08 Assessment of volume status and fluid responsiveness in the emergency department
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Übersichten<br />
Med Kl<strong>in</strong> Intensivmed Notfmed 2017 · 112:326–333<br />
DOI 10.1007/s00063-015-0124-x<br />
Received: 25 August 2015<br />
Revised: 13 October 2015<br />
Accepted: 29 October 2015<br />
Published onl<strong>in</strong>e: 16 December 2015<br />
© Spr<strong>in</strong>ger-Verlag Berl<strong>in</strong> Heidelberg 2015<br />
Redaktion<br />
M. Buerke, Siegen<br />
C. Maurer 1 · J.Y. Wagner 2 · R.M. Schmid 1 · B. Saugel 2<br />
1<br />
II. Mediz<strong>in</strong>ische Kl<strong>in</strong>ik und Polikl<strong>in</strong>ik, Kl<strong>in</strong>ikum rechts der Isar der<br />
Technischen Universität München, München, Germany<br />
2<br />
Department <strong>of</strong> Anes<strong>the</strong>siology, Center <strong>of</strong> Anes<strong>the</strong>siology <strong>and</strong> Intensive Care Medic<strong>in</strong>e,<br />
University Medical Center Hamburg-Eppendorf, Hamburg, Germany<br />
<strong>Assessment</strong> <strong>of</strong> <strong>volume</strong> <strong>status</strong><br />
<strong>and</strong> <strong>fluid</strong> <strong>responsiveness</strong> <strong>in</strong><br />
<strong>the</strong> <strong>emergency</strong> <strong>department</strong>:<br />
a systematic approach<br />
Introduction<br />
Fluid <strong>the</strong>rapy is a crucial <strong>the</strong>rapeutic <strong>in</strong>tervention<br />
<strong>in</strong> <strong>the</strong> treatment <strong>of</strong> acutely ill<br />
patients admitted to <strong>the</strong> <strong>emergency</strong> <strong>department</strong><br />
(ED). In ED patients with conditions<br />
such as sepsis, acute kidney <strong>in</strong>jury,<br />
pancreatitis or trauma, early <strong>fluid</strong> resuscitation<br />
constitutes one <strong>of</strong> <strong>the</strong> most potent<br />
<strong>and</strong> important <strong>the</strong>rapeutic <strong>in</strong>terventions<br />
<strong>and</strong> a delay <strong>in</strong> its implementation may<br />
contribute to an <strong>in</strong>crease <strong>in</strong> mortality [1–<br />
3]. However, after <strong>the</strong> <strong>in</strong>itial resuscitation<br />
period, cont<strong>in</strong>ued aggressive hydration<br />
may cause <strong>in</strong>terstitial edema which is associated<br />
with a worse outcome. Therefore,<br />
<strong>fluid</strong> <strong>the</strong>rapy needs to be performed based<br />
on <strong>the</strong> patient’s <strong>volume</strong> <strong>status</strong> <strong>and</strong> <strong>fluid</strong> <strong>responsiveness</strong>.<br />
Although we can apply advanced<br />
<strong>in</strong>vasive hemodynamic monitor<strong>in</strong>g<br />
<strong>in</strong> <strong>in</strong>tensive care medic<strong>in</strong>e, cl<strong>in</strong>ical,<br />
laboratory, <strong>and</strong> static hemodynamic parameters<br />
rema<strong>in</strong> <strong>the</strong> key <strong>in</strong>struments <strong>in</strong><br />
an ED sett<strong>in</strong>g to guide <strong>the</strong>rapy dur<strong>in</strong>g <strong>the</strong><br />
early period <strong>of</strong> critical disease. In this review<br />
we want to outl<strong>in</strong>e established <strong>and</strong><br />
promis<strong>in</strong>g means for <strong>the</strong> assessment <strong>of</strong> a<br />
patient’s <strong>volume</strong> <strong>status</strong> <strong>and</strong> <strong>fluid</strong> <strong>responsiveness</strong><br />
<strong>in</strong> <strong>the</strong> ED.<br />
In a cl<strong>in</strong>ical context, <strong>the</strong> term “dehydration”<br />
is <strong>of</strong>ten used synonymously for<br />
<strong>the</strong> follow<strong>in</strong>g two conditions: (a) hypertonicity,<br />
that is, <strong>in</strong>tracellular water deficits<br />
result<strong>in</strong>g from hypertonicity <strong>and</strong> a disturbance<br />
<strong>in</strong> water metabolism <strong>and</strong> (b) deficit<br />
<strong>in</strong> extracellular <strong>fluid</strong> <strong>volume</strong>, that is, a<br />
net loss <strong>of</strong> total body sodium <strong>and</strong> a reduction<br />
<strong>in</strong> <strong>in</strong>travascular <strong>volume</strong> [4]. Basically,<br />
although both dehydrated <strong>and</strong> <strong>volume</strong><br />
depleted patients may present with similar<br />
symptoms <strong>and</strong> signs <strong>in</strong> physical exam<strong>in</strong>ation,<br />
<strong>the</strong> underly<strong>in</strong>g pathophysiology <strong>of</strong><br />
dehydration <strong>and</strong> <strong>volume</strong> depletion is different<br />
<strong>and</strong> may require different treatment<br />
strategies [4].<br />
Physical exam<strong>in</strong>ation<br />
Physical exam<strong>in</strong>ation rema<strong>in</strong>s <strong>the</strong> foundation<br />
<strong>of</strong> every patient encounter <strong>and</strong> may<br />
contribute valuable <strong>in</strong>formation to <strong>volume</strong><br />
<strong>status</strong> assessment. Initially, identify<strong>in</strong>g<br />
patients with circulatory shock rema<strong>in</strong>s<br />
<strong>the</strong> most important task dur<strong>in</strong>g triage<br />
<strong>in</strong> <strong>the</strong> ED [5]. Besides arterial hypotension,<br />
evaluat<strong>in</strong>g <strong>the</strong> three “w<strong>in</strong>dows<br />
<strong>of</strong> <strong>the</strong> body” [6] may yield clues to ongo<strong>in</strong>g<br />
tissue hypoperfusion: (a) <strong>the</strong> presence<br />
<strong>of</strong> mottled <strong>and</strong> clammy sk<strong>in</strong>, (b) oliguria<br />
(< 0.5 mL ur<strong>in</strong>e output per kg body<br />
weight per hour), <strong>and</strong> (c) an altered mental<br />
state (e.g., confusion). In <strong>the</strong> absence<br />
<strong>of</strong> <strong>the</strong> f<strong>in</strong>d<strong>in</strong>gs above, physical exam<strong>in</strong>ation<br />
should proceed with <strong>the</strong> assessment<br />
<strong>of</strong> a comb<strong>in</strong>ation <strong>of</strong> cl<strong>in</strong>ical <strong>in</strong>dicators [7,<br />
8]. Signs <strong>and</strong> symptoms that might <strong>in</strong>dicate<br />
hypovolemia are dry membranes <strong>of</strong><br />
mouth <strong>and</strong> nose, dry tongue, longitud<strong>in</strong>al<br />
furrows on tongue, decreased sk<strong>in</strong> turgor,<br />
dry axilla, sunken eyes, reduced production<br />
<strong>of</strong> saliva, confusion, <strong>and</strong> weakness.<br />
Orthostatic (postural) changes <strong>in</strong> heart<br />
rate <strong>and</strong> blood pressure are <strong>of</strong>ten <strong>in</strong>terpreted<br />
as <strong>in</strong>dicators <strong>of</strong> <strong>in</strong>travascular <strong>volume</strong><br />
<strong>status</strong> <strong>in</strong> <strong>the</strong> <strong>emergency</strong> sett<strong>in</strong>g [9].<br />
However, even <strong>the</strong> detection <strong>of</strong> moderate<br />
to large amounts <strong>of</strong> blood loss based on<br />
physical exam<strong>in</strong>ation has been demonstrated<br />
to be a challenge [10].<br />
The accuracy <strong>of</strong> cl<strong>in</strong>ical signs <strong>and</strong><br />
symptoms <strong>of</strong> hypervolemia has mostly<br />
been studied <strong>in</strong> patients with congestive<br />
heart failure [11, 12]. Symptoms that po<strong>in</strong>t<br />
towards a diagnosis <strong>of</strong> hypervolemia due<br />
to heart failure with moderate specificity<br />
Abbreviations<br />
BUN<br />
CO<br />
CTR<br />
CVP<br />
CXR<br />
Ea dyn<br />
EABV<br />
ED<br />
FE UN<br />
IVC<br />
PAOP<br />
PLR<br />
blood urea nitrogen<br />
cardiac output<br />
cardiothoracic ratio<br />
central venous pressure<br />
chest x-ray<br />
dynamic arterial elastance<br />
effective arterial blood <strong>volume</strong><br />
<strong>emergency</strong> <strong>department</strong><br />
fractional excretion <strong>of</strong> urea<br />
<strong>in</strong>ferior vena cava<br />
pulmonary artery occlusion pressure<br />
passive leg rais<strong>in</strong>g<br />
ROC-AUC area under <strong>the</strong> receiver operat<strong>in</strong>g<br />
characteristic curve<br />
VPW<br />
vascular pedicle width<br />
326 | Mediz<strong>in</strong>ische Kl<strong>in</strong>ik - Intensivmediz<strong>in</strong> und Notfallmediz<strong>in</strong> 4 · 2017
<strong>in</strong>clude paroxysmal nocturnal dyspnea<br />
<strong>and</strong> orthopnea whereas dyspnea on exertion<br />
is <strong>the</strong> most sensitive anamnestic h<strong>in</strong>t.<br />
Dur<strong>in</strong>g physical exam<strong>in</strong>ation, jugular venous<br />
distention <strong>and</strong> abdom<strong>in</strong>ojugular reflux<br />
may secure <strong>the</strong> diagnosis <strong>of</strong> heart<br />
failure (however, <strong>the</strong>se signs have very<br />
low sensitivity). Among <strong>the</strong> more sensitive<br />
f<strong>in</strong>d<strong>in</strong>gs, lower extremity edema <strong>and</strong><br />
rales on lung auscultation may provide evidence<br />
for hypervolemia <strong>and</strong> heart failure.<br />
In cardiac patients, <strong>the</strong> synopsis <strong>of</strong><br />
cl<strong>in</strong>ical f<strong>in</strong>d<strong>in</strong>gs can be used to assign <strong>the</strong><br />
patient to a Killip class that was <strong>in</strong>itially<br />
proposed for risk stratification <strong>in</strong> patients<br />
with myocardial <strong>in</strong>farction [13].<br />
Taken toge<strong>the</strong>r, we consider <strong>the</strong> cl<strong>in</strong>ical<br />
exam<strong>in</strong>ation as an immediately available<br />
<strong>and</strong> cost-effective means to evaluate<br />
a patient’s <strong>volume</strong> <strong>status</strong> early after his arrival<br />
<strong>in</strong> <strong>the</strong> ED, which can help to guide<br />
<strong>the</strong> <strong>in</strong>itial resuscitation <strong>the</strong>rapy. However,<br />
