June 2021 Newsletter
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
News from MHCE<br />
JUNE <strong>2021</strong> EDITION<br />
Monthly <strong>Newsletter</strong><br />
WWW.MHCE.US<br />
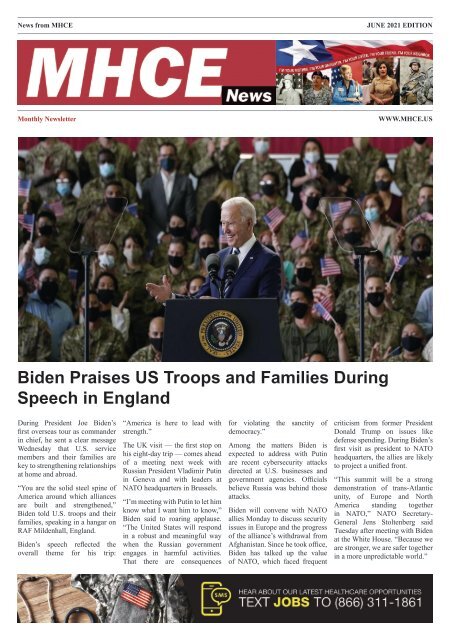
Biden Praises US Troops and Families During<br />
Speech in England<br />
During President Joe Biden’s<br />
first overseas tour as commander<br />
in chief, he sent a clear message<br />
Wednesday that U.S. service<br />
members and their families are<br />
key to strengthening relationships<br />
at home and abroad.<br />
“You are the solid steel spine of<br />
America around which alliances<br />
are built and strengthened,”<br />
Biden told U.S. troops and their<br />
families, speaking in a hangar on<br />
RAF Mildenhall, England.<br />
Biden’s speech reflected the<br />
overall theme for his trip:<br />
“America is here to lead with<br />
strength.”<br />
The UK visit — the first stop on<br />
his eight-day trip — comes ahead<br />
of a meeting next week with<br />
Russian President Vladimir Putin<br />
in Geneva and with leaders at<br />
NATO headquarters in Brussels.<br />
“I’m meeting with Putin to let him<br />
know what I want him to know,”<br />
Biden said to roaring applause.<br />
“The United States will respond<br />
in a robust and meaningful way<br />
when the Russian government<br />
engages in harmful activities.<br />
That there are consequences<br />
for violating the sanctity of<br />
democracy.”<br />
Among the matters Biden is<br />
expected to address with Putin<br />
are recent cybersecurity attacks<br />
directed at U.S. businesses and<br />
government agencies. Officials<br />
believe Russia was behind those<br />
attacks.<br />
Biden will convene with NATO<br />
allies Monday to discuss security<br />
issues in Europe and the progress<br />
of the alliance’s withdrawal from<br />
Afghanistan. Since he took office,<br />
Biden has talked up the value<br />
of NATO, which faced frequent<br />
criticism from former President<br />
Donald Trump on issues like<br />
defense spending. During Biden’s<br />
first visit as president to NATO<br />
headquarters, the allies are likely<br />
to project a unified front.<br />
“This summit will be a strong<br />
demonstration of trans-Atlantic<br />
unity, of Europe and North<br />
America standing together<br />
in NATO,” NATO Secretary-<br />
General Jens Stoltenberg said<br />
Tuesday after meeting with Biden<br />
at the White House. “Because we<br />
are stronger, we are safer together<br />
in a more unpredictable world.”
2 | MHCE - News www.mhce.us JUNE <strong>2021</strong> EDITION
WWW.MHCE.US Monthly <strong>Newsletter</strong> | 3<br />
Brown joined the Army Reserve as<br />
an enlisted Soldier four years ago.<br />
He received an ROTC scholarship<br />
and attended college, afterwards<br />
commissioning as a medical service<br />
officer.<br />
He said the opportunity to do more<br />
was there and felt a calling to the<br />
PA program. Once he had the 60<br />
credit hours necessary — and other<br />
prerequisites — he decided to put in his<br />
application.<br />
GLWACH’s Ed. Dept. Helps Secure<br />
Future of Army Medicine<br />
Healthcare professionals spend years<br />
obtaining complex medical degrees.<br />
The Education Department at General<br />
Leonard Wood Army Community<br />
Hospital helps ensure the learning<br />
continues, not only for GLWACH staff,<br />
but for hospitals across the entire state<br />
of Missouri.<br />
Jordan Walters, chief of Hospital<br />
Education and Staff Development<br />
at GLWACH, said the training and<br />
education support programs offered<br />
here include virtual and in-person<br />
clinical training opportunities.<br />
“Our HESD clinical staff members<br />
provide the required training healthcare<br />
professionals need to maintain their<br />
credentials,” Walters said.<br />
One of the programs the hospital<br />
supports is the Interservice Physician<br />
Assistant Program, which offers<br />
enlisted and officer service members<br />
from any career field the opportunity to<br />
become PAs, said Maj. Jon Thibodeau,<br />
GLWACH’s PA training coordinator.<br />
GLWACH trains about 10 students each<br />
year in the hands-on, phase two portion<br />
of the 29-month program.<br />
Staff Sgt. Stephanie Foster, a medic in<br />
the Oklahoma National Guard, is set to<br />
graduate the PA program in October.<br />
She called the course challenging.<br />
“So many challenges and a lot of<br />
successes, too,” she said. “It’s like<br />
drinking from a fire hose with the<br />
information and putting it all back<br />
together in phase two when you actually<br />
have the patient in front of you.”<br />
Foster said GLWACH’s education<br />
department allows PA students like her<br />
the chance to rehearse trauma scenarios<br />
— an invaluable resource.<br />
“Trauma is increased muscle memory<br />
for us,” she said. “It’s like an algorithm<br />
when to do what actions. That way<br />
when it’s a scary situation, you have<br />
practiced it enough and remember it.”<br />
Like Foster, 1st Lt. Austin Brown,<br />
from Hebrew Springs, Arkansas, is also<br />
currently enrolled in the PA program<br />
here.<br />
“I got some really good advice from my<br />
PA, Capt. Robert Gibson, and he gave<br />
me some advice on what to do for my<br />
(application) packet and I got picked<br />
up on the first go-around. I felt very<br />
blessed for that.”<br />
Brown said phase two is a demanding<br />
time, where students live weekby-week<br />
through various tests and<br />
challenges.<br />
“I did not have a medical background<br />
beforehand,” he said. “But we had<br />
students who were master sergeants<br />
or flight medics, or Special Forces<br />
medics with a lot of diverse knowledge.<br />
Listening to them and their experience<br />
was a huge advantage.”<br />
Brown said he studies at home when he<br />
can to spend more time with his wife<br />
and kids, and has advice for anyone<br />
thinking of applying.<br />
“Go and talk to PAs,” he said. “Go get<br />
the prerequisites; look up the program<br />
to get a lot of information. Find<br />
someone who has already gone through<br />
the program because that’s where you<br />
get most of your knowledge.”
