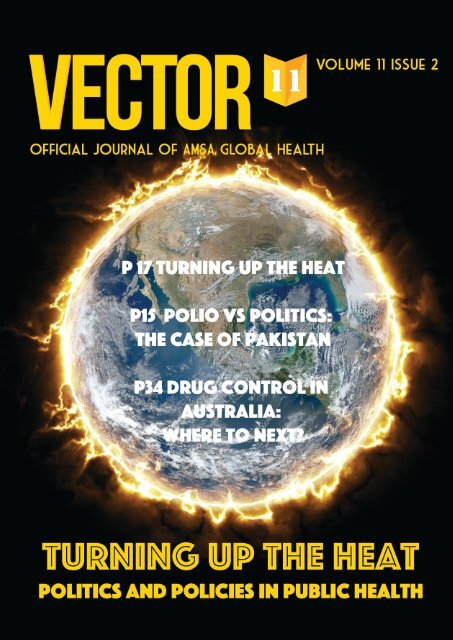
Vector Volume 11 Issue 2 - 2017
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
1
Advisory Board<br />
The Advisory Board, established in <strong>2017</strong>, consists of academic mentors who provide guidance for the present and future<br />
direction of <strong>Vector</strong>.<br />
Dr Claudia Turner<br />
Consultant paediatrician and clinician scientist with the University of Oxford & Chief Executive Officer of Angkor Hospital for<br />
Children.<br />
Professor David Hilmers<br />
Professor in the Departments of Internal Medicine and Pediatrics, the Center for Global Initiatives, and the Center for Space<br />
Medicine at the Baylor College of Medicine<br />
Associate Professor Nicodemus Tedla<br />
Associate Professor at the University of New South Wales School of Medical Sciences<br />
Dr Nick Walsh<br />
Medical Doctor (RACP) & Regional Advisor for Viral Hepatitis at the Pan American Health Organization / World Health<br />
Organization Regional Office for the Americas<br />
Thank you to the <strong>Vector</strong> Journal peer reviewers for <strong>2017</strong>:<br />
Dr Phil Baker<br />
Dr Denton Callander<br />
Professor Nicholas Crofts<br />
Dr Greg Fox<br />
Dr Alexandra Gibson<br />
Dr Max Hopwood<br />
Ms Alexandra Jones<br />
Dr Erik Martin<br />
Dr Bridianne O’Dea<br />
Dr Dominique Martin<br />
Professor Geetha Ranmuthugala<br />
Dr Mitchell Smith<br />
Dr Adrienne Torda<br />
Dr Leonie Watterson<br />
Professor Bridget Wills<br />
<strong>2017</strong> <strong>Vector</strong> Committee<br />
Editor-in-chief<br />
Carrie Lee carrie.lee@amsa.org.au<br />
Associate Editors<br />
Kryollos Hanna Sophie Lim Koshy Matthew Nic Mattock Aidan Tan<br />
Ash Wilson-Smith Sophie Worsfold Danica Xie<br />
Publication Designer<br />
Lucy Yang<br />
Design and layout<br />
© <strong>2017</strong>, <strong>Vector</strong><br />
Australian Medical Students’ Association Ltd, 42 Macquarie Street, Barton ACT 2600<br />
vector@globalhealth.amsa.org.au<br />
vector.amsa.org.au<br />
Content<br />
© <strong>2017</strong>, The Authors<br />
Cover design image accessed from https://pixabay.com/p-2349893/?no_redirect<br />
<strong>Vector</strong> Journal is the official student-run journal of AMSA Global Health.<br />
Responsibility for article content rests with the respective authors. Any views contained within articles are those of the authors and do not necessarily<br />
reflect the views of the <strong>Vector</strong> Journal or the Australian Medical Students’ Association.<br />
i
Contents<br />
Editor’s Note: Turning Up the Heat 1<br />
Features<br />
Non-Health for Non-Persons: Rohingya Muslims in Crisis 2<br />
Jumaana Abdu<br />
LGBTIQ people’s experiences of and barriers to healthcare 5<br />
Salwa Barmaky and Alex Lee<br />
Commercial surrogacy in Australia: the benefits of harm minimisation through legalisation 10<br />
Keyur Doolabh and Emily Feng-Gu<br />
Polio vs Politics: The Case of Pakistan 15<br />
Jeanine Hourani<br />
Turning up the heat 17<br />
Tara Kannan<br />
Coal mining, climate change and the global impacts on health: examining Adani’s proposed Carmichael coal mine 21<br />
John E Morgan<br />
Paddling upstream: Experiences from a medical placement in rural Papua New Guinea 26<br />
Nicholas Snels<br />
Reviews<br />
Sugar tax: a sweet solution for obesity? 29<br />
Saiuj Bhat<br />
Drug control in Australia: where to next? 34<br />
Raquel Maggacis<br />
Dengue in the Pacific Islands 38<br />
Madeleine Marsland and Dunya Tomic<br />
Conference reports<br />
AIDA <strong>2017</strong> - Family, Unity and Success 44<br />
Narawi Foley Boscott<br />
World Congress on Public Health 47<br />
Michael Au, Ka Man Li, Helena Qian, Michael Wu<br />
Commentary<br />
Welfare cuts to refugees 50<br />
AMSA Global Health Crossing Borders National Managers Sibella Breidahl, Jasmine Sekhon<br />
GHC <strong>2017</strong><br />
Start where you are, use what you have, do what you can - Adelaide Global Health Conference <strong>2017</strong> Closing<br />
Address 52<br />
Liz Bennett, AMSA Global Health Chair <strong>2017</strong><br />
GHC Competition Winner: “Where to now?” 54<br />
Helena Qian<br />
Book review<br />
A walk to remember 55<br />
Anna Marie Plant<br />
ii
Editor’s Note- Turning up the heat<br />
Global health is intrinsically linked to the changing social,<br />
economic, cultural and political environment. Political leaders<br />
powerfully shape responses to global health, whether in a<br />
positive or negative way. Historically, when health issues<br />
have risen on the political agenda, they received greater<br />
media attention, and importantly, funding – the HIV/AIDS<br />
epidemic exemplifies this. The change in leadership in the<br />
World Health Organization under the new Director-General Dr<br />
Tedros offers new opportunities to advocate for issues such<br />
as universal health coverage, women’s health and rights, and<br />
climate health.<br />
However, like many others, I find myself disappointed<br />
by the lack of political will to assist refugees and people<br />
seeking asylum. This is an ongoing problem, in Australia with<br />
the recent welfare cuts to refugees, described by Sibella<br />
Briedahl and Jasmine Sekhon (pg 2) , and internationally,<br />
with the plight of the stateless Rohingya people fleeing<br />
persecution in Myanmar, in a feature article by Jumaana Abdu<br />
(pg 50).<br />
Over the past year, controversial policies have dominated<br />
public health discourse on both a national and international<br />
scale. Non-communicable diseases continues to rise on<br />
the agenda. A tax set to cut sugar-sweetened beverage<br />
consumption takes a step towards tackling Big Sugar in the<br />
footsteps of movements against Big Tobacco, as covered in<br />
a review by Saiuj Bhat (pg 29).<br />
In Australia, we have also seen pushes for safe injecting<br />
rooms and pill testing at festivals. Does this reflect the<br />
global shift in attitudes from criminalisation towards harm<br />
minimisation, with decriminalisation in Portugal providing<br />
successful proof-of-concept? Raquel Maggacis overviews<br />
drug control approaches worldwide, arguing that Australia<br />
should adopt a harm minimisation approach (pg 34).<br />
Global health does not obey borders, and health policies<br />
have far-reaching effects. Infectious diseases certainly<br />
require no passport to spread from country to country,<br />
and Madeleine Marsland and Dunya Tomic highlight the<br />
importance of strong regional surveillance systems and<br />
prevention strategies (pg 38) Moreover, so long as one child<br />
has polio, all countries remain at risk, as described by Jeanine<br />
Hourani (pg 19). However, polio eradication in Pakistan, one<br />
of the last remaining polio-endemic countries, is incredibly<br />
complex due to political instability and competing agendas.<br />
Local policies certainly have broader international<br />
consequences, and Keyur Doolabh and Emily Feng-Gu<br />
explore issues around commercial surrogacy such as<br />
exploitation in countries where surrogacy is cheaper or<br />
poorly regulated (pg 10). Similar to drug control approaches,<br />
a harm minimisation approach may offer a better alternative<br />
to regulate processes and protect the rights of parents and<br />
children.<br />
Other contentious topics in Australia include the Adani<br />
coal mine and the postal vote for same sex marriage. These<br />
will have significant implications both now and in the future.<br />
With the recent postal vote, the mental health and wellbeing<br />
of LGBTIQA+ people could not be of more relevance.<br />
However, as Salwa Barmaky and Alex Lee write, LGBTIQA+<br />
people also face barriers in access to healthcare, including<br />
discrimination from the medical profession itself (pg 5).<br />
Aboriginal and Torres Strait Islander people also<br />
experience discrimination within the health care system,<br />
as Narawi Foley-Boscott explains (pg 44). So what then is<br />
the way forward for such issues? Both authors emphasise<br />
the importance of educating medical professionals to be<br />
culturally sensitive, to be open to learning, and to be aware of<br />
the structural factors that contribute to discrimination.<br />
Evan Morgan (pg 21) argues that the Adani coal mine<br />
endangers our health and the environment and is a poor<br />
investment for tax-payers. It hinders Australia’s ability to fulfil<br />
its global commitments under the Paris Agreement to reduce<br />
carbon emissions and temperature rises.<br />
Divestment offers a solution to climate change: take money<br />
away from the fossil fuel industry. We, as medical societies<br />
and the future medical profession, have an important role to<br />
add to this social movement, as thoughtfully argued by Tara<br />
Kannan (pg 17) The title of her article, “Turning up the heat”,<br />
captures the energy that connects the articles in this issue, a<br />
panoramic range of contemporary and controversial issues.<br />
It calls on us to take action and to challenge the paradigm of<br />
seeing health as purely a biomedical issue, but one inherently<br />
connected to regional and international social and political<br />
forces.<br />
As medical students, we are well-placed to educate<br />
and upskill ourselves to contribute to global health in the<br />
future. Attend conferences (Australian Indigenous Doctors’<br />
Association, pg 44 World Congress of Public Health, pg<br />
47. Take elective placements in developing countries, and<br />
prepare yourself with pre-departure training (Nicholas Snels,<br />
pg 26 ). As yourself, what can we do about these global health<br />
issues? (Helena Qian, pg 54)<br />
One of the statements that left a lasting impression on<br />
me from this year’s Global Health Conference was from the<br />
AMSA Global Health Chair, Liz Bennett: “It is not enough to be<br />
inspired... We do not have the luxury of apathy and you cannot<br />
afford to waste time thinking that you are too small to make<br />
a difference.” (pg 52).<br />
I am continually amazed and grateful to the incredible<br />
work of the authors, editorial team, peer reviewers and<br />
Advisory Board. It has been a privilege and a half to lead<br />
<strong>Vector</strong> Journal this year and hope that this issue inspires you<br />
and challenges you to take action.<br />
Carrie Lee<br />
Editor-in-chief, <strong>2017</strong><br />
1
Non-Health for Non-Persons:<br />
Rohingya Muslims in Crisis<br />
[Feature article]<br />
Jumaana Abdu<br />
Jumaana is currently finishing her first year of medicine at the University of New South Wales.<br />
She aims to find a career path which combines her passion for medicine and human rights.<br />
She also hopes her future involves as a side-profession of writing, fiction or otherwise.<br />
In a tightening spiral of human suffering that winds<br />
back five decades, the Rohingya have come to be<br />
mentioned as a customary precursor to the phrase “most<br />
persecuted minority in the world”. The long-disowned<br />
nationals of Myanmar are estimated at a population<br />
of 1.2 million,[1] stateless victims of humanitarian<br />
violations so comprehensive and extensive that the<br />
world’s empathy can only be directed towards a vague<br />
fog of injustice. However, as flagbearers of the right to<br />
health and human dignity, healthcare professionals must<br />
be able to shine a torch into the fog and discern the<br />
faces within.<br />
Current Situation<br />
While systematic persecution of the Rohingya Muslims<br />
has been noted since the stripping of voting rights and<br />
the military “purges” of the 1970s, events within the past<br />
year have seen violence escalate dramatically. A border<br />
attack by a group of radicalised Rohingya Muslims on<br />
Myanmar’s police last October resulted in an estimated<br />
10 casualties. Extremist violence is unacceptable and<br />
unhelpful, though one can see the desperation, injustice<br />
and generations-worth of marginalisation from which<br />
this radicalisation was inevitably born. Since the attack,<br />
disproportionate and indiscriminate military retaliation<br />
has resulted in hundreds of deaths and torrents of<br />
Rohingya fleeing Myanmar’s northern Rakhine state,<br />
where the situation is worst. The United Nations (UN)<br />
reports that from the last week of October <strong>2017</strong> to the<br />
first week of September <strong>2017</strong> alone – just two weeks –<br />
270,000 people fled to Bangladesh for safety.[2]<br />
The humanitarian crisis in which the Rohingya find<br />
themselves is undeniable. Officially stateless, access<br />
to basics such as healthcare, education, employment,<br />
security and freedom is often impossible. Tragically,<br />
these deprivations are far less confronting than other<br />
reasons for which the Rohingya have been forced to flee.<br />
With UNHCR reports documenting common experiences<br />
2
of “mass gang-rape, killings, including of babies and<br />
young children, brutal beatings, disappearances and<br />
other serious human rights violations by the country’s<br />
security forces”, returning to Myanmar is not an option.[3]<br />
UNHCR interviews with<br />
Rohingya refugees detail random<br />
shooting at crowds who were<br />
fleeing houses, schools, mosques<br />
and markets that had been set<br />
alight by Myanmar’s army, police<br />
and occasionally civilian mobs.[4]<br />
Destruction of food, livestock and<br />
food sources; cases where the army or Rakhine civilians<br />
have trapped an entire family, including the elderly and<br />
disabled, inside a house and set it on fire “killing them all”;<br />
mothers assaulted by “security” forces while being forced<br />
to watch their babies stabbed and killed – words cannot<br />
do it justice.[4]<br />
Recent news reveals that Burmese officials have<br />
planted landmines along the Bangladesh border, posing<br />
a lethal threat to Rohingya peoples fleeing atrocities.<br />
Deemed unlawful for their inability to distinguish between<br />
civilians and militants, children and adults, landmines have<br />
been banned in many countries under the 1997 Mine Ban<br />
Treaty. Not a signatory to this, Myanmar officials continue<br />
to use them against Rohingya civilians, protected by the<br />
unsurprising denial by the Burmese government that such<br />
landmine plantings have taken place.<br />
An assortment of condemnations have been offered<br />
by the UN; crimes against humanity,[3] genocide, ethnic<br />
cleansing. The UN High Commissioner for Human<br />
Rights Zeid Ra’ad Al Hussein, concludes his report on<br />
the Myanmar atrocities by despairing, “What kind of<br />
‘clearance operation’ is this? What national security<br />
goals could possibly be served by this?”.[3] As Hussein<br />
seems painfully aware, these words fall on deaf ears.<br />
Medical Crisis<br />
Humanitarian agencies are floundering, desperately<br />
attempting to provide emergency care for the monsoonal<br />
influx of Rohingya refugees, most of whom have a variety<br />
of physical and psychological conditions. Studies of the<br />
health conditions within Bangladesh’s two main registered<br />
refugee camps present unsurprisingly dire findings.<br />
One psychiatric study surveyed a group of registered<br />
Rohingya refugees and reported experiences of torture<br />
(39.9%), sexual abuse (12.8%), rape (8%), forced<br />
abortions (2.4%), PTSD (36%), depressive symptoms<br />
(89%), suicidal ideations (19%) and deaths of friends or<br />
family due to illness or starvation while fleeing (22.4%).<br />
[5] Hopelessness was the common theme, with one<br />
Rohingyan interviewee asking, “Our future has been<br />
spoiled, but what will happen to the future of our children?”<br />
Hopelessness was the common theme,<br />
with one Rohingyan interviewee asking,<br />
“Our future has been spoiled, but what<br />
will happen to the future of our children?”<br />
In 2015, another study investigated the general health<br />
conditions of Bangladesh’s largest Rohingya refugee<br />
camp, Nayapara.[1] With a population of 18,777, the camp<br />
was attended by only four trained doctors and six nurses.<br />
The infant mortality rate was 45.4 per 1000 livebirths and<br />
one quarter of the population was<br />
children, most of whom were born<br />
in a camp. Additionally, the study<br />
reported widespread stunting due<br />
to malnutrition (57%), anaemia<br />
(49%), and a high prevalence of<br />
respiratory (46.9%), endocrine<br />
(21.9%) and cardiovascular<br />
disorders (14.8%). Mental health<br />
conditions were ubiquitously poor; 18.7% of camp<br />
injuries were caused by self-harm, and in Bangladesh’s<br />
other major camp, 43.3% of Rohingya refugees were<br />
diagnosed with a psychotic disorder.<br />
Importantly, health conditions in registered refugee<br />
camps far surpass those of the many unregistered camps<br />
in countries neighbouring Myanmar. These makeshift<br />
shelters, which house twice as many Rohingya as the<br />
registered camps, are conferred no security or support<br />
from the already-drowning NGOs servicing the area.<br />
This, however, is still favourable to staying in the northern<br />
Rakhine state of Myanmar where health conditions are<br />
so abysmal that, for example, mortality in children under 5<br />
has reached 224 per 1000 livebirths.[6]<br />
Role of Health Professionals in Social Justice<br />
In situations where political and military injustice<br />
seem impenetrable, often the most basic human<br />
right affordable is emergency medical care, but is the<br />
assumption that medical aids are exempt from political<br />
and military violence still applicable today? As seen<br />
in reports of hospitals targeted in Syria by Western<br />
military, it seems that medical neutrality is no longer a<br />
guarantee. Combined with the Myanmar government’s<br />
notoriously uncooperative relationship with humanitarian<br />
organisations, one must ask what responsibility<br />
healthcare professionals are expected to bear in the<br />
realm of human rights.<br />
In 2014, Médecins Sans Frontières was banned<br />
in Rakhine, and a month later, when humanitarian aid<br />
agencies were attacked by Buddhist anti-Rohingya<br />
radicals, Myanmar’s government only further restricted<br />
humanitarian aid.[6] This ban has since been lifted<br />
but access is now parlous again due to the Myanmar<br />
government’s “formulated and disseminated accusations<br />
against the UN and international NGOs, denial of required<br />
travel and activity authorisations, and threatening<br />
statements and actions by hardline groups”.[7] Also<br />
recently, the UNHCR High Commissioner Hussein has<br />
struggled with repeated government restrictions on<br />
humanitarian access to the worst affected regions of<br />
Rakhine, and bans on UN investigative officials entering<br />
3
Rohingyan regions of Myanmar. Forced to work within the<br />
law, the UN can only deploy officers to the Bangladeshi<br />
border.[2]<br />
These tensions between humanitarian aid and the<br />
state beg the question: in health emergencies and human<br />
rights violations as staggering as those experienced by<br />
the Rohingya Muslims, should human rights and healthcare<br />
organisations bend to the will of unjust – even criminal –<br />
governments? It is a problem the UN and its subcommittee,<br />
the World Health Organization, still grapple with. Do they<br />
obey their mandate to respect the sovereignty of their<br />
member states? Or do they perform their constitutional<br />
role of helping member states “respond to... emergencies<br />
with public health consequences”?[8] How can they, when<br />
the member state itself is perpetuating the emergency?<br />
Additionally, the aforementioned lack of confidence in<br />
medical neutrality makes it unsafe for health workers to<br />
stand against government and military opposition.<br />
The only solution where a full response to this<br />
... should human rights and healthcare<br />
organisations bend to the will of unjust –<br />
even criminal – governments?<br />
humanitarian crisis can be appropriated lies in either<br />
cooperation with Myanmar’s government – which seems<br />
unlikely – or direct actions against the government by<br />
UN member states. Ideally, the Burmese government<br />
would grant the Rohingya some form of internationally<br />
recognised citizenship, allowing for better organisation<br />