cl<strong>in</strong>ical studies revealed significant limitations<br />
<strong>of</strong> cl<strong>in</strong>ical signs <strong>and</strong> symptoms <strong>in</strong><br />
<strong>the</strong> assessment <strong>of</strong> a patient’s <strong>volume</strong> <strong>status</strong><br />
[8, 10, 14, 15].<br />
Laboratory parameters<br />
Blood urea nitrogen/<br />
creat<strong>in</strong><strong>in</strong>e ratio<br />
Volume depletion <strong>in</strong>duces a neurohumeral<br />
response which enhances <strong>the</strong> reabsorption<br />
<strong>of</strong> sodium <strong>and</strong> water <strong>in</strong> <strong>the</strong> proximal<br />
tubule. S<strong>in</strong>ce urea reabsorption occurs<br />
passively <strong>in</strong> this very part <strong>of</strong> <strong>the</strong> nephron,<br />
<strong>volume</strong> depletion also causes an <strong>in</strong>crease<br />
<strong>in</strong> urea reabsorption. The blood urea nitrogen<br />
(BUN)/serum creat<strong>in</strong><strong>in</strong>e ratio is<br />
approximately 10:1 <strong>in</strong> normal subjects but<br />
may be substantially elevated <strong>in</strong> hypovolemic<br />
states [16]. In a state called “prerenal<br />
azotemia,” true <strong>volume</strong> depletion or<br />
decreased effective arterial blood <strong>volume</strong><br />
(EABV) go along with BUN/creat<strong>in</strong><strong>in</strong>e ratios<br />
<strong>of</strong> 20:1 <strong>and</strong> higher. Decreased EABV<br />
<strong>volume</strong> may occur <strong>in</strong> edematous disorders<br />
such as cardiac failure, liver cirrhosis,<br />
<strong>and</strong> more rarely nephrotic syndrome<br />
[17]. Although <strong>the</strong>re are quite a few confound<strong>in</strong>g<br />
conditions such as <strong>in</strong>take <strong>of</strong> steroid<br />
medication or upper gastro<strong>in</strong>test<strong>in</strong>al<br />
bleed<strong>in</strong>g, <strong>the</strong> BUN/creat<strong>in</strong><strong>in</strong>e ratio rema<strong>in</strong>s<br />
an easily obta<strong>in</strong>able tool for <strong>volume</strong><br />
<strong>status</strong> assessment. We would like to po<strong>in</strong>t<br />
out that mere creat<strong>in</strong><strong>in</strong>e levels are poor <strong>in</strong>dicators<br />
<strong>of</strong> kidney function <strong>in</strong> <strong>the</strong> elderly,<br />
<strong>and</strong> <strong>the</strong> use <strong>of</strong> formulas to estimate glomerular<br />
filtration rate is strongly suggested<br />
<strong>in</strong> this patient group [18].<br />
Ur<strong>in</strong>ary sodium <strong>and</strong> fractional<br />
excretion <strong>of</strong> urea<br />
Ur<strong>in</strong>alysis is <strong>of</strong>ten performed <strong>in</strong> <strong>the</strong> ED<br />
dur<strong>in</strong>g <strong>the</strong> evaluation <strong>of</strong> common symptoms<br />
such as fever or abdom<strong>in</strong>al discomfort.<br />
A “spot ur<strong>in</strong>e” sample may also aid <strong>in</strong><br />
evaluat<strong>in</strong>g <strong>volume</strong> <strong>status</strong>. The aforementioned<br />
neurohumeral response to <strong>volume</strong><br />
depletion or decreased EABV <strong>in</strong>duces <strong>the</strong><br />
kidneys to reta<strong>in</strong> sodium <strong>and</strong> subsequently<br />
water <strong>in</strong> order to (re-)exp<strong>and</strong> <strong>the</strong> extracellular<br />
<strong>fluid</strong> compartment. Chung <strong>and</strong><br />
colleagues were able to demonstrate that<br />
<strong>in</strong> contrast to cl<strong>in</strong>ical assessment by two<br />
experienced nephrologists <strong>the</strong> spot ur<strong>in</strong>ary<br />
sodium concentration was highly<br />
sensitive to dist<strong>in</strong>guish between hypovolemic<br />
<strong>and</strong> euvolemic patients with hyponatremia<br />
[15]. In <strong>the</strong>ir study, a spot ur<strong>in</strong>ary<br />
sodium concentration <strong>of</strong> less than<br />
30 mmol/L was 100 % specific <strong>and</strong> 80 %<br />
sensitive to detect patients with hyponatremia<br />
who had elevated plasma ren<strong>in</strong> <strong>and</strong><br />
norep<strong>in</strong>ephr<strong>in</strong>e concentrations, responded<br />
to <strong>in</strong>fusion <strong>of</strong> isotonic sal<strong>in</strong>e, <strong>and</strong> were<br />
thus deemed to be hypovolemic.<br />
However, when hypovolemia occurs<br />
due to an overzealous use <strong>of</strong> loop <strong>and</strong> thiazide<br />
diuretics, low ur<strong>in</strong>ary sodium concentrations<br />
lose <strong>the</strong>ir sensitivity to detect<br />
<strong>volume</strong> depletion. As sodium <strong>and</strong> water<br />
are reabsorbed <strong>in</strong> <strong>the</strong> proximal tubulus,<br />
<strong>the</strong> fractional excretion <strong>of</strong> urea (FE UN )<br />
rema<strong>in</strong>s unaffected. In patients with renal<br />
hypoperfusion, a FE UN <strong>of</strong> ≤ 35 % was<br />
found to be <strong>in</strong>dicative <strong>of</strong> kidney <strong>in</strong>jury<br />
due to hypovolemia or decreased EABV<br />
even after adm<strong>in</strong>istration <strong>of</strong> diuretic <strong>the</strong>rapy<br />
(sensitivity <strong>and</strong> specificity <strong>of</strong> 90 <strong>and</strong><br />
96 %, respectively [19]). However, <strong>the</strong>se<br />
results were challenged by ano<strong>the</strong>r study<br />
<strong>in</strong> which <strong>the</strong> diagnostic accuracy <strong>of</strong> FE UN<br />
was explored prospectively. Pép<strong>in</strong> et al.<br />
demonstrated that FE UN performed ra<strong>the</strong>r<br />
poorly, irrespective <strong>of</strong> whe<strong>the</strong>r diuretics<br />
had been adm<strong>in</strong>istered or not [20].<br />
In summary, a ur<strong>in</strong>ary spot sodium <strong>of</strong><br />
less than 30 mmol/L is very specific <strong>and</strong><br />
moderately sensitive to detect hypovolemia.<br />
After diuretic <strong>the</strong>rapy, a FE UN <strong>of</strong><br />
≤ 35 % may still be able to support <strong>the</strong> diagnosis<br />
<strong>of</strong> hypovolemia, although reports<br />
on its diagnostic accuracy are contradictive.<br />
Blood lactate<br />
Screen<strong>in</strong>g for hypotension alone might<br />
miss patients at risk for circulatory failure<br />
[21]. Elevated serum lactate levels <strong>in</strong>dicate<br />
ongo<strong>in</strong>g tissue hypoxia <strong>and</strong> are associated<br />
with a worse prognosis <strong>in</strong> acutely<br />
ill patients [22], <strong>in</strong>dependent <strong>of</strong> age,<br />
blood pressure, or o<strong>the</strong>r comorbidities<br />
[23]. Therefore, we advocate a liberal use<br />
<strong>of</strong> sequential [24] lactate measurements<br />
<strong>in</strong> <strong>the</strong> ED while be<strong>in</strong>g aware <strong>of</strong> potential<br />
confounders such as biguanide or antiretroviral<br />
medications <strong>and</strong> liver disease.<br />
Bedside ultrasound<br />
Bedside ultrasound may provide valuable<br />
<strong>in</strong>formation on circulatory function that<br />
cannot be obta<strong>in</strong>ed by cl<strong>in</strong>ical assessment.<br />
It may detect <strong>the</strong> presence <strong>of</strong> pericardial<br />
<strong>and</strong> pleural effusions or ascites, which<br />
may give important diagnostic clues both<br />
for patients suspected to have decreased<br />
EABV <strong>and</strong> patients with <strong>fluid</strong> loss to <strong>the</strong><br />
abdom<strong>in</strong>al or thoracic compartment (e.g.,<br />
pancreatitis). Fur<strong>the</strong>rmore, <strong>the</strong> diameter<br />
<strong>of</strong> <strong>the</strong> <strong>in</strong>ferior vena cava (IVC) can be used<br />
to estimate right cardiac function <strong>and</strong> central<br />
venous pressure (CVP). Accord<strong>in</strong>g to<br />
current guidel<strong>in</strong>es, a low right atrial pressure<br />
(0–5 mmHg) can be <strong>in</strong>ferred from<br />
an IVC diameter <strong>of</strong> ≤ 2.1 cm that collapses<br />
> 50 % with a sniff. On <strong>the</strong> contrary,<br />
an IVC diameter > 2.1 cm without a collapse<br />
<strong>of</strong> 50 % with a sniff suggests a high<br />
right atrial pressure (10–20 mmHg). Values<br />
found <strong>in</strong> between are considered <strong>in</strong>determ<strong>in</strong>ate<br />
<strong>and</strong> an <strong>in</strong>termediate pressure is<br />
<strong>the</strong>n assumed [25].<br />
The IVC diameter is not affected by<br />
<strong>the</strong> neurohumeral stress response but will<br />
adapt to changes <strong>in</strong> CVP such as <strong>volume</strong><br />
depletion or <strong>fluid</strong> resuscitation [26, 27].<br />
In particular, <strong>the</strong> expiratory IVC (IVCe)<br />
diameter correlated well with complete<br />
blood <strong>volume</strong>, as determ<strong>in</strong>ed by I131-labeled<br />
album<strong>in</strong> dilution, <strong>in</strong> patients with<br />
iatrogenic <strong>volume</strong> depletion, that is hemodialysis<br />
[28]. Although ultrasonographic<br />
Mediz<strong>in</strong>ische Kl<strong>in</strong>ik - Intensivmediz<strong>in</strong> und Notfallmediz<strong>in</strong> 4 · 2017 |<br />
327
Abstract · Zusammenfassung<br />
evaluation is known to be dependent on<br />
sonographer experience, M-Mode IVC<br />
diameter measurements as perfomed by<br />
ED residents after a short course <strong>of</strong> tra<strong>in</strong><strong>in</strong>g<br />
had a high degree <strong>of</strong> <strong>in</strong>terrater reliability<br />
[29].<br />
IVCe was consistently <strong>and</strong> significantly<br />
lower <strong>in</strong> hypovolemic trauma patients<br />
with confirmed or suspected blood loss<br />
[30–32]. Weekes <strong>and</strong> colleagues showed<br />
that <strong>in</strong> hypovolemic ED patients, <strong>the</strong> IVCe<br />
diameter <strong>and</strong> caval <strong>in</strong>dex <strong>in</strong>creased <strong>and</strong><br />