4 | MHCE - News www.mhce.us JUNE <strong>2021</strong> EDITION<br />
Navy Medicine announces<br />
FY20 Sailor of the Year<br />
Force Master Chief Michael J. Roberts, Director of the Hospital<br />
Corps poses with Navy Medicine’s fiscal year 2020 Sailor of the Year<br />
candidates. (From left to right) Hospital Corpsman 1st Class Dylan<br />
Marrone, assigned to Walter Reed National Military Medical Center,<br />
Bethesda, Maryland; Hospital Corpsman 1st Class Thurman McCray<br />
III, assigned to Naval Hospital Guam; Hospital Corpsman 1st Class<br />
Alexis J. Sandoval, assigned to Bureau of Medicine and Surgery,<br />
Falls Church, Virginia and Hospital Corpsman Petty Officer 1st Class<br />
Michael Shoener, from Navy Medicine Training Support Center /<br />
Naval Medical Forces Support Command(NMTSC/NMFSC)<br />
TO ADVERTISE<br />
contact Nathan.Stiles@mhce.us<br />
Even the Opportunities are Sunnier<br />
The region’s most comprehensive and preferred health system, located in one of the nation’s<br />
most sought-after destinations, is seeking physicians in the following specialties:<br />
OBGYN • Family and Internal Medicine • General Cardiology • Interventional Cardiology<br />
Inpatient Medical Oncology • Neuromuscular • Orthopedics • Geriatrics<br />
Ideal Place to Practice<br />
n<br />
n<br />
n<br />
n<br />
Structurally and financially strong<br />
organization<br />
Work-life balance<br />
High-caliber, physician-led teams<br />
Extensive support from the<br />
region’s largest and most<br />
comprehensive clinically<br />
integrated network<br />
World Class Quality of Life<br />
n Northeast Florida is alive with over 1,100 miles of beaches and<br />
waterways, 80,000 acres of parks and trails, a strong and prosperous<br />
economy, multiple professional sports teams, renowned golf courses<br />
and diverse cultural experiences<br />
n The area serves as home to some of the Sunshine State’s best cost of<br />
living and the nation’s most sought after quality of life<br />
n Jacksonville was recently ranked by Forbes Magazine<br />
as the second most desirable city for<br />
relocation in the United States<br />
n No state income tax<br />
Please contact us at 904.202.5124, or email your<br />
CV to PhysicianCareers@bmcjax.com<br />
BH 33518 Specialties Recruitment Practice Link Ad_v04.indd 1<br />
2/3/20 2:08 PM
WWW.MHCE.US Monthly <strong>Newsletter</strong> | 5<br />
TO ADVERTISE contact Kyle.Stephens@mhce.us
6 | MHCE - News www.mhce.us JUNE <strong>2021</strong> EDITION<br />
Navy Sexual Assault Prevention Response program-victim advocate,<br />
Voting Assistance Officer, Diversity Officer, and Command Managed<br />
Equal Opportunity (CMEO) Program Manager<br />
“All of my assignments have been exciting and challenging in a<br />
variety of ways,” Washington said.<br />
As the nation – and armed services – come to grips with confronting<br />
not just the current pandemic outbreak, but also racial injustice,<br />
Washington’s role as CMEO program manager is crucial in providing<br />
all staff members – active duty and civil service – a safe and secure<br />
setting to perform to their maximum ability.<br />
I Am Navy Medicine,<br />
and Command<br />
Managed Equal<br />
Opportunity Program<br />
Manager – Lt. Shanece<br />
Washington<br />
“I am Lt. Shanece Washington, Navy Medical Service Corps officer<br />
and Occupational Audiologist, Regional Hearing Conservation<br />
Program Manager, and Command Managed Equal Opportunity<br />
Program Manager at Navy Medicine Readiness and Training<br />
Command (NMRTC) Bremerton.<br />
Washington has been in the Navy for four years and is originally<br />
from Colorado Springs, Colo. and Rampart High School 2004-2008.<br />
She is a graduate from University of Northern Colorado, 2008-2012,<br />
in Audiology & Speech Language Sciences, B.S., with her Clinical<br />
Doctorate in Audiology, AuD from University of Washington, 2012-<br />
2016.<br />
“I am a direct accession into the Navy. I completed all of my<br />
educational training prior to joining. During my clinical doctorate<br />
training, I was offered a spot with the Navy’s Audiology Externship<br />
Program, however, I had to decline the offer. I finished my residency<br />
training at the Veteran Affairs Puget Sound Health Care System, and<br />
made the decision to join the Navy upon my completion,” explained<br />
Washington.<br />
“The CMEO program is in place to ensure an environment that is free<br />
from social, personal, and institutional barriers that would prevent<br />
service members from rising to the highest level of responsibility<br />
possible. The ultimate goal is to foster and promote an environment<br />
that prevents harassment and unlawful discrimination. There are six<br />
protected categories for which harassment and discrimination are<br />
prohibited: race, color, gender (including gender identity), sexual<br />
orientation, national origin, and religion,” noted Washington.<br />
Washington’s role as CMEO program manager has her as the point of<br />
contact for command related equal opportunity concerns.<br />
“I do not do this alone, but rather with a team,” Washington stressed.<br />
“Our duties include ensuring proper documentation and processing<br />
of all reports of harassment and unlawful discrimination, both formal<br />
and non-formal, providing updates regarding ongoing reports and<br />
complaints to the commanding officer, coordinating the Command<br />
Climate Assessment survey, and most importantly assessing the<br />
impact of the CMEO program.”<br />
Washington attests that the importance of the CMEO program cannot<br />
be understated.<br />
“Discrimination and harassment undermine the capability of a<br />
functioning team and are a disservice to the staff members and<br />
beneficiaries we serve at this command. The CMEO program is<br />
essential to promoting a positive command climate and fostering an<br />
environment where all Service Members can thrive,” Washington<br />
said.<br />
“I hope to promote a climate that goes beyond the idea of equality, but<br />
rather highlights the need of equity and equitable practices that must<br />
be built into everyday occurrences across the command to ensure<br />
Washington grew up in a military family, and always knew from a<br />
young age that she wanted to work with military members or veterans.<br />
“My father served in the Air Force as a captain and instilled a sense<br />
of responsibility and service to community in his children. It took me<br />
several years to finalize the capacity in which I wanted to serve my<br />
community,” said Washington.<br />
Despite her relatively short time on active duty, Washington has<br />
served on both sides of the Pacific, from the Far East to the Pacific<br />
Northwest. Navy Medicine has afforded her the opportunity to serve<br />
in Yokosuka, Japan, Chinhae, South Korea, and now at NMRTC<br />
Bremerton, Washington.<br />
That fatherly advice learned when growing up has also empowered<br />
