Apr 2016
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
THE MAGAZINE FOR NEW ZEALAND’S OPHTHALMIC COMMUNITY<br />
PO BOX 106 954, AUCKLAND CITY 1143<br />
Email: info@nzoptics.co.nz Website: www.nzoptics.co.nz<br />
APRIL <strong>2016</strong><br />
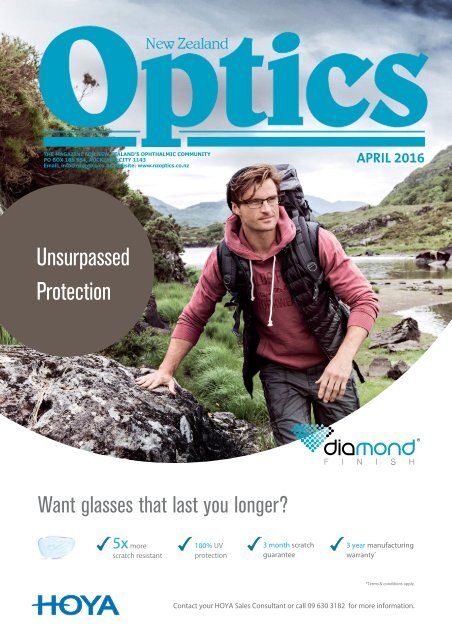
Unsurpassed<br />
Protection<br />
Want glasses that last you longer?<br />
5x more<br />
scratch resistant<br />
100% UV<br />
protection<br />
3 month scratch<br />
guarantee<br />
3 year manufacturing<br />
warranty *<br />
*Terms & conditions apply<br />
Contact your HOYA Sales Consultant or call 09 630 3182 for more information.
2015 was a challenging year for Bausch and Lomb with plenty of<br />
drama. The stage is set for a much improved <strong>2016</strong>:<br />
• Better supply direct from B+L Australia to your door<br />
• A dedicated B+L customer services team<br />
• An expanded sales team to ensure better service in store<br />
• Simplified universal pricing to ensure fairness and profitability for all<br />
• A game changing web service that will enable you to compete with the<br />
internet - watch this space!<br />
We’re determined to regain your trust and your business through<br />
exceptional service and world class products.<br />
We’re getting our act together<br />
2 NEW ZEALAND OPTICS <strong>Apr</strong>il <strong>2016</strong><br />
If you would like to talk to us about our new web service or<br />
the new lenses we’re about to launch, call us on 0800 658 386
OTs tackle low vision<br />
Collaboration<br />
between the<br />
occupational<br />
therapy (OT) community<br />
and an advocacy group<br />
has resulted in several<br />
public awareness<br />
projects and a developing<br />
curriculum for OT<br />
students to specialise in<br />
low vision care.<br />
The development began<br />
a few years ago when<br />
Dr Mary Butler, Otago<br />
Polytechnic principal<br />
lecturer, put some<br />
third-year students<br />
in-touch with the Visual<br />
Impairment Charitable<br />
Trust Aotearoa (VICTA) to develop ideas for projects<br />
to help that community. Around the same time<br />
Associate Professor Gordon Sanderson from<br />
Otago University encouraged Dr Butler to develop<br />
a curriculum for postgraduate OT students to<br />
concentrate on that area.<br />
Occupational therapists are interested in<br />
function and practical ways to improve lives,<br />
says Dr Butler. Low vision is a central field in OT<br />
practice overseas, but in New Zealand, there are<br />
opportunities for OTs to become more involved in<br />
helping low vision patients to navigate life in spite<br />
of their visual problems and to work far more<br />
closely with optometrists.<br />
“I’m very much trying to create a space where<br />
the profession will say, ‘we can do this’, and to<br />
encourage OTs to work closely with optometrists.<br />
I’m encountering too many old neighbours and<br />
clients who are unnecessarily disabled by visual<br />
impairment,” says Dr Butler.<br />
“Too often they are told by their ophthalmologist<br />
that there is nothing that can be done. This is<br />
not true. There are many things that OTs can do<br />
by problem solving everyday functions such as<br />
cooking, community mobility and remaining active.<br />
We tend to use the simplest equipment or none at<br />
all to bring about these outcomes.”<br />
Projects arising from student collaboration with<br />
VICTA include the development of high visibility<br />
canes and wristbands for low vision pedestrians to<br />
make drivers aware of their presence on the street.<br />
“The whole question of road safety was a big<br />
issue from the time we started the group,” says Dr<br />
Lynley Hood, founding trustee of VICTA.<br />
The Trust actually began as the Dunedin Visually<br />
Impairment group, a lively cadre of elderly people<br />
diagnosed with various problems that will lead to<br />
permanent sight loss. When it became clear their<br />
issues were of national significance, particularly in<br />
regard to the ageing population, Dr Hood and her<br />
cohort established the Trust.<br />
“If you’re no longer allowed to drive, even if<br />
you get half-priced taxi fares with a disability<br />
allowance, getting around becomes very<br />
expensive. Buses are the better option,” says Dr<br />
Hood. “But if you catch the bus, you still have to<br />
cross the road. (Low vision people) don’t have<br />
white canes or guide dogs, so motorists don’t<br />
know that they can’t see them properly. So, one<br />
of the first suggestions was high visibility walking<br />
sticks. They are a hit with bus drivers.”<br />
Still from video promoting the use of high visibility sticks and wristbands from OTs<br />
collaboration with VICTA<br />
VICTA worked with a local fabricator to develop<br />
four high visibility walking sticks, made from<br />
carbon fibre with high contrast colours sure to be<br />
visible from blocks away. Go Bus and Richies now<br />
train drivers to recognise high visibility canes and<br />
wrist bands thanks to VICTA’s efforts. While one of<br />
Dr Butler’s third year OT students, Keri McMullan,<br />
helped produce a video promoting the service,<br />
which VICTA intends to use to promote visibility<br />
canes around the country for World Sight Day in<br />
October.<br />
McMullan was also responsible for a video<br />
promoting the use of iPads among low vision<br />
recipients and, according to Dr Butler, a third<br />
video promoting safe use of mobility scooters is in<br />
the works.<br />
“I applied for a small amount of funding to help<br />
promote what occupational therapy can do for<br />
people with low vision,” says Dr Butler. “We have<br />
been running student placements, making videos,<br />
creating Facebook pages, setting up an equipment<br />
library, running iPad classes for people with low<br />
vision and workshops for OTs. Lynley and VICTA have<br />
been very important in helping us to get traction<br />
and the profession is now coming on board.”<br />
A postgraduate paper in vision rehabilitation will<br />
be rolled out at Otago Polytechnic in the second<br />
semester of the <strong>2016</strong> academic year. Dr Butler says<br />
this has been brewing for some time.<br />
“It came about in a number different ways. My<br />
main area is brain injury and a few years ago I had<br />
a master’s student doing work on neurological<br />
vision impairment. She was working for the Blind<br />
Foundation, but she pointed out that people with<br />
neurological vision impairment and other kinds of<br />
low vision did not qualify for help from this service.<br />
At about the same time, Lynley and Gordon were<br />
setting up VICTA, which draws together 20-30 with<br />
low vision every month who are passionate and<br />
increasingly articulate about what they need. Put<br />
that together with the figures from the Disability<br />
Survey (2014), which found that that self-reported<br />
visual impairment among adults increased an<br />
astonishing 100% between 2001 and 2013 (from<br />
81,500 to 163,000) and it all clearly points to an<br />
area where we all have to do our bit; and we are<br />
particularly keen to work closely with optometrists<br />
both in practice and research about low vision”<br />
To see more on of what Kiwi OTs are doing for low<br />
vision patients check out: https://www.facebook.<br />
com/Vision-Matters-OT-866464940127100. ▀<br />
Celebration and a question of style<br />
Our last month before going to press has been a<br />
whirlwind of functions. The wonderful Macular<br />
Degeneration Race Day was a chance to enjoy a<br />
stunning day for a fabulous cause. Though my hat<br />
played havoc from a picture-taking point of view,<br />
it was a pure pleasure to be involved and Jai, our<br />
new editor, got her first taste of what a wonderful<br />
industry this is.<br />
There were more celebrations at the upbeat<br />
Excellence in Ophthalmology and Vision<br />
Research Prize Evening, where some of our most<br />
experienced professionals stepped up to support<br />
and celebrate some of our budding newcomers;<br />
at Auckland Eye, which was celebrating the<br />
end of its refurbishment; and at the Summer<br />
Students Research Symposium, covered by our<br />
well-known editor-at-large, Maryanne—all<br />
included in this month’s issue.<br />
A question of style<br />
We’ve tweaked a few things this month after<br />
some of you were kind enough to provide<br />
feedback on the magazine.<br />
Thanks to all those who say you’re loving<br />
the slightly fresher, more modern look of the<br />
magazine; the content mix of news, views, and<br />
celebrations; and the more national focus—<br />
though we can always do with more stories from<br />
around the country, so keep them coming.<br />
We’ve also listened to those who weren’t quite<br />
ready for the evolution (perhaps revolution) to<br />
that doyen of journalism styles, the Associated<br />
Press (AP), followed by most western publications.<br />
The AP only use full titles on first mention and<br />
thereafter simply refer to the person by their<br />
surname. (Even President Barack Obama becomes<br />
simply Obama). This ensures consistency, clarity,<br />
accuracy and brevity—a constant challenge in<br />
publishing as there are always more stories than<br />
ads to support the publication of those stories.<br />
AP’s style was also developed to avoid<br />
stereotypes and upsetting anyone as it treats<br />
everybody the same. Many women have a<br />
problem with the “Ms”, “Mrs” or “Miss” honorifics,<br />
which force them to reveal their married status,<br />
compared with men’s simple “Mr”. Sweden even<br />
EDITORIAL C ▀<br />
introduced a gender neutral title “hen” to avoid<br />
the problem. Some publications use first names<br />
for students instead of surnames, but just how<br />
much study, experience or age should a person<br />
have before they can be referred to in the same<br />
manner as their peers? Then there’s the question<br />
of medical doctors versus PhDs—the latter given a<br />
particularly bad rap by some honorary PhDs using<br />
the title—with many publications deciding to<br />
now only acknowledge someone’s PhD when it’s<br />
relevant to the story and only use the title “Dr” for<br />
medical practitioners.<br />
Here at NZ Optics we are your industry<br />
publication and though we can’t promise to do<br />
everything you ask (as that could diminish the<br />
editorial integrity of the publication, which is<br />
something we hold in very high regard to ensure<br />
all are treated fairly) we do care what you think<br />
and so have reinstated professional honorifics—so<br />
no Mr’s but lots of Dr’s.<br />
We love your feedback, especially your praise,<br />
and we do listen. This is your publication and the<br />
next generation’s too and everyone should have<br />
a voice, which is why we’re delighted to have an<br />
article this month from Nikku Singh (no title yet),<br />
the new president of the NZ Optometry Student<br />
Society (NZOSS).<br />
So enjoy this month’s issue, celebrating so many<br />
wonderful things people in this industry have<br />
achieved, and don’t be afraid to let us know what<br />
you think—we can take it!<br />
Lesley Springall, publisher, and Jai Breitnauer at the<br />
MDNZ Race Day<br />
NEW ZEALAND<br />
University’s generous gift<br />
Joan Ready, former Faculty of Medicine<br />
and Health Sciences administrator with<br />
the Department of Ophthalmology, has<br />
donated $250,000 to her former department for<br />
department head Professor Charles McGhee to<br />
spend at his discretion.<br />
Talking at the <strong>2016</strong> Excellence in Ophthalmology<br />
and Vision Research Awards (see story p4), Professor<br />
McGhee said he was both surprised and delighted at<br />
Ready’s generous gift, which would be used to help a<br />
number of young people reach their goals.<br />
Ready worked at the Faculty for more than 35<br />
years in various research and management roles,<br />
including research technician and manager for<br />
Physiology, Pathology, Clinical Sciences, School of<br />
Nursing and the Rural Health Inter-professional<br />
Immersion Programme. She joined Professor<br />
McGhee when the Department of Ophthalmology<br />
was in its infancy and stayed there for the last 17<br />
years.<br />
In the Faculty newsletter, Professor McGhee<br />
said he was extremely grateful to have had “Joan<br />
University vice-chancellor Professor Stuart McCutcheon and<br />
Joan Ready (front) with Professor John Fraser, dean of Faculty of<br />
Medical and Health Sciences, and Professor Charles McGhee (back)<br />
as a great friend and colleague over the last 17<br />
years” and that she played an integral part in<br />
many of the department’s major developments in<br />
ophthalmology.<br />
He anticipates the Joan Ready Fund will help start<br />
the careers of several future ophthalmologists and<br />
clinician scientists in New Zealand, he said. ▀<br />
Supplying Kiwi Optometrists<br />
with exclusive digital lens<br />
designs, quality and service<br />
Visit us at<br />
shamir.co.nz<br />
For more information contact<br />
DONALD CRICHTON<br />
New Zealand Sales Rep<br />
021 449 819<br />
Shamir quarter page ad NZ OPTICS APRIL <strong>2016</strong>.indd 1<br />
<strong>Apr</strong>il <strong>2016</strong><br />
11/03/<strong>2016</strong> 3:55:24 PM<br />
NEW ZEALAND OPTICS<br />
3
News<br />
in brief<br />
RANZCO WARNS AGAINST EYEBALL TATTOOS<br />
The inclusion of eyeball tattooing in health legislation passed by<br />
the NSW Labour government in February has effectively legalised<br />
this experimental form of “body modification” in the state. RANZCO<br />
responded by issuing a strong warning against the practice, which<br />
involves injecting ink into the sclera to make it a solid or mix of<br />
colour. “The eye is a very complex and sensitive organ and in no<br />
way should anyone consider tattooing it if they wish to retain their<br />
sight over the long-term,” said Associate Professor Mark Daniell, a<br />
corneal specialist. Eyeball tattooing has been banned in some US<br />
states due to a link to blindness and cancer.<br />
SMART CONTACTS FROM CHINA<br />
In a huge leap forward for next-generation wearable tech, a<br />
Chinese research team have built an “invisible” circuit layer within<br />
a contact lens for the first time. The team’s research, published in<br />
the journal Advanced Materials in March, was led by Professor Song<br />
Yanlin at the Chinese Academy of Sciences in Beijing. The built-in<br />
electronic circuit is invisible to the naked eye because it measures<br />
one micrometre in width, making it narrower than the average<br />
bacterial cell. It could be used to measure glucose levels in the tears<br />
of diabetic patients or become part of a layer of “invisible skin”<br />
giving a sense of feeling back to patients with prosthetic limbs, the<br />
authors said.<br />
PENNY THE PIRATE CROWNED QUEEN<br />
OPSM’s Penny the Pirate--an eye test turned into a book and an<br />
associated app, designed to test kids’ eyes while reading with their<br />
parents--has been crowned the world’s most successful marketing<br />
campaign in the Warc 100 rankings, an annual report that judges<br />
the world’s best marketing campaigns by business impact.<br />
The campaign, created for OPSM by Saatchi & Saatchi Sydney with<br />
the help of paediatric eye care specialists, resulted in thousands of<br />
children having their eyes checked and increased the number of<br />
eye tests conducted by OPSM by 22.6% year-on-year. The book is<br />
now being used by not-for-profit organisation OneSight to help test<br />
children’s eyes in remote and rural Australia.<br />
ESSILOR AQUIRES UK ASSET, PUBLISHES STRONG RESULTS<br />
Essilor International has acquired UK-based Vision Direct Group,<br />
one of Europe’s leading online contact lens retailers, with<br />
revenue of around £33 million ($71 million) in 2015. Essilor said<br />
the acquisition strengthens its current position in Europe by<br />
complementing existing activities. Fuelled by 19 new acquisitions<br />
and partnerships, Essilor also published strong financial results for<br />
2015, as the company continues to focus on its lens and optical<br />
instrument divisions, innovation and consumer marketing. Revenue<br />
was up 18.4% to €6,716 million ($11,205 million), while operating<br />
profit increased 19.6% to €1,183 million ($1,974 million).<br />