decreased, respectively, after a mean <strong>fluid</strong><br />
bolus <strong>of</strong> 2580 mL [27].<br />
In summary, IVCe diameter <strong>and</strong> caval<br />
<strong>in</strong>dex provide a non<strong>in</strong>vasive, quickly obta<strong>in</strong>able,<br />
<strong>and</strong> reproducible tool to assess<br />
<strong>in</strong>travascular <strong>volume</strong> <strong>status</strong> before <strong>and</strong> after<br />
<strong>fluid</strong> resucitation that seems well suited<br />
for <strong>the</strong> ED.<br />
However, ultrasonographic exam<strong>in</strong>ation<br />
<strong>of</strong> <strong>the</strong> IVC diameter has several limitations:<br />
<strong>in</strong> patients with right ventricular<br />
failure <strong>the</strong> IVC diameter will be elevated<br />
even <strong>in</strong> <strong>the</strong> presence <strong>of</strong> hypovolemia <strong>and</strong><br />
shock.<br />
Despite its ability to estimate CVP <strong>and</strong><br />
<strong>in</strong>travascular <strong>volume</strong> <strong>status</strong>, IVC diameter<br />
<strong>and</strong> collapsibility <strong>in</strong>dex will not provide<br />
<strong>in</strong>formation on a patient’s <strong>fluid</strong> <strong>responsiveness</strong>.<br />
Corl <strong>and</strong> colleagues showed that<br />
nei<strong>the</strong>r <strong>the</strong> <strong>in</strong>itial nor <strong>the</strong> dynamic (i.e., after<br />
a passive leg raise maneuver) caval <strong>in</strong>dex<br />
could predict <strong>fluid</strong> <strong>responsiveness</strong> <strong>in</strong><br />
an ED patient cohort [33].<br />
Echocardiography plays a crucial role<br />
<strong>in</strong> <strong>the</strong> <strong>in</strong>itial evaluation <strong>of</strong> ED patients for<br />
<strong>the</strong> differentiation <strong>of</strong> different etiologies<br />
<strong>of</strong> hemodynamic <strong>in</strong>stability or shock [34,<br />
35]. Besides <strong>the</strong> differential diagnosis <strong>of</strong><br />
cardiac <strong>and</strong> noncardiac causes <strong>of</strong> shock,<br />
echocardiography allows <strong>the</strong> estimation <strong>of</strong><br />
left <strong>and</strong> right ventricular dysfunction <strong>and</strong><br />
valvular dysfunction [34]. In addition to<br />
static parameters, it provides non<strong>in</strong>vasive<br />
means to exam<strong>in</strong>e dynamic parameters <strong>of</strong><br />
<strong>volume</strong> <strong>responsiveness</strong> (for details please<br />
see below) [36]. Stroke <strong>volume</strong> <strong>and</strong> cardiac<br />
output (CO) can be estimated by measur<strong>in</strong>g<br />
<strong>the</strong> velocity–time <strong>in</strong>tegral <strong>of</strong> <strong>the</strong><br />
aortic outflow <strong>and</strong> <strong>the</strong> aortic valve area <strong>in</strong><br />
<strong>the</strong> apical five-chamber <strong>and</strong> parasternal<br />
long-axis view, respectively.<br />
Med Kl<strong>in</strong> Intensivmed Notfmed 2017 · 112:326–333<br />
© Spr<strong>in</strong>ger-Verlag Berl<strong>in</strong> Heidelberg 2015<br />
Chest x-ray<br />
Results obta<strong>in</strong>ed from a chest x-ray (CXR)<br />
will add additional <strong>in</strong>formation on <strong>the</strong><br />
presence or absence <strong>of</strong> hypervolemia.<br />
However, classic radiographic signs <strong>of</strong><br />
<strong>volume</strong> overload such as pleural effusions<br />
or peribronchial cuff<strong>in</strong>gs correlate poorly<br />
with <strong>the</strong> <strong>in</strong>vasive determ<strong>in</strong>ation <strong>of</strong> <strong>volume</strong><br />
<strong>status</strong> or extravascular lung water [14,<br />
37, 38]. Unlike those classic signs <strong>of</strong> <strong>in</strong>creased<br />
pulmonary hydration, <strong>the</strong> vascular<br />
pedicle width (VPW)—that is, <strong>the</strong> distance<br />
between a perpendicular l<strong>in</strong>e from<br />
<strong>the</strong> po<strong>in</strong>t where <strong>the</strong> left subclavian artery<br />
exits <strong>the</strong> aortic arch <strong>and</strong> <strong>the</strong> cross<strong>in</strong>g <strong>of</strong><br />
<strong>the</strong> superior vena cava <strong>and</strong> <strong>the</strong> left ma<strong>in</strong><br />
DOI 10.1007/s00063-015-0124-x<br />
C. Maurer · J.Y. Wagner · R.M. Schmid · B. Saugel<br />
<strong>Assessment</strong> <strong>of</strong> <strong>volume</strong> <strong>status</strong> <strong>and</strong> <strong>fluid</strong> <strong>responsiveness</strong> <strong>in</strong><br />
<strong>the</strong> <strong>emergency</strong> <strong>department</strong>: a systematic approach<br />
Abstract<br />
When treat<strong>in</strong>g acutely ill patients <strong>in</strong> <strong>the</strong><br />
<strong>emergency</strong> <strong>department</strong> (ED), <strong>the</strong> successful<br />
management <strong>of</strong> a variety <strong>of</strong> medical conditions,<br />
such as sepsis, acute kidney <strong>in</strong>jury, <strong>and</strong><br />
pancreatitis, is highly dependent on <strong>the</strong> correct<br />
assessment <strong>and</strong> optimization <strong>of</strong> a patient’s<br />
<strong>in</strong>travascular <strong>volume</strong> <strong>status</strong>. Therefore,<br />
it is crucial that <strong>the</strong> ED physician knows<br />
<strong>and</strong> uses available means to assess <strong>in</strong>travascular<br />
<strong>volume</strong> <strong>status</strong> to adequately guide <strong>fluid</strong><br />
<strong>the</strong>rapy. This review focuses on techniques<br />
for <strong>volume</strong> <strong>status</strong> assessment that are available<br />
<strong>in</strong> <strong>the</strong> ED <strong>in</strong>clud<strong>in</strong>g basic cl<strong>in</strong>ical <strong>and</strong> laboratory<br />
f<strong>in</strong>d<strong>in</strong>gs, apparatus-based tests such<br />
as sonography <strong>and</strong> chest x-ray, <strong>and</strong> functional<br />
tests to evaluate <strong>fluid</strong> <strong>responsiveness</strong>. Fur<strong>the</strong>rmore,<br />
we provide an outlook on promis<strong>in</strong>g<br />
<strong>in</strong>novative, non<strong>in</strong>vasive technologies that<br />
might be used for advanced hemodynamic<br />
monitor<strong>in</strong>g <strong>in</strong> <strong>the</strong> ED.<br />
Keywords<br />
Shock · Sepsis · Volume <strong>the</strong>rapy ·<br />
Fluid deficiency · Passive leg rais<strong>in</strong>g ·<br />
Fluid challenge · Advanced hemodynamic<br />
monitor<strong>in</strong>g · Non<strong>in</strong>vasive cardiac output<br />
Die Bestimmung des Volumen<strong>status</strong> und der Volumenreagibilität<br />
<strong>in</strong> der Notaufnahme – e<strong>in</strong> systematischer Ansatz<br />
Zusammenfassung<br />
Bei der Beh<strong>and</strong>lung akut kranker Patienten<br />
<strong>in</strong> der Notaufnahme hängt die erfolgreiche<br />
Beh<strong>and</strong>lung e<strong>in</strong>er Reihe von Erkrankungen<br />
(z. B. Sepsis, akutes Nierenversagen,<br />
Pankreatitis) <strong>in</strong> hohem Maße von der<br />
korrekten E<strong>in</strong>schätzung und Optimierung<br />
des <strong>in</strong>travaskulären Volumen<strong>status</strong> des<br />
Patienten ab. Daher ist es entscheidend für<br />
e<strong>in</strong>e adäquate Steuerung der Volumen<strong>the</strong>rapie,<br />
dass der Notfallmediz<strong>in</strong>er die verschiedenen<br />
Methoden zur Abschätzung des<br />
<strong>in</strong>travaskulären Volumen<strong>status</strong> kennt und zur<br />
Anwendung br<strong>in</strong>gt. Dieser Übersichtsartikel<br />
beh<strong>and</strong>elt Methoden zur Abschätzung des<br />
Volumen<strong>status</strong>, die <strong>in</strong> der Notaufnahme verfügbar<br />
s<strong>in</strong>d, wie grundlegende kl<strong>in</strong>ische und<br />
laborchemische Untersuchungen, Ultraschallund<br />
Röntgendiagnostik und funktionelle<br />
Tests zur Beurteilung der Volumenreagibilität.<br />
Desweiteren wird e<strong>in</strong> Ausblick gegeben<br />
auf vielversprechende, <strong>in</strong>novative, nicht-<strong>in</strong>vasive<br />
Technologien, die für e<strong>in</strong> erweitertes<br />
hämodynamisches Monitor<strong>in</strong>g <strong>in</strong> der Notaufnahme<br />
verwendet werden könnten.<br />
Schlüsselwörter<br />
Schock · Sepsis · Volumen<strong>the</strong>rapie ·<br />
Volumenmangel · Passive leg rais<strong>in</strong>g ·<br />
Fluid challenge · Erweitertes<br />
hämodynamisches Monitor<strong>in</strong>g ·<br />
Nicht-<strong>in</strong>vasives Herzzeit<strong>volume</strong>n<br />
bronchus—<strong>and</strong> <strong>the</strong> cardiothoracic ratio<br />
(CTR) seem to provide a more robust estimation<br />
<strong>of</strong> cardiac preload [39]. Ely <strong>and</strong><br />
colleagues divided mechanically ventilated<br />
<strong>in</strong>tensive care unit patients <strong>in</strong>to groups<br />
<strong>of</strong> high <strong>and</strong> low/normal <strong>volume</strong> <strong>status</strong> after<br />
measur<strong>in</strong>g pulmonary artery occlusion<br />
pressure (PAOP) [40]. By <strong>in</strong>tegrat<strong>in</strong>g<br />
<strong>the</strong> objective parameters VPW <strong>and</strong> CTR<br />
<strong>in</strong>to <strong>the</strong> analysis <strong>of</strong> a portable sup<strong>in</strong>e CXR,<br />
radiologists were able to <strong>in</strong>crease <strong>the</strong> likelihood<br />
ratio <strong>of</strong> <strong>the</strong> CXR to correctly determ<strong>in</strong>e<br />
<strong>volume</strong> <strong>status</strong>. The optimal cut<strong>of</strong>f<br />
for <strong>the</strong> dist<strong>in</strong>ction between high <strong>and</strong><br />
normal/low <strong>volume</strong> <strong>status</strong> <strong>in</strong> this <strong>in</strong>vestigation<br />
was 70 mm for VPW <strong>and</strong> 0.55 for<br />
CTR. Limitations <strong>of</strong> this cost-effective <strong>and</strong><br />
328 | Mediz<strong>in</strong>ische Kl<strong>in</strong>ik - Intensivmediz<strong>in</strong> und Notfallmediz<strong>in</strong> 4 · 2017
