You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Greenlane ups low<br />
vision services<br />
The low vision (LV) clinic at Greenlane<br />
Clinical Centre has recently welcomed<br />
two new optometrists to its team. Deepa<br />
Kumar and Deborah Chan, have joined Sandy<br />
Grant, LV clinic coordinator and therapist, to<br />
provide a multi-disciplinary low vision service<br />
to patients referred by eye health specialists,<br />
general practitioners, the Blind Foundation and<br />
other ADHB departments.<br />
The most common referrals are for patients<br />
with macular degeneration (MD) and<br />
glaucoma, although the clinic will accept<br />
anyone with functional vision issues, said<br />
Grant.<br />
Patients seen at early stages of MD often<br />
identify reading, handwriting and glare issues<br />
as their main difficulties, while patients with<br />
glaucoma, retinitis pigmentosa, hemianopias<br />
or monocular vision may experience mobility<br />
and reading issues. Other visual concerns<br />
highlighted in the assessment are also<br />
addressed through LV strategies such as<br />
eccentric viewing, low vision aids, both optical<br />
and non-optical (eg. magnifiers, task lamps,<br />
signature guides), basic training with aids or<br />
sighted-guide, information, peer support or<br />
referrals, such as Blind Foundation membership.<br />
Early intervention often alleviates many<br />
patients and helps the patient develop coping<br />
mechanisms, said Grant.<br />
The low vision clinic runs Tuesday and<br />
Thursday afternoons and on average about<br />
four patients per clinic are seen. Wednesday<br />
afternoons is a therapist-only clinic, though<br />
Grant said she hopes to add another fullservice<br />
clinic in the near future.<br />
Patients referred to the clinic are interviewed<br />
first by Grant and then the optometrist,<br />
who refracts the patient and determines<br />
magnification requirements. Follow-up<br />
appointments are often required, or patients<br />
can self-refer back should they feel their vision<br />
has deteriorated.<br />
Originally from Canada, and trained in<br />
rehabilitation teaching, orientation and<br />
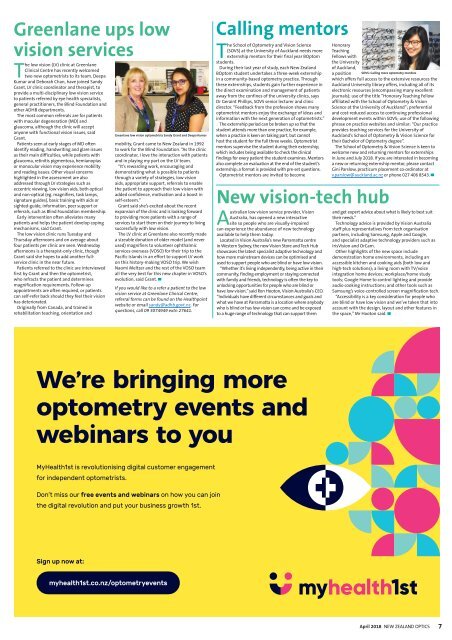
Greenlane low vision optometrists Sandy Grant and Deepa Kumar<br />
mobility, Grant came to New Zealand in 1992<br />
to work for the Blind Foundation. “As the clinic<br />
coordinator, I love the interaction with patients<br />
and in playing my part on the LV team.<br />
“It’s rewarding work, encouraging and<br />
demonstrating what is possible to patients<br />
through a variety of strategies, low vision<br />
aids, appropriate support, referrals to enable<br />
the patient to approach their low vision with<br />
added confidence, motivation and a boost in<br />
self-esteem.”<br />
Grant said she’s excited about the recent<br />
expansion of the clinic and is looking forward<br />
to providing more patients with a range of<br />
services to start them on their journey to living<br />
successfully with low vision.<br />
The LV clinic at Greenlane also recently made<br />
a sizeable donation of older model (and never<br />
used) magnifiers to volunteer ophthalmic<br />
services overseas (VOSO) for their trip to the<br />
Pacific Islands in an effort to support LV work<br />
on this history-making VOSO trip. We wish<br />
Naomi Meltzer and the rest of the VOSO team<br />
all the very best for this new chapter in VOSO’s<br />
evolution, said Grant. ▀<br />
If you would like to a refer a patient to the low<br />
vision service at Greenlane Clinical Centre,<br />
referral forms can be found on the Healthpoint<br />
website or email sandy@adhb.govt.nz. For<br />
questions, call 09 3074949 extn 27641.<br />
Calling mentors<br />
The School of Optometry and Vision Science<br />
(SOVS) at the University of Auckland needs more<br />
externship mentors for their final year BOptom<br />
students.<br />
During their last year of study, each New Zealand<br />
BOptom student undertakes a three-week externship<br />
in a community-based optometry practice. Through<br />
these externships, students gain further experience in<br />
the direct examination and management of patients<br />
away from the confines of the university clinics, says<br />
Dr Geraint Phillips, SOVS senior lecturer and clinic<br />
director. “Feedback from the profession shows many<br />