Washington to take on a host of overlapping duties, which include<br />
Hearing Conservation Program Manager, COVID-19 Level 1 Triage<br />
provider, Occupational Audiology department head, Controlled<br />
Substance Inventory board chair, Medical Service Corps secretary,
WWW.MHCE.US Monthly <strong>Newsletter</strong> | 7<br />
equality,” added Washington. “Ultimately, I hope to grow NMRTC<br />
Bremerton into an example of best practices for the Department of the<br />
Navy’s Equal Opportunity and Sexual Harassment programs.”<br />
According to Washington, the best part of her career has been<br />
collaborating with talented, passionate and forward thinking<br />
individuals who strive to a make positive change within the Navy.<br />
“I’ve witnessed the value of intervention and the impact that prevention<br />
has on the quality of life of service members and their families. I started<br />
my audiology career reactively by treating hearing loss in veterans.<br />
Now I proactively try and prevent hearing loss from occurring in<br />
service members. Additionally, I serve as a resource to operational<br />
commanders and leadership to strategize appropriate interactions and<br />
feasible recommendations related to hearing readiness. This is a great<br />
gift that gives me purpose and motivation to continue this essential<br />
work,” stated Washington.<br />
Washington’s duty as audiologist directly contribute to the Navy<br />
surgeon general priority on operational readiness and Navy Medicine’s<br />
core mission of producing force medical readiness and medical force<br />
readiness.<br />
“The mission of Navy Audiology is to prevent occupational-related<br />
hearing injuries and increase medical readiness. Hearing loss can<br />
place members in danger, diminish oral and communication skills,<br />
and lead to ineffective command control with a potential for mission<br />
failure,” said Washington. “Hearing directly impacts the ability/<br />
inability to localize and identify sound sources in an environment.<br />
The vision of Navy Audiology is to ensure mission readiness in worldwide<br />
operations by optimizing warfighter lethality, survivability<br />
and situational awareness. We accomplish this through advocacy,<br />
outreach, training, hearing protection, medical surveillance, and<br />
treatment/rehabilitative services.”<br />
When asked to sum up her Navy Medicine career in one sentence,<br />
Washington replied, “My Navy career has been the most challenging<br />
and rewarding thing I have ever done, and has propelled me to higher<br />
levels of responsibility that I previously had not considered.<br />
Join Our Team!<br />
Embark on a new career<br />
with Central New York<br />
Psychiatric Center!<br />
Our Team Promotes<br />
Hope, Resilience and Recovery!<br />
Central New York Psychiatric Center is seeking<br />
candidates to fill the following positions;<br />
Psychiatrists, Psychiatric Nurse Practitioners,<br />
Psychologists, and Registered Nurses.<br />
These positions are available at our Inpatient<br />
Forensic Hospital in Marcy, New York, as<br />
well as our Corrections Based Satellite Units<br />
across the State.<br />
Benefits Include:<br />
• NYS Pension<br />
• Competitive Salaries<br />
• Comprehensive Health Insurance<br />
• Flexible Spending Accounts for<br />
Healthcare & Dependent Care<br />
• Generous Paid Time Off<br />
Contact Us:<br />
315-765-3375 or by e-mail<br />
CNpersonnel@omh.ny.gov
8 | MHCE - News www.mhce.us JUNE <strong>2021</strong> EDITION<br />
Auburn’s Harbert College of Business ranked as One of<br />
the Nation’s Best by U.S. News & World Report<br />
The Harbert College of Business is Auburn University’s second largest academic unit and<br />
continuing to grow. They’ve excelled at over 30 years of providing distance learning to graduate<br />
students around the U.S. For some of us, Zoom classes became a reality just last year. That’s<br />
old news to Auburn’s business unit because they’ve been on the distance learning train long<br />
before it became a common practice for schools everywhere.<br />
“In this dynamic and ever evolving online program space,<br />
few colleges have such a strong foundation and history of<br />
program development and recognized excellence in graduate<br />
online programs. We are honored to have our programs again<br />
be recognized [in] U.S. News & World Report.”<br />
—Harbert College of Business Dean Annette L. Ranft for The Harbert College of<br />
Business at Auburn University<br />
VISIT OUR WEBSITE<br />
AT MHCE.US<br />
With that expertise in the digital, education space, it’s no surprise that their online programs<br />
have been recognized nationally.<br />
TO ADVERTISE<br />
contact Nathan.Stiles@mhce.us
WWW.MHCE.US Monthly <strong>Newsletter</strong> | 9<br />
When the practice of medicine<br />
becomes the business of medicine.<br />
You spent years studying medicine.<br />
But what about the business side of<br />
your practice?<br />
It’s easy to get started.<br />
Take the next step toward a<br />
Physicians Executive MBA<br />
and contact us:<br />
auburn-military.mba<br />
334-844-4060<br />
Auburn MBA
10 | MHCE - News www.mhce.us JUNE <strong>2021</strong> EDITION<br />
Readiness at Forefront of Regional Health Command-<br />
Pacific Commander’s Spring Symposium<br />
JOINT BASE PEARL HARBOR-HICKAM, Hawaii – Brig. Gen. Jack<br />
M. Davis, commanding general, Regional Health Command-Pacific, and<br />
Command Sgt. Maj. Abuoh E. Neufville, hosted the region’s <strong>2021</strong> Spring<br />
Commander's Symposium May 4-6, at the Tradewinds Club here.<br />
The theme of the symposium was ‘Ready Pacific,’ with an emphasis on RHC-<br />
P’s role in enabling a ready medical force across the Indo-Pacific Command.<br />
"As we get into MEDCOM’s pivot to readiness, we’re looking at what that<br />
means for us here in the Pacific, and how we support it,” said Davis.<br />
With readiness at the forefront of discussions throughout the symposium,<br />
attendees came together virtually and in-person from around the Pacific<br />
region.<br />
Participants heard from senior leaders from across the U.S. Army, U.S.<br />
Indo-Pacific Command, Defense Health Agency, and U.S. Army Medical<br />
Department, about important strategic topics impacting military medicine,<br />
readiness, workforce development, and healthcare delivery.<br />
DHA. Closing out the symposium was Maj. Gen. Michael Place, commanding<br />
general, 18th Medical Command, who spoke about the battlefield of the<br />
future and how Army medicine will be engaged.<br />
At the conclusion of the event, Davis, the RHC-P commanding general,<br />
expressed his appreciation to each of the speakers for their informative<br />
updates.<br />
Davis also thanked leaders for participating both in-person and virtually.<br />
He also recognized the RHC-P staff the planning and implementation of a<br />
successful symposium.<br />