MORE MAORI SURGEONS PLEASE<br />
The Royal Australasian College of Surgeons (RACS) has committed<br />
to increasing the number of Maori surgeons in New Zealand as part<br />
of a newly developed Maori Health Action Plan. “At present, there<br />
are only a small number of surgeons in New Zealand who identify<br />
as Maori,” said Dr Jonathan Koea, an Auckland-based hepatobiliary<br />
and general surgeon and member of the Plan’s working group.<br />
Dr Koea notes that while this programme will take a sustained<br />
effort over years, it is a significant step forward for the College’s<br />
commitment to Maori health. “Through the Action Plan, RACS<br />
intends to increase the number of Maori in the surgical workforce,<br />
embed cultural competency as a fundamental professional skill,<br />
focus more surgical research into Maori Health and promote<br />
initiatives that will decrease the disparities that currently exist for<br />
Maori.”<br />
BAYER OFFERS GRANTS<br />
Bayer and the American Association for Cancer Research (AACR)<br />
announced the availability of the “AACR-Bayer Innovation and<br />
Discovery Grants”. The programme aims to promote the key tenets<br />
of the Bayer Grants4Targets initiative with a focus on oncology<br />
to provide new treatment options for cancers with high unmet<br />
medical need, to encourage innovation and translation of ideas<br />
from basic research into novel drugs and to foster collaborations<br />
between academic groups and the pharmaceutical industry.<br />
BIONIC EYES BECOMING A REALITY<br />
Once the privilege<br />
of TV’s Six Million<br />
Dollar Man, bionic<br />
vision is becoming<br />
more commonplace<br />
for the everyday<br />
patient. Pixium<br />
Vision have<br />
launched the Iris II,<br />
their first epiretinal<br />
implant with 150<br />
electrodes—more<br />
than three times what is currently available—suitable for patients<br />
who have lost their sight due to retinitis pigmentosa (RP). The<br />
France-based research team, headed by Professor Michel Weber,<br />
said early results with patients with RP are positive.<br />
Meanwhile in the US, optics specialist Eric Tremblay unveiled a<br />
unique contact lens that will provide the wearer with telescopic<br />
vision. The lens is just 1.55 mm thick and features a thin, reflective<br />
telescope that enables the user to zoom in and out via winking. ▀<br />
Excellence in<br />
ophthalmology<br />
celebrated<br />
The annual Excellence in<br />
Ophthalmology and Vision Research<br />
prize evening is an upbeat affair,<br />
bringing together those at the beginning<br />
of their careers with those who have more<br />
experience to share.<br />
This year event’s on March 1 was no<br />
different, with a celebratory atmosphere<br />
pervading the halls at the University of<br />
Auckland. The event was well-attended<br />
by members of the Ophthalmology<br />
Department, senior staff from the School of<br />
Medicine, donors, benefactors and friends<br />
and family members of the prize winners.<br />
Ophthalmologist and department head<br />
Professor Charles McGhee presided,<br />
explaining the evening was about<br />
celebrating past and future potential<br />
success. He reviewed the achievements of<br />
the department since it was established<br />
in 1999, including gaining more than $33<br />
million in research funding, increasing<br />
research fellows from one to 75, 700<br />
research papers published or soon-to-be<br />
published, 30 higher research degrees<br />
awarded or submitted, and 18 PhD and MD<br />
students currently enrolled. There has also<br />
been a myriad of national and international<br />
connections developed through the success<br />
of past students, many of whom have gone<br />
on to become leaders in their field both here<br />
and overseas. Professor McGhee thanked<br />
the department’s benefactors, those who’ve<br />
been supporting the department from the<br />
start such as Drs Bruce and Wendy Hadden<br />
and the Ring family to the newest supporter,<br />
former faculty administrator Joan Ready<br />
(see story P3) who he says blew him away<br />
with her generous retirement donation of<br />
$250,000.<br />
Doctoral candidate Yeri Kim provided<br />
an outline of her PhD research into the<br />
Development of connexin inhibitors for the<br />
treatment of retinal diseases to understand<br />
the mode of action of Peptagon and HCB1019<br />
to potentially treat diabetic retinopathy and<br />
macula oedema, and dry and wet AMD. Given<br />
the initial success of Kim’s research, clinical<br />
trials with Peptagon are expected to start this<br />
year.<br />
But the main reason for the evening was<br />
to celebrate seven award winners: the noted<br />
summer studentships and the winners of the<br />
prestigious William MacKenzie Medal, Arthur<br />
Thomas Paterson scholarship and Calvin Ring<br />
Undergraduate awards:<br />
Calvin Ring Undergraduate Prize in<br />
Ophthalmology—Victoria Utley<br />
Dr Peter Ring presented the Calvin Ring<br />
Undergraduate Prize for the best allround<br />
undergraduate student in clinical<br />
ophthalmology to fifth year medical student<br />
Victoria Utley.<br />
In presenting the award, Dr Ring explained<br />
that the award was given in honour of<br />
his father, Dr Calvin Ring, who was at<br />
the forefront of ophthalmology for his<br />
generation, who spearheaded good practice<br />
and the use of new IOLs in cataract surgery<br />
and who was instrumental in bringing about<br />
the Maurice Paykel Chair of Ophthalmology,<br />
held by Professor McGhee.<br />
Utley comes from a dynasty of surgeons in<br />
Christchurch whose publications and research<br />
showed a strong surgical bias, he said. Utley<br />
said she was excited to receive the award, the<br />
first since school, and though she was still<br />
undecided which direction to follow she’d<br />
always had an interest in ophthalmology. “I<br />
enjoyed my ophthalmology placement last<br />
year. I’ve always been interested in eyes, but<br />
being able to see the research and being able<br />
to understand that the eyes aren’t their own<br />
separate entity, they are kind of a window to<br />
what’s going on generally in the body, I found<br />
fascinating.” Utley said how privileged she<br />
felt to have won the award and to have met<br />
the Ring family.<br />
William MacKenzie Medal—Michael Wang<br />
The William MacKenzie Medal is awarded<br />
each year for “Early Excellence in Eye<br />
Research.” It is a highly prized award<br />
that recognises<br />
the significant<br />
contribution<br />
made by a<br />
medical student<br />
or trainee intern<br />
towards a research project, which reached<br />
publication status during the year of the<br />
award.<br />
This year’s winner, Michael Wang, a fifth<br />
year undergraduate medical student,<br />
received his award from Associate Professor<br />
Jennifer Craig who said Wang’s academic<br />
achievement, dedication toward research and<br />
enthusiastic approach was commended by<br />
a number of staff members. She explained<br />
how Wang had done an exceptional job<br />
working on a number of different projects<br />
in her department looking at some of the<br />
treatments for dry eye, mostly in the area of<br />
ocular surface disease. He has published two<br />
papers and submitted a third on the work<br />
he’s been doing and has at least two more in<br />
the pipeline. He now has eight papers to his<br />
name and six in preparation, she said.<br />
Award winners (L to R) Michael Wang, Eileen Song, Clare Wu, Victoria Utley, Andy<br />
Kim, Benjamin Wright and Dr Leo Sheck. Picture by Godfrey Boehnke (GB)<br />
Arthur Thomas Paterson Scholarship—Dr Leo<br />
Sheck<br />
Auckland Eye’s Dr Sarah Welch, the current<br />
clinical director of ophthalmology at<br />
Greenlane Clinical Centre, specialising in<br />
medical and surgical retina, presented the<br />
Arthur Thomas Paterson Postgraduate<br />
Scholarship to Dr Leo Sheck. The<br />
scholarship supports a vocational trainee<br />
in ophthalmology to pursue a fellowship<br />
overseas.<br />
In presenting the award Dr Welch said it<br />
was a pleasure having Dr Sheck as a registrar<br />
in the department and that he’s been a<br />
great asset. Dr Sheck is going to Moorfields<br />
Eye Hospital in London to study genetic eye<br />
diseases, in particular retinal dystrophies and<br />
electrophysiology and diagnostics. All areas<br />
of great need in the country and within the<br />
Auckland district, said Dr Welch.<br />
In his citation, Dr Sheck said at Moorfields<br />
he’d be working with Professor Graham<br />
Holder, a well-recognised international expert<br />
in electrodiagnostics, while his supervisor<br />
will be Professor Michel Michaelides, an<br />
international expert in retinal dystrophies.<br />
Eye Institute Summer Studentship—Andy<br />
Kim<br />
Eye Institute ophthalmologist and patron of<br />
the Buchanan Ocular Therapeutics Unit at<br />
Auckland Unversity Dr Trevor Gray, presented<br />
the Eye Institute Summer Studentship award<br />
to third year medical student Andy Kim.<br />
Kim conducted a comprehensive literature<br />
review over the summer on Demodex<br />
blepharitis under the supervision of Associate<br />
Professors Jennifer Craig and Trevor Sherwin.<br />
The aim of his project was to review the<br />
current knowledge on Demodex mites and<br />
Demodex blepharitis with the intention<br />
of identifying molecules which could be<br />
uniquely and readily expressed by Demodex<br />
mites. It was also a pre-cursor to Kim’s<br />
honours project to develop a diagnostic test<br />
for ocular demodicosis.<br />
Retina New Zealand Summer Studentship—<br />
Benjamin Wright<br />
Frazer Alexander, president of Retina New<br />
Zealand, presented the Retina NZ Summer<br />
Studentship award to fifth year medical<br />
student Benji Wright.<br />
Wright undertook a summer studentship<br />
Characterising Cystic Maculopathy in<br />
Inherited Retinal Disease, funded through<br />
Retina New Zealand and supervised by<br />
Retina Specialists’ ophthalmologist Dr<br />
Andrea Vincent, who he worked with in the<br />
Greenlane Clinicical Centre.<br />
During the summer studentship Wright<br />
determined the incidence of cystic<br />
maculopathy in a number of inherited<br />
retinal diseases, identified from the NZ<br />
Database of Inherited Retinal Disease. He<br />
reported on the differing incidences of cystic<br />
changes between autosomal dominant,<br />
autosomal recessive and x-linked retinitis<br />
PhD research presenter Yeri Kim and Professor<br />
McGhee entertain the audience. Picture by GB<br />
Naveed Yasin, Raul Ayala and Priyanka Agarwal<br />
Clare Wu and Dr Bruce Hadden share a laugh<br />
during the prize giving. Picture by GB<br />
pigmentosa. He also investigated the rates<br />
of response to carbonic anhydrase inhibitor<br />
treatment in patients who have developed<br />
cystic maculopathy, and correlated this with<br />
their genetic cause, in order to ascertain the<br />
likelihood of successful treatment.<br />
Tom Cat Trust Summer Studentship—Clare<br />
Wu<br />
Associate Professor Bruce Hadden presented<br />
the Tom Cat Trust Summer Studentship award<br />
to third-year medical student Clare Wu.<br />
Supervised by Associate Professor Trevor<br />
Sherwin and Jane McGhee, Wu researched<br />
stem cell proliferation, migration and<br />
differentiation of excised limbal tissue verses<br />
neurospheres. The cell sources were seeded<br />
onto amniotic membranes then placed on<br />
donated human cornea for varying time<br />
periods. She found neurospheres proliferated<br />
and migrated more favourably than their<br />
limbal tissue explant counterparts, informing<br />
future treatment options for patients with<br />
limbal stem cell deficiency.<br />
Ombler Trust Summer Studentship—Eileen<br />
Song<br />
Dr Andrea Vincent presented the final<br />
Summer Studentship Award, the Ombler<br />
Trust Award, to third-year medical student<br />
Eileen Song.<br />
Under Dr Vincent’s supervision, Song<br />
characterised the nature and spectrum of<br />
X-linked inherited retinal disease within<br />
New Zealand. Using the Inherited Retinal<br />
Disease Database, she identified individuals<br />
with X-linked disease and investigated the<br />
correlation between their clinical features,<br />
disease in females and the genetic test<br />
results. Results from her project show<br />
9.26% of patients from the Inherited Retinal<br />
disease Database harbour a diseasecausing<br />
mutation in a retinal gene on the X<br />
chromosome. The population studied also<br />
contained several families where the obligate<br />
female carriers were as severely affected<br />
phenotypically as the affected male family<br />
members, challenging the conventional<br />
concept that female carriers have a later<br />
onset and a milder course of disease than<br />
affected males. The study highlighted the<br />
importance of local knowledge in order to<br />
optimise management and treatment, said<br />
Dr Vincent. ▀<br />
4 NEW ZEALAND OPTICS <strong>Apr</strong>il <strong>2016</strong>
IT’S TIME TO PLAY...<br />
$..‘000’S ON OFFER FOR EVERY REFERRAL<br />
OR… REFER YOURSELF AND STILL TAKE HOME THE $$<br />
With a market shortage of optometrists in both Australia and New Zealand, alongside a goal<br />
of further growth from Specsavers franchise partners in <strong>2016</strong>, we’re taking a new<br />
approach to boosting our optometry team – and everyone can benefit.<br />
For the months of <strong>Apr</strong>il and May, every optometrist you refer to our recruitment<br />
teams – who subsequently joins us as a locum, as a partner or in an employed role<br />
- will earn a ‘Refer a Friend’ payment. Depending on the location<br />
and role taken up, payments you are eligible for range from $1000 to $50,000!<br />
And here’s a tip – if you’re really up for it and refer yourself, you’ll still be<br />
entitled to claim your referral payment…<br />
To find out more and to explore the Terms and Conditions associated with this<br />
industry-wide offer, contact Carly Parkinson on +61 478 201 057 or<br />
carly.parkinson@specsavers.com – or visit spectrum-blog.com.<br />
Retail<br />
Employer<br />
of the Year<br />
2015<br />
Franchise<br />
Innovation<br />
Award<br />
2015<br />
NZ Franchise<br />
System of<br />
the Year<br />
2014<br />
Retail<br />
Innovator<br />
of the Year<br />
2014<br />
Multichannel<br />
Retailer<br />
of the Year<br />
2014<br />
Roy Morgan<br />
Research<br />
No. 1 for eye tests<br />
2014<br />
FCA International<br />
Franchisor<br />
of the Year<br />
2014<br />
FCA Social<br />
Responsibility<br />
Award<br />
2014<br />
FCA Established<br />
Franchisor<br />
of the Year<br />
2013<br />
FCA Excellence<br />
in Marketing<br />
Award Winner<br />
2013<br />
Australian<br />
Retailer<br />
of the Year<br />
2013<br />
<strong>Apr</strong>il <strong>2016</strong><br />
NEW ZEALAND OPTICS<br />
5
New 3 point test<br />
for teachers<br />
Albany optometrist Stuart<br />
Warren has developed a 3<br />
Point Check Test for school<br />
teachers to administer to determine<br />
if near vision problems may be<br />
contributing to learning difficulties.<br />
Warren, an advocate for students<br />
with dyslexia, developed the test<br />
from his experience treating young<br />
patients whose vision problems<br />
were causing difficulties at school.<br />
“If a child has a learning problem, but passes the school screening<br />
test, teachers assume their vision is fine. But in reality there may<br />
still be a near vision problem. Over the past 10 years there have<br />
been quite a few studies to support the idea that the prevalence<br />
of near-vision problems is quite high especially if there is a<br />
background of learning difficulties.”<br />
Warren’s 3 Point Check Test assesses if a child’s near vision is<br />
clear, single and steady, which Warren refers to as the “near visual<br />
platform”. It measures amplitudes of accommodation, convergence<br />
and asks students if letters appear to be “jumping or moving” on<br />
the page--an indicator of visual stress. This latter symptom can be<br />
assessed with tinted lenses based on those used in controlled trials<br />
by the Dyslexia Research Trust at Oxford University.<br />
Warren says he is planning to sell his test as a kit for teachers, but<br />
is also making it available to optometrists. “I’m currently working<br />