of refugee status and resettlement programs for the<br />
Rohingya in neighbouring countries. Sanctions intended<br />
to force the Burmese government’s hand have failed in<br />
the past,[6] but if the global community can unite with<br />
harsher repercussions for the continued persecution of<br />
Rohingya Muslims, surely the situation can only improve.<br />
Conclusion<br />
The Rohingya peoples are born into a cycle of<br />
poor health outcomes that begin with low birthweight<br />
and continue with dismal access to healthcare. Timid<br />
international responses to the systematic abuse, torture<br />
and dehumanisation of this minority have allowed for the<br />
continuation of historical persecution. The 2015 election<br />
of Nobel Prize laurate Aung San Suu Kyi as Myanmar’s<br />
Prime Minister presented an opportunity for a Myanmar<br />
government to end their denial and dismissal of decades<br />
of Rohingyan suffering. However, as stated by her aide,<br />
it seems she has “other priorities”,[6] which probably<br />
includes avoiding conflict with her majority-Buddhist<br />
supporters and the hugely politically influential Burmese<br />
military. For now, Rohingya Muslims will have to continue<br />
to relying on NGOs who are drowning under resource<br />
insufficiencies and legal restrictions, attempting to deal<br />
with the desperate masses in any way possible.<br />
History paints a picture of peaceful generations<br />
of Rohingya living in Myanmar. Their future seems<br />
increasingly uncertain, although ideally it involves them<br />
returning safely home. One and a half million people await<br />
a saving grace, security for their children, medicine, clean<br />
water. If international global health organisations cannot<br />
work within Myanmar’s policies, then they must find a<br />
conclusive alternative. It is unacceptable that there is still<br />
not a light at the end of this half-a-century long tunnel.<br />
Photo credit<br />
EU/ECHO/Pierre Prakash<br />
Accessed from https://www.flickr.com/photos/eu_<br />
echo/17337141093/in/photostream/<br />
Conflicts of interest<br />
None declared<br />
Correspondance<br />
jumaana.a6000@gmail.com<br />
References<br />
1. Milton, A. H., Rahman, M., Hussain, S., Jindal, C., Choudhury,<br />
S., Akter, S., ... & Efird, J. T. (<strong>2017</strong>). Trapped in Statelessness:<br />
Rohingya Refugees in Bangladesh. International Journal of<br />
Environmental Research and Public Health, 14(8).<br />
2. United Nations (<strong>2017</strong>). UN scales up response as<br />
270,000 flee Myanmar into Bangladesh in two weeks. Retrieved<br />
from http://www.un.org/apps/news/story.asp?NewsID=57480#.<br />
WbZ6eK2B3Vo<br />
3. United Nations (<strong>2017</strong>). UN report details ‘devastating<br />
cruelty’ against Rohingya population in Myanmar’s Rakhine<br />
province. Retrieved from http://www.un.org/apps/news/story.<br />
asp?NewsID=56103#.WbZ4w62B3Vp<br />
4. OHCHR Zeid Ra’ad Al Hussein (<strong>2017</strong>). Interviews with<br />
Rohingyas fleeing from Myanmar since 9 October 2016.<br />
Retrieved from http://www.ohchr.org/Documents/Countries/MM/<br />
FlashReport3Feb<strong>2017</strong>.pdf<br />
5. Riley, A., Varner, A., Ventevogel, P., Taimur Hasan, M. M.,<br />
& Welton-Mitchell, C. (<strong>2017</strong>). Daily stressors, trauma exposure,<br />
and mental health among stateless Rohingya refugees in<br />
Bangladesh. Transcultural Psychiatry, 54(3), 304-331.<br />
6. Mahmood, S. S., Wroe, E., Fuller, A., & Leaning, J. (<strong>2017</strong>).<br />
The Rohingya people of Myanmar: health, human rights, and<br />
identity. The Lancet, 389(10081), 1841-1850.<br />
7. Médecins Sans Frontières (<strong>2017</strong>). Myanmar:<br />
International humanitarian access to Rakhine State must<br />
urgently be permitted. Retrieved from http://www.msf.org/en/<br />
article/myanmar-international-humanitarian-access-rakhinestate-must-urgently-be-permitted<br />
8. Kennedy, J., & McCoy, D. (<strong>2017</strong>). WHO and the health<br />
crisis among the Rohingya people of Myanmar. The Lancet,<br />
389(10071), 802-803.<br />
4
LGBTIQ people’s experiences of and<br />
barriers to healthcare<br />
[Feature Article]<br />
Salwa Barmaky and Alexander Lee<br />
Salwa is a fourth year medical student at the University of New South Wales. and a public<br />
health enthusiast, especially interested in health disparities and programme interventions.<br />
Alexander is an undergraduate medical student currently studying at the University of New<br />
South Wales. His interests include improving healthcare access for marginalised populations<br />
including gender and sexuality diverse groups and reproductive health.<br />
Introduction<br />
Increasing data on sexual orientation and gender<br />
identities in large scale social studies has revealed<br />
that significant portions of the Australian community<br />
are sexuality and/or gender diverse. In the 2014 ABS<br />
General Social Survey, 3% of the Australian population<br />
identified as not heterosexual,[1] and whilst Australian<br />
data is unavailable, a study of 8500 New Zealand<br />
secondary school students revealed that 1.2% identified<br />
as transgender.[2]<br />
LGBTQIA+ refers to lesbian, gay, bisexual,<br />
transgender, queer and questioning, intersex, asexual<br />
and aromantic individuals, with the ‘+’ connoting other<br />
diverse sexualities, sexes and genders. LGBTQIA+<br />
Australians continue to face significant barriers to care<br />
which in turn impact individuals’ help seeking behaviours.<br />
[3, 4]<br />
Until 1973, homosexuality was considered a mental<br />
disorder. Similarly, transgender and gender diverse (TGD)<br />
identities were classified as ‘gender identity disorder’<br />
until the 2013 edition of the Diagnostic & Statistical<br />
Manual (DSM-5) [4] and continues to<br />
be listed as such by the World Health<br />
Organization’s International Statistical<br />
Classification of Diseases and<br />
Related Health Problems (ICD-10).[5]<br />
Furthermore, access to hormonal and/<br />
or surgical intervention largely remains<br />
tied to gatekeeper models requiring<br />
TGD individuals to be ‘diagnosed’.[6, 7]<br />
Despite having been widely condemned as ineffective<br />
and causing significant psychological harm,[8, 9]<br />
pseudoscientific ‘gay conversion therapy’ continues to<br />
persist. Most recently, a New South Wales GP appearing<br />
in a ‘Vote No’ television campaign against same-sex<br />
marriage was identified as a founder of a ‘family values’<br />
Whilst questions such as<br />
“do you have a boyfriend/<br />
girlfriend?” seem innocent, they<br />
carry value judgements on what<br />
is considered ‘normal’.<br />
group advocating this practice. Many intersex individuals<br />
have also been subjected to risky, non-consensual<br />
genital mutilation surgery as infants in a bid to ‘normalise’<br />
them.[10] Furthermore, some clinicians expressly feel<br />
awkward treating LGBTQIA+ individuals.[<strong>11</strong>] Hence, to<br />
effectively advocate for greater inclusivity and equity, it<br />
is paramount that health professionals understand both<br />
current and historical healthcare barriers as well as the<br />
specific health concerns of LGBTQIA+ communities<br />
As such, this article will outline:<br />
1) Effects of individual, interpersonal and structural<br />
social determinants of health on healthcare access for<br />
LGBTQIA+ individuals;<br />
2) Key health issues affecting LGBTQIA+ individuals;<br />
and<br />
3) Recommendations for improving access.<br />
Social determinants of healthcare access for<br />
LGBTQIA+ individuals<br />
Despite the acronym LGBTQIA+ construing<br />
homogeneity, LGBTQIA+ communities are distinctly<br />
heterogeneous. Individuals may have different<br />
experiences of their identity and come from different<br />
social contexts such as ethnic<br />
background or socioeconomic<br />
class.[12] However, they do share a<br />
continued exposure to societal stigma<br />
associated with their diverse identities.<br />
This stigma plays into all levels of the<br />
social determinants of health which in<br />
turn impact both individuals’ health and<br />
healthcare access. These include individual internalised<br />
shame, interpersonal discrimination and ignorance and<br />
structural legal, administrative and systemic challenges.<br />
These determinants limit LGBTQIA+ Australians’<br />
confidence in our healthcare system.<br />
5
Individual and interpersonal<br />
While accessing healthcare, LGBTQIA+ individuals<br />
face interpersonal barriers in the form of clinicians’ lack<br />
of knowledge and discrimination as well as their own<br />
individual internalised homophobia.<br />
DSM-5 now allows for self-identification as asexual as<br />
an alternative to diagnosis with ‘hypoactive sexual desire<br />
disorder’ or ‘female sexual arousal/interest disorder’ [25],<br />
historically, a lack of interest in sex has been pathologised<br />
by Western medicine.[26]<br />
Many practitioners have limited training and<br />
awareness around the importance of comprehensive,<br />
non-judgmental sexual history taking. Clinicians’<br />
unconscious biases often result in LGBTQIA+ clients<br />
being forced to ‘out’ themselves in response to questions<br />
that assume heterosexuality and do not recognise<br />
gender diverse or intersex experiences (e.g. asking a<br />
trans woman about birth control). This exacerbates<br />
existing awkwardness around sexual and mental health<br />
and is associated with significant discomfort, which<br />
may contribute to patients’ decisions<br />
not to disclose their sexuality or gender<br />
identity.[13] Additionally, some GPs did not<br />
understand different sexual practices and<br />
felt uncomfortable broaching the topic.<br />
[14] One third of LGBTQ* Australians<br />
still hide their sexuality or gender identity<br />
when accessing healthcare.[15] In youths, half did not<br />
disclose.[16] This not only impacts individuals’ ability to<br />
build trust with healthcare providers but also undermines<br />
the provision of targeted health services such as human<br />
immunodeficiency virus (HIV) testing in men who have sex<br />
with men (MSM).<br />
Healthcare providers’ lack of knowledge regarding<br />
TGD identities and unique health needs is a common<br />
theme.[17-20] Having to educate healthcare providers<br />
was found to be a key contributor to negative GP<br />
encounters in Australia.[17] A lack of sensitivity [19, 20]<br />
with practitioners asking invasive or offensive questions<br />
[17] and misgendering clients through the use of incorrect<br />
pronouns or old names [15, 21] contributes to these<br />
barriers. Clinicians not working in TGD-specific fields<br />
often have little knowledge on the issue, resulting in<br />
these clients’ exclusion from mainstream health services.<br />
[2, 15, 21] Even clinicians regularly engaged with TGD<br />
clients enlist gatekeeping behaviours which restricts<br />
access to hormonal and surgical intervention.[17, 22] This<br />
discourages TGD individuals from raising mental health<br />
concerns and many find this process of “assessment”<br />
to be degrading and pathologising.[21] Moreover, rigid,<br />
binary views of gender results in non-binary individuals<br />
feeling invisible and unwelcome to services.[23]<br />
LGBTI people in Australia<br />
are five times more likely to<br />
attempt suicide in their lifetimes<br />
Internalised homophobia may manifest as a further<br />
barrier to seeking healthcare services. Consequently,<br />
during periods of illness, individuals turn to pharmacies<br />
and only seek health services when self-medication has<br />
been unsuccessful.[27]<br />
Structural<br />
LGBTQIA+ communities also face a myriad of<br />
structural barriers to quality healthcare.<br />
Australia is currently the only<br />
Western country which requires TGD<br />
adolescents to gain Family Court<br />
‘approval’ to access hormones.<br />
Despite the time-sensitive nature of<br />
hormone therapy, the legal process<br />
can take up to 10 months, and cost<br />
tens of thousands of dollars.[28] However, this is currently<br />
under review by the Family Court.[29]<br />
TGD communities, especially non-binary individuals,<br />
also face inaccurate medical record keeping that do<br />
not reflect individual’s chosen names, genders and/or<br />
pronouns and a lack of gender-neutral bathroom access.<br />
[18, 23] Moreover, TGD individuals experience discomfort<br />
in gendered spaces such as gynaecologists’ clinics [23]<br />
and heightened discomfort surrounding pap smears and<br />
breast checks.[18, 22] The relegation of TGD services to<br />
the realm of expensive private healthcare[15] is at heads<br />
with their increased risk of poverty, underemployment and<br />
housing instability.[18, 19, 23]<br />
Additionally, the view of LGBTQIA+ identities as<br />
inherently pathological by some providers is discriminatory.<br />
[13, 21, 24] TGD individuals may face clinician discomfort,<br />
disgust, ridicule, contempt and even refusal of treatment.<br />
[19, 21-23] One participant of the Australian and New<br />
Zealand TranZnation report was told by their doctor<br />
that she was ‘the filthiest, most perverted thing on earth’<br />
while another was informed they ‘needed to find god not<br />
hormones’.[21] Asexuality is also pathologised. While<br />
Furthermore, unconscious bias can also manifest<br />
in the distribution of research funding and practitioner<br />
training. Compared to the relative visibility of gay men’s<br />
health around the HIV/AIDS epidemic, TGD health as well<br />
as queer women’s health have largely been ignored.[13]<br />
6
Sexual health<br />
LGBTQIA+ individuals may also experience poorer<br />
sexual health. There is evidence to suggest that women<br />
who have sex with women (WSW) are at higher risk for<br />
cervical cancer.[32] Both patients and clinicians lack<br />
awareness around sexually transmitted infection (STI),<br />
specifically human papilloma virus (HPV), transmission<br />
during cisgender woman to woman sexual contact.<br />
Consequently, WSW are less likely to have Pap or other<br />
cervical smears.[33]<br />
Key LGBTQIA+ health issues<br />
Besides issues of access, LGBTQIA+ individuals have<br />
specific healthcare risks, needs and concerns. Pertinently,<br />
LGBTQIA+ individuals have significantly poorer mental<br />
and sexual health. They also have higher incidence of<br />
certain chronic diseases such as cardiovascular disease,<br />
asthma and diabetes.[30]<br />
Mental health<br />
Poorer mental health is one of the ways that stigma<br />
affects LGBTQIA+ individuals’ wellbeing. Compared to<br />
the general population, LGBTI people in Australia are<br />
five times more likely to attempt suicide in their lifetimes<br />
and more specifically, TGD-identifying individuals are<br />
eleven times more likely.[31] LGBT people are also twice<br />
as likely to be diagnosed and treated for mental health<br />
disorders, and 24.4% of LGBT people aged 16 and over<br />
currently meet the full criteria for a major depressive<br />
episode.[31]<br />
Reasons for poorer mental health are also based in<br />
internalised, inter-personal, organisational and structural<br />
stigma and discrimination.[31] These include: bullying at<br />
schools, lack of bullying laws, ostracism from families<br />
and faith communities, fear of employment and economic<br />
stability, and inner conflict and internalised phobia<br />
about their respective identities. LGBTQIA+ individuals<br />
also have higher risk for poor coping mechanisms and<br />
substance abuse.[32]<br />
In addition, MSM have greater incidence of HIV. In<br />
Australia, HIV transmission occurs primarily through<br />
male-to-male sex with 68% of new HIV diagnoses in 2015<br />
having been attributed to male-to-male sex.[34] Besides<br />
the greater susceptibility of anal mucosa, this increased<br />
incidence arises from the concentration of HIV within<br />
MSM sexual networks in Western nations.[35] Receptive<br />
anal intercourse in male-to-male sex may also increase<br />
risk of hepatitis B, HPV and herpes.[32] In NSW, MSM<br />
are also more likely to report ever having had an STI,<br />
particularly chlamydia, pubic lice, genital herpes, syphilis,<br />
anal warts and gonorrhoea.[36] As some of these STIs<br />
are risk factors for anal cancer, MSM are also at greater<br />
risk for anal cancer.[32] However, MSM are also more<br />
likely than any non-MSM to be tested for STIs.[36]<br />
Furthermore, poor data collection means that the<br />
sexual health of TGD populations in Australia remain<br />
poorly understood. The tendency to collapse TGD<br />
experiences into a single ‘third gender’ category ignores<br />
the vast differences in risk associated with different<br />
gender identities, sexual orientations and partners. For<br />
example, the Kirby Institutes’ 2016 annual report on<br />
STIs recorded sex as ‘male’, ‘female’ and ‘transgender/<br />
missing’.[37] This is particularly disappointing in the<br />
context of trans women in particular being significantly<br />
overrepresented in global HIV prevalence.[38]<br />
Aging<br />
Owing to Australia’s aging population, the issue of older<br />
Key messages<br />
• LGBTIQA+ people face barriers to healthcare access,<br />
historically influenced by discrimination from the medical profession<br />
• Health disparities exist between LGBTIQA+ individuals and<br />
the general population, particularly in the areas of mental health,<br />
sexual health and chronic disease<br />
• Further research and education, a collective effort to treat<br />
LGBTIQA+ people with individual respect, and a willingness to learn,<br />
will help to reduce health inequalities<br />
*In certain parts of this article, terms to refer to the sex, sexuality and gender diverse individuals may change dependent<br />
on the groups of people being researched in the various research articles cited.<br />
7
LGBTQIA+ individuals is topical. LGBTQIA+ individuals in<br />
aged care have specific care needs such as ongoing<br />
HIV/AIDS treatment and hormone therapy. Having lived<br />
through the criminalisation of homosexuality, many may<br />
be impacted by an internalised need to go ‘back into the<br />
closet’ for fear of discrimination.[39]<br />
Improving access<br />
To reduce the aforementioned barriers and risks,<br />
various areas can be improved. Institutionally, education<br />
around LGBTQIA+ issues of sexuality, gender diversity,<br />
access and risk should be integrated into the medical<br />
curriculum. Trainees should be taught to adopt<br />
non-judgmental approaches to history taking and<br />
communication.[16, 40] Whilst questions such as “do you<br />
have a boyfriend/girlfriend?” seem innocent, they carry<br />
value judgements on what is considered ‘normal’. Instead,<br />
more inclusive terminology should be encouraged to<br />
enable clinicians to invite discussion around sexual health<br />
without assuming heterosexuality or gender binaries.<br />
Encouragingly, previous efforts in introducing LGBTQIA+<br />
content through lectures and clinical simulations have<br />
been effective in decreasing at least clinician discomfort<br />
in providing LGBTQIA+ related care.[41-44]<br />
Clinicians should also create environments of<br />
inclusiveness. This includes respecting patients’ chosen<br />
pronouns and names, and keeping open minds about<br />
their relationships. This is imperative to building trust.<br />
Introducing intake forms that include diverse gender<br />
identities and LGBTQIA+ specific signage or educational<br />
brochures also increase patient comfort.[40] Additionally,<br />
revision of current data collection systems would enable<br />
more targeted healthcare delivery for TGD populations.<br />
This could be aided through mandatory recording of<br />
both sex assigned at birth and current gender identity<br />
which would enable the disaggregation of different TGD<br />
experiences.[45]<br />
Conclusion<br />
LGBTQIA+ people face on-going barriers to healthcare<br />
on individual, interpersonal and structural levels and have<br />
an increased risk of mental, sexual and chronic illnesses.<br />
Thus, in order to improve health outcomes, barriers to<br />
access should be targeted on both interpersonal and<br />
structural levels. Ultimately, treating LGBTQIA+ people<br />
with individual respect and a willingness to learn will go a<br />