RHC-P, headquartered at JBLM and in Honolulu, is the most geographicallydispersed<br />
command in Army Medicine, stretching more than 5,000 miles<br />
and five time zones across the Pacific. The command oversees Army medical<br />
treatment facilities and units in the Pacific Northwest, Alaska, Hawaii, Japan<br />
and South Korea.<br />
Day one of the symposium kicked-off with a briefing from Cmdr. Shawn<br />
Clausen, chief of Force Health Protection, INDOPACOM, who provided an<br />
overview of INDOPACOM’s response to COVID-19.<br />
Col. Nelson So, commander of the 47th Combat Support Hospital at Joint<br />
Base Lewis-McChord, Wash., gave an update on the hospital’s conversion to<br />
a Hospital Center and Field Hospital from its current configuration as a CSH.<br />
The second day began with a briefing on the DHA transition from Maj.<br />
Gen. Telita Crosland, deputy surgeon general, MEDCOM. Sgt. Maj. Jimmy<br />
Sellers, deputy chief of staff, U.S. Army Logistics (G-4), gave a presentation<br />
on the relationship between officers and non-commissioned officers.<br />
Col. Deydree S. Teyhen, chief of the U.S. Army Medical Specialist Corps,<br />
gave a presentation on improving the health, fitness, and readiness of our force.<br />
Teyhen has recently been serving as the Department of Defense therapeutics<br />
lead for the federal government’s COVID-19 response operations.<br />
At the end of the day, Dr. Brian Lein, assistant director, health care<br />
administration, DHA, discussed clinical readiness opportunities.<br />
On day three, leaders received an update on Professional Military Education<br />
from Maj. Gen. Dennis LeMaster, commanding general, Medical Center of<br />
Excellence.<br />
Attendees also heard from Mrs. Veronica Dudley, director, MEDCOM<br />
Intelligence and Security, and Mr. Richard Beauchemin, chief of staff,<br />
MEDCOM, who addressed the topic of Army civilians and their transition to
WWW.MHCE.US Monthly <strong>Newsletter</strong> | 11<br />
needs<br />
you!<br />
View current jobs<br />
or apply online at<br />
JOBS.LA.GOV<br />
For more info<br />
contact Katie Gaulden at<br />
(225) 634-4303 or katheryn.gaulden@la.gov<br />
EQUAL OPPORTUNITY EMPLOYER | JOINT COMMISSION ACCREDITED
NEW<br />
12 | MHCE - News www.mhce.us JUNE <strong>2021</strong> EDITION<br />
CDC Lowers Guam’s risk level, Clearing Fully Vaccinated<br />
People to Travel There<br />
The Centers for Disease Control and Prevention<br />
lowered Guam’s coronavirus travel-risk level<br />
from “very high” to “moderate” on Monday,<br />
meaning fully vaccinated people are now OK<br />
to fly to the U.S. island territory.<br />
However, unvaccinated travelers who are apt<br />
to become severely ill from the coronavirus<br />
respiratory disease are encouraged to avoid all<br />
unnecessary travel there.<br />
The CDC’s “moderate” designation, also<br />
called level two, means Guam has tallied<br />
between 50 and 99 new COVID-19 cases over<br />
the past 28 days. The island had been at level<br />
four, which urges people to avoid all travel<br />
because of a high number of new infections,<br />
since May 17.<br />
Since the pandemic began, Guam has<br />
confirmed 8,210 coronavirus cases, 59<br />
of which were active as of Monday, and<br />
139 deaths, according to the island’s Joint<br />
Information Center. Six new patients were<br />
identified between Friday and Sunday.<br />
“We welcome CDC’s downgrade in travel<br />
risk for Guam from very high to moderate,”<br />
Gov. Lou Leon Guerrero said in a statement<br />
Tuesday. “This complements our recently<br />
updated protocols that allow vaccinated<br />
travelers to enter our borders without<br />
quarantine.”<br />
The news comes a little more than a week after<br />
the CDC discovered a COVID-19 “variant of<br />
interest” – B.1.617.2, or the Indian variant<br />
– among samples collected on Guam this<br />
spring. Twenty-five samples taken in March<br />
and April underwent genome sequencing by<br />
the CDC, which returned the results to the<br />
island’s Department of Public Health and<br />
Social Services on May 28.<br />
Of those, 16 were identified as B.1.1.7, the<br />
United Kingdom variant, and one was B.1.341,<br />
the South African variant. Both are variants<br />
“of concern,” according to the CDC, meaning<br />
there is evidence of increased transmissibility,<br />
hospitalizations or deaths.<br />
Another of the samples turned out to be the<br />
Indian variant, which the CDC and World<br />
Health Organization call a “variant of<br />
interest” because its potential risks warrant<br />
close monitoring.<br />
VISIT OUR WEBSITE<br />
AT MHCE.US
WWW.MHCE.US Monthly <strong>Newsletter</strong> | 13<br />
CDC Discovers<br />
Indian Variant<br />
Among COVID-19<br />
Samples Recently<br />
Returned to Guam<br />
The Centers for Disease Control and Prevention<br />
lowered Guam’s coronavirus travel-risk level<br />
from “very high” to “moderate” on Monday,<br />
meaning fully vaccinated people are now OK<br />
to fly to the U.S. island territory.<br />
However, unvaccinated travelers who are apt<br />
to become severely ill from the coronavirus<br />
respiratory disease are encouraged to avoid all<br />
unnecessary travel there.<br />
The CDC’s “moderate” designation, also<br />
called level two, means Guam has tallied<br />
between 50 and 99 new COVID-19 cases over<br />
the past 28 days. The island had been at level<br />
four, which urges people to avoid all travel<br />
because of a high number of new infections,<br />
since May 17.<br />
Since the pandemic began, Guam has<br />
confirmed 8,210 coronavirus cases, 59<br />
of which were active as of Monday, and<br />
139 deaths, according to the island’s Joint<br />
Information Center. Six new patients were<br />
identified between Friday and Sunday.<br />
“We welcome CDC’s downgrade in travel<br />
risk for Guam from very high to moderate,”<br />
Gov. Lou Leon Guerrero said in a statement<br />
Tuesday. “This complements our recently<br />
updated protocols that allow vaccinated<br />
travelers to enter our borders without<br />
quarantine.”<br />
The news comes a little more than a week after<br />
the CDC discovered a COVID-19 “variant of<br />
interest” – B.1.617.2, or the Indian variant<br />
– among samples collected on Guam this<br />
spring. Twenty-five samples taken in March<br />
and April underwent genome sequencing by<br />
the CDC, which returned the results to the<br />
island’s Department of Public Health and<br />
Social Services on May 28.<br />
VISIT OUR WEBSITE<br />
AT MHCE.US<br />
TO ADVERTISE<br />
contact Susan.Keller@mhce.us
14 | MHCE - News www.mhce.us JUNE <strong>2021</strong> EDITION<br />
A Look Back at the First African-American Nurses<br />
in the Navy<br />
From the dawn of the U.S Navy, African-<br />
Americans have played a vital role in its<br />
history and have embodied the basic tenets<br />
of service and commitment to duty. At the<br />
same time, the African-American experience<br />