with a small handful of schools. I was invited to speak to a group<br />
of teachers at the end of last year and I discussed the 3 Point Check<br />
Test and they were very positive about it. Some of the teachers<br />
were surprised because they never considered that near-vision<br />
could be a problem.”<br />
Warren says one school he worked with arranged for a dozen<br />
students with known learning difficulties to be screened and found<br />
that four of them had previously unidentified near-vision problems.<br />
The test is designed for children aged seven to 17 and can be<br />
conducted by a trained teacher in less than a minute.<br />
Children with near-vision problems may have difficulties<br />
with reading accuracy and fluency or they may have difficulty<br />
concentrating in class. Warren says he frequently uses a<br />
questionnaire that he sends out to parents and teachers to identify<br />
any correlation between vision and learning. A common symptom<br />
that appears in the questionnaire is a child’s inability to keep their<br />
place in a text. “They’re not able to allocate attention to the task of<br />
learning,” he says.<br />
Warren’s interest in behavioural optometry and helping patients<br />
with learning difficulties, led him to develop the kit. But one<br />
particular patient he saw in early 2015 was instrumental in creating<br />
the test: an eight-year-old boy who was on reading recovery for 18<br />
months and was even taken to a psychologist to determine other<br />
reasons for his reading difficulty. “When I tested the patient, I found<br />
he couldn’t converge at all, which really surprised the parents. These<br />
kinds of problems are all too common, so it makes sense to have a<br />
near screening test out there. It could solve a lot of problems.”<br />
After selling his practice, Warren is now working at Albany<br />
Optometrists and is building a number of tools for schools and<br />
optometrists to help students with learning problems including<br />
a video to demonstrate the 3 Point Check Test. For more visit his<br />
website at http://icept.co.nz. ▀<br />
See the light,<br />
not the UV<br />
Australian<br />
researchers<br />
have developed<br />
a nanoscale device<br />
that is able to filter<br />
specific colours from<br />
light. Researchers<br />
at RMIT University<br />
and the University<br />
of Adelaide have developed a stretchable material able to<br />
manipulate light while remaining transparent. Using artificial<br />
crystals known as dielectric resonators that are just 100 nm to<br />
200 nm in size, the material could be used to make contact lenses<br />
that prevent harmful rays—such as UV light—from penetrating<br />
the eye.<br />
Right now, dielectric resonators only work with specific colours,<br />
but because the scientists were able to build the material to be<br />
elastic, they were able to control the properties of the surface and<br />
filter out more colours. When combined with other advances in<br />
technology, the result could be a smart contact lens that protects<br />
the eye while gathering and transmitting live data—like a tiny<br />
version of Google Glass.<br />
“With this technology, we now have the ability to develop<br />
light weight wearable optical components, which also allow for<br />
the creation of futuristic devices such as smart contact lenses<br />
or flexible ultrathin smartphone cameras,” said lead author and<br />
RMIT researcher Dr Philipp Gutruf.<br />
The paper, Mechanically tunable dielectric resonator<br />
metasurfaces at visible frequencies, was published in the journal<br />
ACS Nano. ▀<br />
A review of ocular coherence<br />
tomography angiography<br />
BY DR SHANU SUBBIAH AND DR<br />
PETER HADDEN*<br />
Optical coherence tomography (OCT)<br />
has evolved over the past decade as<br />
one of the most important ancillary<br />
tests in ophthalmic practice. The technology<br />
was first developed in 1991 and the first<br />
clinical application reported in 1994 for the<br />
investigation of macular disease. 1, 2<br />
The first iteration time-domain OCT had<br />
both speed and sensitivity issues that<br />
limited its accuracy, reliability, and efficiency.<br />
These limitations were supplanted by the<br />
introduction of spectral-domain OCT (SD-OCT)<br />
systems, which used spectral interferometry<br />
and Fourier analysis. This allowed image<br />
acquisition 50 to 100 times faster than timedomain<br />
technology with a subsequent and<br />
dramatic improvement in quality.<br />
Optical coherence tomography angiography<br />
(OCTA) is a new non-invasive approach to<br />
diagnostic imaging in retinal disease. It<br />
identifies blood vessels because the blood<br />
flowing through them causes the reflected<br />
OCT signal to vary slightly on consecutive<br />
scans, since it is moving and altering rather<br />
than staying still like the rest of the eye,<br />
and can generate angiographic images in a<br />
matter of seconds. 3, 4 It is a new technique<br />
that enables us to image yet another<br />
anatomic structure of the eye with OCT, this<br />
time the vasculature.<br />
Previously the “gold standard” investigation<br />
for diagnosis of retinal vascular disease has<br />
been “injected dye” angiography. Standard<br />
angiography allows for dynamic visualisation<br />
of blood flow with a wide field of view.<br />
Patterns of dye leakage, pooling, and staining<br />
can be appreciated, thus allowing diagnosis<br />
of pathology. Fluorescein angiography (FA)<br />
and indocyanine green angiography (ICGA)<br />
are, however, invasive tests that require<br />
intravenous administration of dye and<br />
imaging of 10–30 minutes.<br />
Standard angiography does of course have<br />
limitations; retinal pathology can be obscured<br />
by leakage, hemorrhage and media opacities.<br />
Also, the images provided are also twodimensional,<br />
hence one cannot distinguish<br />
between blood vessels at different depths<br />
within the retina. FA and ICGA have other<br />
drawbacks that can limit their widespread<br />
use. They are invasive, relatively expensive,<br />
and time-consuming, consequently they are<br />
not ideally suited for use on a regular basis<br />
in a busy clinical setting. Although very safe,<br />
the dyes pose risks ranging from nausea to<br />
allergic reactions, including anaphylaxis in<br />
rare instances. 5 Indocyanine green dye is also<br />
contraindicated in pregnancy and kidney<br />
disease.<br />
OCTA, in comparison, is a non-invasive<br />
technique that acquires volumetric<br />
angiographic information without the use of<br />
dye. Each three-dimensional scan set takes<br />
approximately six seconds to obtain. Enface<br />
images (OCT angiograms) can then be<br />
scrolled outward from the internal limiting<br />
membrane (ILM) to the choroid to visualise<br />
the individual vascular plexus and segment<br />
the inner retina, outer retina, choriocapillaris<br />
or other area of interest. In fact the 3 × 3 mm<br />
OCT angiograms appear to be of equivalent<br />
if not a higher resolution than the currently<br />
available FA/ICGA images. 6<br />
Exact delineation and size measurements<br />
can be performed for pathology such as<br />
choroidal neovascularisation (CNV) in “wet”<br />
age-related macular degeneration (AMD).<br />
OCTA also demonstrates changes in the<br />
choriocapillaris surrounding CNV lesions.<br />
Some of these changes are thought to occur<br />
prior to CNV development, which means that<br />
we may be able to identify patients who are at<br />
risk of developing wet AMD. 7<br />
OCTA has been used to assess optic nerve<br />
head perfusion in glaucoma. OCTA of<br />
glaucomatous optic nerves demonstrated a<br />
significant decrease in blood flow compared<br />
with controls. A correlation between blood<br />
flow in the disc and visual field pattern<br />
standard deviation was observed, implying an<br />
association between decreased perfusion of<br />
the optic disc and glaucoma severity. 8<br />
As well as AMD and glaucoma, OCTA<br />
reveals the vascular changes (impaired<br />
capillary perfusion, microaneurysm turnover,<br />
and quantification of blood flow) seen in<br />
conditions such as diabetic retinopathy, retinal<br />
vein occlusions and macular telangiectasia.<br />
Of course there are some limitations to<br />
OCTA. The area visualised is much smaller<br />
than with angiography, typically commercially<br />
available machines visualise a 6 x 6 mm<br />
area compared to the 200 degree imaging<br />
now available with wide angle FA and the<br />
leakage of dye is not appreciable making<br />
conditions such as chronic central serous<br />
chorioretinopathy difficult to diagnose.<br />
Conclusion<br />
We have been fortunate enough to have<br />
the AngioPlex OCT angiography upgrade on<br />
the Zeiss Cirrus HD-OCT at Eye Institute for<br />
the last two months. The technology has<br />
been incredibly useful for the assessment<br />
and treatment of patients with retinal<br />
Eye Institute appoints CEO<br />
Eye Institute has appointed a chief<br />
executive officer to spearhead the<br />
company’s future.<br />
Dr David Fitzpatrick-Cockram brings<br />
both the knowledge and expertise to<br />
take Eye Institute to the next chapter of<br />
its development as the practice has now<br />
reached a size where it will benefit from<br />
being professionally led, said Dr Peter Ring,<br />
one of Eye Institute’s original co-founding<br />
ophthalmologists. “It’s an exciting step. He<br />
will be able to bring a wealth of personal<br />
experience in the health care world to help<br />
Eye Institute to continue to stand out as an<br />
ever-improving provider of exceptional eye<br />
care.”<br />
In Auckland, as well as its flagship premises<br />
in Remuera, Eye Institute runs fullyfunctioning<br />
surgical and clinical facilities in<br />
Manukau and North Shore, with satellite<br />
clinics in New Lynn and St. Heliers.<br />
“We were seeking someone with<br />
exceptional qualities. We have found that<br />
in David. He will be able to help guide us<br />
Fig 1. This OCTA image shows<br />
ischaemia superior to the<br />
fovea in a superotemporal<br />
branch retinal vein occlusion.<br />
No amount of avastin will<br />
be able to bring the vision<br />
back in this ischaemic area<br />
Fig 2. Telangiectatic vessels<br />
can be seen temporal to the<br />
fovea in this patient with<br />
juxtafoveal telangiectasis<br />
Fig 3. A choroidal neovascular<br />
membrane can be<br />
identified in this image,<br />
colour coded by depth<br />
disease. Importantly<br />
OCTA has minimal,<br />
if any, impact on the<br />
amount of time that<br />
the patient spends in<br />
the clinic and reduces<br />
the need for further<br />
appointments for<br />
FA and ICG. We have<br />
access to immediate<br />
imaging that can<br />
be used for disease<br />
management.<br />
We realise this technology is still in its<br />
infancy, especially with regards to image<br />
interpretation, so in the present at least<br />
OCTA is not going to replace FA and ICG<br />
entirely, but it will decrease the need for<br />
these tests and will also allow us to provide<br />
a more accurate diagnosis in cases where the<br />
risk and inconvenience of FA or ICG makes<br />
us reluctant to use those techniques. The<br />
illustrated cases show that it is turning out<br />
to be a very valuable and frequently used<br />
adjunct for Eye Institute. ▀<br />
References<br />
1. Huang D, Swanson EA, Lin CP, et al. Optical coherence<br />
tomography. Science. 1991;254 (5035):1178-1181<br />
2. Imaging of macular diseases with optical coherence<br />
tomography. Puliafito CA, Hee MR, Lin CP, Reichel<br />
E, Schuman JS, Duker JS, Izatt JA, Swanson EA,<br />
Fujimoto JG. Ophthalmology. 1995 Feb;102(2):217-29<br />
3. Kim DY, Fingler J, Zawadzki RJ, Park SS, Morse<br />
LS, Schwartz DM, et al. Optical Imaging of the<br />
chorioretinal vasculature in the living human eye.<br />
Proc Natl Acad Sci. 2013;110:14354–9<br />
4. Spaide RF, Klancnik JM, Cooney MJ. Retinal Vascular<br />
Layers Imaged by Fluorescein Angiography and<br />
Optical Coherence Tomography Angiography. JAMA<br />
Ophthalmol. 2014; E1-6.<br />
5. Kwiterovich KA, Maquire MG, Murphy RP, Schachat<br />
AP, Bressler NM, Bressler SB, et al. Frequency<br />
of adverse systemic reactions after fluorescein<br />
angiography. Results of a prospective study.<br />
Ophthalmology. 1991;98:1139–42<br />
6. Matsunaga D, Puliafito CA, Kashani AH. OCT<br />
Angiography in Healthy Human Subjects.<br />
Ophthalmic Surg Lasers Imaging Retina.<br />
2014;45(6):510–5<br />
7. Jia Y, Bailey ST, Wilson DJ, Tan O, Klein ML, Flaxel CJ,<br />
et al. Quantitative Optical Coherence Tomography<br />
Angiography of Choroidal Neovascularization in<br />
Age-Related Macular Degeneration. Ophthalmology.<br />
2014;121:1435–44<br />
8. Jia Y, Wei E, Wang X, et al. Optical coherence<br />
tomography angiography of optic disc perfusion in<br />
glaucoma. Ophthalmology. 2014;121(7):1322-1332<br />
ABOUT THE AUTHORS<br />
* Dr Shanu Subbiah is a refractive cataract surgeon,<br />
with dual fellowship training in both retinal and<br />
corneal disease. He’s involved in clinical research<br />
into macular degeneration and retinal disease and is<br />
actively involved in teaching.<br />
Dr Peter Hadden is a refractive-cataract and retinal<br />
surgery specialist and a clinical senior lecturer in<br />
ophthalmology at the University of Auckland. He’s<br />
involved in several research programmes and has<br />
published more than six papers.<br />
Both are consultant ophthalmologists with Eye<br />
Institute.<br />
Dr Trevor Gray, Barbara Hare and Dr Peter Ring<br />
welcome new CEO Dr David Fitzpatrick-Cockram<br />
(second from left)<br />
to provide a level of service and excellence<br />
in eye care that’s unmatched by others,”<br />
said Dr Trevor Gray. “David’s experience as<br />
both a provider and a procurer of healthcare<br />
services gives him a unique insight into<br />
healthcare management.”<br />
Dr Fitzpatrick-Cockram has more than 25<br />
years of clinical training and experience,<br />
including qualifications in healthcare<br />
leadership from Yale University and post<br />
graduate qualifications in strategy and<br />
innovation from the University of Oxford.<br />
Prior to coming to New Zealand in 2013, the<br />
South African-born Dr Fitzpatrick-Cockram<br />
was director of innovation, director of mental<br />
health and professional lead for clinical<br />
psychology for the NHS in the UK. More<br />
recently he was the senior clinical lead at<br />
Southern Cross Health Society.<br />
Dr Fitzpatrick-Cockram said he was both<br />
delighted to have returned to the warmth of<br />
the Southern hemisphere and to be joining<br />
a leading ophthalmological practice like<br />
Eye Institute. “I have a passion for patientcentred<br />
excellence in healthcare and Eye<br />
Institute is the perfect place for me to<br />
contribute to New Zealand ophthalmology<br />
with such an amazing group of surgeons and<br />
the fantastic team that supports them.”<br />
Eye Institute general manager Barbara Hare<br />
will be assisting Dr Fitzpatrick-Cockram with<br />
the running of the practice and with project<br />
management under the new title of chief<br />
operating officer. ▀<br />
6 NEW ZEALAND OPTICS <strong>Apr</strong>il <strong>2016</strong>
Making the revolutionary, routine.<br />
CIRRUS HD-OCT with AngioPlex<br />
// ANGIOPLEX<br />
MADE BY ZEISS<br />
NEW<br />
ZEISS AngioPlex OCT Angiography<br />
Introducting All-New Technology<br />
Ultra-clear visualisation of microvascular blood flow using non-invasive CIRRUS OCT Angiography<br />
New vascular information<br />
• Ultra-clear 3D microvascular visualisations powered by OMAG C<br />
• OMAG C - the proprietary processing technique that detects motion of red-blood<br />
cells within sequential OCT B-scans performed repeatedly at the same location<br />
• Depth of retinal vasculature colour coded for ease of visual assessment<br />
Enhanced workflow<br />
• Ideal non-invasive, dye-free angiography<br />
• Single-Scan simplicity: capture OCT angiography with just one scan<br />
• Real-time tracking with FastTrac ensures artifact-free scans and precise<br />
location identification during follow-up visits<br />
ZEISS<br />
Ph: 1800 882 041 (AU)<br />
Ph: 0508 765 271 (NZ)<br />
med.au@zeiss.com<br />
<strong>Apr</strong>il <strong>2016</strong><br />
NEW ZEALAND OPTICS<br />
7
Auckland Eye celebrates new look<br />