long way in in reducing these inequities.<br />
Acknowledgements<br />
The authors acknowledge and thank Gale Chan for<br />
their contributions to the drafting and revising of this<br />
article.<br />
Photo credit<br />
©2008 laverrue, accessed from https://www.flickr.<br />
com/photos/23912576@N05/2942525739<br />
Ryan melaugh, accessed from https://www.flickr.com/<br />
photos/120632374@N07/13974181800<br />
Conflicts of interest<br />
None declared<br />
Correspondance<br />
salwasayeed70@hotmail.com<br />
alexanderlee193@gmail.com<br />
References<br />
1. Australian Bureau of Statistics. General Social Survey:<br />
Summary Results, Australia, 2014 2014 [cited <strong>2017</strong> September<br />
9]. Available from: http://www.abs.gov.au/ausstats/abs@.nsf/<br />
mf/4159.0.<br />
2. Clark TC, Lucassen MFG, Bullen P, Denny SJ, Fleming<br />
TM, Robinson EM, et al. The health and well-being of transgender<br />
high school students: Results from the New Zealand Adolescent<br />
Health Survey. Journal of Adolescent Health. 2014;55:93-9.<br />
3. Mulé NJ, Ross LE, Deeprose B, Jackson BE, Daley A,<br />
Travers A, et al. Promoting LGBT health and wellbeing through<br />
inclusive policy development. International Journal for Equity in<br />
Health. 2009;8(18).<br />
4. Potter J, Goldhammer H, Makadon M. Clinicians and the<br />
care of sexual minorities Potter J, Goldhammer H, Makadon M,<br />
Mayer K, editors. Philadelphia: American College of Physicians;<br />
2008.<br />
5. World Health Organisation. International Statistical<br />
Classification of Diseases and Related Health Problems 10th<br />
Revision 1992 [updated 2016. 10:[Available from: http://apps.<br />
who.int/classifications/icd10/browse/2016/en#/F60-F69.<br />
6. Australian and New Zealand Professional Association<br />
for Transgender Health. Standards of Care [Available from:<br />
http://www.anzpath.org/about/standards-of-care/.<br />
7. World Professional Association for Transgender Health.<br />
Standards of care for the health of transsexual, transgender<br />
and gender nonconforming people 20<strong>11</strong> [Available from: http://<br />
www.wpath.org/site_page.cfm?pk_association_webpage_<br />
menu=1351&pk_association_webpage=3926.<br />
8. Mayers L, Chow K. Same-sex marriage survey: Petition<br />
to deregister Pansy Lai, doctor in No campaign ad, taken down.<br />
ABC News. <strong>2017</strong>.<br />
9. Daniel H, Butkus R. Lesbian, Gay, Bisexual, and<br />
Transgender Health Disparities: Executive Summary of a Policy<br />
Position Paper From the American College of Physicians.<br />
Annals of Internal Medicine. 215(163):135 — 7.<br />
10. Minto CL, Liao L-M, Creighton SM, Woodhouse CRJ,<br />
Ransley PG. The effect of clitoral surgery on sexual outcome<br />
in individuals who have intersex conditions with ambiguous<br />
genitalia: A cross-sectional study. Lancet. 2003;361(9365):1252<br />
— 7.<br />
<strong>11</strong>. Smith D, Mattews W. Physicians’ attitudes toward<br />
homosexuality and HIV: a survey of a California medical Societyal<br />
of Homosexuality. Journal of Homosexuality. 2007;52(3/4):1 — 9<br />
12. Ard KL, Makadon HJ. Improving the health care of<br />
lesbian, gay, bisexual an transgender people: understanding<br />
and eliminating health disparities. Boston, Massachusetts: The<br />
Fenway Institutee; 2012.<br />
13. Australian Human Rights Commission. Resilient<br />
Individuals: Sexual Orientation, Gender Identity & Intersex<br />
Rights 2015.<br />
14. Hinchliff S, Gott M, Galena E. ‘I daresay I might find<br />
it embarrassing’: general practitioners’ perspectives on<br />
discussing sexual health issues with lesbian and gay patients.<br />
Health & Social Care in the Community. 2005;13(4):345.<br />
8
15. Leonard W, Pitts M, Mitchell A, Lyons A, Smith A, Patel S,<br />
et al. Private Lives 2: The second national survey of the health<br />
and wellbeing of gay, lesbian, bisexual and transgender (GLBT)<br />
Australians. Melbourne: The Australian Research Centre in Sex,<br />
Health & Society, La Trobe University; 2012.<br />
16. Robinson KH, Bansel P, Denson N, Ovenden G, Davies<br />
C. Growing Up Queer: <strong>Issue</strong>s Facing Young Australians Who Are<br />
Gender Variant and Sexuality Diverse. Melbourne Young and<br />
Well, Cooperative Research Centre 2014.<br />
17. Riggs DW, Coleman K, Due C. Healthcare experiences<br />
of gender diverse Australians: a mixed-methods, self-report<br />
survey. BMC Public Health. 2014;14(1):230.<br />
18. Roberts TK, Fantz CR. Barriers to quality health care for<br />
the transgender population. Clinical biochemistry. 2014;47(10-<br />
<strong>11</strong>):983-7.<br />
19. Safer JD, Coleman E, Feldman J, Garofalo R, Hembree<br />
W, Radix A, et al. Barriers to healthcare for transgender<br />
individuals. Current opinion in endocrinology, diabetes, and<br />
obesity. 2016;23(2):168-71.<br />
20. Snelgrove JW, Jasudavisius AM, Rowe BW, Head EM,<br />
Bauer GR. “Completely out-at-sea” with “two-gender medicine”:<br />
A qualitative analysis of physician-side barriers to providing<br />
healthcare for transgender patients. BMC Health Services<br />
Research. 2012;12(1):<strong>11</strong>0.<br />
21. Couch M, Pitts M, Mulcare H, Croy S, Mitchell A, Patel<br />
S. TranZnation: A report on the health and wellbeing of<br />
transgendered people in Australia and New Zealand Melbourne<br />
Australain Research Centre in Sex, Health & Society, La Trobe<br />
University 2007.<br />
22. Pitts M, Couch M, Croy S, Mitchell A, Hunter M. Health<br />
service use and experiences of transgender people: Australian<br />
and New Zealand Perspectives Gay & Lesbian <strong>Issue</strong>s and<br />
Psychology. 2009;5(3):167-76.<br />
23. Mogul-Adlin H. Unanticipated: Healthcare Experiences of<br />
Gender Nonbinary Patients and Suggestions for Inclusive Care.<br />
United States, Connecticu: Yale University; 2015.<br />
24. Transgender and Gender Diverse Health and Wellbeing:<br />
Background paper. Victoria Gay, Lesbian, Bisexual, Transgender<br />
and Intersex Health and Wellbeing Ministerial Advisory<br />
Committee, ; 2014.<br />
25. Bogaert A. Asexuality: What It Is and Why It Matters. The<br />
Journal of Sex Research. 2015;52(4):362-79.<br />
26. Gupta K. “And Now I’m Just Different, but There’s<br />
Nothing Actually Wrong With Me”: Asexual Marginalization and<br />
Resistance. Journal of Homosexuality. <strong>2017</strong>;64(8):991-1013.<br />
27. Alencar Albuquerque G, De Lima Garcia C, Da Silva<br />
Quirino G, Alves MJH, Belém JM, Dos Santos Figueiredo FW,<br />
et al. Access to health services by lesbian, gay, bisexual,<br />
and transgender persons: systematic literature review. BMC<br />
international health and human rights. 2016;16(2):22.<br />
28. Taylor J. Chief Justice vows change to ‘traumatic’ court<br />
process for transgender children. ABC News. 2016.<br />
29. Ryan E. Access to justice for young transgender<br />
Australians: Laywers Weekly <strong>2017</strong> [Available from: https://www.<br />
lawyersweekly.com.au/opinion/2<strong>11</strong>01-access-to-justice-foryoung-transgender-australians.<br />
30. Bolderston A, Ralph S. Improving the health care<br />
experiences of lesbian, gay, bisexual and transgender patients.<br />
Radiography. 2016;22:207 — <strong>11</strong>.<br />
31. Alliance NLH. Snapshot of mental health and suicide<br />
prevention statistics for LGBTI people. National LGBTI Health<br />
Alliance; 2016.<br />
32. Lee R. Health care problems of lesbian, gay, bisexual,<br />
and transgender patients. The Western Journal of Medicine.<br />
2000;172(6):403 — 8.<br />
33. Curmi C, Peters K, Salamonson Y. Lesbians’ attitudes<br />
and practices of cervical cancer screening: a qualitative study.<br />
BMC Women’s Health. 2014;14(153).<br />
34. The Kirby Institute. HIV, viral hepatitis and sexually<br />
transmissible infections in Australia. The Kirby Institute; 2016.<br />
35. Amirkhanian YA. Social Networks, Sexual Networks and<br />
HIV Risk in Men Who Have Sex with Men. Current HIV/AIDS<br />
reports. 2014;<strong>11</strong>(1):81-92.<br />
36. Richters J, Zou H, Yeung A, Caruana T, O de Visser R,<br />
Rissel C, et al. Sexual health and behaviour of men in New South<br />
Wales 2013–2014. School of Public Health and Community<br />
medicine 2015.<br />
37. The Kirby Institute. HIV, viral hepatitis and sexually<br />
transmissible infections in Australia Annual Surveillance Report<br />
2016. Sydney, Sydney NSW 2052: The Kirby Institute<br />
38. Groves A. Transgender women and HIV: A footnote to the<br />
epidemic. HIV Australia. 2012;9(4):30-2.<br />
39. Australian Department of Health and Aging. National<br />
Lesbian, Gay, Bisexual, Transgender and Intersex (LGBTI):<br />
Ageing and Aged Care Strategy. 2012.<br />
40. Ard KL, Makadon HJ. Improving the Health Care of<br />
Lesbian, Gay, Bisexual and Transgender People: Understanding<br />
and Eliminating Health Disparities Boston, MA: The National<br />
LGBT Health Education Center; 2012.<br />
41. Arora M, Walker K, Duvivier RJ, Wynne K. Transgender<br />
health delivery and education in the Hunter New England local<br />
health district. ANZPATH <strong>2017</strong> Biennial Conference; Sydney,<br />
Australia<strong>2017</strong>.<br />
42. Canty J, Gray L. The last taboo? Teaching skills for<br />
clinical consultations with sex/gender diverse people in medical<br />
education. . ANZPATH <strong>2017</strong> Biennial Conference; Sydney,<br />
Australia<strong>2017</strong>.<br />
43. Grosz AM, Gutierrez D, Lui AA, Chang JJ, Cole-Kelly K,<br />
Ng H. A Student-Led Introduction to Lesbian, Gay, Bisexual, and<br />
Transgender Health for First-Year Medical Students. Family<br />
Medicine. <strong>2017</strong>;49(1):52-6.<br />
44. Safer JD, Pearce E. A simple curriculum content change<br />
increased medical student comfort with transgender medicine.<br />
Endocrine Practice. 2013;19(4):633-7.<br />
45. Sizemore LA, Rebeiro PF, Mcgoy SL. Improving HIV<br />
Surveillance Among Transgender Populations in Tennessee.<br />
LGBT Health. 2016;3(3):208-13.<br />
9
Commercial surrogacy in Australia:<br />
the benefits of harm minimization<br />
through legalisation<br />
[Feature Article]<br />
Emily Feng-Gu and Keyur Doolabh<br />
Emily is an enthusiastic fourth year medical student at Monash University. She is completing<br />
a Diploma of Liberal Arts (Philosophy), and hopes to complete a Bachelor of Medical<br />
Science next year in her area of interest: bioethics. In her spare moments, she can be found<br />
with a coffee in one hand and a book in the other.<br />
Keyur is a medical student with an interest in philosophy. He enjoys writing, and is particularly<br />
interested in poverty, climate change and animal welfare.<br />
Surrogate /sʌrəɡət/<br />
A substitute, or someone or something that<br />
represents another person or thing in their<br />
stead.[1]<br />
The status quo<br />
There is much controversy around surrogacy<br />
in Australia. We have what is known as ‘altruistic<br />
surrogacy,’ whereby a woman cannot be compensated<br />
beyond reasonable expenses for gestating a baby<br />
intended for someone else. Even the name puts our<br />
moral intuitions at ease. Altruistic. Contrast this with<br />
the term ‘commercial surrogacy’, which makes many<br />
of us instinctively recoil. So what is it about commercial<br />
surrogacy, where a woman is paid to gestate a baby, that<br />
we take issue with?<br />
The most common type of surrogacy is gestational<br />
surrogacy, wherein the commissioning parent(s)<br />
uses IVF to create an embryo from their own or donor<br />
gametes and transfer it into the uterus of the gestational<br />
surrogate. With this method, the surrogate mother does<br />
not provide any genetic material. People that seek out<br />
surrogacy commonly include infertile heterosexual<br />
couples and homosexual couples desiring children of<br />
their own. The demand for surrogacy has heightened in<br />
recent years following changes to child protection policy,<br />
which lead to drastic falls in the number of children for<br />
adoption and stricter criteria implemented by overseas<br />
countries regarding the age and family types who<br />
can adopt. For example, none of Australia’s current<br />
international adoption agreements allow same-sex<br />
couples to adopt.[2] The status quo in Australia (except<br />
the Northern Territory) only allows altruistic surrogacy,<br />
where one must not compensate the surrogate mother<br />
beyond out-of-pocket expenses like medical cost, travel,<br />
and time off work. The options are further limited by the<br />
fact that surrogacy is illegal for single people and samesex<br />
couples in certain states like Western Australia and<br />
South Australia. The increasing number of roadblocks<br />
to accessing surrogacy has left many desperate<br />
couples resorting to offshore commercial surrogacy.<br />
But even this option is becoming more restricted now<br />
that Thailand, Cambodia, India, and Nepal have banned<br />
foreigners from commercial surrogacy following the<br />
notorious “Gammy scandal” in 2014.[3]<br />
Objections to commercial surrogacy<br />
Commercial surrogacy commonly encounters several<br />
types of objections. Some think it is inescapably a form<br />
of exploitation of women, reducing the surrogate to her<br />
base reproductive capability, and effectively turning her<br />
into a walking incubator. Certainly, the idea of a class<br />
of ‘breeders’ is eerily reminiscent of Margaret Atwood’s<br />
classic novel The Handmaid’s Tale, which could be<br />
interpreted as a cautionary tale warning against the<br />
harms of surrogacy. In a similar vein, some argue that<br />
pregnancy belongs in a special moral realm, and that by<br />
bringing market forces into the arena we degrade the<br />
intrinsic value of creating life. Maybe there are some<br />
things in life which simply should not come with a price<br />
tag.<br />
Certainly, the idea of a class<br />
of ‘breeders’ is eerily reminiscent<br />
of Margaret Atwood’s classic<br />
novel The Handmaid’s Tale<br />
10
Commercial surrogacy also raises objections that<br />
intersect with other ethical and societal issues. Some<br />
assume that a child is best raised with both a father<br />
and a mother figure, and therefore believe that enabling<br />
same-sex couples to access surrogacy would be harmful<br />
for children. However, existing Australian law allows<br />
same-sex couples to adopt, and it is difficult to see why,<br />
on the grounds of concern for the child, surrogacy would<br />
be different. Furthermore, the assumption that samesex<br />
parenting is harmful to children is not borne-out in<br />
the evidence,[4] and so we do not see this as a relevant<br />
argument against commercial surrogacy.<br />
Another objection to commercial<br />
surrogacy is that it would change the<br />
nature of the family unit by involving the<br />
surrogate as a third parent figure. But<br />
these changes to the more ‘traditional’<br />
family unit are already common in<br />
society. Take for example adoption,<br />
where both biological and adoptive<br />
parents may be involved in the child’s<br />
life. It is also possible for women to<br />
become single parents through the help<br />
of donor sperm and IVF. In neither case has disruption<br />
of the ‘traditional’ family unit been viewed as reason for<br />
prohibition, and it would be inconsistent ban commercial<br />
surrogacy on these grounds.<br />
These ethical objections may be why Australia has<br />
made commercial surrogacy illegal. But given that no one<br />
has ever been prosecuted on these grounds,[5] the legal<br />
threat is a poor deterrence.[6] For people desperate to<br />
have a baby of their own, but who are otherwise unable<br />
to, the risks of commissioning illegal surrogacy can pale<br />
in comparison to the intoxicating notion of holding a fleshand-blood<br />
child.<br />
Banning commercial surrogacy<br />
domestically has created a<br />
transnational black market of<br />
commercial surrogacy that does<br />
not protect the best interests of<br />
the surrogate, the child, or the<br />
intended parents<br />
Undesirable consequences<br />
The supply of altruistic surrogates in Australia falls<br />
well short of demand, driving Australian couples to search<br />
for surrogates overseas. Most are travelling to countries<br />
like India or Thailand where the process was until recently<br />
legal, cheaper, and poorly regulated. It is this scene that<br />
has become inextricably associated with commercial<br />
surrogacy. The transnational surrogacy market operating<br />
out of developing countries has been widely criticised in<br />
popular media,[7,8] and rightly so. Women who become<br />
surrogates in these countries tend to be poorly educated,<br />
have low incomes, and may even<br />
be coerced into surrogacy by family<br />
members or intermediaries seeking to<br />
turn a profit.[9] Often, very little of the<br />
money actually reaches the surrogate<br />
herself. There are some surrogacy<br />
agencies which effectively imprison<br />
surrogates, controlling their diet, sleep,<br />
sexual activity, and contact with the<br />
outside world. All this is done under the<br />
guise of antenatal care, which is in truth<br />
scant and inadequate.[9] It is difficult to<br />
see how informed consent could truly be said to exist in<br />
this environment.[10]<br />
Even if the surrogacy results in a liveborn child, the<br />
challenges do not necessarily resolve. The lack of<br />
enforceable contracts between commissioning parents<br />
and surrogates, combined with issues of legal citizenship<br />
and parentage, can create a veritable labyrinth if<br />
conflict arises or if commissioning parents change their<br />
minds and no longer want the child. Case examples of<br />
transnational surrogacy debacles abound in the media.<br />
For example, commissioning parents have divorced<br />
before the surrogacy was complete, leaving the child<br />
<strong>11</strong>
with an uncertain future.[<strong>11</strong>] Another case saw a baby left<br />
stranded with no identity or legal papers for as long as two<br />
years.[<strong>11</strong>] Fortunately, Australian laws allow a child born<br />
from an international surrogacy arrangement to be given<br />
Australian citizenship, provided that at least one parent<br />
is an Australia citizen and a parent-child relationship is<br />
proven with DNA testing, although other measures of<br />
‘parent’ can be used. If ineligible, commissioning parents<br />
may be required to apply for a permanent visa or an<br />
adoption visa. Despite being lengthy and difficult for<br />
parents to navigate, these processes and laws minimise<br />
the risk of children born internationally via surrogacy<br />
being left stateless.[12,13]<br />
Australia’s current approach is to prohibit commercial<br />
surrogacy because it is regarded as immoral, but is this<br />
policy helping the situation or making it worse? At present,<br />
Australians for whom altruistic surrogacy is simply not<br />
feasible appear to be turning to transnational surrogacy.<br />
In 20<strong>11</strong>, only 21 births by altruistic surgery were recorded<br />
in Australia.[14] In the same year, it is estimated over 270<br />
babies were born via transnational commercial surrogacy<br />
arrangements.[6] Banning commercial surrogacy<br />
domestically has created a transnational black market<br />
of commercial surrogacy that does not protect the best<br />
interests of the surrogate, the child, or the intended<br />
parents; the process is expensive, risky, poorly regulated,<br />
and is largely a profit-making exercise for overseas<br />
surrogacy agencies. Despite being designed to prevent<br />
exploitation, our current system might in fact ironically be<br />
encouraging it.<br />
Harm minimisation<br />
Simply prohibiting a behaviour on the basis of its<br />
supposed immorality is not necessarily an effective<br />
strategy. Data shows that in Australia and overseas,<br />
drug use and morbidity increased under policies of<br />
prohibition, and decreased with decriminalization and<br />
regulation.[15] Harm minimisation is a principle we see<br />
being used more often in Australia’s approach to illicit<br />
drug use and prostitution. It recognises that prohibition<br />
can be counterproductive in achieving its overarching<br />
goal of improving the lives of Australian citizens. Instead,<br />
our laws regulate the potentially damaging behaviour or<br />
substance in a way that realistically protects the people<br />