in naval history is a story about breaking<br />
barriers, living through a segregated service,<br />
and overcoming limitations of opportunity<br />
on the path to what Admiral Elmo “Bud”<br />
Zumwalt called “One Navy.”<br />
During the Civil War, African-Americans<br />
comprised twenty-five percent of the total<br />
naval force; not included in this statistic<br />
were five African-American women (Alice<br />
Kennedy, Sarah Kinno, Ellen Campbell,<br />
Betsy Young, and Dennis[e] Downs) who<br />
served as nurses aboard the Navy’s “first”<br />
hospital ship, USS Red Rover in 1863.<br />
Although only volunteers, it is remarkable<br />
to note that for over the next century these<br />
women would represent the Navy’s only<br />
black nurses.<br />
Mixed crews were common in the Navy until<br />
“Jim Crow” state laws become the policy of<br />
the service. From 1922 to 1942, blacks were<br />
barred from serving as anything but mess<br />
attendants or stewards. Four months after the<br />
attack on Pearl Harbor, President Franklin<br />
Roosevelt called for the end of the Navy’s<br />
discriminatory policies. On April 7, 1942,<br />
Secretary of the Navy Frank Knox announced<br />
that the Navy would start accepting enlistment<br />
of blacks in ratings other than messmen.<br />
By 1943, African-Americans were finally<br />
allowed to serve as Hospital Corpsmen; and<br />
by March 1944 blacks—following the lead<br />
of the “Golden Thirteen”—were allowed<br />
to serve as dentists, physicians, as well as<br />
Hospital Corps officers.<br />
After October 1944, black women were<br />
permitted to serve as reserve officers<br />
in administrative capacities. Ironically,<br />
the Navy Nurse Corps, which had long<br />
battled for gender equality within the Navy<br />
establishment, would be the last to open its<br />
doors to African-Americans.<br />
Since being established in May 1908 the<br />
Navy Nurse Corps had a history of barring<br />
married women, single mothers, and men into<br />
its ranks on a permanent basis. And although<br />
black nurses were not officially prohibited<br />
from entering the services after 1944, they
WWW.MHCE.US Monthly <strong>Newsletter</strong> | 15<br />
were often “overlooked” in Army, Navy and<br />
Red Cross recruiting drives until early 1945.<br />
First Lady Eleanor Roosevelt and Mable<br />
Keaton Staupers, Executive Secretary of the<br />
National Association of Colored Graduate<br />
Nurses were among the most vocal critics of<br />
the implicit “ban” on black nurses. A longtime<br />
advocate for racial equality in the nursing<br />
profession, Staupers wrote that military<br />
service was the responsibility for all citizens<br />
of the United States, especially during a time<br />
of war.<br />
On March 8, 1945, the longstanding barrier<br />
in the Navy was finally broken when a<br />
25-year old New York-born nurse named<br />
Phyllis Mae Daley received a commission<br />
in the U.S. Navy Reserve. A graduate of<br />
Lincoln School of Nursing in New York and<br />
student of public health at Teachers College,<br />
Columbia University, Daley had previously<br />
been rejected from entering the Army Air<br />
Force. Determined to serve, Daley stated<br />
that she “knew the barriers were going to be<br />
broken down eventually and…felt the more<br />
applicants the better the chances would be for<br />
each person.”<br />
Daley’s path would be soon after followed<br />
by Edith Mazie Devoe, of Washington, D.C.,<br />
on 18 April 18th, Helen Fredericka Turner, of<br />
Augusta, Ga., on April 20th, and Eula Loucille<br />
Stimley, of Centreville, Miss., on May 8th,<br />
1945.<br />
Following the war all but Devoe would leave<br />
active duty. Devoe would later make history<br />
as the first black nurse in the Regular Navy on<br />
January 6, 1948. In 1950 she would become<br />
the first African-American Navy nurse to<br />
serve outside the continental United States<br />
(Triple General Hospital, Hawaii).<br />
VISIT OUR WEBSITE<br />
AT MHCE.US
16 | MHCE - News www.mhce.us JUNE <strong>2021</strong> EDITION<br />
Navy Medicine<br />
Staff Cited<br />
for Stellar<br />
COVID Vaccine<br />
Teamwork<br />
The concept, implementation and fulfillment<br />
of team work was recognized May 13, <strong>2021</strong>.<br />
Not in an arena, at a stadium or on a field of<br />
play.<br />
The acknowledgement took place at a Navy<br />
Medicine coordinated COVID-19 mass<br />
vaccine site.<br />
Rear Adm. James A. Aiken, Commander,<br />
Carrier Strike Group Three, presented the<br />
Navy and Marine Corps Commendation<br />
Medal to several staff members of Navy<br />
Medicine Readiness Training Command<br />
(NMRTC) `Bremerton for their COVID-19<br />
vaccine efforts in the third largest fleet<br />
concentration area.<br />
Hospital Corpsman 1st Class James A.<br />
Gibbens was cited for meritorious service<br />
from December 2020 to May <strong>2021</strong> ensuring<br />
COVID19 vaccine inventory totaling 42,000<br />
doses were properly managed in accordance<br />
with the strict guidelines, which included<br />
training eight petty officers on the proper<br />
handling of Moderna and Pfizer COVID-19<br />
vaccine, He also coordinated mass vaccines<br />
for USS Nimitz (CVN 68) crewmembers,<br />
provided onsite expertise in vaccine<br />
management, patient flow and site selection,<br />
which set the standard for the shipboard<br />
vaccination.<br />
The reports of a steady increase of eligible<br />
beneficiaries getting vaccinated has been<br />
welcome news to Navy leadership. Yet<br />
what has also been just as appreciated is the<br />
behind-the-scene coordination, collaboration<br />
and cooperation to administer the vaccine.<br />
“You have come together as a team. What<br />
you are doing, and have done, is bigger than<br />
yourself. This (mass vaccination) wouldn’t<br />
work unless each one of you did your part.<br />
I applaud your effort and drive. For what<br />
you have accomplished, I am thankful,” said<br />
Aiken.<br />
Lt. Cmdr. Matthew G. Case was recognized<br />
for his contributions serving as public health<br />
emergency officer from December 2020<br />
to May <strong>2021</strong>. During that time frame, the<br />
Medical Corps officer oversaw the successful<br />
COVID-19 vaccination effort for the entire<br />
Kitsap Peninsula, delivering more than<br />
34,000 vaccines to 8,100 active duty service<br />
members, 12,000 eligible beneficiaries,<br />
civilians and contract employees for Navy<br />
Region Northwest.<br />
Case was also noted for providing technical<br />
assistance to Carrier Strike Group Three<br />
ensuring that the vaccine administration plan<br />
adhered to Defense Health Agency guidance.<br />
Additionally, Case oversaw logistical<br />
handling of more than 42,000 vaccines and<br />
redistribution of several thousand vaccine<br />
doses to outlying clinics.<br />
“What most don’t know is how many extra<br />