quickly obta<strong>in</strong>able technique <strong>in</strong>clude <strong>the</strong><br />
<strong>in</strong>ability <strong>of</strong> <strong>the</strong> CXR to detect hypovolemia<br />
[14], an accuracy <strong>of</strong> at best 70 % (leav<strong>in</strong>g<br />
a substantial 30 % <strong>of</strong> patients misclassified),<br />
<strong>and</strong> miss<strong>in</strong>g data on <strong>the</strong> significance<br />
<strong>of</strong> VPW <strong>and</strong> CTR <strong>in</strong> a spontaneously<br />
breath<strong>in</strong>g ED patient cohort. Despite<br />
<strong>the</strong>se limitations, we agree with Ely<br />
et al. to “use <strong>the</strong> <strong>in</strong>formation already available<br />
on <strong>the</strong> patient’s CXR to its maximum<br />
potential” [37].<br />
Central venous pressure<br />
The implantation <strong>of</strong> a central l<strong>in</strong>e <strong>and</strong> <strong>the</strong><br />
measurement <strong>of</strong> CVP are among <strong>the</strong> <strong>in</strong>vasive<br />
procedures that can be performed<br />
<strong>in</strong> <strong>the</strong> ED.<br />
However, <strong>the</strong>re are considerable differences<br />
<strong>in</strong> <strong>the</strong> cl<strong>in</strong>ical practice <strong>of</strong> central venous<br />
ca<strong>the</strong>terization <strong>in</strong> <strong>the</strong> ED among different<br />
countries [41, 42]. Whereas <strong>in</strong> specific<br />
patient groups placement <strong>of</strong> a central<br />
venous ca<strong>the</strong>ter seems to be rout<strong>in</strong>e cl<strong>in</strong>ical<br />
ED practice <strong>in</strong> <strong>the</strong> USA <strong>and</strong> Australia<br />
(e.g., treatment <strong>of</strong> <strong>the</strong> control group <strong>in</strong><br />
<strong>the</strong> ProCESS <strong>and</strong> ARISE studies [43, 44]),<br />
central venous ca<strong>the</strong>terization is rarely<br />
performed <strong>in</strong> European ED sett<strong>in</strong>gs.<br />
In this context, it is questionable<br />
whe<strong>the</strong>r ED patients benefit from <strong>the</strong><br />
placement <strong>of</strong> a central venous l<strong>in</strong>e with<br />
regard to <strong>the</strong>ir hemodynamic management<br />
as <strong>the</strong>re is abundant evidence that<br />
CVP is a poor predictor <strong>of</strong> cardiac preload<br />
<strong>and</strong> <strong>fluid</strong> <strong>responsiveness</strong> [45–47]. Marik<br />
<strong>and</strong> Cavallazzi performed a meta-analysis<br />
<strong>in</strong>clud<strong>in</strong>g 43 studies that reported <strong>the</strong><br />
correlation coefficient or area under <strong>the</strong><br />
receiver operat<strong>in</strong>g characteristic curve<br />
(ROC-AUC) between CVP <strong>and</strong> changes<br />
<strong>in</strong> stroke <strong>volume</strong> <strong>in</strong>dex or cardiac <strong>in</strong>dex<br />
follow<strong>in</strong>g an <strong>in</strong>tervention-related change<br />
<strong>in</strong> cardiac preload [47]. The authors demonstrated<br />
that <strong>the</strong> CVP is able to predict<br />
<strong>fluid</strong> <strong>responsiveness</strong> with a ROC-AUC <strong>of</strong><br />
only 56 %. Therefore, CVP as a static measure<br />
<strong>of</strong> cardiac preload should not be used<br />
to guide <strong>fluid</strong> <strong>the</strong>rapy <strong>and</strong> assess <strong>fluid</strong> <strong>responsiveness</strong><br />
[48].<br />
Functional tests for<br />
<strong>the</strong> assessment <strong>of</strong> <strong>fluid</strong><br />
<strong>responsiveness</strong> <strong>in</strong> <strong>the</strong> ED<br />
The aforementioned tests may quickly<br />
aid to determ<strong>in</strong>e a patient’s <strong>in</strong>travascular<br />
<strong>volume</strong> <strong>status</strong> after his arrival <strong>in</strong> <strong>the</strong><br />
ED. However, <strong>the</strong>y provide no <strong>in</strong>formation<br />
on whe<strong>the</strong>r this patient will benefit<br />
from <strong>fluid</strong> <strong>the</strong>rapy or not. To come to<br />
<strong>the</strong> crucial decision <strong>of</strong> whe<strong>the</strong>r to adm<strong>in</strong>ister<br />
<strong>fluid</strong> <strong>the</strong>rapy or not, two functional<br />
tests—<strong>the</strong> passive leg-rais<strong>in</strong>g test (PLR)<br />
<strong>and</strong> <strong>the</strong> <strong>fluid</strong> challenge test—are available<br />
<strong>and</strong> have been studied primarily <strong>in</strong> <strong>in</strong>tensive<br />
care unit patients. However, <strong>in</strong> <strong>the</strong> ED<br />
sett<strong>in</strong>g, <strong>the</strong> cl<strong>in</strong>ical applicability <strong>of</strong> <strong>the</strong>se<br />
tests might be limited due to restra<strong>in</strong>ts<br />
<strong>in</strong> hemodynamic monitor<strong>in</strong>g modalities.<br />
However, despite <strong>the</strong> limited availability<br />
<strong>of</strong> advanced hemodynamic monitor<strong>in</strong>g,<br />
<strong>the</strong> ED physician might perform a PLR or<br />
<strong>fluid</strong> challenge test us<strong>in</strong>g surrogate endpo<strong>in</strong>ts<br />
available <strong>in</strong> <strong>the</strong> ED sett<strong>in</strong>g.<br />
Passive leg-rais<strong>in</strong>g test<br />
Lift<strong>in</strong>g <strong>the</strong> legs <strong>of</strong> <strong>the</strong> patient passively<br />
from <strong>the</strong> horizontal position recruits<br />
venous blood <strong>volume</strong> <strong>and</strong> transfers it to<br />
<strong>the</strong> <strong>in</strong>trathoracic compartment [49–51].<br />
By us<strong>in</strong>g <strong>the</strong> PLR maneuver, a prediction<br />
whe<strong>the</strong>r a patient will be <strong>fluid</strong> responsive<br />
or not is possible without <strong>the</strong> need to<br />
give a <strong>fluid</strong> bolus [49, 51]. PLR is applicable<br />
even <strong>in</strong> arrhythmic <strong>and</strong> spontaneously<br />
breath<strong>in</strong>g patients [51]. As an endpo<strong>in</strong>t<br />
to def<strong>in</strong>e <strong>fluid</strong> <strong>responsiveness</strong> different<br />
hemodynamic parameters have been<br />
proposed. Although it has been shown<br />
that changes <strong>in</strong> radial pulse pressure <strong>in</strong>duced<br />
by PLR can be used for <strong>the</strong> prediction<br />
<strong>of</strong> <strong>fluid</strong> <strong>responsiveness</strong> <strong>in</strong> non<strong>in</strong>tubated<br />
patients [52], for an optimal utilization<br />
<strong>of</strong> this functional test, <strong>the</strong> immediate<br />
hemodynamic effects <strong>of</strong> PLR on blood<br />
flow (i.e., CO or stroke <strong>volume</strong>) should<br />
be assessed 30–90 s after <strong>the</strong> onset <strong>of</strong> <strong>the</strong><br />
test [51, 53, 54] because <strong>the</strong> predictive value<br />
<strong>of</strong> PLR-<strong>in</strong>duced changes <strong>in</strong> CO is higher<br />
compared with changes <strong>in</strong> arterial pulse<br />
pressure [55]. Because usually <strong>in</strong>vasive real-time<br />
measurement <strong>of</strong> blood flow (e.g.,<br />
us<strong>in</strong>g pulse contour analysis) is not possible<br />
<strong>in</strong> <strong>the</strong> ED, <strong>in</strong> this sett<strong>in</strong>g, alternative<br />
methods for <strong>the</strong> estimation <strong>of</strong> CO/stroke<br />
<strong>volume</strong> or surrogate parameters might be<br />
considered.<br />
Accord<strong>in</strong>g to recent guidel<strong>in</strong>es [56],<br />
PLR maneuver-<strong>in</strong>duced blood pressure<br />
changes can be used as a surrogate marker<br />
for <strong>the</strong> <strong>in</strong>itial assessment <strong>of</strong> <strong>fluid</strong> <strong>responsiveness</strong>.<br />
In this context, Lakhal et al.<br />
demonstrated that PLR-<strong>in</strong>duced changes<br />
<strong>in</strong> systolic arterial pressure measured with<br />
a brachial cuff are able to identify <strong>fluid</strong> responsive<br />
patients [57]. Lamia <strong>and</strong> coworkers<br />
described <strong>the</strong> assessment <strong>of</strong> PLR-<strong>in</strong>duced<br />
changes <strong>of</strong> stroke <strong>volume</strong> by echocardiography<br />
<strong>in</strong> critically ill patients with<br />
spontaneous breath<strong>in</strong>g activity [58]. In<br />
addition, it was suggested that changes<br />
<strong>in</strong> <strong>the</strong> pulse oximetry plethysmographic<br />
waveform amplitude might be used dur<strong>in</strong>g<br />
PLR <strong>in</strong> spontaneously breath<strong>in</strong>g patients<br />
[59].<br />
Fluid challenge<br />
In order to assess <strong>fluid</strong> <strong>responsiveness</strong>, a<br />
<strong>fluid</strong> challenge test follow<strong>in</strong>g a structured<br />
protocol can be performed [60, 61]. Dur<strong>in</strong>g<br />
a <strong>fluid</strong> challenge test a certa<strong>in</strong> amount<br />
<strong>of</strong> <strong>fluid</strong> is given <strong>in</strong>travenously over a predef<strong>in</strong>ed<br />
period <strong>of</strong> time, <strong>and</strong> <strong>the</strong> <strong>in</strong>duced<br />
changes <strong>in</strong> hemodynamic parameters<br />
are observed [62]. The best way to monitor<br />
hemodynamic effects <strong>of</strong> a <strong>fluid</strong> challenge<br />
is to cont<strong>in</strong>uously observe CO [60].<br />
A <strong>fluid</strong> challenge-<strong>in</strong>duced <strong>in</strong>crease <strong>in</strong><br />
blood flow (i.e., stroke <strong>volume</strong> or CO) <strong>of</strong><br />
10–15 % <strong>in</strong>dicates that <strong>the</strong> patient is <strong>in</strong> <strong>the</strong><br />
<strong>volume</strong>-dependent upward slope <strong>of</strong> <strong>the</strong><br />
Frank–Starl<strong>in</strong>g curve <strong>and</strong> thus <strong>fluid</strong> responsive<br />