Auckland Eye celebrated the complete<br />
refurbishment, expansion and<br />
modernisation of its headquarters at the<br />
end of February.<br />
Auckland Eye doctors and new chief executive<br />
Dr David Pendergrast, Arrow’s Mario Cross, Tracey Molloy,<br />
John Kelsey and Nia Stonex<br />
Peter Stoute with Drs Brian Kent-Smith and Hussain Patel<br />
Visionz<br />
With just over six months to go<br />
before New Zealand’s Premier Optical<br />
Event, Visionz <strong>2016</strong> opens its doors, it’s<br />
time to get organised and plan your visit.<br />
We hope 60 exhibitors will commit to Visionz<br />
<strong>2016</strong> which is being held in Auckland October<br />
14th - 16th October.<br />
WHERE<br />
Ellerslie Events Centre Ellerslie Auckland.<br />
Newmarket & Pakuranga Hunt Club Rooms<br />
WHEN<br />
Friday 14th October - 9.00am -6.00pm<br />
Saturday 15th October - 9.00am – 6.00pm<br />
Sunday 16th October - 9.30am -1.00pm<br />
<strong>2016</strong><br />
2014<br />
CONFERENCE PROGRAMME<br />
Education is one of the foundation elements of any good industry<br />
exhibition and at Visionz <strong>2016</strong> delegates have the opportunity to earn<br />
CPD and general points. Further details to follow.<br />
FREE ENTRY<br />
There is no charge for admission for all optical practitioners, practice<br />
managers, optical staff or students from the Auckland school of<br />
Optometry to the trade exhibition.<br />
For more Information, please contact: Gary Edgar at nzowa@live.com<br />
Registration details to follow.<br />
GRAND OPENING – 23 SEPT. <strong>2016</strong><br />
Deb Boyd, and the organisation’s former CEO<br />
Moira McInerney—who started the destruction<br />
and construction process, were joined by others<br />
involved in the project, including representatives<br />
from architects Jasmax and construction company<br />
Arrow, a host of optometrists, eye care company<br />
representatives and other special guests. All<br />
were invited to raise a glass to the new building<br />
and celebrate the end of the “noise, dust and<br />
disturbance” of the past several months.<br />
Dr Stephen Best and Dr David Pendergrast<br />
thanked attendees for their patience with their<br />
patients and support during the process, as<br />
the practice moved its clinic from one part of<br />
the building to another to maintain services<br />
throughout the duration of the project.<br />
Today the practice is larger and lighter, with more<br />
consulting rooms, waiting rooms and staff areas; a<br />
better flow between areas; no more leaky building<br />
concerns; and a whole new “less clinical” look and<br />
feel, explained Dr Pendergrast. What was two quite<br />
distinct buildings have now been joined into one,<br />
unified in their design, and related to Auckland Eye’s<br />
Oasis Surgical building, with the same external<br />
cladding, gable angles and through the use of<br />
external metal screens, which modify light entry<br />
and give the building a contemporary design. Dr<br />
Pendergrast joked there had been some arguments<br />
as to what the screens’ design represented. “They<br />
are endothelial cells from my point of view, but<br />
others say they are retinal epithelial cells, but we<br />
are decided they are cells of the eye.”<br />
Silmo Sydney<br />
partners<br />
with NRA<br />
New Australasian optical fair<br />
Silmo Sydney announced it will<br />
include an Independent Retailers<br />
Conference, which will be organised in<br />
partnership with the Australian National<br />
Retail Association (NRA).<br />
“The most successful trade shows are<br />
those which meet the needs of buyers and<br />
match them to sellers. The key is to present<br />
the right mix aligned to a common goal;<br />
it’s all about the balance,” said Gary Fitz-<br />
Roy, managing director of Silmo Sydney<br />
exhibition organisers Expertise Events.<br />
The Independent Retailers Conference<br />
programme will enable practitioners<br />
to pick up valuable retailing ideas that<br />
can have real impact and would not<br />
normally be available to them, said<br />
Fitz-Roy. “Quite often the industry is<br />
so focused on their practices that the<br />
behind-the-scenes every day running<br />
of the business doesn’t get the focus it<br />
should and it’s these aspects that can<br />
greatly affect profitability, such as leases,<br />
law and specific retailing training such as<br />
merchandising.<br />
“Our programme will run on the show<br />
floor and be made up of small concise<br />
sessions and visitors will have the<br />
opportunity to sit one-on-one with NRA<br />
specialists to discuss specifics.”<br />
Phillippa Pitcher, Naomi Meltzer and Dr Sarah Welch<br />
The newly refurbished building is also sustainably<br />
future-proofed with tanks for rainwater collection,<br />
the facility to add solar panels, room to grow and<br />
the ability for the practice to be flexible about how<br />
it uses its new, naturally-lit spaces. “The move to<br />
the reduced paper practice is accelerating, so we<br />
have made sure we have the IT infrastructure to<br />
support this,” said Dr Pendergrast.<br />
The refurbishment also allows space for the<br />
continued growth of Auckland Eye’s research<br />
department, headed by Dr Dean Corbett, while<br />
the increasing number of retinal specialists in the<br />
practice has allowed it to incorporate a dedicated<br />
retinal wing, including a small procedure room.<br />
“Tonight we wanted to say publicly that we are<br />
done and finished and back in business full speed,”<br />
summarised Dr Pendergrast. “And we have got to<br />
the finish line of what I think is an excellent<br />
result.” ▀<br />
In the same announcement, Silmo Sydney<br />
also announced that its official charity will<br />
be the Australian Royal Institute for Deaf<br />
and Blind Children (RIDBC). Funds will be<br />
donated to them from the exhibition and<br />
the organisation will have a presence at<br />
the show. “Children are our future and this<br />
is an extremely worthy cause. More than<br />
1 in 2,500 children in Australia have vision<br />
loss, there has been a 100% increase in<br />
vision-impaired children enrolled in RIDBC<br />
programmes in the last seven years,” said<br />
Fitz-Roy.<br />
“We promised to push the boundaries<br />
and create a world class event that<br />
unites the key market players and adds<br />
value to buyers. The involvement of NRA<br />
certainly adds real value and clout to the<br />
overall event; we are excited by what we<br />
have announced so far, but expect more<br />
exciting announcements soon. We have<br />
only just begun outlining our plans for<br />
SILMO Sydney.”<br />
Fitz-Roy said currently stand bookings<br />
are strong and Expertise Events was<br />
looking forward to hosting the Silmo Paris<br />
organising team in early <strong>Apr</strong>il when they<br />
come to conduct a site visit of the new<br />
Darling Harbour Centre.<br />
Silmo Sydney is set to take place from<br />
March 9-11. ▀<br />
ACBO runs<br />
basics seminar<br />
Optometrists from around New Zealand<br />
attended a seminar to learn about<br />
integrating behavioural optometry<br />
methods within their existing practice.<br />
Workshop leader Adrian Bell with ABCO member Keith<br />
Miller and CR Surfacing’s Steph Court and Lynton Dodge<br />
The Australian College of Behavioural<br />
Optometrists Kickstarter Seminar on February 21<br />
featured presentations and workshops by Adrian<br />
Bell, a Sunshine Coast-based optometrist with 30<br />
years’ experience in the field.<br />
The course was designed for new ACBO<br />
members or others getting started in Behavioural<br />
Optometry. In addition to a dinner, sponsored by<br />
CR Surfacing, attendees were taken on a step-bystep<br />
look at behavioural examinations, testing,<br />
decision-making and prescribing. It was also a reintroduction<br />
to near retinoscopy, an under-utilised<br />
tool, according to organisers.<br />
“This course is enough to make people start<br />
thinking and prescribing in different ways,” said<br />
Keith Miller, ACBO’s New Zealand director. “It’s<br />
using the tests they’re already doing but looking<br />
at the results in a slightly different manner.<br />
They’re learning new ways and getting a better<br />
understanding of using the retinoscope for<br />
investigating what a person is doing with their<br />
visual system when they’re, say, reading.”<br />
Bell took the group through an afternoon session<br />
that ended in a workshop on the retinoscope.<br />
“Retinoscopy is one of those things that some<br />
people think we don’t need any more. But I will<br />
encourage you to get your ret out, charge it, blow<br />
off the dust, because it’s a great way of observing<br />
vision, in a dynamic sense.”<br />
Bell said the retinoscope provides a dynamic view,<br />
over time, of where patients are focusing and even if<br />
they are paying attention. He also discussed methods<br />
for using the retinoscope with younger patients.<br />
“Remember your refraction is a subjective<br />
test. Retinoscopy is much more objective. You’re<br />
directing attention to a particular place, but you’re<br />
more in control. It’s objective, real-time and it’s<br />
dynamic. The focus moves, the eyes move, the<br />
reflex moves.”<br />
Feedback from the 27 attendees was positive,<br />
said Miller. If optometrists wanted to pursue<br />
behavioural optometry and earn certification,<br />
they can attend additional seminars offered over<br />
the year. March’s Practical Vision Therapy NZ -<br />
Workshop 1 with New Zealand optometrist Evan<br />
Brown was sold out.<br />
“There really are not enough behavioural<br />
optometrists in New Zealand,” Miller said. “With<br />
one-in-five children suffering a vision-related<br />
problem that can interfere with their learning,<br />
there’s a lot that could be done. But if all those<br />
children came to a behavioural optometrist for<br />
examination and vision care, we couldn’t cope.<br />
But [they] aren’t seeking help because they don’t<br />
know; nobody is offering them the appropriate<br />
levels of care.” ▀<br />
REINVENTING BUSINESS.<br />
23> 26 SEPT. <strong>2016</strong><br />
PARIS NORD VILLEPINTE<br />
Conception : CARLIN<br />
SILMOPARIS.COM<br />
Neuro-ophthalmology evening from CVRT<br />
BY DR JESSE GALE*<br />
The first Capital Vision Research<br />
Trust (CVRT) education event for<br />
<strong>2016</strong> was themed around neuroophthalmology.<br />
Many optometrists and<br />
ophthalmologists feel less confident dealing<br />
with neuro-ophthalmic complaints because<br />
the cause of the problem is not usually visible<br />
with the slit lamp. The presenters were fellow<br />
Wellington neuro-ophthalmologist Dr Neil<br />
Aburn and myself.<br />
I started with a talk on abnormalities<br />
of the pupil, where I discussed various<br />
physiological and pathological aspects from<br />
the interesting melanopsin ganglion cells,<br />
to tips on examining pupils and measuring<br />
a relative afferent pupil defect (RAPD),<br />
causes of light-near dissociation, and a<br />
number of cases of anisocoria.<br />
Dr Aburn presented on optic neuropathies<br />
with a great range of varied cases to<br />
demonstrate the crucial principles about<br />
how the history guides the differential<br />
diagnosis and investigation. Among<br />
the interesting cases were both the<br />
common and bizarre, from urgent medical<br />
emergencies to gradual inherited problems.<br />
Our sponsor OptiMed made a brief<br />
presentation on the scanning laser<br />
ophthalmoscope called Eidon, which takes<br />
wide-field retinal images without dilation.<br />
I then presented another talk on diplopia,<br />
with cases to illustrate several important<br />
principles and some of the important<br />
patterns to recognise. Cases of monocular<br />
diplopia, cranial nerve palsies, myasthenia<br />
and orbital disease were covered, with<br />
emphasis on red flags. Both Dr Aburn and<br />
I tried to use plenty of case studies and<br />
questions to stimulate thought and draw<br />
feedback from the participants and to<br />
highlight the underlying principles and safety<br />
issues of these challenging presentations.<br />
Other CVRT education event dates for<br />
Wellington in <strong>2016</strong> are: Wednesday <strong>Apr</strong>il<br />
25, Wednesday August 24 and Thursday<br />
December 1. For more information, please<br />
visit www.capitalvision.org.nz or email<br />
info@capitalvision.org.nz. ▀<br />
ABOUT THE AUTHOR<br />
* Dr Jesse Gale is an ophthalmologist with Capital &<br />
Coast District Health Board and Capital Eye Specialists<br />
in Wellington. He is a new board member at Capital<br />
Vision Research.<br />
8 NEW ZEALAND OPTICS <strong>Apr</strong>il <strong>2016</strong>
A NEW LOOK FOR AUCKLAND EYE<br />
After nearly two years of building,<br />
refurbishment, expansion and<br />
modernisation, Auckland Eye is delighted<br />
to announce the completion of our new<br />
and improved St Marks Road site.<br />
Welcome to the future of ophthalmic care<br />
Now finished, our new development reinforces<br />
Auckland Eye’s position as a state-of-the-art<br />
consulting facility, allowing us to accommodate<br />
future technological developments as they arise, in this<br />
highly specialised and fast-moving field.<br />
A better working environment<br />
We hope patients will enjoy the new look clinic as much as<br />
our doctors and staff do. With more consulting rooms, new<br />
examination equipment and allocated space for dedicated<br />
services like our research department headed by Dr Dean<br />
Corbett, it’s a win-win for everyone concerned.<br />
A new vision for all<br />
We believe everyone will benefit from what has been a<br />
ground-up refurbishment. Our patients remain our first<br />
priority. They will enjoy the welcoming atmosphere, the<br />
new and modernised waiting areas and facilities, enhanced<br />
by the use of natural light throughout the practice –<br />
designed to provide a better overall patient experience.<br />
Our doctors and support staff will continue to provide<br />
their expertise and perform their vital roles as ever, in<br />
a centre purposely designed for ophthalmology in the<br />
21st century.<br />
Design with focus<br />
The new clinic design unifies the two previously very<br />
different parts of the building and integrates us perfectly<br />
with our premier day-stay centre, Oasis Surgical.<br />
The new front site houses our dedicated retinal suite, designed<br />
to allow the team to provide the specialised care that patients<br />
with medical and surgical retinal problems require. The previous<br />
Auckland Eye building has been extended to cater for all eye<br />
care needs, with all areas benefitting from a modernised look<br />
and feel. Exterior cladding and external screens blend the two<br />
parts of the practice together seamlessly.<br />
Sustainability and<br />
future-proofing<br />
Wherever possible, we have incorporated sustainable<br />
technology into our new design. This includes tanks for<br />
rainwater re-use, high performance insulation, double-glazing<br />
and the facility to add solar panels in the near future.<br />
See our lives change<br />
So here’s to the new look Auckland Eye. We’d like to say<br />
thank you to everyone involved in the refurbishment – not<br />
least our patients who have been very understanding with the<br />
disruptions; our development partners who have done such<br />
an outstanding job and of course to you, our referrers, who<br />
have continued to support us throughout.<br />
With the move towards a paper-reduced practice accelerating,<br />
we have also made sure we have the IT infrastructure in place<br />
to support this, including dedicated server rooms, UPS, data<br />
cabling and upgradeable and expandable hardware.<br />
www.aucklandeye.co.nz<br />
<strong>Apr</strong>il <strong>2016</strong><br />
NEW ZEALAND OPTICS<br />
9
Photo by ACBO’s Kickstarter Seminar keynote, optometrist Adrian Bell<br />
Great day for MDNZ<br />
Macular Degeneration NZ hosted the<br />
third annual charity race day on<br />
February 20. The summer sun shone,<br />
360 guests filled the Guineas Ballroom at the<br />
Ellerslie Racecourse in Auckland—dressed in<br />
their “race day best”—and everyone had a<br />
wonderful time.<br />
“We are very grateful for the ongoing support<br />
from New Zealand’s ‘eye world’ for this annual<br />