hours I put him through, whether it was<br />
counting shots and doses every late night<br />
or coming up with ideas on the best way<br />
to administer the vaccine. Lt. Cmdr. Case<br />
has been flexible and innovative,” said<br />
Capt. Jeffrey H. Feinberg, NHB/NMRTC<br />
Bremerton executive officer.<br />
Aiken affirmed that the singular actions by<br />
Case, Gibbens and others, were essential to<br />
a successful team effort, and were a main<br />
reason why 'we have been succeeding in our<br />
efforts' to eradicate the virus since the vaccine<br />
was first offered to eligible beneficiaries in<br />
the Pacific Northwest on Dec. 23, 2020.<br />
“Whether someone was 75 and older, a<br />
family member or active duty, the courtesy<br />
and respect given to everyone by the mass<br />
vaccination team was very well received and<br />
professional,” Aiken said. “I had retirees<br />
come up to me after getting vaccinated on a<br />
Saturday morning back in January and they<br />
told me, ‘thanks.’ Not just for getting the shot<br />
that day, but for being personally contacted<br />
beforehand and taking the time to explain<br />
and answer any questions and concerns.”<br />
TO ADVERTISE<br />
contact Kyle.Stephens@mhce.us
WWW.MHCE.US Monthly <strong>Newsletter</strong> | 17<br />
TO ADVERTISE<br />
contact Karen.Scott@mhce.us<br />
TO ADVERTISE contact Paul.Randall@mhce.us
18 | MHCE - News www.mhce.us JUNE <strong>2021</strong> EDITION<br />
How Military Spouses Can Use the<br />
Transition Assistance Program<br />
The Defense Department's transition assistance program (TAP) is<br />
designed to help service members get out of the military and back to<br />
civilian life. But what about their spouses? What's in the transition<br />
program for them? Before 2019, the most spouses knew about the<br />
transition program was that they could attend on a space-available<br />
basis. In October 2019, however, a new, congressionally mandated<br />
program rolled out and, with it, specific guidance for how and when<br />
some military spouses can get involved in the transition process with<br />
their military member.<br />
While the DoD is also developing a spouse-specific set of transition<br />
programming available online through Military OneSource, this<br />
policy addresses spouses and TAP as it's designed for the service<br />
member.<br />
What is TAP?<br />
resources. Finally, a capstone session makes sure all of the boxes on<br />
the transition paperwork have been checked -- literally.<br />
Virtual TAP Training<br />
The in-person sessions represent a lot of time in transition training.<br />
If you have a day job or child care needs, you probably can't or don't<br />
want to commit that much time to sitting in sessions with your service<br />
member spouse.<br />
TO ADVERTISE<br />
contact Nathan.Stiles@mhce.us<br />
TAP is presented to troops in five distinct parts, starting in most cases<br />
no later than 365 days from their final-out date.<br />
The process starts with a one-on-one initial counseling session during<br />
which the service member creates and walks through a self assessment<br />
and individualized plan. Next, troops attend a pre-separation briefing<br />
where they get a broad overview of the transition. The third step<br />
focuses on three different briefings from the Defense Department,<br />
the Department of Labor and the Department of Veterans Affairs.<br />
Next, they'll pick a focused track that walks through education or job
WWW.MHCE.US Monthly <strong>Newsletter</strong> | 19
20 | MHCE - News www.mhce.us JUNE <strong>2021</strong> EDITION<br />
allow aircrew to wear their usual length arms and hems, decreasing the<br />
risk of safety hazards."<br />
But most pregnant naval aviators are still stuck on the ground. While the<br />
Air Force has moved in recent years to create policies allowing pregnant<br />
pilots to fly for a greater portion of their pregnancies if they choose, the<br />
Navy has yet to follow suit.<br />
According to Navy guidance updated in 2017, pregnancy is considered<br />
a disqualifier for flying duties, although aircrew members may request a<br />
waiver requiring approval from a local board of flight surgeons.<br />
"Designated Naval Aviators who are authorized to fly during pregnancy<br />
shall perform flight duties in a Medical Service Group 3 capacity only,"<br />
the guidance states. That category refers to aviators limited to operating<br />
aircraft with dual controls and accompanied on all flights by a pilot or<br />
copilot with a less-restrictive medical qualification.<br />
Navy Quietly Rolls Out<br />
First Maternity Flight<br />
Suits<br />
The Navy welcomed its first female aviators in 1974. A mere 47 years<br />
later, it's giving pregnant pilots a flight suit that fits them.<br />
The service quietly issued the first maternity flight suit to Lt. Cmdr.<br />
Jacqueline Nordan, a mobilization program manager in the Naval Air<br />
Force Reserve, as part of an early distribution program, officials said this<br />
week. Several other pregnant members of the command also received<br />
the uniform in a test run to determine its usefulness, Navy spokeswoman<br />
Amie Blade.<br />
The Navy also began issuing the flight suit more broadly in May via an<br />
Aircrew Systems Advisory to the fleet, Blade said.<br />
"An Interim Rapid Action Change was drafted for the aircrew clothing<br />
maintenance manual informing the maintainers on the procedures for<br />
how to acquire a maternity flight suit," she said.<br />
All pregnant Navy aircrew members are now eligible to wear the<br />
garment, which features adjustable side panels and provides a snugger,<br />
more professional fit as an aviator's pregnancy progresses.<br />
Prior to the maternity flight suit, pregnant aircrew have generally<br />
collected larger sized flight suits and gone up through additional sizes<br />
throughout their pregnancy, potentially needing three to five additional<br />
flight suits," Nordan, who has previously been assigned to an EA-18G<br />
Growler squadron, said in the release. "Wearing a larger-sized flight suit<br />
results in longer hems and sleeves, potentially presenting a safety hazard<br />
in the aircrew cleared to fly during pregnancy."<br />
She added that baggy and oversized flight suits simply look unprofessional.<br />
"Pregnant aircrew who are not flying are still conducting squadron<br />
business," she said. "They're still instructing classes, working in<br />
simulators, giving briefings, and representing their organizations. It<br />
makes a big difference to be able to continue to represent ourselves<br />
professionally in a well-fitting uniform throughout a pregnancy."<br />
It was actually the safety hazard of the larger flight suits that prompted<br />
development of the maternity uniform, Blade said.<br />
"A single adjustable flight suit can expand across multiple trimesters<br />
depending on each pregnancy, saving pregnant aircrew the added expense<br />