involved. So why not apply a similar harm-minimization<br />
approach to surrogacy? Given that our prohibitive model<br />
is failing to protect Australian couples seeking surrogacy,<br />
and instead funnelling business into exploitative<br />
transnational surrogacy agencies, we should instead look<br />
to harm minimisation to guide how we approach the issue<br />
at hand. This could be best accomplished through the<br />
decriminalisation of commercial surrogacy in Australia.<br />
Decriminalisation and the establishment of a strictly<br />
regulated system would better enable us to protect the<br />
interests and rights of the intending parents, surrogates,<br />
and children. But what should these regulations actually<br />
look like?<br />
A suggested solution<br />
Ideally, a reformed system in Australia would be<br />
carried out by a centralised institution that could oversee<br />
the entire process, from psychological screening and<br />
matching, to counselling, and support services. This<br />
centralised institution could be national, state-run or notfor-profit.<br />
Strict criteria of eligibility could then more easily<br />
be applied, screening out individuals who are unsuitable<br />
for surrogacy arrangements due to medical, social, or<br />
psychological reasons. This assessment could draw on<br />
existing assessment processes for adoption.[16]<br />
The relationship between the surrogate and intending<br />
couple appears to be the most crucial factor affecting<br />
satisfaction with the experience and the likelihood of<br />
conflict regarding parentage of the baby.[17] In fact,<br />
some studies suggest the most common reason for a<br />
surrogate to want to keep the baby is being unsure of the<br />
commissioning couples ability to provide adequate care.<br />
[17] With this in mind, matching surrogates and intended<br />
parents with similar values and desired levels of contact,<br />
12
as well as facilitating educated discussion about the<br />
possibilities of chromosomal abnormalities or multifetal<br />
gestation, would also mitigate conflict. Antenatal and<br />
postnatal support, including mental health checks, could<br />
also be provided through this system.<br />
The exclusion of profiting intermediaries increases the<br />
likelihood that the interests of all parties would be equally<br />
considered, rather than sacrificing the surrogate’s health<br />
and experience in favour of maximising profits. Moreover,<br />
any surrogacy arrangements would still be constrained<br />
by Australia’s existing common law and family law. This<br />
ensures that the surrogate maintains all the decisionmaking<br />
powers throughout the pregnancy, including her<br />
rights to access termination of pregnancy and to bodily<br />
autonomy.<br />
In terms of the appropriate compensation, it seems<br />
prudent to set both a minimum and a maximum limit.<br />
Pregnancy is unavoidably risky for a woman, and gestating<br />
a growing fetus is no easy task. Why should it not, like<br />
many other jobs, receive recompense proportionate to<br />
the task? Moreover, pregnancy is intrinsically care-based<br />
‘women’s work’, which is still insidiously undervalued<br />
even in modern times. Conversely, to titrate the price of<br />
surrogacy to the intensity of a commissioning couple’s<br />
desire for a child is hardly ethical. The US can shed light<br />
on what prices may look like in an uncapped surrogacy<br />
market; the estimated reimbursement for surrogates<br />
advertised by leading US agency Circle Surrogacy, not<br />
including medical or otherwise associated expenses,<br />
is US$30,000.[18] Most couples experiencing infertility<br />
would struggle to pay this price, which does not include<br />
medical and legal costs. The aim of setting both minimum<br />
and maximum limits on a surrogate’s compensation is to<br />
strike a balance between the interests of the surrogate<br />
and the commissioning parents - or more simply put,<br />
ensuring fair pay for fair work.<br />
Furthermore, a centralised agency would also offer<br />
benefits for children born from surrogacy arrangements.<br />
There would exist a database through which children<br />
could later in life track down their surrogates should<br />
they choose to, just as adopted children can request<br />
information regarding their birth origins after turning 18.<br />
The laws regarding surrogacy should be standardised<br />
across all Australian states and territories. At present, the<br />
laws are fractured and discordant, diverging on points<br />
including whether same-sex couples should be eligible<br />
to be intended parents, the legality of advertisement for<br />
surrogacy, as well as that of seeking overseas surrogates.<br />
The murky legalities of surrogacy make it confusing for<br />
surrogates without deterring commissioning parents; if<br />
they are willing to pay tens of thousands of dollars for<br />
surrogacy, they would probably be happy to travel to<br />
states with more favourable laws.[6]<br />
Challenges of decriminalisation of commercial<br />
surrogacy<br />
One might argue that by decriminalising commercial<br />
surrogacy in Australia, we simply shift the burden of<br />
exploitation from overseas to our own shores. The<br />
concern is that commercial surrogates will be uneducated<br />
and disempowered, and have little informed choice in<br />
the matter. If we assume that the demographic of paid<br />
surrogates in Australia would resemble that of the US,<br />
then this concern does not appear to be relevant.[17, 19]<br />
Small studies of commercial surrogates in the US have<br />
suggested the while surrogates do tend to have lower<br />
incomes and less education than commissioning parents,<br />
they are generally not of a vulnerable population. In one<br />
study, most had gone to college, or at least finished high<br />
13
school, were from middle income earning families, and<br />
were in long-term relationships.[17,20] Furthermore, their<br />
primary motivation was not the money, but rather to help<br />
a couple start their families. While self-report studies<br />
do have limitations, perhaps we are too quick to assign<br />
altruistic and commercial surrogates into two camps:<br />
those who are doing it purely for selfless reasons and<br />
those who are doing it for money.<br />
The move may also be politically unpopular, with<br />
possible public resistance making the implementation<br />
slow and difficult. Moreover, creating a system which<br />
successfully protects commissioning parents, surrogates,<br />
and children born from surrogate arrangements would<br />
be a time-consuming and expensive exercise, fraught<br />
with pitfalls. Unless it is well-designed, decriminalising<br />
commercial surrogacy could perpetuate the very<br />
consequences it was designed to mitigate.<br />
Why should it not, like many<br />
other jobs, receive recompense<br />
proportionate to the task?<br />
Conclusion<br />
Our approach is not to judge the morality of<br />
surrogacy, neither promoting or undermining its value<br />
as a reproductive option relative to other methods<br />
such as adoption. The problem is a thorny and possibly<br />
intractable one, and requires careful consideration of<br />
racial politics, gender and income inequality, and human<br />
rights. Even in a moral grey zone, however, there are<br />
things which are arguably more morally reprehensible<br />
than others. Australian couples are resorting to the<br />
unregulated and deeply unethical commercial surrogacy<br />
market in developing countries, as a result of the failure<br />
of our current system. Working towards a safer, more<br />
regulated model of surrogacy should be on the Australian<br />
and international agenda.<br />
Acknowledgements<br />
The authors would like to acknowledge the contribution<br />
of ideas and research from their fellow medical students,<br />
Su Ern Poh and Eli Ivey.<br />
Photo credit<br />
http://maxpixel.freegreatpicture.com/Pregnant-<br />
Pregnancy-Pregnant-Woman-M-Mother-2640994<br />
https://www.pexels.com/photo/pregnancy-pregnantmotherboard-parenthoof-57529/<br />
http://www.publicdomainpictures.net/view-image.<br />
php?image=54223&picture=man-holding-newborn<br />
Conflicts of interest:<br />
None declared<br />
Correspondance<br />
keyurd12@gmail.com<br />
References<br />
1. Company H. The American Heritage Dictionary entry:<br />
surrogate [Internet]. Ahdictionary.com. <strong>2017</strong>. Available from:<br />
https://www.ahdictionary.com/word/search.html?q=surrogate<br />
2. Australian Institute of Health and Welfare. Adoptions<br />
Australia 20<strong>11</strong>-12. Canberra: AIHW; 2012. Contract No.: CWS<br />
42.<br />
3. Baby Gammy case reveals murky side of commercial<br />
surrogacy [Internet]. The Conversation. 2014 [cited 1<br />
October <strong>2017</strong>]. Available from: https://theconversation.com/<br />
baby-gammy-case-reveals-murky-side-of-commercialsurrogacy-30081<br />
4. Crouch S, Waters E, McNair R, Power J, Davis E. Parentreported<br />
measures of child health and wellbeing in same-sex<br />
parent families: a cross-sectional survey. BMC Public Health.<br />
2014;14(1).<br />
5. Stuhmcke A. The regulation of commercial surrogacy:<br />
The wrong answers to the wrong questions. Journal of Law and<br />
Medicine. 2015;23:333.<br />
6. Everingham SG, Stafford-Bell MA, Hammarberg K.<br />
Australians’ use of surrogacy. The Medical Journal of Australia.<br />
2014;201(5):270-3.<br />
7. Alford P. Surrogacy Scandal Widens with Southeast Asia<br />
Infant Trafficking Operation Exposed. The Australian. 2014 9<br />
August 2014.<br />
8. Murdoch L. Australian couples’ baby plans in limbo as<br />
Cambodia bans commercial surrogacy. The Sydney Morning<br />
Herald. 2016 4 November 2016.<br />
9. Saxena P, Mishra A, Malik S. Surrogacy: ethical and legal<br />
issues. Indian Journal of Community Medicine. 2012;37(4):2<strong>11</strong>.<br />
10. Deonandan R, Green S, van Beinum A. Ethical concerns<br />
for maternal surrogacy and reproductive tourism. Journal of<br />
Medical Ethics. 2012;38(12):742-5.<br />
<strong>11</strong>. Trimmings K, Beaumont P. International surrogacy<br />
arrangements: legal regulation at the international level:<br />
Bloomsbury Publishing; 2013.<br />
12. Fact sheet - International surrogacy arrangements<br />
[Internet]. Border.gov.au. [cited 1 October <strong>2017</strong>]. Available from:<br />
http://www.border.gov.au/about/corporate/information/factsheets/36a-surrogacy#offshore<br />
13. Birth, adoption and surrogacy [Internet]. Smartraveller.gov.<br />
au. [cited 1 October <strong>2017</strong>]. Available from: http://smartraveller.<br />
gov.au/guide/all-travellers/birth-death-marriage/pages/birthadoption-and-surrogacy.aspx<br />
14. Macaldowie A, Wang YA, Chambers GM, Sullivan EA.<br />
Assisted reproductive technology in Australia and New Zealand<br />
2010: AIHW; 2012.<br />
15. Wodak A. The failure of drug prohibition and the<br />
future of drug law reform in Australia. Australian Prescriber.<br />
2015;38(5):148-9.<br />
16. Review of the Adoption Act 1984. Melbourne: Victorian<br />
Law Reform Commission; 2015.<br />
17. Busby K, Vun D. Revisiting The Handmaid’s Tale: Feminist<br />
theory meets empirical research on surrogate mothers. Can J<br />
Fam L. 2010;26:13.<br />
18. Circle Surrogacy. Anticipated Costs for Gestational<br />
Surrogacy [Available from: http://www.circlesurrogacy.com/<br />
costs.<br />
19. Jadva V, Murray C, Lycett E, MacCallum F, Golombok<br />
S. Surrogacy: the experiences of surrogate mothers. Human<br />
Reproduction. 2003;18(10):2196-204.<br />
20. Ciccarelli J, Beckman L. Navigating Rough Waters:<br />
An Overview of Psychological Aspects of Surrogacy. Journal of<br />
Social <strong>Issue</strong>s. 2005;61(21):21-43.<br />
14
Polio vs Politics: The Case of Pakistan<br />
[Feature Article]<br />
Jeanine Hourani<br />
Jeanine has just completed her first year of the Master of Public Health at the University of<br />
Melbourne, having come from an Immunology & Microbiology background. She is particularly<br />
interested in refugee and migrant health as well as the effect of warfare on Public Health.<br />
Her previous work includes ‘As Syria Bleeds’ which explores the effect of the Syrian Crisis on<br />
the health system.<br />
Polio is a highly infectious disease caused by<br />
poliovirus which predominantly infects young children by<br />
invading the nervous system and can result in paralysis.<br />
[1] Polio reached epidemic proportions in the early 1900s<br />
but was brought under control after the introduction of<br />
effective vaccines in the 1950s and 1960s.[1] Despite<br />
the progress that has been made, as long as a single<br />
child remains infected with poliovirus, children in all<br />
countries are at risk of contracting the disease.[2] This<br />
is because poliovirus can easily be imported into poliofree<br />
countries and subsequently spread, potentially<br />
resulting in as many as 200,000 new cases every year.<br />
There is no cure for polio, it can only be prevented by<br />
the polio vaccine which, if administered correctly, can<br />
protect a child for life.[2] As such, vaccination programs<br />
are key to achieving global polio eradication.<br />
War and civil unrest have a destructive effect on<br />
population health. In particular, conflict increases<br />
the prevalence of vaccine preventable diseases and<br />
decreases the success of vaccination programs.[3] For<br />
instance, Pakistan is one of the few countries in the world<br />
where polio is still endemic [1, 4, 5] and this is largely<br />
due to its geopolitical and socioeconomic challenges.<br />
[6] In 2006, Taliban insurgency intensified in Pakistan<br />
and the resulting political insecurity has been directly<br />
associated with the rise in polio transmission.[7] Failure<br />
to achieve polio eradication in Pakistan demonstrates<br />
the importance of non-health sector issues, such as<br />
barriers to access in war and conflict zones [6].<br />
Conflict and insecurity in Pakistan is clustered in<br />
Khyber Pakhtunkhwa (KP) and Federally Administered<br />
Tribal Areas (FATA) which are home base to the Taliban<br />
and al-Qaeda.[5, 7, 8] The conflict and insecurity in KP<br />
and FATA has led to a dramatic rise of reported paralytic<br />
polio cases in Pakistan with more than 85% of the<br />
global polio cases coming from these regions.[7, 9] The<br />
establishment of KP and FATA as major polio reservoirs<br />
is undeniably linked to active conflict and insecurity in<br />
these regions.[7-10]<br />
It is clear that global health<br />
programs can no longer isolate<br />
themselves from economic,<br />
security, and political interests.<br />
Polio eradication in Pakistan jeopardises worldwide<br />
efforts aimed at eradicating polio.[6] In 2013, polio<br />
strains originating in Pakistan were detected in sewage<br />
samples in Egypt, Israel, the West Bank, the Gaza Strip,<br />
Syria, and Iraq.[1, 7] The first subsequent polio case<br />
occurred in Syria in October 2013, resulting in 35 children<br />
being paralysed by November.[1] The first Iraqi polio<br />
case was confirmed in March 2014.[1] Polio has spread<br />
from Pakistan in South Asia to countries in the Middle<br />
East that have been polio-free for decades, unraveling<br />
progress that has been made on a global scale [1, 7]<br />
and confirming that polio eradication is no longer solely<br />
Pakistan’s problem, but a global one.<br />
Fueling this problem is the United States’ involvement<br />
in Pakistan. In 20<strong>11</strong>, the CIA attempted to obtain DNA<br />
samples from the children in KP as part of the search for<br />
Osama bin Laden. In order to do this, the CIA conducted<br />
a fake vaccination program against hepatitis B, leading<br />
to an erosion of public trust in immunisation.[1, 7-9]<br />
The use of aid workers for intelligence purposes and<br />
the use of health initiatives to advance security and<br />
15
foreign policy motives has undermined global healthcare<br />
initiatives aimed at polio eradication, jeopardising longterm<br />
global health goals.[7]<br />
Recent fatal attacks on polio vaccination workers in<br />
politically fragile parts of Pakistan pose a further threat<br />
to the global eradication of polio.[<strong>11</strong>] It is believed that<br />
the international attention paid to polio eradication may<br />
have led terrorist groups to believe that they can achieve<br />
some of their aims by interfering with its eradication.<br />
[<strong>11</strong>] As such, the Pakistani Taliban announced in June<br />
2012 that it would place a ban on all vaccinations until<br />
the United States ended drone strikes.[9] Since then,<br />
the Taliban have orchestrated targeted attacks on<br />
immunisation teams that have tragically killed over 40<br />
vaccinators.[1, 7] This includes the killing of Abdul Ghani<br />
(who was the head of the government’s vaccination<br />
campaign) by a road-side bomb after upon his return<br />
from a meeting with tribal elders to dispel rumours that<br />
vaccination is a U.S. conspiracy to sterilize their children.<br />
[5] To this day, vaccination program staff remain under<br />
threat of kidnappings, beatings, harassment, and even<br />
assassinations in conflict zones.[9]<br />
It is believed that the actions against polio workers may<br />
be driven by two objectives; to terrorise local populations<br />
and government workers, or to stop the house-to-house<br />
movement of polio workers who some terrorist groups<br />
suspect of carrying out US surveillance activity (brought<br />
about by the fake hepatitis B campaign).[<strong>11</strong>] Regardless<br />
of the reason, it is clear that polio eradication has evolved<br />
into a war tactic resulting in an environment of fear and<br />
anarchy.<br />
Global health initiatives are becoming increasingly<br />
intertwined with diplomatic, foreign policy, and security<br />
interests.[7] This is not limited to Pakistan: earlier this<br />
year, six Red Cross Aid workers were killed in Afghanistan<br />
[12], and healthcare in Syria has been transformed into a<br />
target of war.[13] It is clear that global health programs<br />
can no longer isolate themselves from economic,<br />
security, and political interests.[7] The recent portrayal of<br />
polio as the new battleground between Western forces<br />
and terrorist groups illustrates the importance of efforts<br />
to depoliticise polio activities.[<strong>11</strong>] We can no longer allow<br />
security or foreign policy motives to undermine polio<br />
eradication and thus compromise the wellbeing of the 7.5<br />
billion people living on earth.<br />
Photo credit<br />
Sanofi Pasteur / Almeena Ahmed / Sanaullah Afridi,<br />
accessed from https://www.flickr.com/photos/sanofipasteur/29837040256/in/album-72157673062558422/<br />
Conflicts of interest<br />
None declared<br />
Correspondance<br />
jeaninehourania@live.com.au<br />
References<br />
1. Akil L, Ahmad HA. The recent outbreaks and reemergence<br />
of poliovirus in war and conflict-affected areas. Int J Infect Dis.<br />
2016;49:40-6.<br />
2. WHO. Does polio still exist? Is it curable? <strong>2017</strong> [Available<br />
from: http://www.who.int/features/qa/07/en/.<br />
3. Glatman-Freedman A, Nichols K. The effect of<br />
social determinants on immunization programs. Hum Vaccin<br />
Immunother. 2012;8(3):293-301.<br />
4. Afzal O, Rai MA. Battling polio in Pakistan: breaking new<br />
ground. Vaccine. 2009;27(40):5431.<br />
5. Ahmad K. Pakistan struggles to eradicate polio. The<br />
Lancet Infectious Diseases. 2007;7(4):247.<br />
6. Nishtar S. Pakistan, politics and polio. Bull World Health<br />
Organ. 2010;88(2):159-60.<br />
7. Hussain SF, Boyle P, Patel P, Sullivan R. Eradicating polio<br />
in Pakistan: an analysis of the challenges and solutions to this<br />
security and health issue. Global Health. 2016;12(1):63.<br />
8. Roberts L. Fighting Polio in Pakistan. Science. 2012;337.<br />
9. Chang A, Chavez E, Hameed S, Lamb RD, Mixon K.<br />
Eradicating Polio in Afghanistan and Pakistan. A Report of the<br />
CSIS Global Health Policy Center. 2012.<br />
10. Shah M, Khan MK, Shakeel S, Mahmood F, Sher Z, Sarwar<br />
MB, et al. Resistance of polio to its eradication in Pakistan. Virol<br />
J. 20<strong>11</strong>;8:457.<br />
<strong>11</strong>. Abimbola S, Malik AU, Mansoor GF. The Final Push for<br />
Polio Eradication: Addressing the Challenge of Violence in<br />