event as without them there simply would be<br />
no event,” said Philippa Pitcher, MDNZ general<br />
manager.<br />
In her welcoming address Dr Dianne<br />
Sharp, MDNZ chair and Retina Specialists’<br />
ophthalmologist, told race day guests of<br />
the revolution over the last few years in the<br />
treatment of macular degeneration, even for<br />
the most severe cases, and the ability today to<br />
deliver amazing results for people who would<br />
otherwise experience significant troubles and<br />
hardship. Timing is critical, she said, and MDNZ<br />
is working to seize this opportunity to save sight<br />
by raising awareness and ensuring good access<br />
to treatment for everyone across the country.<br />
Race day guests were treated to a superb<br />
buffet lunch, a great day of racing and a brilliant<br />
selection of goodies in the auctions and raffles.<br />
Many also took up the opportunity to get even<br />
closer to the action through the exciting race<br />
day experiences. People went home very happy<br />
whether they won or lost, said Pitcher, with<br />
many enjoying the additional compensation of a<br />
surprise bottle of wine to take home when their<br />
“losing ticket” was drawn and became a winner<br />
after all.<br />
MDNZ Ambassadors Sir Colin Meads, John<br />
Adshead and Viv Jones joined guests on the day,<br />
while others were there in spirit if not person<br />
(due to other commitments) by providing<br />
exciting auction items, securing tables of ten or<br />
making other forms of donations. Once again<br />
Sir Colin produced two signed rugby balls to<br />
add to the auction proceeds.<br />
“The day was a great success, raising $45,000<br />
for MDNZ to continue its sight saving work for<br />
which we are very grateful,” said Pitcher. ▀<br />
The <strong>2016</strong> MDNZ 1600 race supporters group<br />
OIC’s Tim Way with Karen and Alan Saks<br />
Richard and Joy Goddard, Kumuda Setty, Chris Aldous and Barbara and Darren Savage<br />
with the winner of the Essilor 1200, Kinagat, and his jockey Chris Johnson<br />
Dr Sarah Welch, Yvonne New, Philip Walsh, Janet Wigmore, Tracey Molloy, Dr Archie McGeorge, Dr Kathryn<br />
Philipson, Lahiru Gunasena and Bethan Rajwer supporting the Auckland Eye Avondale Guineas<br />
NZ Optics’ designer Kirsten Newton with her<br />
wonderful hat and new ed. Jai Breitnauer<br />
MDNZ’s fascinator brigade: Sandy Grant, Julie Worsley,<br />
Viv Jones, Sandra Budd and Phillippa Pitcher<br />
OptiMed’s Mokta and Chris Simonson, Kerry and Craig<br />
Norman, and Robert and Karen Nyenkamp<br />
Dr Dianne Sharp, Vicki Lindsay, Julianne Horgan, Zanelle and Neville Angelo<br />
and Drs Narme Deva, Andrea Vincent and Rachel Barnes<br />
Julie Worsley, Dr Ian Elliott and Glenda<br />
Bostwick<br />
Auctioneer Michael Boulgaris, Di Goldsworthy and<br />
“best dressed lady” Paula Farrar<br />
10 NEW ZEALAND OPTICS <strong>Apr</strong>il <strong>2016</strong><br />
Hamilton Eye’s Selma Matloob, Monika Pradhan, Marina Nasmith, Joanna Hood, Sally<br />
Rosenberg and Jena Youdif, backing the Hamilton Eye Clinic 1600<br />
The team from Blackmores, including country manager Deva Dhar (left of banner) with<br />
Saint Emilion, winner of the opening MDNZ 1500 race and the horse’s trainers and owners
oDocs goes commercial,<br />
seeks investment<br />
Innovative New Zealand startup and social<br />
enterprise oDocs Eye Care is rolling out its first<br />
commercial products in <strong>Apr</strong>il.<br />
oDocs (short for OphthalmicDocs) is the<br />
brainchild of registrar Dr Sheng Chiong Hong<br />
and Dr Benjamin O’Keeffe, senior house officer<br />
of ophthalmology at Wellington Eye Clinic. Its<br />
fundamental initiative was the development of<br />
an inexpensive system combining smartphones<br />
with 3D printable attachments to allow accurate,<br />
mobile visual acuity tests, slit-lamp examinations<br />
and retinal imaging with a lens that gives a 50<br />
degree field of view into the back of the eye. Sales<br />
of oDocs’ commercial products will help underwrite<br />
efforts to provide devices to health services in<br />
under-served and remote areas, especially in the<br />
developing world.<br />
To this end the company has launched visoScope,<br />
an upgraded version of its original Fundus product,<br />
and visoClip, a tool for viewing the anterior segment.<br />
“We’ve reduced the Fundus to a simplified form<br />
with a stronger structure and less parts, making it<br />
ultimately more efficient to build, and we’ve evolved<br />
it using better suited manufacturing techniques for<br />
higher quality. The lenses will be included so it will<br />
be ready to go out of the box,” says Hanna Eastvold-<br />
Edwins, oDocs chief executive officer.<br />
Keeping its social ideals at the forefront of the<br />
commercial part of the operation, oDocs is running<br />
a pre-order campaign, where half of the profits<br />
generated will go into research, education and<br />
supply of equipment to those regions most in<br />
need, says Dr Hong.<br />
oDocs will market visoScope and visoClip to<br />
ophthalmologists and optometrists. The products<br />
work with an app that currently runs on iOS<br />
tablets and handsets only. Eastvold-Edwins says<br />
the company will develop an Android app in the<br />
near future.<br />
The commercial products will be targeted at the<br />
New Zealand market first, while the company seeks<br />
approval for commercial sales in overseas markets,<br />
oDocs’ Dr Sheng Chiong Hong accepting a highly<br />
commended award at NZ Innovators <strong>2016</strong> in February<br />
from former Prime Minister Jim Bolger<br />
oDoc’s new visoScope and visoClip<br />
particularly Europe and the Americas. oDocs will<br />
begin to raise investment capital following the<br />
commercial rollout, says Eastvold-Edwins.<br />
“We are self-funded up to this point, but we will<br />
be actively seeking investment. We are hoping to<br />
attract an investor who understands how these<br />
innovations could impact eye health, not just for<br />
developed markets, but also emerging ones who<br />
really embrace mobile health technology.<br />
“At our core, we are an innovative technical team<br />
working on a medical hardware product with the<br />
potential to go global.”<br />
Eastvold-Edwins says oDocs aims to sell 1,000 kits<br />
this year. The units will be sold online with delivery<br />
expected by third quarter <strong>2016</strong>. Once the company<br />
achieves sustainability, it will develop more<br />
advanced iterations of the product, she says.<br />
To find out more go to www.odocs-tech.com. ▀<br />
New doctor for Christchurch Eye<br />
Christchurch Eye Surgery announced that<br />
Dr Logan Robinson has joined its team<br />
as an experienced cataract surgeon with<br />
subspecialty training in vitreoretinal surgery and<br />
diseases of the retina and macula.<br />
Dr Robinson joins Drs Jim Borthwick and Sean<br />
Every to complete Christchurch Eye Surgery’s<br />
surgical retinal team at the only private facility in<br />
Christchurch with a vitreoretinal surgical suite.<br />
Graduating from the University of Otago, Dr<br />
Robinson undertook his ophthalmology training in<br />
Wellington and Christchurch. He then completed<br />
vitreoretinal surgery fellowships in Wellington and<br />
at Manchester Royal Eye Hospital in the United<br />
Kingdom, where he learned the latest techniques<br />
in vitreoretinal and cataract surgery.<br />
He took up a position as a consultant<br />
ophthalmologist at Christchurch Hospital in 2015,<br />
where he is involved in the training of junior<br />
ophthalmologists as well as educational sessions<br />
for GPs and optometrists. He also joined the team<br />
at Southern Eye Specialists.<br />
Dr Robinson says he believes it is important<br />
to communicate clearly with his patients so<br />
they have a good<br />
understanding of<br />
their condition and<br />
can make informed<br />
decisions about<br />
their treatment.<br />
“When I returned<br />
to Christchurch I<br />
wanted to operate<br />
in a modern, wellequipped<br />
facility so<br />
Dr Logan Robinson<br />
I could provide the highest quality of surgical care<br />
for my patients. Christchurch Eye Surgery more<br />
than meets my expectations. It has state-of-the art<br />
surgical equipment and technology, together with<br />
experienced and friendly staff and a beautifullydesigned<br />
building. This combination makes for the<br />
best experience possible for the patient.”<br />
Away from ophthalmology, Dr Robinson is an avid<br />
sports fan and enjoys mountain-biking, golf and<br />
fishing when he isn’t spending time with his wife<br />
and young son.<br />
Christchurch Eye Surgery opened its doors in<br />
June 2014. ▀<br />
Christchurch education day<br />
Around 60 optometrists gathered for a daylong<br />
seminar in Christchurch in February,<br />
the third consecutive year for this event.<br />
Drs Zainah Asagloff, Antony Bedggood, David<br />
Kent, Ainsley Morris and Logan Robinson gave<br />
presentations this year.<br />
Dr Morris said she really enjoys the annual day<br />
spent with the optometrists—both local and<br />
from around the country. “It is a chance to learn<br />
together, build on the importance of collaboration,<br />
especially in the therapy and treatment of patients,<br />
as well as having a great day with nice people.”<br />
Dr Morris, in her first presentation, discussed<br />
pseudophakic macular oedema. The essentials of<br />
recognition and diagnosis were detailed and the<br />
importance of appropriate treatment and advice<br />
to patients emphasised. While in Glaucoma—to<br />
treat or not to treat, Dr Morris discussed conditions<br />
which can mimic glaucoma, aren’t pathological,<br />
but which have high pressures and the important<br />
fact that not all patients who develop glaucoma<br />
will lose sight over their lifetime.<br />
Dr Kent presented on corneal collagen cross<br />
linking with riboflavin (CXL)—indications,<br />
techniques and post-operative management. He<br />
covered the physicochemical changes that occur<br />
in the cornea during CXL, the original Dresden<br />
protocol and what the published studies of CXL<br />
show. The primary indication for CXL is progressive<br />
corneal ectasia including keratoconus and post-<br />
LASIK keratectasia. He discussed accelerated CXL<br />
and whether it may or may not be as effective as<br />
the original protocol and he covered post-operative<br />
management and expected clinical course.<br />
Dr Kent’s second talk was on multifocal and<br />
extended-depth-of-focus IOLs. He discussed both<br />
bifocal and trifocal diffractive multifocal IOLs and<br />
that the trifocal IOLs, such as Zeiss and FineVision,<br />
have now superseded the older bifocal IOLs. He<br />
also discussed the pros and cons of the different<br />
types of extended-depth-of-focus IOLs.<br />
His third talk was on post-LASIK keratectasia<br />
where he discussed his own cases and reviewed<br />
the risk factors and how they have been managed.<br />
He emphasised that any post-LASIK patient who<br />
develops increasing astigmatism needs corneal<br />
topography to exclude keratectasia and that CXL<br />
should be done earlier before it progresses. Dr<br />
Kent’s final talk was on the history of LASIK.<br />
Dr Robinson discussed the new OCT-based<br />
classification system for vitreomacular adhesion,<br />
vitreomacular traction, full-thickness macular<br />
holes and lamellar macular holes. He also spoke on<br />
how to differentiate papilloedema from pseudopapilloedema,<br />
with the most important message<br />
being to consider the entire clinical picture when<br />
assessing an elevated disc, and he gave tips on how<br />
to use OCT to differentiate between disc drusen<br />
and papilloedema. Dr Robinson’s final talk was<br />
on pigmented lesions of the retina and choroid,<br />
and in particular how to differentiate between a<br />
choroidal nevus and choroidal melanoma using<br />
the mnemonic: “To Find Small Ocular Melanoma<br />
Using Helpful Hints Daily”. Using this will prompt<br />
timely referral for high risk lesions, allowing earlier<br />
diagnosis, he said.<br />
In Eye diseases in South East Asia, Dr Asagloff<br />
made the following points:<br />
••<br />
Asians are more prone to endophthalmitis<br />
from blepharitis<br />
••<br />
Asian eyelids can have epicanthal folds/<br />
epiblepharon<br />
••<br />
In thyroid orbital inflammation, optic nerve<br />
compression is more common<br />
••<br />
In a submacula bleed, look out for PCV<br />
••<br />
Giant cell arteritis is most uncommon<br />
Speakers: Drs Zainah Asagloff, Logan Robinson, Antony<br />
Bedggood, Ainsley Morris and David Kent<br />
Dr Ainsley Morris (second from left) and optometrists<br />
Gavin Lim, Suney Cheung, Rochelle van Eysden and<br />
Michaella Dolling<br />
••<br />
In a bilateral panuveitis, VKH is a common cause<br />
••<br />
Angle-closure glaucoma is more common<br />
In angle-closure glaucoma, optometrists can play<br />
a vital role in detecting patients who have narrow<br />
angles before they progress to glaucoma, she said.<br />
“It is vital to detect shallow anterior chambers.<br />
And this should lead to examination of the angles,<br />
via Gonioscopy or Imaging.” Imaging modalities<br />
include the eyeCam, Scheimpflug photography,<br />
UBM and AS-OCT.<br />
Dr Asagloff went on to discuss the diagnosis<br />
of dry eyes, which can be diagnosed by simple<br />
clinical means using tests such as TBUT, Schirmer’s,<br />
staining or meniscus level. Optometrists should<br />
look for the treatable underlying cause, she said,<br />
and refer to an ophthalmologist if the dry eye<br />
is moderate to severe and if there is a definite<br />
underlying cause to treat.<br />
Dr Bedggood explained how paediatric<br />
ophthalmology is challenging, with potentially<br />
sight or life-threatening diseases presenting few<br />
or no symptoms. Fortunately there are some<br />
quite specific patterns and ‘mantras’ that can be<br />
followed.<br />
Causes of red eye in children were discussed<br />
and, apart from the rare and serious causes of<br />
retinoblastoma or rhabdomyosarcoma, they<br />
are mainly corneal and anterior segment diseases,<br />
often chronic and more aggressive than in adults.<br />
Corneal opacities and vascularisation due to<br />
staphylococcus/blepharitis is one of these, he said.<br />
Glaucoma in children and young adults is rare<br />
and universally has high IOP, so a large disc, big cup<br />
and normal IOP need not be a ‘suspect’ in someone<br />
less than 35, said Dr Bedggood, while genetic<br />
causes related to the Myocillin gene predominate.<br />
Children from five years of age presenting with<br />
bilaterally reduced vision, often mild at first, need<br />
to be “robustly followed up” and sometimes tested<br />
for retinal dystrophies, he added. “Subtle macular<br />
signs, OCT changes, retinal flecks and family history<br />
are key findings.”<br />
Finally Dr Bedggood discussed the care of children<br />
with low vision. “Providing excellent services<br />
and communicating between ophthalmologist,<br />
optometrist, BLENNZ and parents is an important<br />
priority for all of us.”<br />
Seminar organised by Fendalton Eye Clinic. Words<br />
supplied by speakers. ▀<br />
Opportunity for Community Optometrists<br />
A fantastic opportunity for optometrists who are motivated to upskill in the assessment, diagnosis and treatment<br />
of glaucoma is offered by the Department of Ophthalmology, The University of Auckland. We have established a<br />
collaborative glaucoma clinic with the Department of Ophthalmology Auckland District Health Board. The long<br />
term vision of this clinic is as a gateway to providing community based glaucoma care in the future.<br />
For further information about this clinic and associated cost please contact:<br />
Sue Raynel<br />
Department of Ophthalmology<br />
The University of Auckland<br />
Ph: (09) 923-6337 or e-mail: s.raynel@auckland.ac.nz<br />
<strong>Apr</strong>il <strong>2016</strong><br />
NEW ZEALAND OPTICS<br />
11
with<br />
Prof Charles McGhee<br />
& A/Prof Dipika Patel<br />
Series Editors<br />
The ABCs of OCT in glaucoma<br />
Background<br />
BY HANNAH KERSTEN*<br />
AND PROFESSOR HELEN DANESH-MEYER<br />
Glaucoma is a multifactorial optic neuropathy characterised by<br />
slowly progressive degeneration of the retinal ganglion cells and<br />