optometrist mentors enjoy the exchange of ideas and<br />
information with the next generation of optometrists.”<br />
The externship period can be broken up so that the<br />
student attends more than one practice, for example,<br />
when a practice is keen on taking part, but cannot<br />
host the student for the full three weeks. Optometrist<br />
mentors supervise the student during their externship,<br />
which includes being available to check the clinical<br />
findings for every patient the student examines. Mentors<br />
also complete an evaluation at the end of the student’s<br />
externship; a format is provided with pre-set questions.<br />
Optometrist mentors are invited to become<br />
New vision-tech hub<br />
Australian low vision service provider, Vision<br />
Australia, has opened a new interactive<br />
site so people who are visually-impaired<br />
can experience the abundance of new technology<br />
available to help them today.<br />
Located in Vision Australia’s new Parramatta centre<br />
in Western Sydney, the new Vision Store and Tech Hub<br />
showcases the latest specialist adaptive technology and<br />
how more mainstream devices can be optimised and<br />
used to support people who are blind or have low vision.<br />
“Whether it’s living independently, being active in their<br />
community, finding employment or staying connected<br />
with family and friends, technology is often the key to<br />
unlocking opportunities for people who are blind or<br />
have low vision,” said Ron Hooton, Vision Australia’s CEO.<br />
“Individuals have different circumstances and goals and<br />
what we have at Parramatta is a location where anybody<br />
who is blind or has low vision can come and be exposed<br />
to a huge range of technology that can support them<br />
Honorary<br />
Teaching<br />
Fellows with<br />
the University<br />
of Auckland,<br />
a position SOVS: Calling more optometry mentors<br />
which offers full access to the extensive resources the<br />
Auckland University library offers, including all of its<br />
electronic resources (encompassing many excellent<br />
journals); use of the title “Honorary Teaching Fellow<br />
affiliated with the School of Optometry & Vision<br />
Science at the University of Auckland”; preferential<br />
and cost-reduced access to continuing professional<br />
development events within SOVS; use of the following<br />
phrase on practice websites and similar: “Our practice<br />
provides teaching services for the University of<br />
Auckland’s School of Optometry & Vision Science for<br />
their Bachelor of Optometry degree”.<br />
The School of Optometry & Vision Science is keen to<br />
welcome new and returning mentors for externships<br />
in June and July <strong>2018</strong>. If you are interested in becoming<br />
a new or returning externship mentor, please contact<br />
Gini Parslow, practicum placement co-ordinator at<br />
v.parslow@auckland.ac.nz or phone 027 406 8543. ▀<br />
and get expert advice about what is likely to best suit<br />
their needs.”<br />
Technology advice is provided by Vision Australia<br />
staff plus representatives from tech organisation<br />
partners, including Samsung, Apple and Google,<br />
and specialist adaptive technology providers such as<br />
IrisVision and OrCam.<br />
Other highlights of the new space include<br />
demonstration home environments, including an<br />
accessible kitchen and cooking aids (both low and<br />
high-tech solutions); a living room with TV/voice<br />
integration home devices; workplace/home study<br />
tools; Google Home to control lighting and provide<br />
audio cooking instructions; and other tools such as<br />
Samsung’s voice-controlled screen magnification tech.<br />
“Accessibility is a key consideration for people who<br />
are blind or have low vision and we’ve taken that into<br />
account with the design, layout and other features in<br />
the space,” Mr Hooton said. ▀<br />
We’re bringing more<br />
optometry events and<br />
webinars to you<br />
MyHealth1st is revolutionising digital customer engagement<br />
for independent optometrists.<br />
Don’t miss our free events and webinars on how you can join<br />
the digital revolution and put your business growth 1st.<br />
Sign up now at:<br />
myhealth1st.co.nz/optometryevents<br />
<strong>April</strong> <strong>2018</strong><br />
NEW ZEALAND OPTICS<br />
7