Afghanistan, Pakistan, and Nigeria. PloS Med. 2013;10(10):1-4.<br />
12. SBS. Opinion: Aid workers are not a target, and never<br />
should be <strong>2017</strong> [Available from: http://www.sbs.com.au/news/<br />
article/<strong>2017</strong>/02/17/opinion-aid-workers-are-not-target-andnever-should-be.<br />
13. The Guardian. Syria ‘the most dangerous place on<br />
earth for healthcare providers’ <strong>2017</strong> [Available from: https://<br />
www.theguardian.com/world/<strong>2017</strong>/mar/15/syria-conflict-studycondemns-weaponisation-of-healthcare.<br />
Key Messages<br />
• The persistence of polio in Pakistan jeopardises worldwide<br />
efforts aimed at eradicating the disease.<br />
• Global health initiatives are becoming increasingly<br />
intertwined with the diplomatic, foreign policy, and security interests<br />
• With the portrayal of polio as a battleground between<br />
Western forces and terrorist groups, greater effort should be made<br />
to depoliticise polio activities<br />
16
turning up the heat<br />
[Feature Article]<br />
Tara Kannan<br />
Tara Kannan is a first-year MD student at the University of Newcastle. Passionate about<br />
global health, she represents AMSA’s <strong>2017</strong> Code Green portfolio within her university’s<br />
global heath group. She believes that a major way forward in advancing medicine on the<br />
world stage is through nursing our environment back to good health. Aside from that, when<br />
she’s not busy dissecting Guyton’s diagrams, she enjoys perusing news articles online and<br />
loves her Cadbury.<br />
American environmentalist and journalist, Bill<br />
McKibben, offers a simple yet revolutionary proposition<br />
in the climate debate: “Leave oil in the soil, coal in the<br />
hole and gas under the grass”.<br />
The birth of an idea<br />
Divestment is a very simple idea. You just remove your<br />
money from companies that are involved in extracting<br />
fossil fuels. It’s a novel movement in the climate debate<br />
that is different from your traditional change-yourlightbulb<br />
kind of ideas.<br />
Its underlying basis is that to avoid catastrophic<br />
global warming, we will need to reduce our carbon dioxide<br />
emissions. There are three key numbers that explain<br />
this. First, 2˚C is the maximum global temperature rise<br />
this century that is aspired to in the Paris Agreement.[1]<br />
Secondly, we have a ‘carbon budget’ of 565 gigatons<br />
which is essentially the amount of carbon dioxide that<br />
can safely be released into the atmosphere while still<br />
complying to our 2˚C rule.[2] Most importantly, the third<br />
number to know is 2795 gigatons. This is the amount<br />
of carbon dioxide that will be released if all of the<br />
documented fossil fuel reserves<br />
were burned.[2]<br />
Addressing a sixfold rise<br />
in energy demand in the last<br />
50 years, fossil fuels provide<br />
roughly 80% of the energy we<br />
need through coal, gas and oil.[3]<br />
Yet, the money-making industry<br />
releases greenhouse gases into<br />
the atmosphere and thickens Earth’s blanket of air<br />
pollution which led to 3.7 million deaths in 2012 due to<br />
pneumonia, asthma, heart disease, stroke and cancer.<br />
[3] Needless to say, carbon dioxide is a tiny molecule with<br />
a big bite.<br />
So, while as individuals we could make some<br />
adjustments such as changing our lightbulbs and<br />
switching from car use to public transport, if companies<br />
continue to dig up and burn their reserves, these<br />
measures will prove rather insignificant. This is where<br />
divestment comes in - a movement about shifting your<br />
money away from the problem and towards the solution.<br />
Turning back time<br />
So, while as individuals we could make<br />
some adjustments such as changing our<br />
lightbulbs and switching from car use to<br />
public transport, if companies continue<br />
to dig up and burn their reserves, these<br />
measures will prove rather insignificant.<br />
In history, divestment has been shown to be a powerful<br />
political tool in several major movements.<br />
In the latter half of the 20th century, a time when South<br />
Africa’s Apartheid was our world’s largest moral issue,<br />
two prominent figures created massive change. Nelson<br />
Mandela and Desmond Tutu suggested a revolutionary<br />
tactic to help counter institutionalised racial segregation<br />
and white supremacy, imploring Western institutions<br />
to cut their economic ties with companies backing<br />
the Apartheid regime. Experts often deem this as the<br />
model of symbolic pressure as it raised awareness and<br />
embarrassed many American businesses.[4]<br />
Then, through the 1990s, a<br />
movement against the tobacco<br />
industry took place to shun the<br />
industry’s negative impacts on<br />
health. Along with regulation and<br />
taxation, tobacco divestment had<br />
a sizeable impact on society,<br />
shrinking the industry and<br />
smoking rates.[4]<br />
Most recently, divestment has had a role in the<br />
Darfur genocide - the first genocide of the 21st century.<br />
Darfur divestment involves removing money away from<br />
companies with ties to the Sudanese government. Some<br />
17
Western institutions including Brown University divested;<br />
however, other investors interested in the nation’s<br />
valuable resources simply filled their place. Drawing from<br />
this rather unsuccessful campaign, fossil free activists<br />
are encouraged to consider how their actions could lead<br />
to the success or failure of the divestment movement.<br />
More specifically, it is important to weigh the impact of<br />
divesting from a company relative to giving up your voice<br />
as a shareholder.<br />
Fuelling a movement<br />
Nevertheless, the balance scales show that<br />
divestment is well worth the bet. Major goals of the<br />
fossil fuel divestment campaign can be captured in the<br />
following:[4]<br />
a) leverage the power of investors and institutions to<br />
make strong political statements and influence policy<br />
change<br />
b) raise awareness of the impact of the fossil fuel<br />
industry in our society<br />
c) lead the market to consider the effects of climate<br />
change when evaluating any investments<br />
d) drive capital investment into clean energy and<br />
other climate mitigation strategies<br />
Above all else, divestment stigmatises the fossil fuel<br />
industry, eroding its social license to operate and posing<br />
the largest threat to these companies.<br />
Back home, Australian universities are making<br />
bold statements with the help of several fossil free<br />
organisations on campus. La Trobe University, Swinburne<br />
University and the Queensland University of Technology<br />
pledged to divest their A$40 million, A$150 million and<br />
A$300 million portfolios from fossil fuels respectively.<br />
[7] Recently, both Monash University and the Australian<br />
National University have partially divested.[8] But sadly,<br />
Westpac, ANZ, NAB and the Commonwealth Bank –<br />
which make up the ‘big four’ banks of Australia — have<br />
failed to divest, instead funding the industry to the tune of<br />
A$5.5 billion in 2015.[7]<br />
the ‘carbon bubble’ has its<br />
underlying roots in the fact that<br />
our financial markets maintain<br />
an extraordinary overvaluation<br />
of fossil fuel reserves that has<br />
the potential to burst.<br />
Pop goes the bubble<br />
From an economic point of view, fossil fuel divestment<br />
is falsely thought to come with financial uncertainty and<br />
major repercussions. Addressing this, a key argument<br />
in the fossil fuel divestment campaign is that returns<br />
will, in fact, improve once investors have divested – an<br />
And, if you have not figured it out yet, the fossil fuel<br />
divestment campaign is not a normal movement. There<br />
are no great leaders. There is no Gandhi or Martin Luther<br />
King Jr. of the climate movement. But, establishing firm<br />
roots in society, the fossil fuel movement is set to be<br />
colossal with or without a figurehead.<br />
...divestment stigmatises the<br />
fossil fuel industry, eroding its<br />
social license to operate and<br />
posing the largest threat to<br />
these companies.<br />
Blossoming ideas<br />
Since its initial conception in 2010, the idea of fossil<br />
fuel divestment has been spreading like wildfire. The<br />
campaign celebrated its first major victory in mid-2014<br />
when Stanford University committed to divesting its<br />
US$18.7 billion endowment from the industry.[5] Later that<br />
year, the campaign inspired the People’s Climate March<br />
where a 400,000-strong crowd flooded Manhattan’s<br />
streets, demanding U.N. action on global warming.[4] By<br />
2015, around 2500 investors representing US$2.6 trillion<br />
in assets had divested, including major organisations<br />
such as the Rockefeller Brothers Fund and the Canadian<br />
Medical Association.[6]<br />
Figure 1: Global health groups are leading the fossil fuel divestment game<br />
with eight societies having divested; while, only three medical societies have<br />
divested so far.<br />
18
argument based on a concept called the ‘carbon bubble’<br />
– named by the Carbon Tracker Initiative. Much like the<br />
US housing bubble of 2009, the ‘carbon bubble’ has its<br />
underlying roots in the fact that our financial markets<br />
maintain an extraordinary overvaluation of fossil fuel<br />
reserves that has the potential to burst.[4, 8] The problem<br />
here is that all reserves simply cannot be burned if we<br />
intend to comply with the ‘carbon budget’, or else, there’s<br />
no doubt that we will find ourselves amidst catastrophic<br />
climate change.<br />
More importantly, with increasing pressure from<br />
pollution regulations, competition from renewables<br />
and one of history’s fastest growing stigmatisation<br />
...the fossil fuel divestment<br />
campaign is not a normal<br />
movement. There are no great<br />
leaders. There is no Gandhi<br />
or Martin Luther King Jr. of the<br />
climate movement.<br />
campaigns, the value of fossil fuels is already diminishing.<br />
[4,8] Last year, energy use emissions grew less than<br />
1% for the third consecutive year.[9] Oxford University<br />
researchers and commercial analysts are predicting that<br />
fossil fuels are likely to become ‘stranded assets’ which<br />
cannot be used, rendering them worthless to investors.<br />
[8, 9] It follows that investors should prepare for such a<br />
scenario by selling their assets now rather than after the<br />
‘carbon bubble’ bursts when investors are likely to lose<br />
money.<br />
Preparing accordingly, investors in Wall Street banks,<br />
such as HSBC and Chase, have demanded that fossil<br />
fuel companies discuss the risks of the bubble; while,<br />
oil companies, including Shell, are now committed to<br />
disclosing their asset portfolios and discussing the<br />
bubble.[4] Similarly, with major financial news venues such<br />
as Bloomberg and the Financial Times now backing the<br />
movement, we are beginning to achieve one of our primary<br />
aims: influencing the economy’s thinking on climate<br />
change.[4] In fact, as of September <strong>2017</strong>, US$5.53 trillion<br />
has been divested by almost 800 institutions.[7]<br />
Renewable energy: a brave new world of investment<br />
So, you move your money away from the fossil fuel<br />
industry and then what? Many experts have shown that<br />
investing in ethical funds such as the renewable energy<br />
industry will have financial returns similar to, if not better<br />
than, the fossil fuel industry.[10]<br />
Renewable energy has made ambitious headlines<br />
around the world. For instance, China recently became<br />
home to the world’s largest solar farm at 27-squarekilometres<br />
which can produce 850 mega-watts of power<br />
- enough to supply around 200,000 households.[<strong>11</strong>]<br />
However, even though renewable technology needs to be<br />
used by all, it’s only accessible to those who can afford<br />
it. Addressing this gap, many grassroots movements are<br />
committed to providing renewable energy to developing<br />
nations. For instance, one such foundation, Liter of Light,<br />
teaches communities to recycle plastic bottles and use<br />
locally sourced materials with the aim of illuminating their<br />
homes – a strategy which has received much recognition<br />
and is often adopted for use in UNHCR camps.[12]<br />
Figure 2: the committee of the University of Newcastle’s global health group, Wake Up!, proudly put their W’s up to<br />
celebrate their divestment win. Congrats Wake Up!<br />
19
Key messages<br />
• Fossil fuel divestment is a very simple idea: a global movement<br />
focussed on shifting money away from a problem and towards a solution.<br />
• Divestment has been shown to be historically successful<br />
• Establishing firm and expansive roots in our society, divestment now<br />
sets out to radically influence the world’s thinking on climate change<br />
The power of smaller players<br />
Speaking of smaller players making big waves,<br />
medical societies and faculties, are major targets of<br />
the fossil fuel divestment campaign. As highly regarded<br />
entities within universities, they are large enough to<br />
matter but small enough to have an influence on. Now,<br />
more than ever, we are seeing Australian medical<br />
university groups divesting (Figure 1). Most recently, the<br />
University of Newcastle’s global health group, Wake Up!,<br />
switched from the Commonwealth Bank to Newcastle<br />
Permanent – a major win in our medical scene (Figure 2).<br />
Although divestment will not cripple the fossil fuel industry<br />
overnight, this strategy can still operate effectively,<br />
conveying a loud and clear message of disapproval – an<br />
objective we are closer to achieving thanks to societies<br />
like Wake Up!<br />
One of divestment’s main jobs is to draw attention<br />
and challenge the status quo – a powerful opportunity to<br />
be noticed, and be remembered, in times of tragedy and<br />
turbulence. It’s a movement that inspires students, banks<br />
and universities alike to make ethical commitments<br />
and invest in a sustainable future. With global warming<br />
looming large, now is the time to blaze trails and boldly<br />
transform the climate debate.<br />
2015; 82:913-37.<br />
5. Carroll R. Major University Divests $18 Billion Endowment<br />
From Coal Companies [Internet]. HuffPost. <strong>2017</strong> [cited 15<br />
September <strong>2017</strong>]. Available from: http://www.huffingtonpost.<br />
com/2014/05/07/stanford-university-divesting_n_5276899.<br />
html<br />
6. Rowe JK, Dempsey J, Gibbs P. The Power of Fossil<br />
Fuel Divestment (And its Secret). The University of California<br />
eScholarship. 2016.<br />
7. Go Fossil Free. Divestment Commitment [Internet]. Go<br />
Fossil Free. <strong>2017</strong> [cited 15 September <strong>2017</strong>]. Available from:<br />
http://gofossilfree.org/commitments<br />
8. Ansar A, Caldecott B, Tilbury J. Stranded assets and<br />
the fossil fuel divestment campaign: what does divestment<br />
mean for the valuation of fossil fuel assets?. Smith School of<br />
Enterprise and the Environment. 2013.<br />
9. Brahic C. Living with climate change: Have we reached<br />
peak emissions? New Scientist. <strong>2017</strong>; 234: 32-4.<br />
10. De George R. Ethics, corruption, and doing business in<br />
Asia. Asia Pacific Journal of Economics and Business. 1997; 1:<br />
39–52.<br />
<strong>11</strong>. Phillips T. China builds world’s biggest solar farm in<br />
journey to become green superpower #GlobalWarning [Internet].<br />
The Guardian. <strong>2017</strong> [cited 15 September <strong>2017</strong>]. Available from:<br />
https://www.theguardian.com/environment/<strong>2017</strong>/jan/19/chinabuilds-worlds-biggest-solar-farm-in-journey-to-become-greensuperpower<br />
12. Liter of Light. Liter of Light - About Us [Internet]. Liter of<br />
Light. <strong>2017</strong> [cited 15 September <strong>2017</strong>]. Available from: http://<br />
literoflight.org/about-us/<br />
Conflicts of interest<br />
None declared<br />
Correspondance<br />
taranikita@hotmail.com<br />
References<br />
1. United Nations Framework Convention on Climate<br />
Change: Adoption of the Paris Agreement. 21st Conference of<br />
the Parties, 2015: Paris, France: United Nations.<br />
2. 350.org. Do the Math [Internet]. Math.350.org. <strong>2017</strong> [cited<br />
15 September <strong>2017</strong>]. Available from: http://math.350.org/<br />
3. Perera F. Multiple Threats to Child Health from Fossil<br />
Fuel Combustion: Impacts of Air Pollution and Climate<br />
Change. Environmental Health Perspectives. <strong>2017</strong>; 125: 141-8.<br />
Doi:10.1289/EHP299<br />
4. Apfel DC. Exploring Divestment as a Strategy for<br />
Change: An Evaluation of the History, Success, and Challenges<br />
of Fossil Fuel Divestment. New School for Social Research.<br />
20
Coal mining, climate change and the<br />
global impacts on health: examining<br />
Adani’s proposed Carmichael coal mine<br />
Introduction<br />
The proposed Adani-owned Carmichael coal mine<br />
in central Queensland is currently in the final stages of<br />
planning with the support of both the Queensland and<br />
Australian governments. It is in the interest of human<br />
health, locally and abroad, for the medical profession<br />
to advocate on behalf of the community and lobby our<br />
legislators to reject this project.<br />
The Carmichael site will be the world’s largest export<br />
coal venture and the biggest mining site in Australia,<br />
consisting of six open cut pits and five underground<br />
mines. Mined in the Galilee Basin, 160km north-west<br />
of Clermont, coal will then be transported on a new<br />
railway network before connecting to shipping terminals<br />
bound for India via the Great Barrier Reef Marine Park.[1]<br />
Adani has stated that it plans to mine 60 million tonnes<br />
of coal every year over the expected 60 year lifespan<br />
of the Carmichael mine site.[2] The estimated annual<br />
average emissions of the proposed Adani coal mine are<br />
equivalent to the annual emissions of Malaysia, Vietnam<br />
or Sri Lanka.[3]<br />
The Carmichael mine is<br />
a highly politicised topic with<br />
widespread implications. This<br />
article considers some of the<br />
impacts on Australia’s economy,<br />
our natural environment (and that<br />
of our regional neighbours), and<br />
crucially; the seriousness of the<br />
Carmichael mine’s contribution to climate change and<br />
its effect on human health.<br />
Health Implications on a Global Scale<br />
The World Health Organization (WHO) has said that<br />
climate change is the greatest threat to human health<br />
this century.[4] This gigantic coal mine is set to contribute<br />
significantly to climate change. It will adversely affect<br />
[Feature Article]<br />
John E Morgan<br />
John Morgan is a fourth year medical student at James Cook University. He is<br />
passionate about advocacy, climate change and issues facing the developing<br />
countries within our region. He is a member of Doctors for the Environment and<br />
AMSA’s Mental Health Campaign. Based in Cairns, he loves bushwalking and<br />
camping (and so far hasn’t had any crocodiles up close).<br />
A report recently published in The<br />
Lancet has condemned the planned<br />
Adani Carmichael project as a “public<br />
health disaster”<br />
population health through greenhouse gas emissions,<br />
waterway damage and land clearing. A report recently<br />
published in The Lancet has condemned the planned<br />
Adani Carmichael project as a “public health disaster”,<br />
arguing that the health impacts and environmental<br />
damage will be significant for Australia and its regional<br />
neighbours.[5]<br />
The net effect of obtaining and using coal from the<br />
Carmichael site is estimated to release 4.7 billion tonnes<br />
of greenhouse gas emissions,[6] which will contribute<br />
to climate change. This will result in increased human<br />
exposure to pollen, moulds and air pollution, reducing<br />
air quality and increase the incidence of respiratory<br />
diseases.[7] Ambient pollution in Australia is primarily<br />
derived from fossil fuel powered electricity generation,<br />
heavy industry and wood or coal based home heating.[8]<br />
