2017 HCHB_digital
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Osteoporosis<br />
Osteoporosis (meaning “porous bones”) is a common bone disease that<br />
leads to an increased risk of fracture. One in three women and one in five<br />
men over the age of 50 are affected by osteoporosis.<br />
Bone is a living tissue made up of proteins and minerals, such as calcium and<br />
phosphorus. Throughout life, bone is constantly being broken down and renewed.<br />
Bone density – the amount of bone tissue in a certain volume of bone – reaches a<br />
peak between 18 and 25 years of age. Higher peak bone masses are associated<br />
with a lower risk of fracture or osteoporosis later in life. Women lose bone density<br />
more quickly after menopause due to a decrease in oestrogen levels. Regular<br />
weight-bearing exercise and an adequate dietary intake of calcium and other<br />
minerals is also needed to maintain good bone density in addition to oestrogen<br />
in women and testosterone in men.<br />
Osteoporosis occurs when bone breaks down faster than it rebuilds. Although<br />
bones remain the same size, they become thinner and more brittle. Osteoporosis<br />
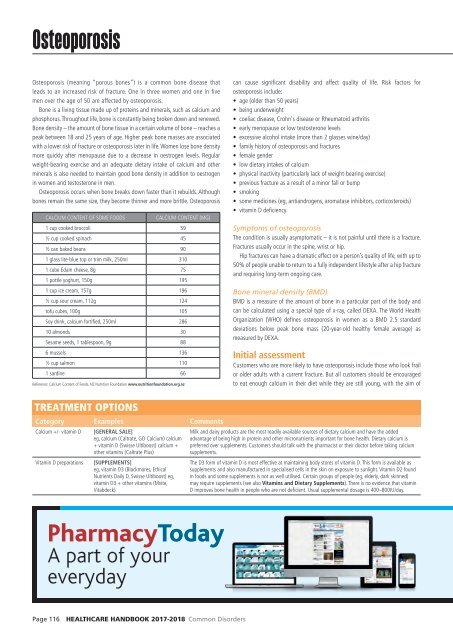
CALCIUM CONTENT OF SOME FOODS<br />
CALCIUM CONTENT (MG)<br />
1 cup cooked broccoli 59<br />
½ cup cooked spinach 45<br />
½ can baked beans 90<br />
1 glass lite-blue top or trim milk, 250ml 310<br />
1 cube Edam cheese, 8g 75<br />
1 pottle yoghurt, 150g 195<br />
1 cup ice cream, 157g 196<br />
½ cup sour cream, 112g 124<br />
tofu cubes, 100g 105<br />
Soy drink, calcium fortified, 250ml 286<br />
10 almonds 30<br />
Sesame seeds, 1 tablespoon, 9g 88<br />
6 mussels 136<br />
½ cup salmon 110<br />
1 sardine 66<br />
Reference: Calcium Content of Foods. NZ Nutrition Foundation www.nutritionfoundation.org.nz<br />
can cause significant disability and affect quality of life. Risk factors for<br />
osteoporosis include:<br />
• age (older than 50 years)<br />
• being underweight<br />
• coeliac disease, Crohn's disease or Rheumatoid arthritis<br />
• early menopause or low testosterone levels<br />
• excessive alcohol intake (more than 2 glasses wine/day)<br />
• family history of osteoporosis and fractures<br />
• female gender<br />
• low dietary intakes of calcium<br />
• physical inactivity (particularly lack of weight-bearing exercise)<br />
• previous fracture as a result of a minor fall or bump<br />
• smoking<br />
• some medicines (eg, antiandrogens, aromatase inhibitors, corticosteroids)<br />
• vitamin D deficiency.<br />
Symptoms of osteoporosis<br />
The condition is usually asymptomatic – it is not painful until there is a fracture.<br />
Fractures usually occur in the spine, wrist or hip.<br />
Hip fractures can have a dramatic effect on a person’s quality of life, with up to<br />
50% of people unable to return to a fully independent lifestyle after a hip fracture<br />
and requiring long-term ongoing care.<br />
Bone mineral density (BMD)<br />
BMD is a measure of the amount of bone in a particular part of the body and<br />
can be calculated using a special type of x-ray, called DEXA. The World Health<br />
Organization (WHO) defines osteoporosis in women as a BMD 2.5 standard<br />
deviations below peak bone mass (20-year-old healthy female average) as<br />
measured by DEXA.<br />
Initial assessment<br />
Customers who are more likely to have osteoporosis include those who look frail<br />
or older adults with a current fracture. But all customers should be encouraged<br />
to eat enough calcium in their diet while they are still young, with the aim of<br />
TREATMENT OPTIONS<br />
Category Examples Comments<br />
Calcium +/- vitamin D<br />
Vitamin D preparations<br />
[GENERAL SALE]<br />
eg, calcium (Caltrate, GO Calcium) calcium<br />
+ vitamin D (Swisse Ultiboost) calcium +<br />
other vitamins (Caltrate Plus)<br />
[SUPPLEMENTS]<br />
eg, vitamin D3 (Blackmores, Ethical<br />
Nutrients Daily D, Swisse Ultiboost) eg,<br />
vitamin D3 + other vitamins (Mvite,<br />
Vitabdeck)<br />
Milk and dairy products are the most readily available sources of dietary calcium and have the added<br />
advantage of being high in protein and other micronutrients important for bone health. Dietary calcium is<br />
preferred over supplements. Customers should talk with the pharmacist or their doctor before taking calcium<br />
supplements.<br />
The D3 form of vitamin D is most effective at maintaining body stores of vitamin D. This form is available as<br />
supplements and also manufactured in specialised cells in the skin on exposure to sunlight. Vitamin D2 found<br />
in foods and some supplements is not as well utilised. Certain groups of people (eg, elderly, dark skinned)<br />
may require supplements (see also Vitamins and Dietary Supplements). There is no evidence that vitamin<br />
D improves bone health in people who are not deficient. Usual supplemental dosage is 400–800IU/day.<br />
PharmacyToday<br />
A part of your<br />
everyday<br />
Page 116 HEALTHCARE HANDBOOK <strong>2017</strong>-2018 Common Disorders