their axons. Unfortunately, there is not yet one single test that can<br />
discriminate glaucomatous eyes from normal eyes; the diagnosis<br />
of glaucoma is made based on a specific pattern of structural and<br />
functional changes. In the past, the retinal nerve fibre layer (RNFL)<br />
was only able to be assessed subjectively by slit-lamp examination<br />
and retinal photography, providing qualitative data. Optical<br />
coherence tomography (OCT) was first described by Huang and<br />
colleagues in 1991 1 . OCT, as used to acquire high resolution, crosssectional<br />
images of the ocular structures, utilises low-coherence<br />
near infrared light (800-1400 nm) generated by a super-luminescent<br />
diode, which passes through the pupil to the posterior structures<br />
of the eye 1 . It is analogous to B-scan ultrasound except that it uses<br />
light instead of sound. Over the past 10 to 15 years, OCT has become<br />
an invaluable tool and is in widespread use in both optometry<br />
and ophthalmology. OCT is used in the diagnosis and longitudinal<br />
analysis of a multitude of ophthalmic disorders that affect the optic<br />
nerve and macula, including glaucoma. Newer spectral-domain OCT<br />
has increased resolution (approximately 3 – 5 µm) and faster scan<br />
acquisition time than older time-domain OCT technology. Common<br />
spectral-domain OCT models include the Zeiss Cirrus and the<br />
Heidelberg Spectralis.<br />
Peripapillary Retinal Nerve Fibre Layer Measurements<br />
Measurement of the peripapillary RNFL thickness using OCT<br />
is now a routine component of the comprehensive glaucoma<br />
assessment. In healthy eyes, the RNFL is generally thickest in<br />
the in the inferior quadrant, followed by the superior, nasal and<br />
temporal quadrants (the “ISNT” rule). There is, however, a large<br />
degree of RNFL variability in “normal” eyes, and there is some<br />
overlap in the structural characteristics of normal eyes and eyes<br />
with early optic nerve damage due to glaucoma 2 . Many patients<br />
will have anomalous structural features that may confound<br />
the interpretation of OCT measurements, and the eye may be<br />
incorrectly classified as “abnormal”. In patients with perimetric<br />
glaucoma, the location of the RNFL thinning should correlate<br />
with the visual field defect. In those with pre-perimetric disease,<br />
it is important to compare the peripapillary RNFL thickness in the<br />
individual quadrants with the appearance of the optic nerve head<br />
on clinical examination.<br />
The ability to detect and measure structural change is essential<br />
in the diagnosis and management of glaucoma. Progression<br />
analysis software, included with some OCT models, is able to<br />
track the progression of RNFL thinning over time (figures 1 and 2).<br />
It is necessary to review the RNFL overview at each visit, as well<br />
as the progression scans, as these overview scans will give more<br />
comprehensive information regarding RNFL thickness in each eye<br />
(as well as the differences between the two eyes). It is important<br />
to discriminate true disease-related changes from measurement<br />
variability and normal age-related change. When a scan is accurate<br />
and well-centred, the 95% tolerance for average RNFL thickness<br />
is approximately 4 µm 2 . Spectral-domain OCT is more sensitive at<br />
detecting glaucoma progression than time-domain OCT 3 .<br />
Fig 1. Guided progression analysis on Zeiss Cirrus OCT. This shows progression of left RNFL<br />
thinning. The first two exams are used as baseline measurements, with subsequent scans<br />
compared to baseline. The signal strength is good in all scans however the first baseline shows<br />
an area nasal to the optic disc with an incomplete scan, hence the reason for the lower average<br />
RNFL thickness in Baseline 1 compared with Baseline 2. Over time, there has been a significant<br />
reduction in RNFL thickness in both the superior and inferior quadrants.<br />
Fig 2. Guided progression analysis on Zeiss Cirrus OCT. This shows stable RNFL thickness over<br />
six consecutive OCT scans. There is marked RNFL thinning, particularly in the superior and<br />
inferior quadrants. The fluctuation in average RNFL thickness between exams is within the 95%<br />
confidence limits for scan repeatability. Signal strength is adequate in all scans.<br />
Macular OCT Scans in Glaucoma<br />
Although the use of OCT in glaucoma has been primarily focused on<br />
the assessment of peripapillary RNFL thickness, in recent years the<br />
macular region has emerged as an area of interest; glaucomatous<br />
macular damage can occur early in the disease process. Although the<br />
macular region represents less than 2% of the retinal area, it contains<br />
30% of the retinal ganglion cells 4 . One of the main advantages of<br />
12 NEW ZEALAND OPTICS <strong>Apr</strong>il <strong>2016</strong><br />
macular assessment in glaucoma is that a significant portion of<br />
retinal thickness at the macula is composed of the RNFL, ganglion<br />
cell layer and the inner plexiform layer. Spectral-domain retinal<br />
layer segmentation algorithms have allowed for the quantification<br />
of individual layers in the macular region, and the measurement<br />
of ganglion cell complex thickness (the combined thickness of the<br />
RNFL, ganglion cell layer and the inner plexiform layer, although<br />
macular analysis in some OCT models includes only the ganglion<br />
cell and inner plexiform layers) 3 . The GCC thins as the glaucomatous<br />
damage progresses, with lower thickness values associated with<br />
poorer mean deviation scores on visual field testing 2,5 . Ganglion cell<br />
complex thickness in glaucoma can correlate well with RNFL thinning<br />
and visual field loss (figure 3). Repeatability of ganglion cell complex<br />
measurements may be reduced in more advanced glaucoma 6 .<br />
Fig 3. Structure-function correlation. The top left image shows a glaucomatous right optic nerve<br />
with vertical elongation of the optic cup and thinning of the superior and inferior neuroretinal<br />
rim. The rim thinning is most pronounced inferiorly. This correlates with functional changes on<br />
visual field testing, with almost complete loss of the superior visual field, and greatly reduced<br />
sensitivity in the inferior visual field. The lower images show diffuse thinning of the ganglion<br />
cell complex (measured with the Zeiss Cirrus OCT), with more extensive thinning in the inferior<br />
region. This correlates with the optic nerve and visual field appearance.<br />
Consider Other Ocular and Systemic Pathology<br />
Glaucoma is not the only condition that can cause thinning of the<br />
retinal layers. A vast number of ocular and systemic disorders can<br />
lead to peripapillary RNFL and macular thickness changes on OCT<br />
and it is always important to consider these conditions as part of<br />
the examination process. A comprehensive history and complete<br />
eye examination is essential. The patterns of RNFL loss can vary<br />
greatly between conditions. For example, patients with optic neuritis<br />
are more likely to have temporal RNFL thinning (figure 4) and the<br />
degree of RNFL loss may be out of proportion to visual field results.<br />
Multiple sclerosis is associated with thinning of the RNFL and macula<br />
(including the ganglion cell complex), even in patients with no history<br />
of optic neuritis 7 . Patients with compressive optic neuropathies<br />
can present with thinning of the RNFL. These patients are likely to<br />
have reduced RNFL thickness in the nasal and temporal quadrants<br />
compared with glaucoma patients 8 . A tilted disc, particularly in<br />
myopic patients, can cause a localised RNFL defect in the superior or<br />
inferior quadrants, similar to glaucomatous RNFL loss 9 . Longitudinal<br />
follow-up is necessary to determine whether the RNFL thinning is<br />
glaucomatous or due to the tilting of the optic nerve head 10 .<br />
Fig 4. RNFL thinning in a patient with a history of optic neuritis. This patient had a single episode<br />
of right optic neuritis (confirmed by MRI examination). Note the dramatic reduction in RNFL<br />
thickness, particularly in the temporal quadrant (less likely to be affected in glaucoma). The<br />
average RNFL thickness was 55 µm. The visual field was normal.<br />
Factors Affecting OCT Measurements<br />
A number of factors influence the quality and accuracy of retinal<br />
measurements acquired with OCT:<br />
••<br />
Image resolution is affected by eye movement. The degradation<br />
of the image is a function of the frequency and size of saccadic<br />
eye movements, compared with the image acquisition time and<br />
the transverse resolution of the OCT 11 . Newer OCT technology<br />
attempts to counter this with the use of eye-tracking systems<br />
incorporated into the software 12 .<br />
••<br />
Scans should be well-centred: macular scans should be centred<br />
at the fovea and accurate measurement of the peripapillary<br />
RNFL requires the reference to be centred precisely at the optic<br />
nerve head 13 .<br />
••<br />
The signal strength of the scan needs to be adequate.<br />
Recommended minimum signal strength varies by manufacturer.<br />
Even scans with adequate signal strength may show software<br />
segmentation failure, where the automatic segmentation of<br />
the retinal layers is incorrect. If possible, these scans should be<br />
re-taken.<br />
••<br />
Scans can be acquired effectively over a range of pupil sizes,<br />
however if the pupil size is less than 3 mm this can affect<br />
thickness measurements and scan quality 14 .<br />
••<br />
Opacities of the lens generally give rise to lower thickness<br />
values (affecting results by up to 12%), with more advanced lens<br />
opacities leading to a greater decrease in thickness 14 . Image<br />
repeatability significantly improves following cataract extraction<br />
••<br />
OCT measurements are affected by axial length and,<br />
subsequently, refractive error 15 , and measurements are most<br />
accurate within the range of +5 to -5 dioptres 14,16 . Longer, more<br />
myopic eyes tend to have thinner RNFL thickness values 15 .<br />
••<br />
RNFL values for people of different ethnicities vary modestly,<br />
although it has been found that all ethnicities examined had<br />
95% confidence limits that overlapped 15 .<br />
••<br />
RNFL thickness decreases with age - by approximately 2 µm per<br />
decade, with loss of about 5000 axons per year 15 .<br />
Anterior Segment OCT in Glaucoma<br />
It is worth briefly mentioning the role of OCT in the examination of<br />
the anterior segment of glaucoma patients. Anterior segment OCT<br />
imaging, using a 1310 nm light source, permits the visualisation<br />
of the angle structures and provides quantitative data that can be<br />
useful in the identification of the mechanism of IOP elevation and<br />
the diagnosis of angle closure glaucoma (figure 5) 17,18 . OCT of the AC<br />
angle is a tool that is a useful addition to gonioscopy, but it should<br />
not replace gonioscopic examination. It can be used to measure<br />
the actual size of the angle, and is also particularly helpful for<br />
visualising structural changes to the angle following YAG peripheral<br />
iridotomy. Anterior segment OCT can also be used to as a noninvasive<br />
measure of central corneal thickness, a useful measure in<br />
initial glaucoma assessment.<br />
Fig 5. Anterior segment OCT scan showing narrow anterior chamber angles<br />
Conclusion<br />
There have been significant developments in glaucoma imaging<br />
over the last decade, and these imaging modalities, particularly<br />
OCT scans of the peripapillary RNFL and macula, are now used<br />
routinely in glaucoma diagnosis and on-going management. There<br />
are continuous advances in spectral-domain OCT technology, with<br />
increased resolution, reduced scan acquisition time, progression<br />
analysis software updates, en face imaging and eye movement<br />
tracking allowing for more accurate and reproducible scans, and<br />
more in-depth analysis of the ocular structures. Although OCT<br />
examination is an important component of the modern glaucoma<br />
assessment, it is not a diagnostic tool 3 ; it is a useful test in the<br />
armamentarium of the ophthalmologist and optometrist, and it<br />
should be used in conjunction with other measures of optic nerve<br />
structure and function. ▀<br />
References<br />
1. Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science 1991;254:1178-1181.<br />
2. Grewal DS, Tanna AP. Diagnosis of glaucoma and detection of glaucoma progression using spectral<br />
domain optical coherence tomography. Curr Opin Ophthalmol 2013;24:150-161.<br />
3. Bussel, II, Wollstein G, Schuman JS. OCT for glaucoma diagnosis, screening and detection of glaucoma<br />
progression. British Journal of Ophthalmology 2014;98 Suppl 2:ii15-19.<br />
4. Curcio CA, Allen KA. Topography of ganglion cells in human retina. Journal of Comparative Neurology<br />
1990;300:5-25.<br />
5. Hood DC, Raza AS, de Moraes CG, Liebmann JM, Ritch R. Glaucomatous damage of the macula. Prog<br />
Retin Eye Res 2013;32:1-21.<br />
6. Sung MS, Kang BW, Kim HG, Heo H, Park SW. Clinical validity of macular ganglion cell complex<br />
by spectral domain-optical coherence tomography in advanced glaucoma. Journal of Glaucoma<br />
2014;23:341-346.<br />
7. Petzold A, de Boer JF, Schippling S, et al. Optical coherence tomography in multiple sclerosis: a<br />
systematic review and meta-analysis. Lancet neurol 2010;9:921-932.<br />
8. Danesh-Meyer HV, Yap J, Frampton C, Savino PJ. Differentiation of Compressive from Glaucomatous<br />
Optic Neuropathy with Spectral-Domain Optical Coherence Tomography. Ophthalmology 2014; 121:<br />
1516-1523<br />
9. Hwang YH, Yoo C, Kim YY. Characteristics of peripapillary retinal nerve fiber layer thickness in eyes<br />
with myopic optic disc tilt and rotation. Journal of Glaucoma 2012;21:394-400.<br />
10. Chang RT, Singh K. Myopia and glaucoma: diagnostic and therapeutic challenges. Curr Opin<br />
Ophthalmol 2013;24:96-101.<br />
11. Hee MR, Izatt JA, Swanson EA, et al. Optical coherence tomography of the human retina. Arch<br />
Ophthalmol 1995;113:325-332.<br />
12. Serbecic N, Beutelspacher SC, Aboul-Enein FC, Kircher K, Reitner A, Schmidt-Erfurth U. Reproducibility<br />
of high-resolution optical coherence tomography measurements of the nerve fibre layer with<br />
the new Heidelberg Spectralis optical coherence tomography. British Journal of Ophthalmology<br />
2011;95:804-810.<br />
13. Cheung CYL, Yiu CKF, Weinreb RN, et al. Effects of scan circle displacement in optical coherence<br />
tomography retinal nerve fibre layer thickness measurement: a RNFL modelling study. Eye<br />
2009;23:1436-1441.<br />
14. Savini G, Zanini M, Barboni P. Influence of pupil size and cataract on retinal nerve fiber layer<br />
thickness measurements by Stratus OCT. Journal of Glaucoma 2006;15:336-340.<br />
15. Budenz DL, Anderson DR, Varma R, et al. Determinants of normal retinal nerve fiber layer thickness<br />
measured by Stratus OCT.[Erratum appears in Ophthalmology. 2008 Mar;115(3):472]. Ophthalmology<br />
2007;114:1046-1052.<br />
16. Menke MN, Knecht P, Sturm V, Dabov S, Funk J. Reproducibility of nerve fiber layer thickness<br />
measurements using 3D fourier-domain OCT. Invest Ophthalmol Vis Sci 2008;49:5386-5391.<br />
17. Sharma R, Sharma A, Arora T, et al. Application of anterior segment optical coherence tomography in<br />
glaucoma. Survey of Ophthalmology 2014;59:311-327.<br />
18. Smith SD, Singh K, Lin SC, et al. Evaluation of the anterior chamber angle in glaucoma: a report by<br />
the american academy of ophthalmology. Ophthalmology 2013;120:1985-1997.<br />
* Hannah Kersten is a therapeutically qualified optometrist with<br />
glaucoma prescriber accreditation. She has recently completed<br />
her doctoral studies in the Department of Ophthalmology<br />
at the University of Auckland, under the supervision of<br />
Professor Helen Danesh-Meyer, and Dr Richard Roxburgh of the<br />
Department of Neurology. The topic of her thesis was optical<br />
coherence tomography in neurodegenerative disease. Hannah<br />
is currently working as a post-doctoral research fellow in the<br />
Department of Ophthalmology and she is also involved in<br />
glaucoma co-management with Professor Danesh-Meyer at Eye<br />
Institute in Auckland.