Annually, 3000 Australians die due to urban air pollution,<br />
more than the national road toll.[9] In its current state,<br />
the air pollution problem is already being insufficiently<br />
addressed. Additionally, exposure to ozone is linked with<br />
increased hospital admissions for respiratory diseases<br />
amongst both children and the elderly.[10] Our legislators<br />
must act decisively and commit meaningful action to<br />
reduce the impact of climate change as it will affect the<br />
health of future generations and<br />
our present vulnerable elderly<br />
population.<br />
Currently, 5% of the<br />
population will experience an<br />
allergic respiratory response to<br />
airborne moulds during their lifetime.[<strong>11</strong>] Changes in<br />
global precipitation are likely to increase the prevalence<br />
of airborne moulds.[7] Additionally, ambient air pollutants<br />
and allergens are most likely to exacerbate respiratory<br />
disease in individuals with pre-existing respiratory<br />
conditions.[12] Climate change associated air pollution<br />
will undoubtedly worsen the quality of life of patients<br />
living with chronic airway diseases.<br />
21
Coal combustion affects the water as well as the air.<br />
Rising water temperatures linked to climate change will<br />
cause further aerosolisation of marine toxins, thereby<br />
increasing respiratory disease prevalence globally.[7]<br />
Asthmatics exposed to the harmful algal bloom Karenia<br />
brevis’ marine aerosols on the south east coast of the<br />
United States of America (USA) experienced respiratory<br />
symptoms after just one hour of exposure. Inland<br />
residents experienced an average of 3.49 symptoms,<br />
more than coastal residents, who experienced an<br />
average of 2.24 symptoms.[13] This suggests that<br />
aerosolisation of marine toxins will increase respiratory<br />
morbidity as climate change related aerosols proliferate<br />
and distribute further afield.<br />
The cardiovascular burden of disease will worsen<br />
in the future if action is not taken now to reduce the<br />
impacts of climate change.[7] Airborne particulate<br />
matter is associated with compromised heart function,<br />
atherosclerotic disease, deep vein thrombosis,[14] and<br />
pulmonary embolism.[15] The particulates contributing<br />
to air pollution include black carbon, sulphates, nitrates,<br />
a complex mixture of metals and other byproducts<br />
from the incomplete combustion<br />
of fossil fuels.[16] In areas with long term<br />
exposure to high levels of particulate matter<br />
air pollution, it was found that an increase<br />
of just 10 ug/m3 is associated with a 70%<br />
increase in DVT risk.[15] Ozone is another<br />
key pollutant - exposure to a 10g/m3<br />
increment has demonstrated an increase<br />
in the risk of cardiopulmonary mortality by 1.014 times.<br />
[14] Both particulate matter and ozone type air pollution<br />
cause adverse cardiovascular outcomes.<br />
Increased global temperatures will exacerbate heat<br />
related deaths due to an increased frequency of heat<br />
stress events.[7] Untreated heat exhaustion can progress<br />
to heat stroke,[17] of which 15% of cases are fatal.[18]<br />
Heat related health events typically occur on the same<br />
day as initial exposure.[19] Emergency departments (ED)<br />
in Brisbane have demonstrated that during days ≥35°C,<br />
elderly patients were 1.9 times as likely to present<br />
to the ED and 3.75 times as likely to present due to<br />
heat-related complications specifically.[20] Based on<br />
current modelling of Brisbane’s population growth, ED<br />
presentations on days ≥35°C and the projected climate<br />
change related temperature increases, it is predicted to<br />
cause a 125-2065% increase in excess visits by 2060.<br />
[20] Consequently, political inaction now will continue to<br />
worsen the burden on public ED services.<br />
In areas with long term<br />
exposure to high levels of<br />
particulate matter air pollution,<br />
it was found that an increase of<br />
just 10 ug/m3 is associated with<br />
a 70% increase in DVT risk.<br />
[22] This emerging group of environmentally displaced<br />
people will need support to cope.[23] Climate change<br />
has the potential to create disasters beyond the capacity<br />
of developing nations’ public health systems.[24] Action<br />
must be taken to reduce the impact of climate change<br />
for the sake of public health. The global community is<br />
interconnected and each nation has the responsibility to<br />
reduce its contributions to climate change. Consequently,<br />
the impact of the planned Carmichael mine site and its<br />
extensive environmental damage will have substantial<br />
impact on human health into the future.<br />
Locally, coal worker’s pneumoconiosis has reemerged<br />
in Queensland with at least 20 cases recently<br />
diagnosed, highlighting the lack of appropriate health<br />
protection within the Queensland coal industry.[25] If the<br />
Queensland and Australian governments can’t manage<br />
these Occupational Health and Safety issues at home,<br />
how can they contribute to the ‘safe’ delivery and burning<br />
of this coal in Adani’s power stations in India – a country<br />
where air pollution already kills an estimated 1.1 million<br />
people annually.[26] If the mine proceeds, the flow on<br />
effects of poor governing locally will<br />
have detrimental health impacts on a<br />
global scale.<br />
Environmental Implications<br />
The establishment of the<br />
proposed Carmichael coal mine<br />
and its shipping impact will damage<br />
vital ecosystems and reshape the lives and health of the<br />
people reliant on waterways and reefs. More than 500<br />
million people around the planet rely on coral reefs for<br />
food, income and storm protection.[29] Climate related<br />
changes in waves, ocean circulation, cyclone frequency,<br />
temperature and precipitation will impact fisheries in<br />
tropical Queensland and further north.[30] Additionally,<br />
fisheries in our region may be contaminated by chemicals<br />
released into seawater by the mine and from increased<br />
shipping traffic. This will have economic, social and<br />
health implications and affect the productivity of the<br />
seafood industry in Australia and surrounding nations,<br />
especially those that rely on it as a major industry and<br />
cultural cornerstone.[30] Climate change associated<br />
contamination of food staples is also likely to impact on<br />
nutrition and human development.[7] In parallel, the social<br />
aspects of recreational fishing are also highly sensitive<br />
to climate change.[30] Thus, along with the state of the<br />
environment, multiple social determinants of health are<br />
at risk of declining for our coastal communities.<br />
The psychological impacts of climate change are<br />
generally indirect and have only recently been considered<br />
as part of the widespread impacts of climate change on<br />
health. Extreme weather events can lead to mental health<br />
disorders associated with loss, displacement and social<br />
disruption. This can increase anxiety about the future, with<br />
already-disadvantaged communities most likely to suffer<br />
the most severe consequences.[21] Two hundred million<br />
people will be displaced by climate change by 2050.<br />
Implications for Australia<br />
In Central Queensland, the proposed Adani mine<br />
will see more than 10,000 hectares of native bushland<br />
cleared from around the Galilee Basin. Combined<br />
with the Carmichael mine’s generous water licence<br />
enabling unlimited groundwater use from the Great<br />
Artesian Basin,[31] this has huge potential for irreversible<br />
environmental damage.<br />
22
The Great Artesian Basin is a drought-prone area that<br />
is critically responsible for supplying an estimated 200<br />
towns and settlements with irrigation and drinking water.<br />
[31] The construction of the world’s largest coal mine at<br />
this site could risk the livelihoods and lives of Australian<br />
primary producers in this region. The importance of<br />
water security in drought-prone areas is tantamount and<br />
supporting this mine renders these remote Australians<br />
even more vulnerable. Australians living in rural and<br />
remote settings already have a lower standard of health<br />
service provision and are more likely to suffer worse<br />
health outcomes as a consequence of their social<br />
determinants.[32] The health impacts from the proposed<br />
mine are likely to impact rural Australians to an even<br />
greater magnitude.<br />
Massive quantities of coal will be shipped overseas<br />
through the Great Barrier Reef.[3] It is feared that this will<br />
exacerbate the already extensive coral bleaching. This<br />
will impact Australian coastal communities as the Great<br />
Barrier Reef and other coral reefs provide protection<br />
from wave and storm damage.[33]<br />
Implications for Australia’s regional neighbours<br />
Climate change is projected to slow economic growth,<br />
erode food security and hinder poverty reduction. The<br />
negative effects will be most felt by those who are already<br />
disadvantaged.[34] This is especially pertinent for our<br />
regional neighbours, predominately developing countries.<br />
prevent the temperature associated rises in sea levels<br />
in order to prevent their nations going underwater. A 2°C<br />
goal requires a 40-70% reduction in greenhouse gas<br />
emissions compared with 2010 levels, whereas a 1.5°C<br />
increase will require a 70-95% reduction.[28] As one of<br />
the most influential developed countries in our region,<br />
Australia has a responsibility to support the continuing<br />
development of our regional peers. This begins with<br />
supporting their call for action to reduce the global<br />
temperature rise to 1.5°C. There is simply no room for<br />
the proposed Carmichael coal mine and its extensive<br />
pollution in a sustainable future – a future that needs<br />
action now.<br />
Economic and Political implications<br />
The proposed Carmichael mine project has struggled<br />
to achieve financing. Nineteen banks (including<br />
Australia’s ‘Big Four’) have refused to fund the venture<br />
due to ethical concerns, environmental policies, or the<br />
likelihood that renewable energy will outprice fossil fuels<br />
over the proposed life of the mine. The use of Australian<br />
mined coal in Indian power plants will also inevitably<br />
become economically foolhardy.[37] Both the Australian<br />
and Queensland governments should not continue to<br />
support this proposal as it will create few lasting jobs and<br />
crucially it will increase the loss of human life and burden<br />
of disease locally and abroad.<br />
Many of our regional neighbours are already suffering<br />
from the effects of climate change. Bangladesh has<br />
experienced increased temperatures, swollen rivers and<br />
sea level rises; all which threaten infrastructure, livelihoods<br />
and homes and undermining the region’s development.<br />
[35] Climate change is now making cyclones on many<br />
of our neighbouring Pacific Islands even more powerful<br />
and destructive. In 2016, Tropical Cyclone Winston hit Fiji,<br />
affecting more than half a million people and decreasing<br />
its national GDP by one-fifth.[36] As a developed nation,<br />
our government has a responsibility to contribute to the<br />
prosperity, safety and health of our region by supporting<br />
these developing nations. This begins with reducing our<br />
carbon footprint by stopping the expansion of our fossil<br />
fuel industry, including the proposed Carmichael coal<br />
mine.<br />
The climate impacts of the proposed Carmichael coal<br />
mine go against Australia’s international commitment<br />
to promote a sustainable future by limiting increases in<br />
global temperatures. The United Nations Framework<br />
Convention on Climate Change (UNFCCC) promotes the<br />
work of the Paris Agreement to limit a global temperature<br />
rise this century to below 2°C above pre-industrial levels.<br />
[27] Many of our regional neighbours do not believe this<br />
goes far enough. The “1point5toStayAlive” movement<br />
by the Caribbean and their partner states is fighting to<br />
The continued approval of Adani’s Carmichael<br />
mine by the Australian and Queensland governments is<br />
unwise as the economic return on taxpayer investment<br />
23
is questionable. The Northern Australia Infrastructure<br />
Facility (NAIF) has proposed a $1 billion AUD loan to<br />
Adani for the North Galilee Basin Rail Project – a 310km<br />
rail link from the mine site to the Abbot Point export<br />
terminal. Despite widespread coverage, little information<br />
was publicly available at the time of writing; only four<br />
documents were published on NAIF’s website, with none<br />
focussing explicitly on coal mining in the Galilee Basin.<br />
[38-41] Both Adani and the former Minister for Resources<br />
and Northern Development have suggested that the<br />
loan is “not critical” and consequently the mine should<br />
be ineligible for NAIF funding.[42] Other requirements<br />
for NAIF funding include public benefit and commercial<br />
viability, both of which are questionable.[42]<br />
Adani continues to claim that the Carmichael mine<br />
will create 10,000 direct and indirect jobs. However, reef<br />
industries threatened by the mine provide approximately<br />
69,000 jobs.[43] The proposed “10,000 jobs” is even more<br />
questionable because Adani has, under oath, stated only<br />
1,464 jobs will be created.[42] A loan of this magnitude<br />
seems wasteful for taxpayers. In September 2016, the<br />
Minister for Resources and Northern Australia Matthew<br />
Canavan stated that opening the Galilee Basin for coal<br />
mining would “not damage the environment”.[38] The<br />
political mismanagement and fabrications surrounding<br />
the Carmichael mine site are a disservice to Australian<br />
taxpayers.<br />
The lifespan of the proposed Carmichael coal mine<br />
is 60 years.[2] Australian coal is expected to be burnt in<br />
India, a country where the Power Minister plans to ban<br />
coal imports. India’s draft National Electricity plan states<br />
that until 2022, India will not require an increase of coal<br />
from its current rate of supply.[44] India is also a signatory<br />
to the Paris Agreement and has declared commitment<br />
to utilising emerging “cleaner sources of energy” as<br />
they become feasible.[45] The long term profitability of<br />
Adani’s Carmichael coal mine is even more questionable<br />
as there is growing public discontent in India with coalbased<br />
power sources and its resulting air pollution. Whilst<br />
there was an absolute increase in the use of coal in India,<br />
renewable generation grew at over six times the rate<br />
of conventional sources. Between April-October 2016,<br />
28% of Indian energy production came from renewable<br />
resources.[44] This demonstrates that the global trend<br />
towards increasing utilisation of renewable energy<br />
sources is extending to India and the coal industry is<br />
declining.<br />
The United Nations (UN) recognises that climate<br />
change is a threat to human health and rights.[4] In 2016,<br />
Australia ratified the Paris Agreement with a declaration<br />
to work towards combatting climate change. Yet due to<br />
the export nature of the proposed Adani Carmichael coal<br />
mine, these Australian sourced emissions will not count as<br />
part of our Intended Nationally Determined Contributions.<br />
The UN’s Committee on Economic, Social and Cultural<br />
Rights (CESCR) stated that Australia’s increasing carbon<br />
footprint is “at risk of worsening in the coming years”[46]<br />
which would undermine the vision of the Paris Agreement<br />
and its predecessor, the Kyoto Protocol, both of which we<br />
are signatories to. The CESCR’s panel of international<br />
human rights experts has recommended Australian<br />
politicians “review (their) position in support of coal<br />
mines and coal export”.[46] In light of the USA’s recent<br />
withdrawal from the Paris Agreement, it is of increased<br />
importance for Australia and other developed countries<br />
to consider the impact of our carbon footprint beyond our<br />
national border.<br />
Conclusion<br />
The real cost of Australia enabling the continuing<br />
burning of coal will be measured in health impacts, hunger<br />
and humanitarian disasters. Therefore, the Australian and<br />
Queensland governments must act now to preserve the<br />
health of Australian and global citizens into the future.<br />
The medical profession has a long and proud history of<br />
protecting public health. We must add our voices to the<br />
wave of protest to stop the construction of the world’s<br />
largest coal mine, and for the sake of our patients’ health,<br />
to make coal history.<br />
Acknowledgements<br />
Doctors for the Environment Australia<br />
Photo credit<br />
Julian Meehan, accessed from https://www.flickr.com/<br />
photos/takver/31283359832<br />
Conflict of Interest<br />
None declared<br />
Correspondance<br />
evan.morgan@my.jcu.edu.au<br />
References<br />
1. Queensland Government. Carmichael coal mine and rail project [Internet].<br />
Brisbane QLD: Department of State Development; 2010 Oct 22 [updated <strong>2017</strong><br />
June 19; cited <strong>2017</strong> Aug 28]. Available from: https://www.statedevelopment.qld.<br />
gov.au/assessments-and-approvals/carmichael-coal-mine-and-rail-project.html<br />
2. Australian Government. Carmichael coal and rail infrastructure factsheet<br />
[Internet]. Canberra ACT: Minister for the Environment’s office; 2014 [cited <strong>2017</strong><br />
Aug 28]. Available from: https://www.environment.gov.au/minister/hunt/2014/pubs/<br />
mr20140728-factsheet.pdf<br />
3. Amos, C. Carmichael in context [Internet]. Canberra ACT: The Australia<br />
Institute; 2015 [cited <strong>2017</strong> Aug 28]. Available from: http://www.tai.org.au/content/<br />
carmichael-context<br />
4. World Health Organisation. WHO calls for urgent action to protect health<br />
from climate change [Internet]. Geneva Switzerland: World Health Organisation;<br />
2015 [cited <strong>2017</strong> Aug 28]. Available from: http://www.who.int/globalchange/globalcampaign/cop21/en/<br />
5. McCall, C. Australia’s new coal mine plan: a “public health disaster”.<br />
Lancet [Internet]. <strong>2017</strong> Feb <strong>11</strong>[cited <strong>2017</strong> Aug 28];389(10069):p588.<br />
Available from: http://www.thelancet.com/journals/lancet/article/PIIS0140-<br />
6736(17)30329-X/fulltext<br />
6. McGrath, C. Carmichael coal mine cases in the Land Court and Supreme<br />
Court of Qld [Internet]. Brisbane QLD: Environmental Law Australia; 2010 [updated<br />
<strong>2017</strong> Aug 25; cited <strong>2017</strong> Aug 28]. Available from: http://envlaw.com.au/carmichaelcoal-mine-case/<br />
7. Portier C, Thigpen Tart K. A human health perspective on climate<br />
change [Internet]. North Carolina, USA: National Institute of Environmental Health<br />
Sciences; 2010 Apr 22 [cited <strong>2017</strong> Oct 15]. 80p. Available from: https://www.niehs.<br />
nih.gov/health/materials/a_human_health_perspective_on_climate_change_<br />
full_report_508.pdf<br />
8. Dennekamp M, Carey M. Air quality and chronic disease: why action on<br />
climate change is also good for health. NSW Public Health Bulletin. 2010 July 16<br />
[cited <strong>2017</strong> Oct 20]; 21(6): <strong>11</strong>5-121. Available from: http://www.publish.csiro.au/<br />
NB/NB10026<br />
9. State of the Environment 20<strong>11</strong> Committee. Australia State of the<br />
environment 20<strong>11</strong> [Internet]. Canberra, ACT: Department of Sustainability,<br />
Environment, Water, Population and Communities; 20<strong>11</strong> [cited <strong>2017</strong> Oct 20]. 940p.<br />
Available from: https://soe.environment.gov.au/sites/g/files/net806/f/soe20<strong>11</strong>-<br />
report-complete.pdf?v=1488164460<br />
10. Yang Q, Chen Y, Shi Y, Burnett R, McGrail K, Krewski D. Association<br />
between ozone and respiratory admissions among children and the elderly in<br />
Vancouver, Canada. Inhal Toxicol [Internet]. 2003 Nov [cited <strong>2017</strong> Oct 20]; 15(13):<br />
24
1297-308. Available from: https://www.ncbi.nlm.nih.gov/<br />
