download as .pdf - PULSION Medical Systems SE
download as .pdf - PULSION Medical Systems SE
download as .pdf - PULSION Medical Systems SE
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
What are the relevant hemodynamic targets<br />
during septic shock and or during ARDS?<br />
(interactive session)<br />
C<strong>as</strong>e Study<br />
A 62 year old woman is admitted to ICU in a coma related to<br />
drug induced self poisoning. This is complicated by <strong>as</strong>piration<br />
pneumonia and moderate renal failure. She h<strong>as</strong> a previous history<br />
of COPD (Chronic Obstructive Pulmonary Dise<strong>as</strong>e), and<br />
severe hypertension. A culture of her tracheal secretions reveals<br />
evidence of Staph aureus, so she w<strong>as</strong> commenced on<br />
amoxicillin–clavulanic acid combination. She w<strong>as</strong> intubated<br />
and ventilated.<br />
Her blood pressure then dropped from 90/63/50 to 65/43/32<br />
mmHg, with a blood lactate of 3.5 mm/L, and PaO / FiO ratio<br />
2 2<br />
of 280. She w<strong>as</strong> given a rapid infusion of one liter of normal<br />
saline, and a norepinephrine (NE) infusion w<strong>as</strong> started at 0.3<br />
µg/Kg/min.<br />
Post Infusion hemodynamics<br />
ABP 74/55/45 mmHg<br />
Urine flow Low<br />
PaO 2 /FiO 2 ratio 210<br />
Lactate 4 mmol/L<br />
Echocardiography showed a left ventricular ejection fraction<br />
(LVEF) of 60%, no left ventricular dilatation and moderate right<br />
ventricular dilatation. An arterial catheter and central venous<br />
catheter were inserted - ScvO 2 70%, CVP 10 mmHg and PPV<br />
20%.<br />
Professor Jean Louis Teboul<br />
<strong>Medical</strong> ICU, Bicetre Hospital, University Paris South, France<br />
Prof Teboul is a Professor of Therapeutics and Critical Care Medicine, at the University Paris-<br />
South in France. He works clinically at the medical intensive care unit of the Bicetre University<br />
Hospital near Paris. His main research interests are in heart-lung interactions, cardiov<strong>as</strong>cular<br />
performance, regional blood flow <strong>as</strong>sessment, tissue oygenation, inv<strong>as</strong>ive and noninv<strong>as</strong>ive hemodynamic<br />
monitoring, and <strong>as</strong>sessment of volume status. Prof Teboul h<strong>as</strong> published around<br />
130 original papers and 100 book chapters, almost all of them in the field of hemodynamics. He<br />
h<strong>as</strong> given 230 invited lectures in international congresses and 150 invited lectures in French<br />
congresses.<br />
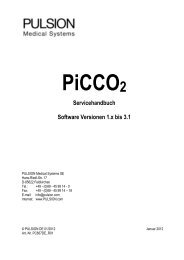
Question 1: How much can we rely on the CVP<br />
value in this patient (10mmHg)?<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
It suggests a<br />
normal right ventricular<br />
preload<br />
It suggests a<br />
high right ventricular<br />
preload<br />
Right ventricular<br />
preload can<br />
still be low<br />
It suggests fluid<br />
unresponsiveness<br />
*Results (in%) of the votes of an interactive session (audience 300) during ISICEM, 2012<br />
Central venous pressure is commonly cited <strong>as</strong> one of the goals<br />
for resuscitation. The Surviving Sepsis Guidelines(1) give a<br />
range of 8-12mmHg for initial resuscitation (first 6 hours) quoting<br />
the Rivers study <strong>as</strong> its main source (2). This study however,<br />
used the same range in both treatment arms and so therefore<br />
did not test this parameter for its sensitivity <strong>as</strong> a resuscitation<br />
goal. The CVP is not a simple me<strong>as</strong>urement. It is affected by<br />
many confounding factors including PEEP, the fact that it must<br />
be me<strong>as</strong>ured at the end of expiration, and even whether the<br />
transducer h<strong>as</strong> been placed at the anatomical zero level. In fact<br />
the CVP h<strong>as</strong> been repeatedly shown in the literature to not <strong>as</strong>sess<br />
right ventricular preload appropriately, and it is not able to<br />
predict fluid responsiveness (3, 4).<br />
The CVP should not be used to make clinical decisions regarding<br />
fluid management.