Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
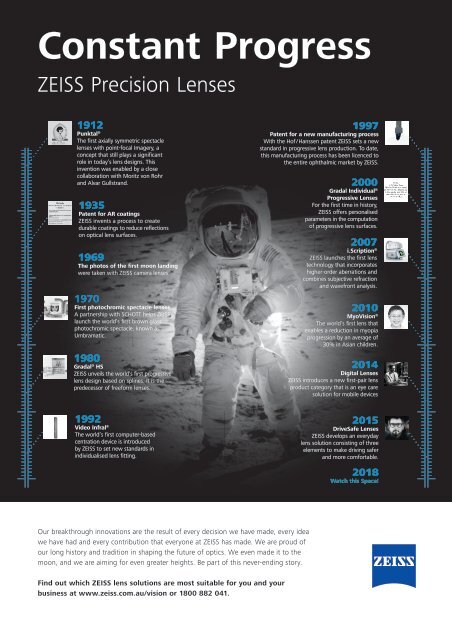
Constant Progress<br />
ZEISS Precision Lenses<br />
1912<br />
Punktal ®<br />
The first axially symmetric spectacle<br />
lenses with point-focal Imagery, a<br />
concept that still plays a significant<br />
role in today’s lens designs. This<br />
invention was enabled by a close<br />
collaboration with Moritz von Rohr<br />
and Alvar Gullstrand.<br />
1935<br />
Patent for AR coatings<br />
ZEISS invents a process to create<br />
durable coatings to reduce reflections<br />
on optical lens surfaces.<br />
1969<br />
The photos of the first moon landing<br />
were taken with ZEISS camera lenses.<br />
1970<br />
First photochromic spectacle lenses<br />
A partnership with SCHOTT helps ZEISS<br />
launch the world’s first brown glass<br />
photochromic spectacle, known as<br />
Umbramatic.<br />
1980<br />
Gradal ® HS<br />
ZEISS unveils the world’s first progressive<br />
lens design based on splines. It is the<br />
predecessor of freeform lenses.<br />
1997<br />
Patent for a new manufacturing process<br />
With the Hof / Hanssen patent ZEISS sets a new<br />
standard in progressive lens production. To date,<br />
this manufacturing process has been licenced to<br />
the entire ophthalmic market by ZEISS.<br />
2000<br />
Gradal Individual ®<br />
Progressive Lenses<br />
For the first time in history,<br />
ZEISS offers personalised<br />
parameters in the computation<br />
of progressive lens surfaces.<br />
2007<br />
i.Scription ®<br />
ZEISS launches the first lens<br />
technology that incorporates<br />
higher-order aberrations and<br />
combines subjective refraction<br />
and wavefront analysis.<br />
2010<br />
MyoVision ®<br />
The world’s first lens that<br />
enables a reduction in myopia<br />
progression by an average of<br />
30% in Asian children.<br />
2014<br />
Digital Lenses<br />
ZEISS introduces a new first-pair lens<br />
product category that is an eye care<br />
solution for mobile devices<br />
1992<br />
Video Infral ®<br />
The world’s first computer-based<br />
centration device is introduced<br />
by ZEISS to set new standards in<br />
individualised lens fitting.<br />
2015<br />
DriveSafe Lenses<br />
ZEISS develops an everyday<br />
lens solution consisting of three<br />
elements to make driving safer<br />
and more comfortable.<br />
<strong>2018</strong><br />
Watch this Space!<br />
Our breakthrough innovations are the result of every decision we have made, every idea<br />
we have had and every contribution that everyone at ZEISS has made. We are proud of<br />
our long history and tradition in shaping the future of optics. We even made it to the<br />
moon, and we are aiming for even greater heights. Be part of this never-ending story.<br />
Find out which ZEISS lens solutions are most suitable for you and your<br />
business at www.zeiss.com.au/vision or 1800 882 041.<br />
<strong>April</strong> <strong>2018</strong><br />
NEW ZEALAND OPTICS<br />
9