January/February 2012 • Volume 10 • Issue 1 - SKINmed Journal
January/February 2012 • Volume 10 • Issue 1 - SKINmed Journal
January/February 2012 • Volume 10 • Issue 1 - SKINmed Journal
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>January</strong>/<strong>February</strong> <strong>2012</strong><br />
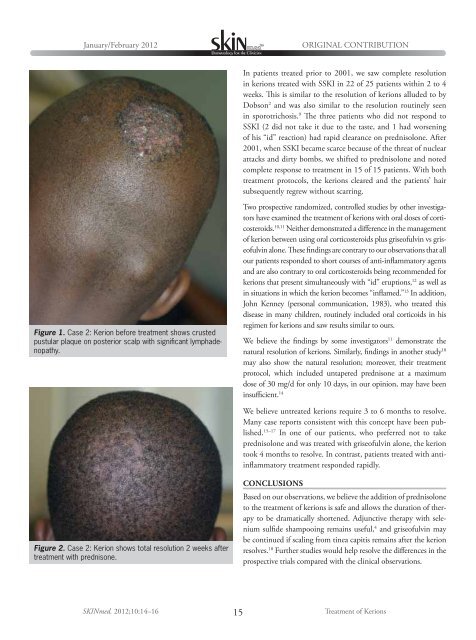
Figure 1. Case 2: Kerion before treatment shows crusted<br />
pustular plaque on posterior scalp with significant lymphadenopathy.<br />
Figure 2. Case 2: Kerion shows total resolution 2 weeks after<br />
treatment with prednisone.<br />
ORIGINAL CONTRIBUTION<br />
In patients treated prior to 2001, we saw complete resolution<br />
in kerions treated with SSKI in 22 of 25 patients within 2 to 4<br />
weeks. This is similar to the resolution of kerions alluded to by<br />
Dobson 2 and was also similar to the resolution routinely seen<br />
in sporotrichosis. 9 The three patients who did not respond to<br />
SSKI (2 did not take it due to the taste, and 1 had worsening<br />
of his “id” reaction) had rapid clearance on prednisolone. After<br />
2001, when SSKI became scarce because of the threat of nuclear<br />
attacks and dirty bombs, we shifted to prednisolone and noted<br />
complete response to treatment in 15 of 15 patients. With both<br />
treatment protocols, the kerions cleared and the patients’ hair<br />
subsequently regrew without scarring.<br />
Two prospective randomized, controlled studies by other investigators<br />
have examined the treatment of kerions with oral doses of corticosteroids.<br />
<strong>10</strong>,11 Neither demonstrated a difference in the management<br />
of kerion between using oral corticosteroids plus griseofulvin vs griseofulvin<br />
alone. These findings are contrary to our observations that all<br />
our patients responded to short courses of anti-inflammatory agents<br />
and are also contrary to oral corticosteroids being recommended for<br />
kerions that present simultaneously with “id” eruptions, 12 as well as<br />
in situations in which the kerion becomes “inflamed.” 13 In addition,<br />
John Kenney (personal communication, 1983), who treated this<br />
disease in many children, routinely included oral corticoids in his<br />
regimen for kerions and saw results similar to ours.<br />
We believe the findings by some investigators 11 demonstrate the<br />
natural resolution of kerions. Similarly, findings in another study <strong>10</strong><br />
may also show the natural resolution; moreover, their treatment<br />
protocol, which included untapered prednisone at a maximum<br />
dose of 30 mg/d for only <strong>10</strong> days, in our opinion, may have been<br />
insufficient. 14<br />
We believe untreated kerions require 3 to 6 months to resolve.<br />
Many case reports consistent with this concept have been published.<br />
15–17 In one of our patients, who preferred not to take<br />
prednisolone and was treated with griseofulvin alone, the kerion<br />
took 4 months to resolve. In contrast, patients treated with antiinflammatory<br />
treatment responded rapidly.<br />
CONCLUSIONS<br />
Based on our observations, we believe the addition of prednisolone<br />
to the treatment of kerions is safe and allows the duration of therapy<br />
to be dramatically shortened. Adjunctive therapy with selenium<br />
sulfide shampooing remains useful, 4 and griseofulvin may<br />
be continued if scaling from tinea capitis remains after the kerion<br />
resolves. 18 Further studies would help resolve the differences in the<br />
prospective trials compared with the clinical observations.<br />
<strong>SKINmed</strong>. <strong>2012</strong>;<strong>10</strong>:14–16 15<br />
Treatment of Kerions