January/February 2012 • Volume 10 • Issue 1 - SKINmed Journal
January/February 2012 • Volume 10 • Issue 1 - SKINmed Journal
January/February 2012 • Volume 10 • Issue 1 - SKINmed Journal
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
PAUCIBACILLARY CTB<br />
<strong>January</strong>/<strong>February</strong> <strong>2012</strong><br />
TB VERRUCOSA CUTIS<br />
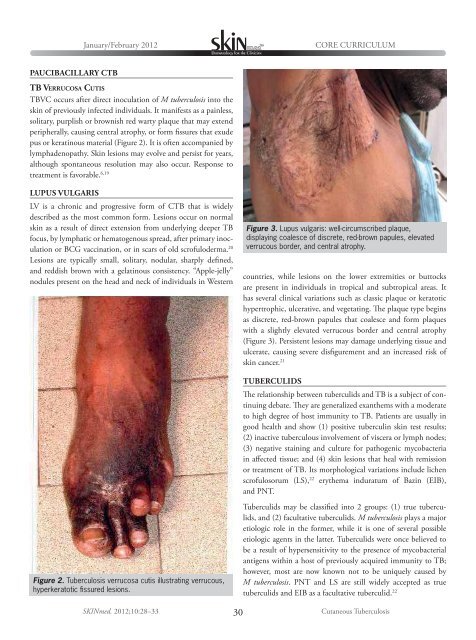
TBVC occurs after direct inoculation of M tuberculosis into the<br />
skin of previously infected individuals. It manifests as a painless,<br />
solitary, purplish or brownish red warty plaque that may extend<br />
peripherally, causing central atrophy, or form fissures that exude<br />
pus or keratinous material (Figure 2). It is often accompanied by<br />
lymphadenopathy. Skin lesions may evolve and persist for years,<br />
although spontaneous resolution may also occur. Response to<br />
treatment is favorable. 6,19<br />
LUPUS VULGARIS<br />
LV is a chronic and progressive form of CTB that is widely<br />
described as the most common form. Lesions occur on normal<br />
skin as a result of direct extension from underlying deeper TB<br />
focus, by lymphatic or hematogenous spread, after primary inoculation<br />
or BCG vaccination, or in scars of old scrofuloderma. 20<br />
Lesions are typically small, solitary, nodular, sharply defined,<br />
and reddish brown with a gelatinous consistency. “Apple-jelly”<br />
nodules present on the head and neck of individuals in Western<br />
Figure 2. Tuberculosis verrucosa cutis illustrating verrucous,<br />
hyperkeratotic fissured lesions.<br />
CORE CURRICULUM<br />
Figure 3. Lupus vulgaris: well-circumscribed plaque,<br />
displaying coalesce of discrete, red-brown papules, elevated<br />
verrucous border, and central atrophy.<br />
countries, while lesions on the lower extremities or buttocks<br />
are present in individuals in tropical and subtropical areas. It<br />
has several clinical variations such as classic plaque or keratotic<br />
hypertrophic, ulcerative, and vegetating. The plaque type begins<br />
as discrete, red-brown papules that coalesce and form plaques<br />
with a slightly elevated verrucous border and central atrophy<br />
(Figure 3). Persistent lesions may damage underlying tissue and<br />
ulcerate, causing severe disfigurement and an increased risk of<br />
skin cancer. 21<br />
TUBERCULIDS<br />
The relationship between tuberculids and TB is a subject of continuing<br />
debate. They are generalized exanthems with a moderate<br />
to high degree of host immunity to TB. Patients are usually in<br />
good health and show (1) positive tuberculin skin test results;<br />
(2) inactive tuberculous involvement of viscera or lymph nodes;<br />
(3) negative staining and culture for pathogenic mycobacteria<br />
in affected tissue; and (4) skin lesions that heal with remission<br />
or treatment of TB. Its morphological variations include lichen<br />
scrofulosorum (LS), 22 erythema induratum of Bazin (EIB),<br />
and PNT.<br />
Tuberculids may be classified into 2 groups: (1) true tuberculids,<br />
and (2) facultative tuberculids. M tuberculosis plays a major<br />
etiologic role in the former, while it is one of several possible<br />
etiologic agents in the latter. Tuberculids were once believed to<br />
be a result of hypersensitivity to the presence of mycobacterial<br />
antigens within a host of previously acquired immunity to TB;<br />
however, most are now known not to be uniquely caused by<br />
M tuberculosis. PNT and LS are still widely accepted as true<br />
tuberculids and EIB as a facultative tuberculid. 22<br />
<strong>SKINmed</strong>. <strong>2012</strong>;<strong>10</strong>:28–33 30<br />
Cutaneous Tuberculosis