Colour vision test ends<br />
Routine, school-based check-ups of 11 and<br />
12-year-old students will no longer include<br />
testing for colour vision deficiency as of July 1.<br />
The Ministry of Health announced it would<br />
eliminate the test in February to allow more time<br />
for technicians to identify hearing and vision<br />
problems among children at an earlier age when<br />
intervention makes a bigger difference.<br />
Colour blindness is relatively unusual, especially<br />
among girls. The condition is found in 0.5% of<br />
the female population, whereas colour vision<br />
deficiency affects about 10% of the 26,000 boys<br />
screened annually as part of the standard Year 7<br />
checks.<br />
The Ministry’s decision was influenced by a<br />
summer research project, which reviewed the<br />
medical literature on the efficacy of colour vision<br />
testing, and was overseen by ophthalmologist Dr<br />
Graham Wilson, in his role as clinical senior lecturer<br />
at the University of Otago, and his brother Nick<br />
Wilson, a professor at Otago’s Department of Public<br />
Health.<br />
“We found there was no evidence to support<br />
screening for colour blindness,” says Dr Wilson.<br />
“We screen for things like breast cancer and<br />
cervical cancer, things that can kill you, and colour<br />
blindness doesn’t rise to that level.”<br />
Ministry Chief Advisor, Child and Youth Health, Dr<br />
Pat Tuohy explained the policy change to medical<br />
technicians who conduct the school checks at a<br />
conference in late February.<br />
“They feel it will free up their time to do other<br />
things,” says Dr Wilson, who attended the conference.<br />
“I think people see the common sense in it.”<br />
Dr Wilson, his brother and Nishanthan<br />
Ramachandran, a health policy student, published<br />
their paper Is screening for congenital colour vision<br />
deficiency in school students worthwhile? A review<br />
in the November 2014 edition of Clinical and<br />
Experimental Optometry.<br />
The review analysed the literature on screening<br />
for congenital colour vision deficiency in school<br />
students, which predominantly uses the Ishihara<br />
test, and found no association between congenital<br />
colour vision deficiency and the level of educational<br />
achievement; only a rare association between the<br />
condition and other health and lifestyle impacts;<br />
and limited interventions.<br />
“Given this picture, the weight of evidence<br />
appears to be in favour of not adopting (or<br />
discontinuing) routine colour vision screening<br />
programmes for school students; however, it may<br />
be worthwhile for a career advisor to refer school<br />
students to an optometrist or ophthalmologist for<br />
colour vision screening, upon expression of interest<br />
in an occupation where normal colour vision is<br />
either particularly desirable or is a regulatory<br />
requirement,” concluded their paper. ▀<br />
Donations for ship-clinic<br />
The Tauranga Rotary club is raising<br />
funds and looking for equipment<br />
donations for a humanitarian group<br />
to bring an ophthalmic clinic to remote<br />
Pacific islands.<br />
The club has launched a campaign<br />
to raise $95,000 for Marine Reach, a<br />
humanitarian organisation that delivers<br />
health services to isolated populations<br />
from its vessel, the MV Pacific Hope. The<br />
total money raised—likely to include a<br />
matching grant from a Rotary international<br />
fund—will be used to purchase items on<br />
an ophthalmic clinic “wish list”, including<br />
a Sonamed Portable AB Scanner, Nidek<br />
hand held keratometer, a slit lamp, an instrument<br />
sterilising container, portable microscope and an<br />
operating bed.<br />
The plan is for the ship-board clinic to be<br />
dedicated and named The Rotary Foundation<br />
Ophthalmology Clinic, with contributors of<br />
over $500 recognised by inscription on a special<br />
plaque displayed in the Clinic. Other donors<br />
will be invited to sponsor a specific piece of<br />
equipment and have their name inscribed on an<br />
appropriate plaque fixed to the item. The club<br />
is also open to surplus equipment donations or<br />
discounted price offerings.<br />
Marine Reach purchased the Pacific Hope and<br />
refit the vessel in 2013. It undertook its first<br />
clinical voyage, with a dental and general medical<br />
outreach programme in Fiji and Vanuatu, from<br />
late June to early October 2015. The next voyage<br />
is likely to begin in June <strong>2016</strong>.<br />
Anyone interested in making a financial or<br />
equipment contribution should contact project<br />
coordinator David Garland on 07 543 2012. You<br />
can also make a direct financial contribution<br />
through Give a Little at https://givealittle.co.nz/<br />
org/tgarotary. For more information on Marine<br />
Reach, visit www.marinereach.com. ▀<br />
ZEISS launches<br />
DriveSafe<br />
Zeiss has launched new DriveSafe lenses to provide better vision<br />
in challenging driving conditions.<br />
Calling them “probably the most exciting safety feature in<br />
your car,” Zeiss says the new lenses are designed to maximise safety<br />
and comfort for spectacle wearers through a new premium coating<br />
and state-of-the art lens design.<br />
According to Zeiss’ research, 83% of drivers wear glasses and the<br />
majority (72%) of these prefer a single pair for everyday use that can<br />
also assist with the visual challenges of driving. Spectacle wearers<br />
report feeling discomfort when driving in rain (94%), at dusk (88%), at<br />
night (76%) and in fog (74%). While the majority of traffic accidents<br />
occur at dusk or after nightfall. “DriveSafe lenses address the major<br />
challenges facing spectacle wearers while driving in difficult light and<br />
weather conditions,” the company said.<br />
To better understand the requirements for dynamic vision while<br />
driving, ZEISS commissioned a study by the Research Institute of<br />
Automotive Engineering and Vehicle Engines in Stuttgart (FKFS) using<br />
a modified car on a real-world course. The setup included head and<br />
eye tracking systems to observe drivers’ visual behaviour.<br />
The study found that drivers focus on the road ahead and distant<br />
moving objects about 97% of the time, look at the dashboard 2% of<br />
the time and alternate viewing between the mirrors 1% of the time.<br />
Progressive lens wearers move their heads more than single vision<br />
wearers in order to avoid lens zones of incorrect power or that have<br />
high levels of aberration. FKFS also found that the closest object<br />
viewed on the dashboard is approximately 50-75 cm away from the<br />
driver’s eye, implying the near zone of a progressive lens, designed for<br />
a much closer distance, is virtually unused.<br />
“Drivers must contend with a rapidly alternating set of<br />
circumstances that require constant attention and dynamic vision.<br />
The DriveSafe lens is optimised to provide uncompromised distance<br />
vision, with a large intermediate zone that supports quick and<br />
comfortable focus when switching between the dashboard and<br />
mirrors.”<br />
The new lenses incorporate ZEISS DuraVision DriveSafe antireflective<br />
coating to mitigate the uncomfortable blue-light glare<br />
from Xenon/HID and LED headlights and Zeiss’ Luminance Design<br />
Technology that takes into account pupil size in different light<br />
conditions to assist drivers in detecting objects in conditions where<br />
they are more likely to feel stressed or insecure, such as twilight, rain<br />
or at night.<br />
European wearer trials revealed very high satisfaction levels for<br />
ZEISS DriveSafe lenses, the company reported, with 97% of test<br />
subjects satisfied with the new lenses when driving, including in<br />
challenging situations such as in the dark and twilight. Respondents<br />
reported good dynamic vision in near, intermediate and distant<br />
zones, good perception of colours and reduced dazzle/glare from<br />
headlights. In addition, 94% of respondents found the new lenses<br />
suitable for doing everyday tasks.<br />
“Drivers require the best technology for their vision needs today,”<br />
says Hilke Fitzsimons, managing director for ZEISS Australia and New<br />
Zealand. “Surveys show over two-thirds of adults have difficulty in<br />
driving in low light or adverse weather conditions. Our new DriveSafe<br />
lenses address problems of glare, depth perception, and vision acuity<br />
at all distances.”<br />
ZEISS DriveSafe will be available in New Zealand from <strong>Apr</strong>il 4<br />
in both progressive and single vision designs. The launch will be<br />
supported by an extensive digital promotion where consumers will<br />
be invited to become “test drivers” and win a pair of ZEISS DriveSafe<br />
Lenses at www.zeiss.com.au/DriveSafe. ▀<br />
Get to the main<br />
cause of dry,<br />
irritated eyes*<br />
Optrex ActiMist – clinically proven to work<br />
How does Optrex ActiMist work?<br />
Optrex ActiMist contains<br />
liposomes (tiny bubbles fi lled with<br />
moisture) that migrate across the<br />
surface of the eyelid and collect<br />
at the edges of the eye.<br />
Hygienic. Can be used<br />
by multiple people<br />
Lasts 6 months<br />
after opening<br />
These liposomes mix with natural<br />
lipids on the eyelid.<br />
Won’t smudge<br />
make-up<br />
ActiMist liposomes<br />
Convenient and<br />
portable<br />
4UP TO<br />
HOURS<br />
RELIEF 2<br />
CLINICALLY PROVEN<br />
Natural lipids<br />
ActiMist liposomes<br />
When the eyes are open the new<br />
lipid mixture spreads over the<br />
whole tear fi lm, and helps fi ll the<br />
gaps to restore the damaged<br />
lipid layer.<br />
Suitable for use<br />
with contact lenses<br />
Order stock for your practice today<br />
FREE CALL 0800 393 564 EYELOGIC<br />
www.optrex.co.nz optrex@eyelogic.com.au<br />
Always read the label. Use only as directed. If symptoms persist, see your healthcare professional. †When wearing make-up, it is recommended to apply from 20cm. *Due to disturbed lipid layer of the tear fi lm. References:<br />
1. Lee S et al. Klin Monatsbl Augenheilkd 2004; 221:1–12. 2. Khaireddin R, Schmidt KG. Klin Monatsbl Augenheilkd. 2010; 227: 128-134. 3. Pult H et al. Contact Lens Anterior Eye 2012, 35:203-207. Reckitt Benckiser, Auckland. TAPS DA1541<br />
<strong>Apr</strong>il <strong>2016</strong><br />
NEW ZEALAND OPTICS<br />
13
Great<br />
Memories<br />
In recent times, I’ve been writing a five<br />
thousand-word article on the history and<br />
evolution of soft lenses. In doing so, I asked<br />
my long term friend, mentor and fellow South<br />
African Des Fonn if he would like to share<br />
some of his thoughts on this subject.<br />
Des was my final year lecturer in contact<br />
lenses, after his return from spending eighteen<br />
months doing his MOptom with Brien Holden<br />
and the gang at the CCLRU in Sydney in 1980.<br />
We did some research together and served on<br />
the South African Contact Lens Society council<br />
and arranged many conferences together. He<br />
was one of the people who motivated me to<br />
excel in contact lenses and inspired me in many<br />
ways. I have mentioned Professor Desmond<br />
Fonn in numerous missives in this column over<br />
the years so won’t repeat it here but this link<br />
will give you some of that. Des is the founder<br />
of the prestigious CCLR at Waterloo, one of the<br />
top CL research facilities in the world and has<br />
published widely.<br />
Des had the following to share.<br />
The 1980s: game<br />
changing events in<br />
which Australia led<br />
the way<br />
1976 was a momentous year for the University<br />
of New South Wales School of Optometry as<br />
the Cornea and Contact Lens Research Unit was<br />
established under the leadership of Brien Holden.<br />
It was this organisation that would lead the<br />
world in cornea and contact lens research and<br />
was the forerunner of all the organisations to<br />
follow culminating in 2010 as the Brien Holden<br />
Vision Institute in recognition for his lifetime of<br />
work in research and humanitarian initiatives<br />
related to vision.<br />
During the mid 70s the popularity of soft lenses<br />
gained momentum to equal that of rigid lenses<br />
but it was soon demonstrated that daily wear of<br />
soft lenses produced clinically significant corneal<br />
edema. During this period, John De Carle had<br />
developed the high-water-content Permalens<br />
and claimed successful extended wear without<br />
ocular complications. These two topics became<br />
the cornerstones of research at the CCLRU. Drs<br />
Steve Zantos and Lewis Williams were Brien’s<br />
first two PhD students working on extended<br />
wear of soft lenses and the effects of soft lenses<br />
and hypoxia on the corneal endothelium. Brien’s<br />
paper in the Australian Journal of Optometry in<br />
1975 on the principles and practice of correcting<br />
astigmatism with soft lenses peaked my interest<br />
at that time, and thousands of others because<br />
he showed that 35% of patients require toric<br />
lenses. This figure was corroborated by others<br />
years later. It was not a coincidence that Brien<br />
and colleagues at the Institute for Eye Research,<br />
which superseded the CCLRU in the late eighties,<br />
developed a unique toric lens design that yielded<br />
millions of royalty dollars.<br />
By 1980 the CCLRU comprised about 30 people<br />
dedicated to research on contact lenses and<br />
their effects on the eye. Brien’s vision in those<br />
early years was that Australian and international<br />
collaboration were essential to understand the<br />
effects of contact lenses and this became the<br />
cornerstone of their research endeavors.<br />
The image below is a collage of colleagues<br />
working at the CCLRU in 1980. Brien used<br />
the image in his presentations to describe a<br />
renaissance that began in 1980. Of course there<br />
were many others at the time and hundreds that<br />
followed in a similar vein to work at the world’s<br />
most exciting institution in the contact lens field.<br />
During the late seventies Dr George Mertz<br />
published two important papers on corneal<br />
swelling. In his 1978 paper he showed that<br />
an ultra-thin low water HEMA lens decreased<br />
corneal swelling compared to a standard<br />
thickness lens suggesting that decreasing<br />
hypoxia led to decreased corneal swelling. His<br />
1980 paper was also on the subject of hypoxia<br />
in which he found that the overnight closed eye<br />
(without a lens) produced significant corneal<br />
swelling. These papers were part of the stimulus<br />
for further study in an attempt to determine<br />
what the critical oxygen transmission of a<br />
DO takes on the Sky Tower<br />
hydrogel lens should be to avoid corneal swelling.<br />
Holden, Mertz and McNally published a series<br />
of papers on hypoxia that started in the early<br />
eighties, the most renowned of which is the<br />
“Critical oxygen levels to avoid corneal edema<br />
for daily and extended wear contact lenses”.<br />
Their conclusion from this study was that 87 x<br />
10-9 oxygen transmissibility (Dk/t) was required<br />
for overnight wear and 24 x 10-9 for daily wear.<br />
The limitation of this work was that only one<br />
high Dk lens (silicone elastomer) and an ultra<br />
thin low water content hydrogel lens (20μm)<br />
was included in the study. This is the second<br />
most cited paper in the contact lens field aside<br />
from those on corneal infection. Since then<br />
the EW value has been revised to 150 – 190<br />
Dk/t to avoid corneal edema as a result of the<br />
availability of silicone hydrogel lenses that we<br />
used in overnight corneal swelling studies.<br />
Brien’s highest cited paper was known as the<br />
Gothenburg study. This study examined the longterm<br />
effects of extended contact lens wear and<br />
the conclusion was that adverse reactions could<br />
be avoided by fitting lenses that have higher<br />
oxygen transmissibility, looser fitting, lenses<br />
should be removed from the eye more frequently<br />
and lenses should be more regularly replaced.<br />
These studies on hypoxia and others on<br />
extended wear were unquestionably the<br />
stimulus to develop a highly oxygen permeable<br />
soft lens. The collaboration between the<br />
Cooperative Research Centre for Eye Research and<br />
Technology at UNSW with an industry partner<br />
developed the first silicone hydrogel contact lens,<br />
which was the game changer for the contact lens<br />
industry by eliminating virtually all the problems<br />
of hypoxia. These materials now constitute<br />
approximately 60% of all contact lenses worn.<br />
The hope was the same for microbial keratitis<br />
(MK) but research with silicone hydrogels has<br />
shown that elimination of hypoxia has not<br />
decreased the incidence of MK nor inflammatory<br />
complications.<br />
How amazingly fortunate I was to meet and<br />
befriend Brien and then work with those people<br />
featured in the photograph. Thirty-five glorious<br />
years of contact lens research that started in<br />
1980 at the CCLRU and was the springboard for<br />
industry/institution collaboration unmatched by<br />
any others.<br />
For more go to www.brienholdenvision.org<br />
Thanks Des for sharing your insights. Next time<br />
we see each other dinner and a few beers are<br />
on me. It’s great to see that our recollections of<br />
such things are more or less on the same page<br />
so it seems our grey matter is still having good<br />
recall of events! ▀<br />
ODMA<br />
appoints<br />
IEC<br />
The Board of the Optical Distributors &<br />
Manufacturers Association (ODMA) has<br />
appointed International Exhibition and<br />
Conference Group (IEC) to organise ODMA2017,<br />
to be held July 7 to 9 at Sydney’s International<br />
Convention Centre.<br />
“The company was selected from a very capable<br />
list due to their key personnel’s history of working<br />
with associations, their commitment to excellence<br />
and their enthusiastic and creative approach,” said<br />
Finola Carey, ODMA’s chief executive, in a statement.<br />
‘’I am confident that IEC is best-placed to closely<br />
work with ODMA to deliver the event to suit the<br />
changing needs of our members and the broader<br />
industry in general.”<br />
IEC has managed a number of major industry<br />
events, including Fashion Exposed and Furnitex,<br />
under the leadership of its CEO Marie Kinsella.<br />
“I have always admired the ODMA fair over<br />
many years for its high quality presentation and<br />
its professional approach,” said Kinsella. “We look<br />
forward to working closely with ODMA and its<br />
members to deliver outstanding results.”<br />
ODMA has frozen floor space rates at 2015<br />
levels and will include new interactive features,<br />
networking events and educational content. ▀<br />
Glaucoma NZ<br />
book fundraiser<br />
Glaucoma NZ is selling Entertainment Books,<br />
with a portion of the proceeds going<br />
towards vital funds for the charity. A digital<br />
membership is also on offer, which allows you to<br />
redeem offers from your smartphone.<br />
Entertainment Books contain hundreds of<br />
25-50% off and two-for-one offers from popular<br />
restaurants, cinemas, hotel accommodation, the<br />
arts, lifestyle and sporting events. All offers are<br />
valid until June <strong>2016</strong> to give buyers plenty of time<br />
to get their money’s worth!<br />
Books are priced at $65 for Auckland (including<br />