associated with purchasing multiple flight suits, as well as the cost of<br />
tailoring larger-sized flight suits historically purchased to accommodate<br />
the changing pregnant form," she said. "The expandable side panels<br />
Single-pilot, ejection seat and high-performance aircraft that can<br />
pull more than 2 Gs are entirely off-limits, as are planes that conduct<br />
shipboard operations and those with cabin altitudes that exceed 10,000<br />
feet. And after the third trimester begins, flying is banned entirely.<br />
In 2019, the Air Force got rid of a medical waiver requirement for<br />
pregnant pilots who wanted to fly later into their pregnancies. It also<br />
expanded the standard flight-duty window for pregnancy by five weeks,<br />
allowing pregnant pilots to fly from weeks 12 to 28 if they choose. Later<br />
the same year, Lt. Col. Jammie Jamieson, a member of the Air Force<br />
Women's Initiative Team, said the service was evaluating the science<br />
with an eye to further reducing restrictions.<br />
The Air Force has also taken steps to design and buy maternity flight<br />
suits, launching solicitation and test efforts in 2020. The initiative caught<br />
the attention of conservative pundit Tucker Carlson earlier this year. He<br />
featured a photo of an Air Force captain wearing one of the flight suit<br />
prototypes and scoffed, saying such efforts were making "a mockery of<br />
the U.S. military."<br />
Military leaders from across the services were swift to condemn Carlson's<br />
attack.<br />
"Women lead our most lethal units with character," Sergeant Major of<br />
the Army Michael Grinston responded in a tweet. "They will dominate<br />
ANY future battlefield we're called to fight on."<br />
Creating a Culture<br />
of Caring<br />
Offering master’s<br />
and doctoral<br />
degrees for<br />
Registered Nurses<br />
Specialties Offered:<br />
Nurse-Midwife<br />
Family Nurse Practitioner<br />
Women’s Health Care NP<br />
Psychiatric-Mental Health NP<br />
Learn more at frontier.edu/military
WWW.MHCE.US Monthly <strong>Newsletter</strong> | 21
22 | MHCE - News www.mhce.us JUNE <strong>2021</strong> EDITION<br />
Fully Vaccinated Sailors Can Make Some Port<br />
Calls, Ditch Masks and Cut Quarantines<br />
After more than a year of grueling Navydeployments that left ships at sea<br />
for months on end with no port visits, leaders announced that some of<br />
the strict restrictions put in place during the pandemic will be lifted for<br />
immunized personnel.<br />
Sailors who've been fully vaccinated against COVID-19 or had the<br />
illness caused by the novel coronavirus in the past three months will<br />
no longer be required to quarantine before deployments, Vice Adm.<br />
Phillip Sawyer, deputy chief of naval operations for operations, plans<br />
and strategy, wrote in a new force-wide message issued Monday. The<br />
change applies to personnel on ships, submarines and aircraft, he said.<br />
Anyone who has declined the vaccine and hasn't built up antibodies for<br />
COVID-19 through an infection in the last three months will still be<br />
required to sequester for 14 days before deployments. Those personnel<br />
will also be required to take COVID-19 tests before deploying.<br />
Immunized sailors will also get the OK to make port calls in some spots<br />
with U.S. military facilities, including Guam, Bahrain and Japan, where<br />
they can use gyms, commissaries and other base services, Sawyer said.<br />
Fully immunized sailors can also stop wearing face masks and social<br />
distancing from others in most situations, his message states.<br />
With more than a year operating in the COVID environment, we have<br />
gained significant expertise in mitigating and preventing the spread of<br />
COVID-19," he said in a news release announcing the changes. "Now<br />
with vaccines and [Centers for Disease Control and Prevention] scientific<br />
data, we are able to relax many of the procedures we put in place and still<br />
provide for the health protection of the force."<br />
The coronavirus pandemic wreaked havoc on military operations,<br />
particularly missions on ships and submarines, where social distancing<br />
in tight quarters is nearly impossible. Early in the pandemic, a massive<br />
COVID-19 outbreak on the aircraft carrier Theodore Roosevelt left the<br />
ship stuck in Guam for weeks as nearly the entire crew was moved ashore<br />
to quarantine.<br />
More than 1,200 sailors on that ship tested positive for the virus, and one<br />
died.<br />
Since then, crews have been required to stretch time away from their<br />
families by boarding ships early for quarantine periods ahead of<br />
deployments. Deployed crews also stopped making most port calls,<br />
leaving some at sea for about 300 consecutive days.<br />
Sawyer said the Navy is now seeing the military's highest vaccination<br />
rate and the lowest number of COVID-19 cases. He credited sailors,<br />
Navy civilians and contractors for assuming "personal responsibility" to<br />
stop the spread of COVID-19, which has killed 26 service members and<br />
infected nearly 39,000 Navy personnel.<br />
So far, more than 230,000 Navy and Marine Corps personnel have been<br />
fully immunized, the message states. Marines, who routinely deploy<br />
on Navy ships, have shown some resistance to the shots, though. As of<br />
April, nearly 40% of the 123,000 Marines who had the chance to receive<br />
the COVID-19 vaccine had turned it down.<br />
"We must continue to pursue full vaccination and apply best health<br />
protection measures both at home and at work to sustain and improve<br />
upon this performance," Sawyer said.<br />
"The science is pretty clear," he added. "Vaccinations are key to best<br />
protecting our sailors. The more sailors that are vaccinated, the better for<br />
them, their families, the Navy and the nation."
WWW.MHCE.US Monthly <strong>Newsletter</strong> | 23<br />
Tricare Select is a new health insurance plan that replaced Tricare Standard<br />
& Extra.<br />
Who Is Covered By Tricare Select?<br />
Everyone eligible for Tricare with the exception of active-duty members<br />
may enroll in the Tricare Select plan. The program is available worldwide.<br />
Tricare Select Basics<br />
With Tricare Select you can get care from any Tricare-authorized provider,<br />
network or non-network. No referrals are required, but some care may<br />
require prior authorization.<br />
If you see a network provider you won't have to pay anything except your<br />
copay or file any claims. If you visit a non-network provider you may have<br />
to pay the full cost and file a claim with Tricare to be reimbursed.<br />
How To Enroll<br />
For information on how to enroll see the Tricare website at https://www.<br />
tricare.mil/<br />
Or visit our Tricare Select coverage page for more information including<br />
coverage and costs at https://www.military.com/benefits/tricare/tricareselect/tricare-select-details.html.