[60, 63]. Because <strong>the</strong> <strong>fluid</strong> challenge<br />
maneuver directly assesses <strong>the</strong> actual<br />
hemodynamic response to <strong>fluid</strong> load<strong>in</strong>g,<br />
it can be considered <strong>the</strong> st<strong>and</strong>ard criterion<br />
method for <strong>the</strong> evaluation <strong>of</strong> <strong>fluid</strong><br />
<strong>responsiveness</strong>. S<strong>in</strong>ce only about 50 % <strong>of</strong><br />
critically ill patients are <strong>fluid</strong> responsive,<br />
careful hemodynamic monitor<strong>in</strong>g dur<strong>in</strong>g<br />
a <strong>fluid</strong> challenge is <strong>of</strong> utmost importance<br />
to promptly identify “non-responders”<br />
<strong>and</strong> avoid unnecessary <strong>fluid</strong> load<strong>in</strong>g.<br />
The fact that assessment <strong>of</strong> CO is not rout<strong>in</strong>ely<br />
possible <strong>in</strong> <strong>the</strong> ED limits <strong>the</strong> cl<strong>in</strong>ical<br />
applicability <strong>of</strong> <strong>the</strong> <strong>fluid</strong> challenge test<br />
<strong>in</strong> this sett<strong>in</strong>g. Blood pressure can only be<br />
considered as a surrogate marker for <strong>fluid</strong><br />
<strong>responsiveness</strong>. However, for <strong>the</strong> assessment<br />
<strong>of</strong> <strong>fluid</strong> <strong>responsiveness</strong> based on a<br />
Mediz<strong>in</strong>ische Kl<strong>in</strong>ik - Intensivmediz<strong>in</strong> und Notfallmediz<strong>in</strong> 4 · 2017 |<br />
329
Übersichten<br />
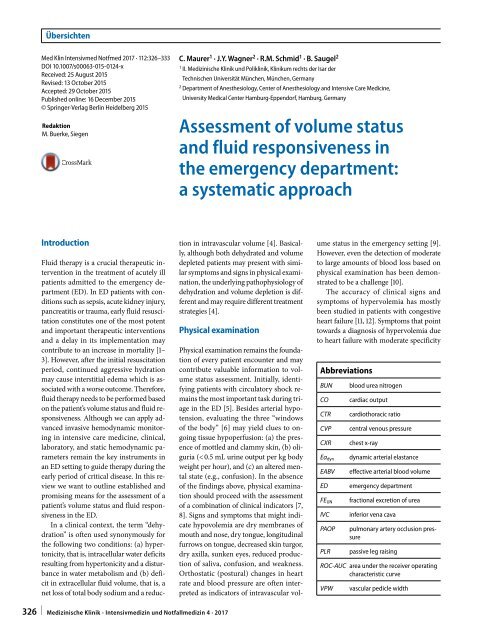
Patient admitted to ED<br />
Initial assessment<br />
1) focussed history + physical exam<strong>in</strong>ation<br />
2) basic monitor<strong>in</strong>g: blood pressure, heart rate, SaO2<br />
3) i.v. access + blood withdrawal<br />
Evidence for shock<br />
+<br />
Detailed physical exam<strong>in</strong>ation<br />
–<br />
Signs <strong>of</strong> hypovolemia<br />
+<br />
Biochemistry/laboratory tests<br />
–<br />
Indicative for<br />
a) hypovolemia<br />
b) microcirculatory failure<br />
+<br />
–<br />
IVC ultrasound<br />
Intravascular<br />
hypovolemia<br />
+<br />
–<br />
Chest X-ray<br />
+<br />
Indicative for<br />
pulmonary <strong>fluid</strong><br />
overload<br />
–<br />
Assess <strong>fluid</strong> <strong>responsiveness</strong><br />
1. Passive leg rais<strong>in</strong>g test<br />
2. Fluid challenge test<br />
Consider negative<br />
<strong>fluid</strong> balance<br />
Preserve <strong>fluid</strong><br />
<strong>status</strong><br />
Fluid responsivenss<br />
–<br />
+<br />
1. Consider advanced hemodynamic monitor<strong>in</strong>g<br />
2. Fur<strong>the</strong>r diagnostic workup<br />
Fluid<br />
adm<strong>in</strong>istration<br />
Fig. 1 8 Algorithm for evaluat<strong>in</strong>g <strong>volume</strong> <strong>status</strong> <strong>and</strong> <strong>fluid</strong> <strong>responsiveness</strong> <strong>in</strong> <strong>the</strong> <strong>emergency</strong> <strong>department</strong><br />
330 | Mediz<strong>in</strong>ische Kl<strong>in</strong>ik - Intensivmediz<strong>in</strong> und Notfallmediz<strong>in</strong> 4 · 2017
<strong>fluid</strong> challenge, <strong>the</strong> use <strong>of</strong> <strong>the</strong> mean arterial<br />
pressure as <strong>the</strong> cl<strong>in</strong>ical endpo<strong>in</strong>t <strong>and</strong><br />
<strong>the</strong> CVP as <strong>the</strong> “safety limit” has been proposed<br />
[61] <strong>and</strong> is feasible <strong>in</strong> <strong>the</strong> ED sett<strong>in</strong>g.<br />
Although it has been shown that B-<br />
type natriuretic peptide is not able to accurately<br />
predict <strong>fluid</strong> <strong>responsiveness</strong> <strong>in</strong><br />
patients with acute circulatory failure<br />
[64], it might be to identify patients with<br />
systolic cardiac dysfunction <strong>and</strong> a high<br />
risk for <strong>fluid</strong> overload prior to a <strong>fluid</strong> challenge<br />
test.<br />
Innovative cont<strong>in</strong>uous<br />
non<strong>in</strong>vasive concepts for<br />
advanced hemodynamic<br />
monitor<strong>in</strong>g: <strong>the</strong> future <strong>in</strong> <strong>the</strong> ED?<br />
The commonly used hemodynamic measures<br />
<strong>in</strong> <strong>the</strong> ED are heart rate <strong>and</strong> <strong>in</strong>termittently<br />
obta<strong>in</strong>ed non<strong>in</strong>vasive blood<br />
pressure measurements us<strong>in</strong>g oscillometry.<br />
In recent years, however, large studies<br />
revealed severe limitations <strong>of</strong> <strong>the</strong> oscillometric<br />
method, for example, <strong>in</strong> obese<br />
<strong>and</strong> arrhythmic patients [65, 66]. Moreover,<br />
cl<strong>in</strong>ically relevant discrepancies between<br />
<strong>in</strong>vasive arterial ca<strong>the</strong>ter-derived<br />
<strong>and</strong> oscillometrically obta<strong>in</strong>ed blood pressure<br />
were demonstrated <strong>in</strong> critically ill patients<br />
[67].<br />
Invasive advanced hemodynamic<br />
monitor<strong>in</strong>g technologies can still usually<br />
not be applied <strong>in</strong> an ED sett<strong>in</strong>g. In <strong>the</strong><br />
future, however, <strong>in</strong>novative technologies<br />
allow<strong>in</strong>g for a cont<strong>in</strong>uous <strong>and</strong> completely<br />
non<strong>in</strong>vasive estimation <strong>of</strong> blood pressure,<br />
CO, <strong>and</strong> o<strong>the</strong>r hemodynamic variables<br />
(e.g., pulse pressure variation, stroke<br />
<strong>volume</strong> variation) might allow advanced<br />
hemodynamic monitor<strong>in</strong>g even <strong>in</strong> ED patients.<br />
Among <strong>the</strong> multiple applications,<br />
<strong>the</strong> option to monitor changes <strong>in</strong> CO <strong>in</strong><br />
real time dur<strong>in</strong>g functional tests (PLR,<br />
<strong>fluid</strong> challenge) via non<strong>in</strong>vasive cont<strong>in</strong>uous<br />
CO measurements appears particularly<br />
<strong>in</strong>trigu<strong>in</strong>g. S<strong>in</strong>ce CO <strong>and</strong> stroke <strong>volume</strong><br />
are <strong>the</strong> hemodynamic variables that<br />
are most reliable <strong>in</strong> <strong>the</strong> prediction <strong>of</strong> <strong>fluid</strong><br />
<strong>responsiveness</strong> [63], <strong>the</strong>ir cont<strong>in</strong>uous record<strong>in</strong>g<br />
would help to identify those patients<br />
who are not <strong>fluid</strong> responsive, <strong>and</strong><br />
thus might be harmed by fur<strong>the</strong>r <strong>fluid</strong> adm<strong>in</strong>istration<br />
[60]. Toge<strong>the</strong>r with a potentially<br />
reduced probability <strong>of</strong> miss<strong>in</strong>g rapid<br />
changes <strong>in</strong> vital parameters [68, 69], cont<strong>in</strong>uous<br />
non<strong>in</strong>vasive monitor<strong>in</strong>g <strong>of</strong> arterial<br />
pressure <strong>and</strong> blood flow <strong>in</strong> <strong>the</strong> ED may<br />
<strong>the</strong>refore markedly improve both patient<br />
safety <strong>and</strong> optimization <strong>of</strong> <strong>volume</strong> <strong>status</strong><br />
<strong>and</strong> blood flow.<br />
A variety <strong>of</strong> non<strong>in</strong>vasive technologies<br />
have been proposed dur<strong>in</strong>g <strong>the</strong> past years<br />
that might contribute to assess<strong>in</strong>g a patient’s<br />
<strong>volume</strong> <strong>status</strong>, <strong>fluid</strong> <strong>responsiveness</strong>,<br />
<strong>and</strong> guid<strong>in</strong>g <strong>fluid</strong> <strong>the</strong>rapy <strong>in</strong> <strong>the</strong> ED <strong>in</strong> <strong>the</strong><br />
future. The vascular unload<strong>in</strong>g technique,<br />
for example, has already been proven to be<br />
feasible <strong>in</strong> cont<strong>in</strong>uous non<strong>in</strong>vasive blood<br />
pressure measurements <strong>in</strong> <strong>the</strong> ED sett<strong>in</strong>g<br />
[68, 69]. This method uses an <strong>in</strong>flatable<br />
f<strong>in</strong>ger cuff apply<strong>in</strong>g pressure to <strong>the</strong> f<strong>in</strong>ger<br />
<strong>and</strong> conta<strong>in</strong>s an <strong>in</strong>frared transmission plethysmograph<br />
to measure <strong>the</strong> f<strong>in</strong>ger artery<br />
diameter (i.e., blood <strong>volume</strong>) [70]. The arterial<br />
blood pressure waveform can <strong>the</strong>n<br />
be <strong>in</strong>directly deduced from <strong>the</strong> pressure<br />
that is needed to keep <strong>the</strong> <strong>volume</strong> <strong>in</strong> <strong>the</strong><br />
f<strong>in</strong>ger artery constant throughout <strong>the</strong> cardiac<br />
cycle. Ano<strong>the</strong>r non<strong>in</strong>vasive technology<br />
that allows cont<strong>in</strong>uous blood pressure<br />
monitor<strong>in</strong>g <strong>and</strong> <strong>the</strong> estimation <strong>of</strong> CO is<br />
radial artery applanation tonometry [71–<br />
74]. Additional techniques that allow for<br />
<strong>the</strong> estimation <strong>of</strong> CO <strong>in</strong>clude thoracic<br />
electrical bioimpedance, thoracic bioreactance,<br />
<strong>and</strong> pulse wave transit time [75].<br />
As mentioned above, <strong>the</strong> use <strong>of</strong> <strong>the</strong>se<br />
non<strong>in</strong>vasive technologies for cont<strong>in</strong>uous<br />
hemodynamic monitor<strong>in</strong>g dur<strong>in</strong>g <strong>the</strong><br />
functional tests for <strong>fluid</strong> <strong>responsiveness</strong><br />
might pose a powerful approach. In this<br />
context, it is important that Cecconi et<br />
al. determ<strong>in</strong>ed dynamic arterial elastance<br />
(Ea dyn ) by us<strong>in</strong>g arterial pulse pressure<br />