<strong>11</strong>. Hardin B, Kelman B, Saxon A. Adverse human health effects associated<br />
with molds in the indoor environment. J Occup Environ Med [Internet]. 2003 May<br />
[cited <strong>2017</strong> Oct 20]; 45(5): 470-478. Available from: https://www.ncbi.nlm.nih.gov/<br />
pubmed/12762072<br />
12. D’Amato G, Cecchi L. Effects of climate change on environmental factors<br />
in respiratory allergic diseases. Clin Exp Allergy. 2008 Aug [cited <strong>2017</strong> Oct 20];<br />
38(8): 1264-1274. Available from: https://www.ncbi.nlm.nih.gov/pubmed/18537982<br />
13. Kirkpatrick B, Fleming L, Bean J, Nierenberg K. Aerosolized red tide toxins<br />
(Brevetoxins) and asthma: Continued health effects after 1 hour beach exposure.<br />
Harmful Algae [Internet]. 20<strong>11</strong> Jan 1 [cited <strong>2017</strong> Oct 20]; 10(2): 138-143. Available<br />
from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3076944/<br />
14. Bacarelli A, Martinelli I, Zanobetti A. Exposure to particulate air pollution<br />
and risk of deep vein thrombosis. Arch Intern Med [Internet]. 2008 [cited <strong>2017</strong><br />
Oct 20]; 168(9): 920-927. Available from: https://jamanetwork.com/journals/<br />
jamainternalmedicine/fullarticle/414214<br />
15. Brook R. Cardiovascular effects of air pollution. Clin Sci (Lond) [Internet].<br />
2008 Sep [cited <strong>2017</strong> Oct 20]; <strong>11</strong>5(6): 175-187. Available from: https://www.ncbi.<br />
nlm.nih.gov/pubmed/1869<strong>11</strong>54<br />
16. Jerret M, Burnett R, Pope C, Kazuhiko I. Long-term ozone exposure and<br />
mortality. N Engl J Med [Internet]. 2009 Mar 12 [cited <strong>2017</strong> Oct 20]; 360: 1085-1095.<br />
Available from: http://www.nejm.org/doi/full/10.1056/NEJMoa0803894#t=article<br />
17. Donoghue E, Graham M, Jentzen J, Liftschulz B, Luke J, Mirchandani H.<br />
Criteria for the diagnosis of heat-related deaths: National Association of Medical<br />
Examiners. Position Paper. National Association of Medical Examiners Ad Hoc<br />
Committee on the Definition of Heat-Related Fatalities. Am J Forensic Med Pathol<br />
[Internet]. 1997 Mar [cited <strong>2017</strong> Oct 20]; 18(1): <strong>11</strong>-14. Available from: https://www.<br />
ncbi.nlm.nih.gov/pubmed/9095294?dopt=Abstract<br />
18. Kilbourne E. Heat waves and hot environments. In: Noji E, editor. The<br />
public health consequences of disasters. New York, USA; Oxford University Press;<br />
1997. p245-269.<br />
19. Basu R, Samet J. Relation between elevated ambient temperature and<br />
mortality: a review of the epidemiologic evidence. Epidemiol Rev [Internet]. 2002<br />
[cited <strong>2017</strong> Oct 20]; 24(2): 190-202. Available from: https://academic.oup.com/<br />
epirev/article-lookup/doi/10.1093/epirev/mxf007<br />
20. Toloo G, Hu W, FitzGerald G, Aitken P, Tong S. Projecting excess<br />
emergency department visits and associated costs in Brisbane, Australia, under<br />
population growth and climate change scenarios. Sci Rep [Internet]. 2015 Aug 6<br />
[cited <strong>2017</strong> Oct 20]; 5: 12860. Available from: https://eprints.qut.edu.au/86502/1/<br />
Projecting%20excess%20ED%20visits%20and%20associated%20costs%20<br />
in%20Brisbane.pdf<br />
21. Fritze J, Blashki G, Burke S, Wiseman J. Hope, despair and transformation:<br />
Climate change and the promotion of mental health and wellbeing. Int J Ment<br />
Health Syst [Internet]. 2008 Sep 17 [cited <strong>2017</strong> Oct 20]; 2(1): 13. Available from:<br />
https://ijmhs.biomedcentral.com/articles/10.<strong>11</strong>86/1752-4458-2-13<br />
22. Myers N. Environmental refugees: a growing phenomenon of the 21st<br />
century. Philos Trans R Soc Lond B Biol Sci [Internet]. 2002 Apr 29 [cited <strong>2017</strong><br />
Oct 20]; 357(1420): 609-613. Available from: https://www.ncbi.nlm.nih.gov/<br />
pubmed/12028796<br />
23. United Nations High Commissioner for Refugees. Climate change and<br />
disasters [Internet]. Geneva, Switzerland: UNHCR; 2015 Jan 1 [cited <strong>2017</strong> Oct 20].<br />
Available from: http://www.unhcr.org/en-au/climate-change-and-disasters.html<br />
24. The CNA Corporation [Internet]. Virginia, USA: The CAN Corporation;<br />
2007. National security and the threat of climate change; 2007 [cited <strong>2017</strong><br />
Oct 20]; [p15]. Available from: https://www.cna.org/cna_files/pdf/national%20<br />
security%20and%20the%20threat%20of%20climate%20change.pdf<br />
25. Queensland Government. Black lung white lies – Report number 2<br />
[Internet]. Brisbane QLD: Coal Workers’ Pneumoconiosis Select Committee;<br />
<strong>2017</strong> May [cited <strong>2017</strong> Aug 28]. Available from: http://www.parliament.qld.gov.au/<br />
Documents/TableOffice/TabledPapers/<strong>2017</strong>/5517T467.pdf<br />
26. Climate and Clean Air Coalition. State of global air <strong>2017</strong>: A special report<br />
on global exposure to air pollution and its disease burden [Internet]. Paris France:<br />
Climate and Clean Air Coalition; <strong>2017</strong> [cited <strong>2017</strong> Aug 28]. Available from: http://<br />
www.ccacoalition.org/en/resources/state-global-air-<strong>2017</strong>-special-report-globalexposure-air-pollution-and-its-disease-burden<br />
27. United Nations Framework Convention on Climate Change. The Paris<br />
Agreement [Internet]. New York USA: United Nations; Oct 2016 [updated Oct <strong>2017</strong>;<br />
cited <strong>2017</strong> Oct 15]. Available from: http://unfccc.int/paris_agreement/items/9485.<br />
php<br />
28. The Caribbean’s Climate Justice Hub. #1point5toStayAlive [Internet].<br />
Saint Lucia: 1.5; 2015 [cited <strong>2017</strong> Oct 15]. Available from: http://1point5.info/<br />
whatsup<br />
29. Global Coral Reef Monitoring Network. Status of coral reefs of the<br />
world: 2004 – Chapter 2 New initiatives in coral reef monitoring, research,<br />
management and conservation [Internet]. Gland Switzerland: International Union<br />
for Conservation of Nature; 2004 [cited <strong>2017</strong> Aug 28]. Available from: https://www.<br />
iucn.org/sites/dev/files/import/downloads/cr_status_2004_vol1.pdf<br />
30. Australian Government. Climate change impacts on the fishing industry<br />
[Internet]. Townsville QLD: Great Barrier Reef Marine Park Authority; <strong>2017</strong> [cited<br />
<strong>2017</strong> Sept 21]. Available from: http://www.gbrmpa.gov.au/managing-the-reef/<br />
threats-to-the-reef/climate-change/what-does-this-mean-for-communities-andindustries<br />
31. Environmental Defenders Office Queensland. Adani Carmichael project<br />
receives water licences [Internet]. Brisbane QLD: Environmental Defenders Office;<br />
<strong>2017</strong> May 31 [cited <strong>2017</strong> Aug 28]. Available from: http://www.edoqld.org.au/news/<br />
adani-pending-water-licence/<br />
32. Bourke L, Humphreys J, Wakerman J, Taylor J. Understanding rural and<br />
remote health: A framework for analysis in Australia. Health Place [Internet]. 2012<br />
Mar [cited <strong>2017</strong> Oct 15];18:496-503. Available from: http://www.flinders.edu.<br />
au/medicine/fms/sites/southgate/documents/events/2014/Understanding%20<br />
rural%20and%20remote%20health_a%20framework%20analysis%20for%20<br />
Australia.pdf<br />
33. Guannel G, Arkema K, Ruggiero P, Verutes G. The power of three: coral<br />
reefs, seagrasses and mangroves protect coastal regions and increase their<br />
resilience. PLoS One [Internet]. 2016 July 13 [cited <strong>2017</strong> Aug 28]; <strong>11</strong>(7): e0158094.<br />
Available from: http://journals.plos.org/plosone/article?id=10.1371/journal.<br />
pone.0158094<br />
34. Working Group II Contribution to the Fifth Assessment Report of the<br />
Intergovernmental Panel on Climate Change. Fifth Assessment Report – Impacts,<br />
Adaptation and Vulnerabilities [Internet]. New York USA: Intergovernmental Panel<br />
on Climate Change; 2014 [cited <strong>2017</strong> Oct 10]. Available from: https://www.ipcc.ch/<br />
report/ar5/wg2/<br />
35. Glennon, R. The unfolding tragedy of climate change in Bangladesh<br />
[Internet]. New York USA: Scientific American; <strong>2017</strong> Apr 21 [cited <strong>2017</strong> Aug 28].<br />
Available from: https://blogs.scientificamerican.com/guest-blog/theunfoldingtragedy-of-climate-change-in-bangladesh/<br />
36. United Nations Office for the Coordination of Humanitarian Affairs.<br />
Tropical Cyclone Winston – Feb 2016 [Internet]. New York USA: ReliefWeb; 2016<br />
[cited <strong>2017</strong> Aug 28]. Available from: https://reliefweb.int/disaster/tc-2016-000014-<br />
fji<br />
37. Climate Council of Australia. Risky business: Health, climate and<br />
economic risks of the Carmichael coalmine [Internet]. Sydney NSW: Climate<br />
Council of Australia; <strong>2017</strong> [cited <strong>2017</strong> Sep 21]. Available from: https://www.<br />
climatecouncil.org.au/uploads/5cb72fc98342cfc149832293a8901466.pdf<br />
38. Ministers and Assistant Ministers for the Department of Industry,<br />
Innovation and Science [Internet]. Canberra, ACT: Australian Government; 2016<br />
Sep 30. Canavan’s Speech to CEDA; 2016 Sep 30 [cited <strong>2017</strong> Oct 20]. Available<br />
from: http://www.minister.industry.gov.au/ministers/canavan/speeches/speechceda<br />
39. Sharon Warburton, Chair, Northern Australia Infrastructure Facility.<br />
Speech – Developing Northern Australian Conference [Internet]. Cairns, QLD:<br />
Northern Australia Infrastructure Facility; <strong>2017</strong> June 19 [cited <strong>2017</strong> Oct 20].<br />
Available from: https://naif-gov-au.industry.slicedtech.com.au/wp-content/<br />
uploads/<strong>2017</strong>/06/Speech-Sharon-Warburton-DNA-final-for-web.pdf<br />
40. Australian Government. Our north, our future: White paper on developing<br />
northern Australia [Internet]. Canberra, ACT: Australian Government; 2015 [cited<br />
<strong>2017</strong> Oct 20]. 200p. Available from: http://northernaustralia.gov.au/files/files/<br />
NAWP-FullReport.pdf<br />
41. Australian Government. Northern Australia audit – infrastructure for a<br />
developing north [Internet]. Canberra, ACT: Australian Government; 2015 Jan<br />
[cited <strong>2017</strong> Oct 20]. 306p. Available from: http://infrastructureaustralia.gov.au/<br />
policy-publications/publications/files/IA_Northern_Australia_Audit.pdf<br />
42. Swann, T. Don’t be so naif; Adani and Governance of the Northern<br />
Australia Infrastructure Facility (NAIF) [Internet]. Canberra ACT: The Australia<br />
Institute; Mar <strong>2017</strong> [cited <strong>2017</strong> Oct 15]. Available from: http://www.tai.org.au/sites/<br />
defualt/files/P318%20Dont%20be%20so%20naif%20FINAL.pdf<br />
43. Deloitte Access Economics. Economic Contribution of the Great Barrier<br />
Reef [Internet]. Townsville Qld: Great Barrier Reef Marine Park Authority; Mar 2013<br />
[cited <strong>2017</strong> Oct 15]. 52p. Available from: http://www.environment.gov.au/system/<br />
files/resources/a3ef2e3f-37fc-4c6f-ab1b-3b54ffc3f449/files/gbr-economiccontribution.pdf<br />
44. Burton B, Fernandes A. Is the Indian coal domino about to fall? [Internet].<br />
Australia: Renew Economy; Dec 2016 [cited <strong>2017</strong> Oct 15]. Available from: http://<br />
reneweconomy.com.au/indian-coal-domino-fall-91973/<br />
45. United Nations Framework Convention on Climate Change. Paris<br />
Agreement – Status of Ratification [Internet]. New York USA: United Nations; Dec<br />
2015 [updated Apr <strong>2017</strong>; cited <strong>2017</strong> Oct 15]. Available from: http://unfccc.int/<br />
paris_agreement/items/9444.php<br />
46. United Nations Committee on Economic, Social and Cultural Rights.<br />
Concluding observations on the fifth periodic report of Australia [Internet]. Geneva<br />
Switzerland: United Nations Office of the High Commissioner; <strong>2017</strong> July <strong>11</strong> [cited <strong>2017</strong><br />
Aug 28]. Available from: http://tbinternet.ohchr.org/_layouts/treatybodyexternal/<br />
Download.aspx?symbolno=E%2fC.12%2fAUS%2fCO%2f5&Lang=en<br />
25
Paddling upstream:<br />
Experiences from a medical placement in<br />
rural Papua New Guinea<br />
[Feature Article]<br />
Nicholas Snels<br />
I sit in an office on my GP rotation. My insides burn,<br />
courtesy of my morning doxycycline. The patient, who<br />
has come in with fever and a sore throat, coughs. I flinch.<br />
My eyes fly across the room, searching for a face mask.<br />
Then I remember I am back in Toowoomba, and not<br />
every fever is likely due to an unpronounceable parasitic<br />
infection. This is perhaps a slight<br />
dramatisation of my GP block, however,<br />
I cannot help but cast my mind back to<br />
when a cough could signal something<br />
far more sinister than an URTI.<br />
I was recently given the opportunity<br />
to spend six weeks at the Kiunga<br />
District Hospital in rural Papua New<br />
Guinea (PNG) as part of the Griffith<br />
Rural Medical Education program. Every rotation block,<br />
four students are given the opportunity to spend six<br />
weeks in Kiunga hospital. For those as unfamiliar with<br />
Papua New Guinean geography as me prior to my visit,<br />
Kiunga is a town in the western province of PNG, on<br />
the banks of the Fly River. The hospital serves a town<br />
of approximately 13000 people, in addition to being<br />
a referral centre for the region, with approximately 45<br />
beds spread over numerous wards (medical, surgical,<br />
women’s), as well as a pathology lab and an emergency<br />
department/outpatient department (OPD). The wards<br />
are managed by a physician and a surgical/obstetrics<br />
and gynaecology doctor, health extension officers,<br />
community health workers and nurses. As medical<br />
students we were well accustomed to being at the<br />
bottom of this hierarchy; however, in PNG we were given<br />
far greater responsibility.<br />
General Ward<br />
Nick is a final year medical student from Griffith University. Throughout his degree he<br />
has been interested in gaining clinical exposure in a variety of settings, ranging from<br />
a rural experience in Warwick to furthering an interest in global health in Papua New<br />
Guinea and India.<br />
Common things occur commonly. This phrase had<br />
been thrown at me all throughout my clinical years. Most<br />
coughs are probably not cancer, most sore throats are<br />
not the harbinger of quinsy. However, the medical ward<br />
showed us just how context-specific this phrase is, with<br />
...the words ‘common things<br />
occur commonly, therefore,<br />
this is probably tuberculosis or<br />
malaria’ heard at least once<br />
per ward round.<br />
the words ‘common things occur commonly, therefore,<br />
this is probably tuberculosis or malaria’ heard at least<br />
once per ward round. Ascites was probably due to<br />
abdominal seeding of tuberculosis, a headache was<br />
probably due to cerebral malaria. We quickly learned to<br />
appease the ward doctor by suggesting tuberculosis as<br />
the cause for nearly every presenting<br />
complaint. The range of tropical<br />
diseases surpassed my expectations,<br />
from tuberculosis, malaria and<br />
malnutrition, to less common cases of<br />
severe AIDS and Buruli ulcers. I was<br />
even exposed to diseases I had not<br />
even fathomed I might see, such as<br />
toxic epidermal necrolysis as a result<br />
of leprosy medications.<br />
Our time in the general ward consisted of a morning<br />
ward round followed by jobs, and it was eye-opening<br />
to see how health care could be limited by a lack of<br />
resources. Intramuscular antimalarials often ran out,<br />
meaning that oral antimalarials had to be followed by<br />
an ondansetron chaser. There was no adrenaline in the<br />
emergency room, meaning it was necessary to trawl the<br />
hospital to find some before it was needed. A lack of<br />
funds for staff meant the occupants of the tuberculosis<br />
ward were at the far end of the general ward, placing<br />
the rest of the patients at risk of nosocomial infection.<br />
Consequently, we soon learned that ward rounds began<br />
by applying appropriate PPE as soon as we entered the<br />
building (Figure 1).<br />
One patient made a particular impression on me. M<br />
was a 7-month old female admitted due to malnutrition.<br />
Throughout the week, she slowly gained weight and<br />
started to take an interest in the strange pale humans<br />
trying to make her smile with a toy koala, and was<br />
eventually discharged. The next week she returned with<br />
a cough, initially thought to be viral in origin. However,<br />
common things occur commonly, and imaging suggested<br />
M had tuberculosis. While unable to pinpoint the exact<br />
26
cause, it was possible that her long stay on the ward<br />
could have been the source. It was incredibly frustrating<br />
knowing that if the hospital had funding, these incidents<br />
could be prevented. Nonetheless, the case of M is not an<br />
isolated one, and the lack of resources was evident in all<br />
the areas of the hospital during our stay.<br />
Surgical Ward<br />
Having heard of other elective experiences, I<br />
expected that surgery in a developing country would<br />
be exceptionally hands-on, however, this was not what<br />
I experienced. The reasons for this were unique. A<br />
number of issues, such as the surgeon having malaria,<br />
or the building having no functioning water with which to<br />
sterilize equipment, resulted in my group having relatively<br />
few surgeries to attend. Something I was exposed to,<br />
however, was overcoming challenges in a resource-poor<br />
setting. In the absence of K-wire cutters, garden pliers<br />
were sterilised with alcohol wipes; on another occasion,<br />
an abdominal drain was secured in place with a tongue<br />
depressor snapped and taped together. The persistence<br />
shown by the staff to make the most of what was<br />
available was inspiring, especially given they face these<br />
challenges continually.<br />
Women’s Ward<br />
Figure 1. Students in PPE<br />
In my third year, I was placed in a rural hospital in<br />
Australia which did not see a huge amount of obstetrics.<br />
You could say I was unprepared for<br />
obstetrics in Kiunga.<br />
Caesarian sections were an<br />
uncommon event, meaning that we<br />
witnessed births which probably<br />
would not have happened in<br />
Australia. Examples of this include<br />
a mother with malaria struggling to<br />
give birth due to severe lethargy, or<br />
the two breech births occurring during my six weeks.<br />
In an Australian setting, we are used to working under<br />
the guidance of a senior team member, especially in<br />
a high-intensity situation. However, in PNG we were<br />
In an Australian setting, we are used<br />
to working under the guidance of a<br />
senior team member, especially in a highintensity<br />
situation. However, in PNG we<br />
were expected to step up and start to<br />
manage situations ourselves.<br />
expected to step up and start to manage situations<br />
ourselves. In the maternity suite births were usually<br />
facilitated by one midwife, and if something went wrong,<br />
the focus was on looking after the mother. This meant<br />
that care of the neonate typically came after the mother’s<br />
situation was controlled.<br />
Therefore, on a number of occasions, a routine birth<br />
would end with the midwife handing a limp neonate to two<br />
medical students. Prior to coming to PNG, I was aware of<br />
the debate regarding medical students overstepping their<br />
boundaries while on elective. However, in that moment we<br />
had to make a choice to either stand by and watch the<br />
neonate die due to a lack of resources and staff, or give<br />
it the best chance it could have in the circumstances by<br />
applying pre-departure training in neonatal resuscitation.<br />
It is hard to imagine the situation where there are no<br />
medical students to assist, but sadly due to lack of<br />
staffing that is the situation this hospital faces every<br />
day. We were involved in three such scenarios during<br />
my time in PNG, and I am thankful for the training we<br />
received on resuscitation prior to departure. In saying<br />
that, the unsuccessful resuscitations were amongst the<br />
most confronting moments in medical school, but I am<br />
glad we were present to intervene when no one else was<br />
available.<br />
Not all births were intense, and even in uncomplicated<br />
births we were routinely supported by the midwives to<br />