Whangarei and Bay of Islands), Christchurch,<br />
Canterbury and Nelson; and $60 for Waikato & Bay<br />
of Plenty, Wellington (includes Palmerston North),<br />
Dunedin, Invercargill and Queenstown.<br />
Visit https://www.entertainmentbook.co.nz/<br />
orderbooks/102253y to buy.<br />
March 6 to 12 was World Glaucoma Week, an<br />
international campaign to help raise awareness<br />
of the disease that can go undetected for years<br />
and eventually lead to blindness. A number<br />
of countries took part with events aimed at<br />
educating the public and getting people tested. ▀<br />
Optical history made at Tattoo<br />
Maria Paterson training for the Sky Tower<br />
Maria Paterson, dispensing technician<br />
with Frederick Swain Optometrists in<br />
Hawke’s Bay is going to race up the Sky<br />
Tower in her full firefighting kit to raise funds and<br />
awareness for Leukaemia & Blood Cancer NZ as<br />
part of the annual Firefighter Sky Tower Challenge.<br />
Paterson has been a volunteer firefighter for<br />
seven years with the Napier Fire Station and says<br />
she loves helping people and a challenge. She also<br />
lost her mother and brother to cancer so is<br />
proud to be able to support Leukaemia & Blood<br />
Cancer NZ.<br />
Now in its eleventh year, the Firefighter Sky<br />
Tower Challenge has grown to include more than<br />
750 firefighters, climbing 51 flights – or 1,103<br />
Sky Tower steps – wearing full kit weighing 25kg.<br />
In 2015 the event raised nearly $1.04 million, its<br />
highest fundraising total to date.<br />
Paterson says she’s had “awesome support” from<br />
her colleagues at Frederick Swain, some of whom<br />
have even been out and about with her climbing<br />
every set of steps they can find in Napier. She’s<br />
even joined a gym, she laughs.<br />
The Firefighter Sky Tower Stair Challenge takes<br />
place on Saturday May 28.<br />
To support Paterson go to http://<br />
firefightersclimb.org.nz/Donate.html and type in<br />
“Maria”. ▀<br />
Dr Simon Dean and sons Lachlan and Cameron perform at the Tattoo<br />
A<br />
little bit of optical history was made at<br />
the end of February, when Eye Institute<br />
ophthalmologist Dr Simon Dean and his sons<br />
Cameron (12) and Lachlan (10) performed with the<br />
Royal Edinburgh Military Tattoo in Wellington.<br />
Cameron on pipes and Lachlan on snare drum were<br />
the youngest performers in the 1200-strong cast,<br />
playing in the City of Auckland Pipe Band along<br />
with their father (also on snare drum).<br />
Known as the<br />
“greatest show on<br />
earth,” the Tattoo<br />
is always a sell-out<br />
in Edinburgh and it<br />
was no different in<br />
Wellington, with more<br />
than 82,000 tickets<br />
sold across four soldout<br />
performances,<br />
making it Wellington’s<br />
most popular show<br />
ever.<br />
Dr Dean said it was a<br />
lot of hard work, with<br />
their days starting at<br />
6 am and finishing at<br />
11 pm most nights for<br />
a week. But he and his<br />
wife, Associate Professor Jennifer Craig, a Scot by<br />
birth, says they couldn’t have been prouder of their<br />
sons or have enjoyed an event more.<br />
“For one of the performances, Jennifer’s parents,<br />
my parents, so all the boys’ grandparents, and Jen<br />
watched. A proud moment for all generations of<br />
our family…and a great experience and honour to<br />
be involved; only made better by having my boys<br />
playing in the band as well,” said Dr Dean. ▀<br />
14 NEW ZEALAND OPTICS <strong>Apr</strong>il <strong>2016</strong>
Summer Student Symposium <strong>2016</strong><br />
A<br />
diversity of research, from the development<br />
of aids for colour deficient optometrists<br />
to optimising a test to assess vision in<br />
Zebrafish, was presented by 11 students from the<br />
Department of Ophthalmology and the School of<br />
Optometry and Vision Science (SOVS) at the annual<br />
Summer Student Symposium hosted by the New<br />
Zealand National Eye Centre (NEC).<br />
Professor Louise Nicholson and Associate Professor<br />
Mark Barrow, associate dean (academic) for the<br />
Faculty of Medical and Health Sciences, were invited<br />
to judge the presentations made by the students<br />
who had been working on their research projects for<br />
five to 10 weeks over the summer.<br />
The symposium presentations, given in a four<br />
minute “rapid fire” format, were well attended by<br />
senior academic staff, students and funders of the<br />
summer studentship programme.<br />
Symposium moderator Associate Professor Trevor<br />
Sherwin explained that for several students their<br />
summer projects had been their first real exposure<br />
to complex research and the symposium was an<br />
opportunity for them to present their findings to<br />
the wider ophthalmic community.<br />
First prize–Jonathan Young<br />
First prize was awarded to fifth-year BOptom<br />
student Jonathan Young who was supervised by<br />
Dr Misha Vorobyev from SOVS. He was the second<br />
presenter on the project Development of aids<br />
for colour deficient optometrists, the first being<br />
John Kwak who explained the development of the<br />
software for the project, while Young presented the<br />
results and conclusions.<br />
The prevalence of inherited red-green colour<br />
deficiency is quite high among the male<br />
population (8%) so colour deficiency among<br />
medical practitioners can pose a substantial<br />
hazard to society. One of the diagnostic problems<br />
that colour deficient optometrists confront<br />
is a difficulty in differentiating pigment from<br />
haemorrhage on a fundus image, said Young. “We<br />
transformed colours in fundus images to improve<br />
the discrimination and reduce ambiguity for the<br />
colour deficient optometrists when making a<br />
diagnosis. Each colour deficient participant’s range<br />
of colour vision was modelled and a personalised<br />
image transformation algorithm was developed.<br />
We tested our participants by showing them<br />
images of either sub-retinal pigments or subretinal<br />
haemorrhages, and prompted them to<br />
make a diagnosis.”<br />
Using colour deficient optometry students<br />
for the research, it was demonstrated that<br />
image transformation improved their ability to<br />
differentiate between pigment and haemorrhage<br />
in fundus images. This was the first study of its<br />
kind to look at colour deficiency in an optometric<br />
clinical setting and was funded by the SOVS.<br />
Second prize–Nikita Govender<br />
Nikita Govender, a fourth-year BOptom student,<br />
was awarded second prize for her presentation<br />
on the Role of the retina in atropine control of eye<br />
MORE CLASSIFIEDS ON PAGE 16<br />
elongation.<br />
Supervised by Dr Monica Acosta from SOVS<br />
and sponsored by SOVS, this project looked at<br />
myopia control from a different perspective. The<br />
aim was to investigate the role of the retina in<br />
atropine control of myopia by examining the effect<br />
of atropine on retinal neurotransmitter levels.<br />
The experiment involved in vitro incubation of<br />
normal and myopic chick eyes with or without<br />
atropine. Tissues were sectioned and stained with<br />
a silver intensified immuno-gold technique to<br />
label key neurotransmitters. Results showed no<br />
significant change in neurotransmitter levels with<br />
atropine, however, from the images it was evident<br />
that atropine triggered redistribution of the<br />
neurotransmitters particularly in the inner retina.<br />
The hypothesis is these effects are mediated by<br />
cholinergic amacrine cells. Neurotransmitter<br />
redistribution may correspond to a change in the<br />
functioning of the retina and perhaps an altered<br />
visual experience. The next step would be to<br />
study the in vivo effects of atropine on the retina<br />
to better understand the mechanisms of myopia<br />
control, said Govender.<br />
Third prize–Samuel Lie<br />
The third prize was awarded to second-year medical<br />
student Samuel Lie. His research, Conducting<br />
polymers as release rate controlling membranes<br />
for electrical stimuli-responsive drug delivery,<br />
was funded by the Faculty of Medical and Health<br />
Sciences and supervised by Naveed Yasin, Dr Darren<br />
Svirskis and Dr Ilva Rupenthal.<br />
Sustained release ocular drug delivery systems<br />
have gained popularity when selecting treatment<br />
methods for diseases that affect the posterior<br />
segment of the eye. There are already a number<br />
of implants on the market, but they release<br />
drugs at a fixed rate, not allowing for adjustment<br />
as required by each individual patient. In this<br />
study, the focus was on the potential of poly(3,4-<br />
ethylenedioxythiophene) (PEDOT) to be used as<br />
a membrane to control drug release rates within<br />
an ocular drug implant where tuned drug delivery<br />
can be achieved via application of electrical<br />
stimuli. Dexamethasone release through PEDOT<br />
membranes was studied using Franz diffusion cells<br />
comparing release with and without application<br />
of electrical stimulus. By comparing PEDOT coated<br />
membranes to plain cellulose membranes it was<br />
found that PEDOT can be effective in limiting drug<br />
release. Further research is required in order to fine<br />
tune the control of release to ultimately fabricate a<br />
PEDOT based ocular implant.<br />
The public’s understanding of optometry<br />
An interesting presentation was made by<br />
Janice Chung whose study was funded by the<br />
New Zealand Association of Optometrists. It was<br />
conducted at the Acute Eye Clinic, Greenlane<br />
Clinical Centre, where 311 patients completed an<br />
anonymous questionnaire. The results show the<br />
basic scope of optometry, such as prescription of<br />
corrective wear and examination of eye health,<br />
Presenters (back row) Benjamin Wright, Jaspreet Singh,<br />
Kenny Wu, Samuel Lie, Rahul Makam and Jonathan<br />
Young, (front row) Janet Chung, Nikita Govender, Eileen<br />
Song, Ye Li, John Kwak and event MC Associate Professor<br />
Trevor Sherwin<br />
The winners with the judges: Nikita Govender, A/Prof<br />
Mark Barrow, Jonathan Young, John Kwak, Prof. Louise<br />
Nicholson and Samuel Lie<br />
Fraser Alexander, Dr Monica Acosta, Shadi Jolzar and Dr<br />
Ehsan Vaghefi<br />
is well understood by the public. However, this<br />
was not the case with regards to therapeutic<br />
management and treatment of ocular disease.<br />
The majority of patient referrals were from GPs,<br />
with some being uncertain of an optometrist’s<br />
capabilities – including the ability to refer,<br />
diagnose and treat eye conditions. These findings<br />
suggest there is room for further public education<br />
by key stakeholders. This research was supervised<br />
by Robert Ng, Tina Gao and Richard Johnson. ▀<br />
NZOSS<br />
objectives for<br />
the year ahead<br />
BY NIKKU SINGH, NZOSS PRESIDENT<br />
Most of the new NZOSS excecutive, (L to R) Kendall<br />
Johnston, Oliver Munro, Jonathan Albert, Nikku Singh,<br />
Sophie Woodburn, Aaron Chin, Gunnika Gill and Alicia Han<br />
Since it was established in 2013, the New<br />
Zealand Optometry Student Society<br />
(NZOSS) has strived to provide a platform<br />
for all students to engage with the professional<br />
community. Although NZOSS has only been<br />
operating for the last few years it has rapidly<br />
built up steam, with the student committee<br />
working hard with the New Zealand eye care<br />
industry to foster a great relationship among<br />
present and future optometrists.<br />
Each year a new bunch of students are elected<br />
to form the NZOSS executive committee and it<br />
is my pleasure to introduce the team for <strong>2016</strong>:<br />
grassroots representative Kendall Johnston;<br />
sports representative Jonathan Albert; vicepresident<br />
Sophie Woodburn; treasurer Aaron<br />
Chin; public relations Gunnika Gill; secretary<br />
Alicia Han; and general members Oliver Munro<br />
and Xheida Mani.<br />
This year, our main objectives are not only to<br />
promote long-lasting relationships among all<br />
optometry students, but to further develop our<br />
strong connections with the eye care industry.<br />
Through the organisation of seminars and<br />
networking events, students will be able to<br />
gain valuable knowledge on the vast number of<br />
specialties and avenues involving optometry and<br />
visual science. We will also facilitate some much<br />
required down time through social events, such<br />
as the Optometry Pub Quiz, pub crawls, the Eye<br />
Ball and much, much more.<br />
<strong>2016</strong> is shaping up to be a great year and we<br />
look forward to all that comes our way! ▀<br />
PROBABLY THE MOST<br />
EXCITING SAFETY<br />
FEATURE IN YOUR CAR.<br />
ZEISS DriveSafe Lenses<br />
FULL-TIME OPTOMETRIST<br />
WITH PARTNERSHIP OPPORTUNITY AT<br />
LEADING DUNEDIN INDEPENDENT<br />
Stewart Caithness Gray Optometrists is a well<br />
established independent practice in the city of<br />
Dunedin with branches in Mosgiel and Gore.<br />
We provide a high level of professional care and<br />
service to our patients and are looking for an<br />
experienced optometrist to join our team. The<br />
position is full time with potential partnership<br />
opportunities for the successful applicant.<br />
We have a wide range of patients of all<br />
ages and therefore, communication and<br />
interpersonal skills must be excellent. You need<br />
to have a passion for independent optometry<br />
and an interest in fitting speciality contact<br />
lenses. You should be TPA endorsed and ideally<br />
have at least 2-4 years experience. Salary will<br />
be reflective on your experience.<br />
We have a fantastic support team and<br />
diagnostic equipment includes OCT, corneal<br />
topographer, fundus and slit-lamp cameras and<br />
both Matrix and Medmont VFA’s.<br />
We pride ourselves in providing excellence in<br />
eye care, eyewear and service and are excited<br />
to be able to offer this opportunity to join our<br />
great team.<br />
Please email Brian Stewart, brian@scgeyes.nz,<br />
for further details.<br />
LOOKING FOR A PRIME<br />
OPTOMETRIST!<br />
Great opportunity for a full-time optometrist<br />
in an independent, family-owned business<br />
in New Plymouth. Known for their superb<br />
service and extremely helpful team (yes, they<br />
have won awards for it!) they really want<br />
someone who “gets their vision”.<br />
They have all the latest technology, including<br />
a Zeiss OCT/Camera and very well equipped<br />
exam room and are led by an extremely<br />
experienced Dispensing Optician.<br />
What’s unique about this practice is the loyal<br />
customer base and the amount of referrals<br />
they get. This is not a High Street “look at me”<br />
business. They really do like their customers<br />
and go out of their way to help.<br />
The good news about this role is it’s not<br />
an immediate start and no late nights or<br />
weekends. They are searching far and wide<br />
for the right person to come and join them<br />
in June of this year. So, if you are thinking<br />
of moving to “the best place to live” in<br />
New Zealand then now’s the time to start<br />
planning.<br />
Salary is in line-of-sight of market rates. For<br />
details and to arrange an interview contact<br />
fitzroyoptom@xtra.co.nz or phone Michael at<br />
027 758 4974.<br />
zeiss.com.au/DriveSafe<br />
An everyday lens for safer and more relaxed driving – even in difficult low-light conditions.<br />
• Better vision in difficult low-light conditions thanks to Luminance Design ® Technology<br />
• Glare reduction at night from oncoming cars or street lights 1<br />
• Accurate vision of the road, dashboard, rear-view mirror and side mirrors<br />
Find out more today at zeiss.com.au/DriveSafe<br />
1 Perceived glare compared to premium ZEISS coatings.<br />
<strong>Apr</strong>il <strong>2016</strong><br />
NEW ZEALAND OPTICS<br />
15
MORE CLASSIFIEDS INSIDE<br />
ON pAgE 15<br />
Need a locum?<br />
Call Bharat Raniga, locum optometrist, on<br />
021 424 253 or email: bharatraniga@yahoo.com<br />
prActicE for sAlE<br />
Get double-digit earnings without the sweat and toil of a CBD<br />
location. Enjoy the superior work-life balance of the countryside,<br />
while still within an easy drive of civilisation in downtown<br />
Auckland. Ideally suited to an optometrist breaking out on their<br />
own, or breaking back into the business after maternity leave or<br />
OE, or a dispenser-optometrist team. Yes, double-digit earnings,<br />
and potential for even more growth. If this sounds like something<br />
you’d like to pursue, please apply in strictest confidence c/- NZ<br />
Optics, info@nzoptics.co.nz Code PFSS1.<br />
SPECIALIST SHOPFITTERS & dESIgnERS TO THE OPTOMETRIC PROFESSIOn<br />
TEL:(09) 486-2070 MOB:(0274) 798-798<br />
Email: tony.maddocks@xtra.co.nz<br />
EquipmEnt And shop fittings<br />
for sAlE<br />
Six wall-mounted frame dispaly units with 10 glass shelves per<br />
unit, 1 x light box (1.2x2m), finished in white two-pot lacquer,<br />
Zeiss Visucam Pro Retinal Camera, Humphrey Matrix perimeter,<br />
Reichart refractor head, Topcon IS-80 Chair and Stand, Topcon<br />
SL3F slit lamp, Topcon OM-4 Keratometer, Nidek CR690 Projector<br />
Chart (with screen and mirror), Kowa HA2 Tonometer with<br />
LED Bulb, LED Confrontation wand, Trial Lens kit, Nidek OL-7<br />
vertometer ,GFC Frame heater, Stenersen Multi-frame gauge,<br />
Pupilometer. All offers considered. Contact<br />
michael@eyestyle.co.nz.<br />
EquipmEnt for sAlE<br />
Topcon IS700 Chair and Stand, Magnon SL350 Slit Lamp, Reichart<br />
Keratometer, Righton NP36 Projector. All in good condition.<br />
Contact c/- info@nzoptics.co.nz, Code: EQFS12<br />
for sAlE<br />
Beautiful brushed aluminium frame display, holds 312 frames.<br />
Plus lockable frame or sunglass display racks, holds 96 sunglasses/<br />
frames. Also Gatehouse internally illuminated Eye Chart. Perfect<br />
for practices wanting to upgrade their frames displays or a newly<br />
opening practice. Contact Mark at 027 3806171<br />
or focusoptom@clear.net.nz.<br />
dispEnsing opticiAn/opticAl<br />
AssistAnt<br />
Paterson Burn Optometrists is one of the largest independent<br />
optometry practice groups in New Zealand. We are totally<br />
independent and Waikato owned and we’ve maintained our<br />
independence in the ever changing environment of New Zealand<br />
optometry. Our core purpose is to improve people’s lives by<br />
providing the best visual solutions available.<br />
Paterson Burn Optometrists value respect, integrity,<br />
accountability, enjoyment, continuous improvement, freedom for<br />
initiative and teamwork.<br />
Paterson Burn Optometrists Cambridge requires an experienced,<br />
confident and enthusiastic Dispensing Optician / Optical<br />
Assistant to join our small, friendly team.<br />
The successful applicant will:<br />
• Be a qualified Dispensing Optician or Optical Assistant with a<br />
minimum of 4 years’ dispensing experience<br />
• Display exceptional customer service and sales skills<br />
• Be committed to providing excellent patient care<br />
• Be well presented with an eye for fashion<br />
• Be a self-starter who can work with minimal supervision<br />
• Be versatile, reliable and motivated.<br />
The successful applicant must be available to work full time and<br />
some Saturdays.<br />
Please email your CV and a cover letter to<br />
sandri@patersonburn.co.nz<br />
16 <strong>Apr</strong>il <strong>2016</strong><br />
NEW ZEALAND OPTICS <strong>Apr</strong>il <strong>2016</strong> classified NEW ZEALAND 1