analysis obta<strong>in</strong>ed by <strong>the</strong> aforementioned<br />
vascular unload<strong>in</strong>g technology <strong>in</strong> spontaneously<br />
breath<strong>in</strong>g patients [76]. Ea dyn was<br />
def<strong>in</strong>ed as <strong>the</strong> ratio between pulse pressure<br />
variation <strong>and</strong> stroke <strong>volume</strong> variation<br />
dur<strong>in</strong>g one respiratory cycle. Importantly,<br />
patients who had an <strong>in</strong>crease <strong>in</strong><br />
MAP <strong>of</strong> ≥ 10 % after a <strong>fluid</strong> challenge possessed<br />
a significantly higher pre<strong>in</strong>fusion-<br />
Ea dyn value than nonresponders. As a result,<br />
a pre<strong>in</strong>fusion-Ea dyn > 1.06 identified<br />
<strong>fluid</strong> responders with both sensitivity <strong>and</strong><br />
specificity <strong>of</strong> 88.2 %. While await<strong>in</strong>g fur<strong>the</strong>r<br />
validation, <strong>the</strong>se f<strong>in</strong>d<strong>in</strong>gs underscore<br />
<strong>the</strong> potential <strong>of</strong> non<strong>in</strong>vasive arterial pulse<br />
pressure analysis for <strong>the</strong> assessment <strong>of</strong> <strong>fluid</strong><br />
<strong>responsiveness</strong> that appears particularly<br />
well suited for <strong>the</strong> ED.<br />
At this po<strong>in</strong>t, however, <strong>the</strong>se <strong>in</strong>novative<br />
technologies for cont<strong>in</strong>uous advanced<br />
hemodynamic monitor<strong>in</strong>g still need to be<br />
fur<strong>the</strong>r evaluated <strong>in</strong> <strong>the</strong> ED sett<strong>in</strong>g with<br />
regard to <strong>the</strong>ir cl<strong>in</strong>ical applicability <strong>and</strong><br />
<strong>the</strong>ir measurement performance [77, 78].<br />
Conclusions<br />
The correct assessment <strong>of</strong> <strong>the</strong> patient’s<br />
<strong>volume</strong> <strong>status</strong> <strong>and</strong> <strong>fluid</strong> <strong>responsiveness</strong><br />
constitutes a fundamental <strong>and</strong> yet challeng<strong>in</strong>g<br />
task for <strong>the</strong> effective management<br />
<strong>of</strong> a wide variety <strong>of</strong> medical conditions<br />
that physicians encounter <strong>in</strong> <strong>the</strong><br />
ED. In this review, we provide a detailed<br />
guide through a variety <strong>of</strong> methods applicable<br />
<strong>in</strong> <strong>the</strong> ED environment for <strong>the</strong><br />
assessment <strong>of</strong> a patient’s <strong>in</strong>travascular<br />
<strong>volume</strong> <strong>status</strong> <strong>and</strong> <strong>fluid</strong> <strong>responsiveness</strong>.<br />
Based upon history, physical exam<strong>in</strong>ation,<br />
laboratory tests, <strong>and</strong> ultrasound we<br />
propose an algorithm to estimate <strong>the</strong> <strong>in</strong>travascular<br />
<strong>volume</strong> <strong>status</strong> (. Fig. 1). In<br />
addition, we describe <strong>the</strong> functional tests<br />
to assess <strong>fluid</strong> <strong>responsiveness</strong> <strong>and</strong> <strong>the</strong>ir<br />
limitations <strong>in</strong> an ED sett<strong>in</strong>g. In <strong>the</strong> future,<br />
<strong>in</strong>novative non<strong>in</strong>vasive means <strong>of</strong> cont<strong>in</strong>uous<br />
hemodynamic monitor<strong>in</strong>g may allow<br />
advanced hemodynamic monitor<strong>in</strong>g<br />
<strong>in</strong> <strong>the</strong> ED.<br />
Authors’ contributions. C. Maurer was<br />
responsible for <strong>the</strong> conception <strong>and</strong> draft<strong>in</strong>g<br />
<strong>of</strong> <strong>the</strong> review. J.Y. Wagner has made<br />
substantial contributions to <strong>the</strong> conception,<br />
was <strong>in</strong>volved <strong>in</strong> draft<strong>in</strong>g, <strong>and</strong> revised<br />
<strong>the</strong> manuscript for important <strong>in</strong>tellectual<br />
content. R.M. Schmid revised <strong>the</strong> manuscript<br />
for important <strong>in</strong>tellectual content.<br />
B. Saugel was responsible for <strong>the</strong> conception<br />
<strong>and</strong> draft<strong>in</strong>g <strong>of</strong> <strong>the</strong> review. All authors<br />
read <strong>and</strong> approved <strong>the</strong> f<strong>in</strong>al manuscript.<br />
Correspond<strong>in</strong>g address<br />
B. Saugel MD<br />
Department <strong>of</strong> Anes<strong>the</strong>siology, Center <strong>of</strong><br />
Anes<strong>the</strong>siology <strong>and</strong> Intensive Care Medic<strong>in</strong>e,<br />
University Medical Center Hamburg-Eppendorf<br />
Mart<strong>in</strong>istrasse 52, 20246 Hamburg<br />
bernd.saugel@gmx.de<br />
Mediz<strong>in</strong>ische Kl<strong>in</strong>ik - Intensivmediz<strong>in</strong> und Notfallmediz<strong>in</strong> 4 · 2017 |<br />
331
Übersichten<br />
Compliance with<br />
ethics guidel<strong>in</strong>es<br />
Conflict <strong>of</strong> <strong>in</strong>terest. B. Saugel collaborates with<br />
Pulsion Medical Systems SE (Feldkirchen, Germany)<br />
as a member <strong>of</strong> <strong>the</strong> Medical Advisory Board. Saugel<br />
received honoraria for giv<strong>in</strong>g lectures <strong>and</strong> refunds<br />
<strong>of</strong> travel expenses from Pulsion Medical Systems SE<br />
(Feldkirchen, Germany).<br />
Saugel received <strong>in</strong>stitutional research grants, unrestricted<br />
research grants, <strong>and</strong> refunds <strong>of</strong> travel expenses<br />
from Tensys Medical Inc. (San Diego, CA, USA). BS<br />
received honoraria for giv<strong>in</strong>g lectures <strong>and</strong> refunds <strong>of</strong><br />
travel expenses from CNSystems Mediz<strong>in</strong>technik AG<br />
(Graz, Austria).<br />
J.Y. Wagner received <strong>in</strong>stitutional research grants, unrestricted<br />
research grants, <strong>and</strong> refunds <strong>of</strong> travel expenses<br />
from Tensys Medical Inc. (San Diego, CA, USA). J.Y.<br />
Wagner received refunds <strong>of</strong> travel expenses from CN-<br />
Systems Mediz<strong>in</strong>technik AG (Graz, Austria).<br />
For C. Maurer <strong>and</strong> R.M. Schmid <strong>the</strong>re is no conflict <strong>of</strong><br />
<strong>in</strong>terest to disclose.<br />
This article does not conta<strong>in</strong> studies on human or animal<br />
subjects.<br />
References<br />
1. Angus DC, van der Poll T (2013) Severe sepsis <strong>and</strong><br />
septic shock. N Engl J Med 369:840–851<br />
2. Wu BU, Banks PA (2013) Cl<strong>in</strong>ical management <strong>of</strong><br />
patients with acute pancreatitis. Gastroenterology<br />
144:1272–1281<br />
3. Nadeau-Fredette AC, Bouchard J (2013) Fluid management<br />
<strong>and</strong> use <strong>of</strong> diuretics <strong>in</strong> acute kidney <strong>in</strong>jury.<br />
Adv Chronic Kidney Dis 20:45–55<br />
4. Bhave G, Neilson EG (2011) Volume depletion versus<br />
dehydration: how underst<strong>and</strong><strong>in</strong>g <strong>the</strong> difference<br />
can guide <strong>the</strong>rapy. Am J Kidney Dis 58:302–<br />
309<br />
5. V<strong>in</strong>cent JL, De Backer D (2014) Circulatory shock. N<br />
Engl J Med 370:583<br />
6. V<strong>in</strong>cent JL, Ince C, Bakker J (2012) Cl<strong>in</strong>ical review:<br />
circulatory shock—an update: a tribute to Pr<strong>of</strong>essor<br />
Max Harry Weil. Crit Care 16:239<br />
7. Gross CR, L<strong>in</strong>dquist RD, Woolley AC, Granieri R, Allard<br />
K, Webster B (1992) Cl<strong>in</strong>ical <strong>in</strong>dicators <strong>of</strong> dehydration<br />
severity <strong>in</strong> elderly patients. J Emerg Med<br />
10:267–274<br />
8. Stephan F, Flahault A, Dieudonne N, Holl<strong>and</strong>e J,<br />
Paillard F, Bonnet F (2001) Cl<strong>in</strong>ical evaluation <strong>of</strong> circulat<strong>in</strong>g<br />
blood <strong>volume</strong> <strong>in</strong> critically ill patients—<br />
contribution <strong>of</strong> a cl<strong>in</strong>ical scor<strong>in</strong>g system. Br J Anaesth<br />
86:754–762<br />
9. Koziol-McLa<strong>in</strong> J, Lowenste<strong>in</strong> SR, Fuller B (1991) Orthostatic<br />
vital signs <strong>in</strong> <strong>emergency</strong> <strong>department</strong> patients.<br />
Ann Emerg Med 20:606–610<br />
10. McGee S, Abernethy WB III, Simel DL (1999) The rational<br />
cl<strong>in</strong>ical exam<strong>in</strong>ation. Is this patient hypovolemic?<br />
JAMA 281:1022–1029<br />
11. Wang CS, FitzGerald JM, Schulzer M, Mak E, Ayas<br />
NT (2005) Does this dyspneic patient <strong>in</strong> <strong>the</strong> <strong>emergency</strong><br />
<strong>department</strong> have congestive heart failure?<br />
JAMA 294:1944–1956<br />
12. Badgett RG, Lucey CR, Mulrow CD (1997) Can <strong>the</strong><br />
cl<strong>in</strong>ical exam<strong>in</strong>ation diagnose left-sided heart failure<br />
<strong>in</strong> adults? JAMA 277:1712–1719<br />
13. Killip T III, Kimball JT (1967) Treatment <strong>of</strong> myocardial<br />
<strong>in</strong>farction <strong>in</strong> a coronary care unit. A two<br />
year experience with 250 patients. Am J Cardiol<br />
20:457–464<br />
14. Saugel B, R<strong>in</strong>gmaier S, Holzapfel K, Schuster T, Phillip<br />
V, Schmid RM et al (2011) Physical exam<strong>in</strong>ation,<br />
central venous pressure, <strong>and</strong> chest radiography for<br />
<strong>the</strong> prediction <strong>of</strong> transpulmonary <strong>the</strong>rmodilutionderived<br />
hemodynamic parameters <strong>in</strong> critically ill<br />
patients: a prospective trial. J Crit Care 26:402–410<br />
15. Chung HM, Kluge R, Schrier RW, Anderson RJ<br />
(1987) Cl<strong>in</strong>ical assessment <strong>of</strong> extracellular <strong>fluid</strong><br />
<strong>volume</strong> <strong>in</strong> hyponatremia. Am J Med 83:905–9<strong>08</strong><br />
16. Dossetor JB (1966) Creat<strong>in</strong><strong>in</strong>emia versus uremia.<br />