24 | MHCE - News www.mhce.us JUNE <strong>2021</strong> EDITION<br />
the FDA had advised that it warranted<br />
review. Company scientists said the<br />
drug’s initial failure was due to some<br />
patients not receiving high enough doses<br />
to slow the disease.<br />
But the changes to dosing and the<br />
company’s after-the-fact analysis made<br />
the results hard to interpret, raising<br />
skepticism among many experts,<br />
including those on the FDA panel.<br />
FDA Approves Much-debated Alzheimer’s<br />
Drug Panned by Experts<br />
WASHINGTON — Government health<br />
officials on Monday approved the first<br />
new drug for Alzheimer’s disease in<br />
nearly 20 years, disregarding warnings<br />
from independent advisers that the<br />
much-debated treatment hasn’t been<br />
shown to help slow the brain-destroying<br />
disease.<br />
The Food and Drug Administration said<br />
it approved the drug from Biogen based<br />
on results that seemed “reasonably<br />
likely” to benefit Alzheimer’s patients.<br />
It’s the only therapy that U.S. regulators<br />
have said can likely treat the underlying<br />
disease, rather than manage symptoms<br />
like anxiety and insomnia.<br />
The decision, which could impact<br />
millions of Americans and their families,<br />
is certain to spark disagreements among<br />
physicians, medical researchers and<br />
patient groups. It also has far-reaching<br />
implications for the standards used<br />
to evaluate experimental therapies,<br />
including those that show only<br />
incremental benefits.<br />
The new drug, which Biogen developed<br />
with Japan’s Eisai Co., did not reverse<br />
mental decline, only slowing it in one<br />
study. The medication, aducanumab,<br />
will be marketed as Aduhelm and is to be<br />
given as an infusion every four weeks.<br />
Dr. Caleb Alexander, an FDA adviser<br />
who recommended against the drug’s<br />
approval, said he was “surprised and<br />
disappointed” by the decision.<br />
“The FDA gets the respect that it does<br />
because it has regulatory standards that<br />
are based on firm evidence. In this case, I<br />
think they gave the product a pass,” said<br />
Alexander, a medical researcher at Johns<br />
Hopkins University.<br />
The FDA’s top drug regulator<br />
acknowledged that “residual<br />
uncertainties” surround the drug, but<br />
said Aduhelm’s ability to reduce harmful<br />
clumps of plaque in the brain is expected<br />
to help slow dementia.<br />
“The data supports patients and<br />
caregivers having the choice to use<br />
this drug,” Dr. Patrizia Cavazzoni<br />
told reporters. She said FDA carefully<br />
weighed the needs of people living with<br />
the “devastating, debilitating and deadly<br />
disease.”<br />
Under terms of the so-called accelerated<br />
approval, the FDA is requiring the<br />
drugmaker to conduct a follow-up<br />
study to confirm benefits for patients.<br />
If the study fails to show effectiveness,<br />
the FDA could pull the drug from the<br />
market, though the agency rarely does<br />
so.<br />
Biogen said the drug would cost<br />
approximately $56,000 for a typical<br />
year’s worth of treatment, and said the<br />
price would not be raised for four years.<br />
Most patients won’t pay anywhere near<br />
that amount thanks to insurance coverage<br />
and other discounts. The company said<br />
it aims to complete its follow-up trial of<br />
the drug by 2030.<br />
The non-profit Institute for Clinical and<br />
Economic Review said that “any price<br />
is too high” if the drug’s benefit isn’t<br />
confirmed in follow-up studies.<br />
Some 6 million people in the U.S. and<br />
many more worldwide have Alzheimer’s,<br />
which gradually attacks areas of the<br />
brain needed for memory, reasoning,<br />
communication and basic daily tasks.<br />
In the final stages of the disease, those<br />
afflicted lose the ability to swallow. The<br />
global burden of the disease, the most<br />
common cause of dementia, is only<br />
expected to grow as millions more baby<br />
boomers progress further into their 60s<br />
and 70s.<br />
Aducanumab (pronounced “add-yoo-<br />
CAN-yoo-mab”) helps clear a protein<br />
called beta-amyloid from the brain.<br />
Other experimental drugs have done<br />
that before but they made no difference<br />
in patients’ ability to think, care for<br />
themselves or live independently.<br />
The pharmaceutical industry’s drug<br />
pipeline has been littered for years<br />
with failed Alzheimer’s treatments.<br />
The FDA’s greenlight Monday is likely<br />
to revive investments in therapies<br />
previously shelved by drugmakers.<br />
The new medicine is manufactured from<br />
living cells and will be given via infusion<br />
at a doctor’s office or hospital.<br />
Researchers don’t fully understand what<br />
causes Alzheimer’s but there’s broad<br />
agreement the brain plaque targeted<br />
by aducanumab is just one contributor.<br />
Evidence suggests family history,<br />
education and chronic conditions like<br />
diabetes and heart disease may all play<br />
a role.<br />
“This is a sign of hope but not the final<br />
answer,” said Dr. Richard Hodes, director<br />
of the National Institute on Aging, which<br />
wasn’t involved in the Biogen studies<br />
but funds research into how Alzheimer’s<br />
forms. “Amyloid is important but not the<br />
only contributing factor.”<br />
Patients taking aducanumab saw their<br />
thinking skills decline 22% more slowly<br />
than patients taking a placebo.<br />
But that meant a difference of just 0.39<br />
on an 18-point score of cognitive and<br />
functional ability. And it’s unclear how<br />
such metrics translate into practical<br />
benefits, like greater independence or<br />
ability to recall important details.<br />
The FDA’s review of the drug has become<br />
a flashpoint in longstanding debates over<br />
standards used to evaluate therapies<br />
for hard-to-treat conditions. On one<br />
side, groups representing Alzheimer’s<br />
patients and their families say any new<br />
therapy — even one of small benefit —<br />
warrants approval. But many experts<br />
warn that greenlighting the drug could<br />
set a dangerous precedent, opening<br />
the door to treatments of questionable<br />
benefit.<br />
The approval came despite a scathing<br />
assessment in November by the FDA’s<br />
outside panel of neurological experts.<br />
The group voted “no” to a series of<br />
questions on whether reanalyzed data<br />
from a single study submitted by Biogen<br />
showed the drug was effective.<br />
Biogen halted two studies in 2019<br />
after disappointing results suggested<br />
aducanumab would not meet its goal of<br />
slowing mental and functional decline in<br />
Alzheimer’s patients.<br />
Several months later, the company<br />
reversed course, announcing that a new<br />
analysis of one of the studies showed the<br />
drug was effective at higher doses and<br />
The FDA isn’t required to follow the<br />
advice of its outside panelists and has<br />
previously disregarded their input when<br />
making similarly high-profile drug<br />
decisions.<br />
About 600 U.S. medical specialists<br />
already prescribe the drug through<br />
Biogen’s studies and many more are<br />
expected to begin offering it. Many<br />
practical questions remain unanswered:<br />
How long do patients benefit? How<br />
do physicians determine when to<br />
discontinue the drug? Does the drug<br />
have any benefit in patients with more<br />
advanced dementia?<br />
With FDA approval, aducanumab<br />
is certain to be covered by virtually<br />
all insurers, including Medicare, the<br />
government plan for seniors that covers<br />
more than 60 million people.<br />
Even qualifying for the drug could be<br />
expensive. It’s only been tested in people<br />
with mild dementia from Alzheimer’s<br />
or a less severe condition called mild<br />
cognitive impairment. To verify a<br />
diagnosis could require brain scans that<br />
cost $5,000 or more. Insurers, including<br />
Medicare, don’t cover the scans because<br />
their benefits are unclear, but that could<br />
change if the scans become a gateway to<br />
treatment.<br />
Additional scans will be needed to<br />
monitor potential side effects. The drug<br />
carries a warning about temporary brain<br />
swelling that can sometimes cause<br />
headaches, confusion and dizziness.<br />
Other side effects included allergic<br />
reactions, diarrhea and disorientation.<br />
For patients in Biogen’s studies, the<br />
decision means they can continue taking<br />
a drug many believe has helped.<br />
Kevin Bonham was diagnosed with<br />
early onset Alzheimer’s in 2016 after<br />
having difficulties with memory, reading<br />
and driving. The 63-year-old from Bear<br />
Creek Village, Pennsylvania, credits the<br />
drug with helping him keep his job as a<br />
mapmaker for another three years.<br />
“Very quickly over a period of months it<br />
was like the fog was lifted from the top<br />
of my head,” said Bonham, who is now<br />
on disability and relies on his wife, Kim,<br />
to help care for him and his teenage<br />
daughter.<br />
Like other trial participants, Bonham<br />
had to stop taking aducanumab in March<br />
2019 after Biogen halted its trials. He<br />
resumed infusions nearly a year ago as<br />
part of the company’s ongoing research.