PULSION Medical Systems SE
download as .pdf - PULSION Medical Systems SE
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
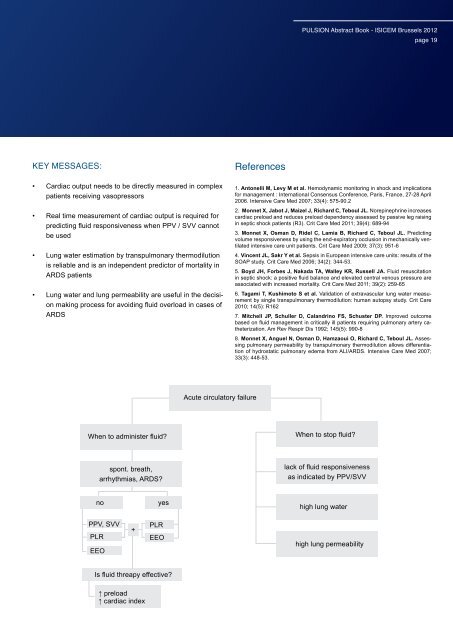
KEY MESSAGES:<br />
• Cardiac output needs to be directly me<strong>as</strong>ured in complex<br />
patients receiving v<strong>as</strong>opressors<br />
• Real time me<strong>as</strong>urement of cardiac output is required for<br />
predicting fluid responsiveness when PPV / SVV cannot<br />
be used<br />
• Lung water estimation by transpulmonary thermodilution<br />
is reliable and is an independent predictor of mortality in<br />
ARDS patients<br />
• Lung water and lung permeability are useful in the decision<br />
making process for avoiding fluid overload in c<strong>as</strong>es of<br />
ARDS<br />
When to administer fluid?<br />
spont. breath,<br />
arrhythmi<strong>as</strong>, ARDS?<br />
no yes<br />
PPV, SVV<br />
PLR<br />
EEO<br />
+<br />
PLR<br />
EEO<br />
Is fluid threapy effective?<br />
↑ preload<br />
↑ cardiac index<br />
Acute circulatory failure<br />
References<br />
<strong>PULSION</strong> Abstract Book - ISICEM Brussels 2012<br />
page 19<br />
1. Antonelli M, Levy M et al. Hemodynamic monitoring in shock and implications<br />
for management : International Consensus Conference, Paris, France, 27-28 April<br />
2006. Intensive Care Med 2007; 33(4): 575-90.2<br />
2. Monnet X, Jabot J, Maizel J, Richard C, Teboul JL. Norepinephrine incre<strong>as</strong>es<br />
cardiac preload and reduces preload dependency <strong>as</strong>sessed by p<strong>as</strong>sive leg raising<br />
in septic shock patients (R3). Crit Care Med 2011; 39(4): 689-94<br />
3. Monnet X, Osman D, Ridel C, Lamia B, Richard C, Teboul JL. Predicting<br />
volume responsiveness by using the end-expiratory occlusion in mechanically ventilated<br />
intensive care unit patients. Crit Care Med 2009; 37(3): 951-6<br />
4. Vincent JL, Sakr Y et al. Sepsis in European intensive care units: results of the<br />
SOAP study. Crit Care Med 2006; 34(2): 344-53.<br />
5. Boyd JH, Forbes J, Nakada TA, Walley KR, Russell JA. Fluid resuscitation<br />
in septic shock: a positive fluid balance and elevated central venous pressure are<br />
<strong>as</strong>sociated with incre<strong>as</strong>ed mortality. Crit Care Med 2011; 39(2): 259-65<br />
6. Tagami T, Kushimoto S et al. Validation of extrav<strong>as</strong>cular lung water me<strong>as</strong>urement<br />
by single transpulmonary thermodilution: human autopsy study. Crit Care<br />
2010; 14(5): R162<br />
7. Mitchell JP, Schuller D, Calandrino FS, Schuster DP. Improved outcome<br />
b<strong>as</strong>ed on fluid management in critically ill patients requiring pulmonary artery catheterization.<br />
Am Rev Respir Dis 1992; 145(5): 990-8<br />
8. Monnet X, Anguel N, Osman D, Hamzaoui O, Richard C, Teboul JL. Assessing<br />
pulmonary permeability by transpulmonary thermodilution allows differentiation<br />
of hydrostatic pulmonary edema from ALI/ARDS. Intensive Care Med 2007;<br />
33(3): 448-53.<br />
When to stop fluid?<br />
lack of fluid responsiveness<br />
<strong>as</strong> indicated by PPV/SVV<br />
high lung water<br />
high lung permeability