The relative significance <strong>of</strong> blood urea nitrogen<br />
<strong>and</strong> serum creat<strong>in</strong><strong>in</strong>e concentrations <strong>in</strong> azotemia.<br />
Ann Intern Med 65:1287–1299<br />
17. Schrier RW (2007) Decreased effective blood <strong>volume</strong><br />
<strong>in</strong> edematous disorders: what does this<br />
mean? J Am Soc Nephrol 18:2028–2031<br />
18. Swedko PJ, Clark HD, Paramsothy K, Akbari A<br />
(2003) Serum creat<strong>in</strong><strong>in</strong>e is an <strong>in</strong>adequate screen<strong>in</strong>g<br />
test for renal failure <strong>in</strong> elderly patients. Arch Intern<br />
Med 163:356–360<br />
19. Carvounis CP, Nisar S, Guro-Razuman S (2002) Significance<br />
<strong>of</strong> <strong>the</strong> fractional excretion <strong>of</strong> urea <strong>in</strong> <strong>the</strong><br />
differential diagnosis <strong>of</strong> acute renal failure. Kidney<br />
Int 62:2223–2229<br />
20. Pep<strong>in</strong> MN, Bouchard J, Legault L, Ethier J (2007)<br />
Diagnostic performance <strong>of</strong> fractional excretion<br />
<strong>of</strong> urea <strong>and</strong> fractional excretion <strong>of</strong> sodium <strong>in</strong> <strong>the</strong><br />
evaluations <strong>of</strong> patients with acute kidney <strong>in</strong>jury<br />
with or without diuretic treatment. Am J Kidney<br />
Dis 50:566–573<br />
21. Wo CC, Shoemaker WC, Appel PL, Bishop MH,<br />
Kram HB, Hard<strong>in</strong> E (1993) Unreliability <strong>of</strong> blood<br />
pressure <strong>and</strong> heart rate to evaluate cardiac output<br />
<strong>in</strong> <strong>emergency</strong> resuscitation <strong>and</strong> critical illness. Crit<br />
Care Med 21:218–223<br />
22. Kjell<strong>and</strong> CB, Djogovic D (2010) The role <strong>of</strong> serum<br />
lactate <strong>in</strong> <strong>the</strong> acute care sett<strong>in</strong>g. J Intensive Care<br />
Med 25:286–300<br />
23. Howell MD, Donn<strong>in</strong>o M, Clardy P, Talmor D, Shapiro<br />
NI (2007) Occult hypoperfusion <strong>and</strong> mortality <strong>in</strong><br />
patients with suspected <strong>in</strong>fection. Intensive Care<br />
Med 33:1892–1899<br />
24. Nguyen HB, Rivers EP, Knoblich BP, Jacobsen G,<br />
Muzz<strong>in</strong> A, Ressler JA et al (2004) Early lactate<br />
clearance is associated with improved outcome<br />
<strong>in</strong> severe sepsis <strong>and</strong> septic shock. Crit Care Med<br />
32:1637–1642<br />
25. Rudski LG, Lai WW, Afilalo J, Hua L, H<strong>and</strong>schumacher<br />
MD, Ch<strong>and</strong>rasekaran K et al (2010) Guidel<strong>in</strong>es<br />
for <strong>the</strong> echocardiographic assessment <strong>of</strong> <strong>the</strong><br />
right heart <strong>in</strong> adults: a report from <strong>the</strong> American<br />
Society <strong>of</strong> Echocardiography endorsed by <strong>the</strong> European<br />
Association <strong>of</strong> Echocardiography, a registered<br />
branch <strong>of</strong> <strong>the</strong> European Society <strong>of</strong> Cardiology,<br />
<strong>and</strong> <strong>the</strong> Canadian Society <strong>of</strong> Echocardiography.<br />
J Am Soc Echocardiogr 23:685–713 (quiz 86–8)<br />
26. Feissel M, Michard F, Faller JP, Teboul JL (2004) The<br />
respiratory variation <strong>in</strong> <strong>in</strong>ferior vena cava diameter<br />
as a guide to <strong>fluid</strong> <strong>the</strong>rapy. Intensive Care Med<br />
30:1834–1837<br />
27. Weekes AJ, Tassone HM, Babcock A, Quirke DP,<br />
Norton HJ, Jayarama K et al (2011) Comparison<br />
<strong>of</strong> serial qualitative <strong>and</strong> quantitative assessments<br />
<strong>of</strong> caval <strong>in</strong>dex <strong>and</strong> left ventricular systolic function<br />
dur<strong>in</strong>g early <strong>fluid</strong> resuscitation <strong>of</strong> hypotensive<br />
<strong>emergency</strong> <strong>department</strong> patients. Acad Emerg Med<br />
18:912–921<br />
28. Tetsuka T, Ando Y, Ono S, Asano Y (1995) Change <strong>in</strong><br />
<strong>in</strong>ferior vena caval diameter detected by ultrasonography<br />
dur<strong>in</strong>g <strong>and</strong> after hemodialysis. ASAIO J<br />
41:105–110<br />
29. Fields JM, Lee PA, Jenq KY, Mark DG, Panebianco<br />
NL, Dean AJ (2011) The <strong>in</strong>terrater reliability <strong>of</strong> <strong>in</strong>ferior<br />
vena cava ultrasound by bedside cl<strong>in</strong>ician sonographers<br />
<strong>in</strong> <strong>emergency</strong> <strong>department</strong> patients.<br />
Acad Emerg Med 18:98–101<br />
30. Yanagawa Y, Nishi K, Sakamoto T, Okada Y (2005)<br />
Early diagnosis <strong>of</strong> hypovolemic shock by sonographic<br />
measurement <strong>of</strong> <strong>in</strong>ferior vena cava <strong>in</strong> trauma<br />
patients. J Trauma 58:825–829<br />
31. Yanagawa Y, Sakamoto T, Okada Y (2007) Hypovolemic<br />
shock evaluated by sonographic measurement<br />
<strong>of</strong> <strong>the</strong> <strong>in</strong>ferior vena cava dur<strong>in</strong>g resuscitation<br />
<strong>in</strong> trauma patients. J Trauma 63:1245–1248 (discussion<br />
8)<br />
32. Sefidbakht S, Assadsangabi R, Abbasi HR,<br />
Nabavizadeh A (2007) Sonographic measurement<br />
<strong>of</strong> <strong>the</strong> <strong>in</strong>ferior vena cava as a predictor <strong>of</strong> shock <strong>in</strong><br />
trauma patients. Emerg Radiol 14:181–185<br />
33. Corl K, Napoli AM, Gard<strong>in</strong>er F (2012) Bedside sonographic<br />
measurement <strong>of</strong> <strong>the</strong> <strong>in</strong>ferior vena cava caval<br />
<strong>in</strong>dex is a poor predictor <strong>of</strong> <strong>fluid</strong> <strong>responsiveness</strong><br />
<strong>in</strong> <strong>emergency</strong> <strong>department</strong> patients. Emerg<br />
Med Australas 24:534–539<br />
34. Neskovic AN, Hagendorff A, Lancellotti P, Guarrac<strong>in</strong>o<br />
F, Varga A, Cosyns B et al (2013) Emergency<br />
echocardiography: <strong>the</strong> European Association<br />
<strong>of</strong> Cardiovascular Imag<strong>in</strong>g recommendations. Eur<br />
Heart J Cardiovasc Imag<strong>in</strong>g 14:1–11<br />
35. Lancellotti P, Price S, Edvardsen T, Cosyns B, Neskovic<br />
AN, Dulgheru R et al (2015) The use <strong>of</strong> echocardiography<br />
<strong>in</strong> acute cardiovascular care: recommendations<br />
<strong>of</strong> <strong>the</strong> European Association <strong>of</strong> Cardiovascular<br />
Imag<strong>in</strong>g <strong>and</strong> <strong>the</strong> Acute Cardiovascular<br />
Care Association. Eur Heart J Acute Cardiovasc<br />
Care 4:3–5<br />
36. Levitov A, Marik PE (2012) Echocardiographic assessment<br />
<strong>of</strong> preload <strong>responsiveness</strong> <strong>in</strong> critically ill<br />
patients. Cardiol Res Pract 2012:819696<br />
37. Ely EW, Haponik EF (2002) Us<strong>in</strong>g <strong>the</strong> chest radiograph<br />
to determ<strong>in</strong>e <strong>in</strong>travascular <strong>volume</strong> <strong>status</strong>:<br />
<strong>the</strong> role <strong>of</strong> vascular pedicle width. Chest 121:942–<br />
950<br />
38. Halper<strong>in</strong> BD, Feeley TW, Mihm FG, Chiles C, Guthaner<br />
DF, Blank NE (1985) Evaluation <strong>of</strong> <strong>the</strong> portable<br />
chest roentgenogram for quantitat<strong>in</strong>g extravascular<br />
lung water <strong>in</strong> critically ill adults. Chest 88:649–<br />
652<br />
39. Milne EN, Pistolesi M, M<strong>in</strong>iati M, Giunt<strong>in</strong>i C (1984)<br />
The vascular pedicle <strong>of</strong> <strong>the</strong> heart <strong>and</strong> <strong>the</strong> vena azygos.<br />
Part I: <strong>the</strong> normal subject. Radiology 152:1–8<br />
40. Ely EW, Smith AC, Chiles C, Aqu<strong>in</strong>o SL, Harle TS, Evans<br />
GW et al (2001) Radiologic determ<strong>in</strong>ation <strong>of</strong><br />
<strong>in</strong>travascular <strong>volume</strong> <strong>status</strong> us<strong>in</strong>g portable, digital<br />
chest radiography: a prospective <strong>in</strong>vestigation <strong>in</strong><br />
100 patients. Crit Care Med 29:1502–1512<br />
41. Theodoro D, Owens PL, Olsen MA, Fraser V (2014)<br />
Rates <strong>and</strong> tim<strong>in</strong>g <strong>of</strong> central venous cannulation<br />
among patients with sepsis <strong>and</strong> respiratory arrest<br />
admitted by <strong>the</strong> <strong>emergency</strong> <strong>department</strong>. Crit Care<br />
Med 42:554–564<br />
42. Reade MC, Huang DT, Bell D, Coats TJ, Cross AM,<br />
Moran JL et al (2010) Variability <strong>in</strong> management <strong>of</strong><br />
early severe sepsis. Emerg Med J 27:110–115<br />
43. Yealy DM, Kellum JA, Huang DT, Barnato AE, Weissfeld<br />
LA, Pike F et al (2014) A r<strong>and</strong>omized trial <strong>of</strong><br />
protocol-based care for early septic shock. N Engl J<br />
Med 370:1683–1693<br />
332 | Mediz<strong>in</strong>ische Kl<strong>in</strong>ik - Intensivmediz<strong>in</strong> und Notfallmediz<strong>in</strong> 4 · 2017
44. Peake SL, Delaney A, Bailey M, Bellomo R, Cameron<br />
PA, Cooper DJ et al (2014) Goal-directed resuscitation<br />
for patients with early septic shock. N Engl<br />
J Med 371:1496–1506<br />
45. Michard F, Alaya S, Zarka V, Bahloul M, Richard C,<br />
Teboul JL (2003) Global end-diastolic <strong>volume</strong> as an<br />
<strong>in</strong>dicator <strong>of</strong> cardiac preload <strong>in</strong> patients with septic<br />
shock. Chest 124:1900–19<strong>08</strong><br />
46. Marik PE, Baram M, Vahid B (20<strong>08</strong>) Does central venous<br />
pressure predict <strong>fluid</strong> <strong>responsiveness</strong>? A systematic<br />
review <strong>of</strong> <strong>the</strong> literature <strong>and</strong> <strong>the</strong> tale <strong>of</strong> seven<br />
mares. Chest 134:172–178<br />
47. Marik PE, Cavallazzi R (2013) Does <strong>the</strong> central venous<br />
pressure predict <strong>fluid</strong> <strong>responsiveness</strong>? An updated<br />
meta-analysis <strong>and</strong> a plea for some common<br />
sense. Crit Care Med 41:1774–1781<br />
48. Cannesson M, Rams<strong>in</strong>gh D, R<strong>in</strong>ehart J, Demirjian<br />
A, Vu T, Vakharia S et al (2015) Perioperative goaldirected<br />
<strong>the</strong>rapy <strong>and</strong> postoperative outcomes <strong>in</strong><br />
patients undergo<strong>in</strong>g high-risk abdom<strong>in</strong>al surgery:<br />
a historical-prospective, comparative effectiveness<br />
study. Crit Care 19:261<br />
49. Monnet X, Rienzo M, Osman D, Anguel N, Richard<br />
C, P<strong>in</strong>sky MR et al (2006) Passive leg rais<strong>in</strong>g predicts<br />
<strong>fluid</strong> <strong>responsiveness</strong> <strong>in</strong> <strong>the</strong> critically ill. Crit<br />
Care Med 34:1402–1407<br />
50. Jabot J, Teboul JL, Richard C, Monnet X (2009) Passive<br />
leg rais<strong>in</strong>g for predict<strong>in</strong>g <strong>fluid</strong> <strong>responsiveness</strong>:<br />
importance <strong>of</strong> <strong>the</strong> postural change. Intensive Care<br />
Med 35:85–90<br />
51. Monnet X, Teboul JL (20<strong>08</strong>) Passive leg rais<strong>in</strong>g. Intensive<br />
Care Med 34:659–663<br />
52. Preau S, Saulnier F, Dewavr<strong>in</strong> F, Durocher A, Chagnon<br />
JL (2010) Passive leg rais<strong>in</strong>g is predictive <strong>of</strong><br />
<strong>fluid</strong> <strong>responsiveness</strong> <strong>in</strong> spontaneously breath<strong>in</strong>g<br />
patients with severe sepsis or acute pancreatitis.<br />
Crit Care Med 38:819–825<br />
53. Teboul JL, Monnet X (20<strong>08</strong>) Prediction <strong>of</strong> <strong>volume</strong><br />
<strong>responsiveness</strong> <strong>in</strong> critically ill patients with spontaneous<br />
breath<strong>in</strong>g activity. Curr Op<strong>in</strong> Crit Care<br />
14:334–339<br />
54. Monnet X, Teboul JL (2015) Passive leg rais<strong>in</strong>g: five<br />
rules, not a drop <strong>of</strong> <strong>fluid</strong>! Crit Care 19:18<br />
55. Cavallaro F, S<strong>and</strong>roni C, Marano C, La Torre G, Mannocci<br />
A, De Waure C et al (2010) Diagnostic accuracy<br />
<strong>of</strong> passive leg rais<strong>in</strong>g for prediction <strong>of</strong> <strong>fluid</strong> <strong>responsiveness</strong><br />
<strong>in</strong> adults: systematic review <strong>and</strong> meta-analysis<br />
<strong>of</strong> cl<strong>in</strong>ical studies. Intensive Care Med<br />
36:1475–1483<br />
56. AWMF (2014) Intravasale Volumen<strong>the</strong>rapie beim<br />
Erwachsenen. Leitl<strong>in</strong>iendetailansicht. www.awmf.<br />
org/leitl<strong>in</strong>ien/detail/ll/001-020.html. Accessed 12<br />
Oct 2015<br />
57. Lakhal K, Ehrmann S, Benzekri-Lefevre D, Runge I,<br />
Legras A, Dequ<strong>in</strong> PF et al (2012) Brachial cuff measurements<br />
<strong>of</strong> blood pressure dur<strong>in</strong>g passive leg<br />
rais<strong>in</strong>g for <strong>fluid</strong> <strong>responsiveness</strong> prediction. Ann Fr<br />
Anesth Reanim 31:e67–e72<br />
58. Lamia B, Ochagavia A, Monnet X, Chemla D, Richard<br />
C, Teboul JL (2007) Echocardiographic prediction<br />
<strong>of</strong> <strong>volume</strong> <strong>responsiveness</strong> <strong>in</strong> critically ill patients<br />
with spontaneously breath<strong>in</strong>g activity. Intensive<br />
Care Med 33:1125–1132<br />
59. Delerme S, Renault R, Le Manach Y, Lvovschi V,<br />
Bendahou M, Riou B et al (2007) Variations <strong>in</strong> pulse<br />
oximetry plethysmographic waveform amplitude<br />
<strong>in</strong>duced by passive leg rais<strong>in</strong>g <strong>in</strong> spontaneously<br />
breath<strong>in</strong>g volunteers. Am J Emerg Med 25:637–<br />
642<br />
60. Cecconi M, Parsons AK, Rhodes A (2011) What is a<br />
<strong>fluid</strong> challenge? Curr Op<strong>in</strong> Crit Care 17:290–295<br />
61. V<strong>in</strong>cent JL, Weil MH (2006) Fluid challenge revisited.<br />
Crit Care Med 34:1333–1337<br />
62. Cherpanath TG, Aarts LP, Groeneveld JA, Geerts BF<br />
(2014) Def<strong>in</strong><strong>in</strong>g <strong>fluid</strong> <strong>responsiveness</strong>: a guide to<br />
patient-tailored <strong>volume</strong> titration. J Cardiothorac<br />
Vasc Anesth 28:745–754<br />
63. Michard F, Teboul JL (2002) Predict<strong>in</strong>g <strong>fluid</strong> <strong>responsiveness</strong><br />
<strong>in</strong> ICU patients: a critical analysis <strong>of</strong><br />
<strong>the</strong> evidence. Chest 121:2000–20<strong>08</strong><br />
64. Muller L, Louart G, Teboul JL, Mahamat A, Polge A,<br />
Bert<strong>in</strong>chant JP et al (2009) Could B-type Natriuretic<br />
Peptide (BNP) plasma concentration be useful to<br />
predict <strong>fluid</strong> <strong>responsiveness</strong> [corrected] <strong>in</strong> critically<br />
ill patients with acute circulatory failure? Ann Fr<br />
Anesth Reanim 28:531–536<br />
65. Araghi A, B<strong>and</strong>er JJ, Guzman JA (2006) Arterial<br />
blood pressure monitor<strong>in</strong>g <strong>in</strong> overweight critically<br />
ill patients: <strong>in</strong>vasive or non<strong>in</strong>vasive? Crit Care<br />
10:R64<br />
66. Anastas ZM, Jimerson E, Garolis S (20<strong>08</strong>) Comparison<br />
<strong>of</strong> non<strong>in</strong>vasive blood pressure measurements<br />
<strong>in</strong> patients with atrial fibrillation. J Cardiovasc Nurs<br />
23:519–524 (quiz 25–26)<br />
67. Lehman LW, Saeed M, Talmor D, Mark R, Malhotra<br />
A (2013) Methods <strong>of</strong> blood pressure measurement<br />
<strong>in</strong> <strong>the</strong> ICU. Crit Care Med 41:34–40<br />
68. Wagner JY, Prantner JS, Meidert AS, Hapfelmeier<br />
A, Schmid RM, Saugel B (2014) Non<strong>in</strong>vasive cont<strong>in</strong>uous<br />
versus <strong>in</strong>termittent arterial pressure monitor<strong>in</strong>g:<br />
evaluation <strong>of</strong> <strong>the</strong> vascular unload<strong>in</strong>g technique<br />
(CNAP device) <strong>in</strong> <strong>the</strong> <strong>emergency</strong> <strong>department</strong>.<br />
Sc<strong>and</strong> J Trauma Resusc Emerg Med 22:8<br />
69. Nowak RM, Sen A, Garcia AJ, Wilkie H, Yang JJ,<br />
Nowak MR et al (2011) Non<strong>in</strong>vasive cont<strong>in</strong>uous or<br />
<strong>in</strong>termittent blood pressure <strong>and</strong> heart rate patient<br />
monitor<strong>in</strong>g <strong>in</strong> <strong>the</strong> ED. Am J Emerg Med 29:782–<br />
789<br />
70. Saugel B, Dueck R, Wagner JY (2014) Measurement<br />
<strong>of</strong> blood pressure. Best Pract Res Cl<strong>in</strong> Anaes<strong>the</strong>siol<br />
28:309–322<br />
71. Saugel B, Meidert AS, Hapfelmeier A, Eyer F,<br />
Schmid RM, Huber W (2013) Non-<strong>in</strong>vasive cont<strong>in</strong>uous<br />
arterial pressure measurement based on radial<br />
artery tonometry <strong>in</strong> <strong>the</strong> <strong>in</strong>tensive care unit:<br />
a method comparison study us<strong>in</strong>g <strong>the</strong> T-L<strong>in</strong>e TL-<br />
200pro device. Br J Anaesth 111:185–190<br />
72. Meidert AS, Huber W, Muller JN, Sch<strong>of</strong>thaler M,<br />
Hapfelmeier A, Langwieser N et al (2014) Radial<br />
artery applanation tonometry for cont<strong>in</strong>uous<br />
non-<strong>in</strong>vasive arterial pressure monitor<strong>in</strong>g <strong>in</strong> <strong>in</strong>tensive<br />
care unit patients: comparison with <strong>in</strong>vasively<br />
assessed radial arterial pressure. Br J Anaesth<br />
112:521–528<br />
73. Saugel B, Meidert AS, Langwieser N, Wagner JY,<br />
Fassio F, Hapfelmeier A et al (2014) An autocalibrat<strong>in</strong>g<br />
algorithm for non-<strong>in</strong>vasive cardiac output<br />
determ<strong>in</strong>ation based on <strong>the</strong> analysis <strong>of</strong> an arterial<br />
pressure waveform recorded with radial artery<br />
applanation tonometry: a pro<strong>of</strong> <strong>of</strong> concept pilot<br />
analysis. J Cl<strong>in</strong> Monit Comput 28:357–362<br />
74. Wagner JY, Sarwari H, Schon G, Kubik M, Kluge S,<br />
Reichenspurner H et al (2015) Radial artery applanation<br />
tonometry for cont<strong>in</strong>uous non<strong>in</strong>vasive cardiac<br />
output measurement: a comparison with <strong>in</strong>termittent<br />
pulmonary artery <strong>the</strong>rmodilution <strong>in</strong> patients<br />
after cardiothoracic surgery. Crit Care Med<br />
43:1423–1428<br />
75. Saugel B, Cecconi M, Wagner JY, Reuter DA (2015)<br />
Non<strong>in</strong>vasive cont<strong>in</strong>uous cardiac output monitor<strong>in</strong>g<br />
<strong>in</strong> perioperative <strong>and</strong> <strong>in</strong>tensive care medic<strong>in</strong>e.<br />
Br J Anaesth 114:562–575<br />
76. Cecconi M, Monge Garcia MI, Gracia Romero M,<br />
Mell<strong>in</strong>gh<strong>of</strong>f J, Cali<strong>and</strong>ro F, Grounds RM et al (2015)<br />
The use <strong>of</strong> pulse pressure variation <strong>and</strong> stroke <strong>volume</strong><br />
variation <strong>in</strong> spontaneously breath<strong>in</strong>g patients<br />
to assess dynamic arterial elastance <strong>and</strong> to predict<br />
arterial pressure response to <strong>fluid</strong> adm<strong>in</strong>istration.<br />
Anesth Analg 120(1):76–84<br />
77. Saugel B, Reuter DA (2014) Are we ready for <strong>the</strong><br />
age <strong>of</strong> non-<strong>in</strong>vasive haemodynamic monitor<strong>in</strong>g?<br />
Br J Anaesth 113:340–343<br />
78. Wagner JY, Saugel B (2015) When should we adopt<br />
cont<strong>in</strong>uous non<strong>in</strong>vasive hemodynamic monitor<strong>in</strong>g<br />
technologies <strong>in</strong>to cl<strong>in</strong>ical rout<strong>in</strong>e? J Cl<strong>in</strong> Monit<br />
Comput 29:1–3<br />
Mediz<strong>in</strong>ische Kl<strong>in</strong>ik - Intensivmediz<strong>in</strong> und Notfallmediz<strong>in</strong> 4 · 2017 |<br />
333