assist the mother in delivering the child. The midwives<br />
in PNG are incredible, managing most births without<br />
intervention of a doctor, and even performing procedural<br />
skills such as perineal repair and vacuum-assisted<br />
delivery.<br />
Emergency and Outpatient Department<br />
Although other areas of the hospital were perhaps<br />
more confronting, I felt most out of my depth in the OPD.<br />
We were expected to independently see patients and<br />
prescribe medications, with no guidance offered unless<br />
required. While the OPD allowed us to practice our<br />
Pidgin, the language barrier remained a significant issue.<br />
Personally, I felt very uncomfortable prescribing antimalarials<br />
according to a guideline<br />
I did not know well, to a 4-year-old<br />
whose parents I could not explain<br />
anything to, a situation I found<br />
myself in on our first day in the<br />
hospital. The staff were probably<br />
annoyed by my constant questions,<br />
however, I was worried about<br />
overstepping my boundaries as<br />
a student and potentially causing<br />
significant harm. In saying that, the<br />
range of presentations was diverse (although malaria<br />
was exceptionally common), and the chance to practice<br />
our newly-acquired language skills was excellent.<br />
27
Similar to the obstetric department, we were<br />
forewarned that if resuscitation needed to be performed,<br />
we would potentially be in charge. Even with this in mind,<br />
I certainly did not expect to be performing compressions<br />
one Sunday afternoon while wearing thongs and board<br />
shorts. Due to a lack of staff on this particular weekend,<br />
three medical students who had been playing soccer with<br />
the local kids were now attempting to resuscitate a man<br />
who had been in the ED since the morning. Eventually the<br />
doctor arrived to take control, but it is hard to imagine<br />
students in Australia ever being in such a situation.<br />
Social<br />
Aside from the clinical experience, one of the<br />
highlights of the placement was the chance to become<br />
involved in the local community. We stayed in a house<br />
a close walk away from the hospital, meaning that we<br />
often had spare time in the afternoons/weekends. Most<br />
afternoons we played sport with the local kids, and every<br />
Sunday we played a movie for them at the hospital. Not all<br />
of the children were so keen, however, as one particular<br />
girl started crying as soon as she saw us, a sobering<br />
reminder that foreign faces are still uncommon in such<br />
parts of the world.<br />
One of the most surreal experiences was going<br />
to a local club and listening to Justin Bieber while<br />
meeting locals over Papua New<br />
Guinean beer. A local gentleman<br />
was adamant Justin was in fact a<br />
Papua New Guinean artist, but in his<br />
defence the local brew was quite<br />
potent. At the end of the night we<br />
were even offered a lift home by<br />
the police chief, provided we let him<br />
finish his drink first. Another highlight<br />
was being shown wild birds of<br />
paradise by a guide who had taken David Attenborough<br />
to see them years ago. The people were exceptionally<br />
welcoming, often stopping on the street or in the markets<br />
to talk to us and see how we were finding the experience.<br />
Reflections<br />
There were a few main lessons I took away from this<br />
experience in regards to students experiencing a global<br />
health elective. The most striking point was the issue<br />
regarding medical students on electives in resource-poor<br />
settings. This issue deserves a review unto itself, but<br />
suffice to say it became very apparent to me how easy<br />
it could be for an overconfident medical student to abuse<br />
the level of trust placed in them by the local population.<br />
Particularly, in a poorly-resourced setting with a lack of<br />
supervision, students may be placed in situations that<br />
are beyond their level of knowledge. However, in certain<br />
circumstances, capable students, and especially those in<br />
their final year, may be able to have a positive impact on<br />
their chosen placement. Such an experience highlighted<br />
At times it seemed like the health care<br />
workers were battling their way upriver<br />
against a tide of financial constraints and<br />
poor government support, however, the<br />
enthusiasm and dedication shown towards<br />
the people of Kiunga was inspiring.<br />
how aware students must be before embarking upon<br />
such an elective, and to have these issues in their minds<br />
while on the placement to avoid overstepping their scope<br />
of practice.<br />
Such difficulty is exacerbated by the challenges<br />
of healthcare provision in resource-poor settings, and<br />
this placement was invaluable in showing me how it<br />
differs compared to Australia. The shortage of staff,<br />
medications and equipment was evident throughout the<br />
hospital, and it was clear that the entire health system<br />
could be improved by further funding. It was confronting<br />
seeing individuals suffer because the medication they<br />
needed was not available, however, it was inspiring to<br />
see the ways staff attempted to overcome these barriers.<br />
Additionally, the attitude of the staff continually stayed<br />
positive, even in the face of these challenges.<br />
Finally, it was evident to me throughout the placement<br />
that global health challenges in developing nations<br />
are changing. While infectious and tropical diseases<br />
were rife, the impact of chronic conditions such as<br />
cardiovascular disease, hypertension and diabetes was<br />
evident during my time in Kiunga. These conditions were<br />
often poorly managed due to lack of proper medications<br />
and monitoring. Their increasing prevalence coupled with<br />
the lack of resources to manage these conditions mean<br />
students doing a similar placement in the future will face<br />
a host of different conditions.<br />
In summary, this elective<br />
was an excellent experience.<br />
Not only for the clinical<br />
exposure, but also for the<br />
chance to see how healthcare<br />
functions in a resource-poor<br />
setting. At times it seemed<br />
like the health care workers<br />
were battling their way upriver against a tide of financial<br />
constraints and poor government support, however, the<br />
enthusiasm and dedication shown towards the people<br />
of Kiunga was inspiring. Additionally, the chance to<br />
experience life in a rural town in PNG was a highlight in<br />
itself. This placement has, undoubtedly, been one of the<br />
most motivating placements of medical school, and I<br />
strongly urge anyone considering something similar to<br />
take the opportunity.<br />
Acknowledgements<br />
QRME and Graeme Hill for continual support of this<br />
program; Aisha, Ryan and Emily for sharing the experience<br />
and for support throughout difficult times.<br />
Conflicts of interest<br />
None declared<br />
Correspondance<br />
nicholas.snels@griffithuni.edu.au<br />
28
Introduction<br />
Sugar tax -<br />
A sweet solution for obesity?<br />
The obesity epidemic<br />
Over the past few decades, overweight and obesity have<br />
risen to epidemic proportions all over the globe. In 2014,<br />
more than 1.9 billion adults were overweight and 600 million<br />
were obese.[1] In 2013, 42 million children under the age of<br />
five were either overweight or obese, and this is predicted<br />
to increase to 70 million by 2025.[2] The growing prevalence<br />
of childhood obesity is particularly alarming given that it is a<br />
predisposing factor for lifelong obesity.[3] Obesity, defined as<br />
having a body mass index (BMI) greater than or equal to 30, is<br />
a major risk factor for non-communicable diseases such as<br />
cardiovascular disease, diabetes, cancer, and mental illness.<br />
[4] Since non-communicable diseases were responsible for<br />
68% of all deaths in 2012, [5] it is apparent that the health<br />
burden of obesity is high.<br />
Obesity is a complex heterogenous disease that arises<br />
from an interplay between our genes and the environment<br />
we live in. Highly energy-dense diets combined with a lack<br />
of adequate physical activity leads to a positive caloric<br />
balance and hence weight gain in genetically susceptible<br />
individuals. Our diet and physical activity are increasingly<br />
[Review]<br />
Saiuj Bhat<br />
Saiuj is a first year medical student at the University of Western Australia with a passion<br />
for understanding the social and commercial determinants of health. He also has<br />
an interest in tissue engineering, in particular organoid technology, and the promising<br />
that holds for many aspects of medicine in the future. He graduated last year with<br />
Honours in pharmacology.<br />
“<br />
Abstract<br />
Background: The rising prevalence of obesity and obesity-related illnesses parallels the increase in sugar consumption<br />
across the globe. To limit consumption of sugar and tackle obesity, the World Health Organization has recommended<br />
that member states implement a tax on sugar. Such a tax is envisioned to reduce sugar consumption at a societal<br />
level, generate stable revenue for governments, and drive product reformulation. However, at present there is insufficient<br />
evidence to suggest any beneficial effect of a sugar tax on the incidence and prevalence of obesity.<br />
Aim: This review examines the effectiveness of a sugar tax as an obesity prevention strategy.<br />
Methods: A qualitative review of modelling and observational studies investigating the link between sugar tax and<br />
obesity, and conducted over the past ten years, was carried out.<br />
Findings: Modelling studies suggest that a tax on high-sugar foods and beverages is likely to have beneficial effects on<br />
obesity as increased price of taxed items leads to reduced consumption. However, observational studies suggest little<br />
benefit of a sugar tax on actual obesity rates in a population. Taxes in combination with other policy and regulatory<br />
approaches, for example health food subsidies and education campaigns, might be more effective than a tax on its own.<br />
Conclusion: A tax on sugar is likely to be a step in the right direction as it would raise public awareness of the negative<br />
health effects of excess sugar and de-normalise consumption of excess sugar.<br />
shaped and driven by broader social, cultural, economic, and<br />
political landscapes that are often beyond individual control<br />
and awareness.[6] The modern obesogenic environment,<br />
which provides easy access to calorie-rich processed food<br />
and encourages sedentary lifestyle, is mismatched to human<br />
physiology that evolved to survive in an environment of food<br />
scarcity.[7] At a population level, obesity can be viewed as<br />
a manifestation of a global economic system that currently<br />
prioritises wealth creation over health creation.[8]<br />
Obesity’s sweet tooth<br />
”<br />
In recent decades, the rising prevalence of obesity has<br />
closely paralleled the burgeoning consumption of sugar all<br />
over the world.[9] Sugar is recognised as one of the biggest<br />
risk factors for obesity,[10-15] and the leading source of<br />
sugar in the diet is sugar sweetened beverages (SSBs).[15]<br />
Therefore, the current review will focus on SSBs as a proxy<br />
for sugar and the discussion about policies aimed at limiting<br />
sugar intake (i.e. sugar taxes), will predominantly revolve<br />
around SSBs.<br />
SSBs are non-alcoholic beverages with added sugar and<br />
include soft drinks, fruit drinks, sports drinks, energy drinks,<br />
29
iced tea and coffee, and lemonade. SSBs are becoming<br />
increasingly popular in low- and middle-income countries, with<br />
Latin America and Asia leading the world in consumption.[16]<br />
The worldwide impact of SSBs on the burden of adiposityrelated<br />
cardiovascular disease, cancer, and diabetes is<br />
estimated at a total of 8.5 million (95% CI: 2.8 – 19.2)<br />
disability-adjusted life years (DALYs) [17].<br />
Limiting the intake of free<br />
sugars to less than 10% of total<br />
daily energy consumption is<br />
strongly recommended by the<br />
World Health Organisation and the<br />
US Dietary Guidelines Advisory<br />
Committee.[18, 19] For every additional serving of SSB per<br />
day, the likelihood of a child becoming obese increases by<br />
60% over the course of two years.[20] The energy obtained<br />
from SSBs is added to an individual’s total energy intake<br />
rather than displacing other sources of calories due to the<br />
poor satiating properties of sugar in liquid form.[21] The net<br />
increase in calorie consumption is likely to contribute to an<br />
increase in body mass. Given the high burden of obesityrelated<br />
illnesses on healthcare systems [17] and the strong<br />
evidence linking excess consumption of SSBs to obesity in<br />
children and adults,[15, 22] a reduction in SSB consumption is<br />
warranted. A decrease in consumption is especially pertinent<br />
as the major SSB consumers are children, adolescents and<br />
poorly educated individuals from lower socio-economic<br />
strata of society who may be less aware of the harmful<br />
effects of added sugar.[10]<br />
Sugar tax as an obesity prevention strategy?<br />
“obesity can be viewed as a manifestation<br />
of a global economic system that currently<br />
prioritises wealth creation over health<br />
creation.”<br />
The success of an SSB tax as an obesity prevention<br />
strategy remains controversial. The plethora of studies<br />
investigating the link between sugar taxation and obesity<br />
prevention demonstrate conflicting results. There is currently<br />
no consensus regarding the best approach to implement a<br />
sugar tax. Furthermore, existing meta-analyses on the topic<br />
show inconsistent findings and are<br />
unable to include many primary<br />
studies in their analysis owing to<br />
methodological inconsistencies.<br />
Recognising these limitations,<br />
this review provides a brief<br />
overview of the current literature on the effectiveness of<br />
a sugar tax as an obesity prevention strategy. Given that<br />
existing studies have been performed in both developing and<br />
developed nations, this review adopts a global perspective on<br />
the issue of sugar taxation. The theoretical basis of a sugar<br />
tax, its economic feasibility, and effectiveness with regards<br />
to obesity prevention will be examined. Alternative strategies<br />
for curbing the obesity epidemic, such as regulation of<br />
advertisements and food labels, are beyond the scope of this<br />
review and will not be explored.<br />
Methods<br />
Electronic databases (PubMed and Web of Science) were<br />
searched for relevant journal articles between 1 January<br />
2007 and 1 July <strong>2017</strong>. The year 2007 was chosen to ensure<br />
included studies were relevant to modern dietary habits and<br />
practices.<br />
Population health interventions aimed at curbing the<br />
consumption of excess sugar are pertinent to curtail<br />
the obesity epidemic. Price is one of the key factors<br />
influencing food purchasing behaviour. People tend to reduce<br />
consumption of unhealthy foods in response to increased<br />
prices of such products.[23] To discourage purchase of<br />
SSBs and address the growing burden of obesity, countries<br />
such as France, Mexico, the UK, and Hungary, and several<br />
jurisdictions in the USA, have implemented a tax on sugar.[10]<br />
Following implementation of a €0.<strong>11</strong> per 1.5 L excise tax on<br />
SSBs, which translated to a 6% price increase, France saw<br />
a 6.7% decline in demand for cola in the first two years.[24]<br />
SSBs are a sensible target for a sugar tax as they have a high<br />
calorie density with no additional nutritional value [10, 25] and<br />
can be clearly defined for policy implementation.[2]<br />
A number of assumptions underscore the success of an<br />
SSB tax [26]: first, the tax must be passed onto consumers,<br />
leading to an increase in cost; second, SSBs follow the law<br />
of demand; and finally, the tax leads to a significant net<br />
reduction in energy intake despite substitution by consumers,<br />
for example by increasing consumption of fruit juices with<br />
comparable caloric content.[27] While a tax on sugary<br />
drinks may not be the silver bullet for obesity on its own, it<br />
has the potential to slow the epidemic. For this reason,<br />
recommendations to implement diet-related taxes should be<br />
taken seriously.[28, 29]<br />
The following search strategy was used: (tax* OR price*<br />
OR economic* OR financial*) AND (sugar OR sweetened<br />
OR beverage* OR drink*) AND (intake OR consumption OR<br />
demand OR sale* OR diet OR weight OR overweight OR<br />
obes* OR body mass index OR BMI).<br />
Searches were limited to articles published in English.<br />
Relevant articles were also identified by searching the<br />
reference lists of included studies. Abstracts were assessed<br />
for suitability of inclusion. Studies that were found to be<br />
suitable were read in full and their salient features reported<br />
here.<br />
Economic feasibility of a sugar tax<br />
Consumers do not bear the full costs of their decisions<br />
when it comes to high-calorie foods and beverages.[30] It<br />
is estimated that an individual with a BMI between 30 and<br />
35 will accumulate 30% higher medical costs than a normal<br />
weight individual;[31] this increases to 50% in individuals<br />
with a BMI greater than 35.[32] In Canada, obesity-related<br />
healthcare costs are close to $6 billion [33] whereas in<br />
Australia this figure is close to $10.7 billion.[34] In addition<br />
to direct healthcare costs, there are indirect costs to the<br />
community associated with absenteeism and obesity-related<br />
premature death.[35]<br />
30
A number of modelling studies have reported substantial<br />
healthcare cost savings and stable revenue streams from a<br />
tax on sugar.[14, 36-38] For example, annual healthcare cost<br />
savings of $23.6 billion (95% CI: 9.33 – 54.9) and annual<br />
revenue of $12.5 billion (95% CI: 8.92 – 14.1) have been<br />
predicted for a tax of $0.01 per ounce of sugar in the United<br />
States (US).[39] Importantly, a sugar tax combined with a fruit<br />
and vegetable subsidy is deemed to be poverty neutral,[37] an<br />
important consideration given the significantly higher relative<br />
cost of fresh produce,[40] especially in rural and remote<br />
communities. The revenue generated from an SSB tax can<br />
be used to cover the healthcare costs of obesity, support<br />
subsidies on healthy food options, and fund public and school<br />
education campaigns promoting childhood nutrition and<br />
obesity prevention.<br />
“a sugar tax combined with a fruit and<br />
vegetable subsidy is deemed to be poverty<br />
neutral, an important consideration given<br />
the significantly higher relative cost of fresh<br />
produce, especially in rural and remote<br />
communities.”<br />
Effectiveness of a sugar tax for preventing obesity<br />
Of various taxes on “unhealthy” foods, a tax on sugar was<br />
modelled to have the biggest health gain in the Australian<br />
population, equating to 270,000 DALYs (95% CI: 250,000<br />
– 290,000) averted.[37] The effect of a sugar tax on BMI<br />
was found to be modest, equating to a BMI reduction of<br />
0.1 in males and 0.06 in females, and a decline in obesity<br />
prevalence of 2.7% in males and 1.2% in females [36]. In a<br />
study modelling the German population, a 20% SSB tax was<br />
shown to reduce the prevalence of obesity by 4% in males<br />
aged 20 to 29.[41] Similarly, a modelling study by Cancer<br />
Research UK estimated that a 20% tax on SSBs could<br />
prevent 3.7 million people from becoming obese by 2025.<br />
Significant, albeit small, inverse associations between SSB<br />
taxes and weight gain have been reported by other modelling<br />
studies.[15] These could represent important changes over<br />
time and alter the prevalence of obesity at a population level.<br />
[42] Importantly, reductions in energy consumption were more<br />
pronounced in low- and middle-income groups.[38, 41, 43]<br />
One of the biggest limitations of these studies is that they<br />
are population models.[37] They rely on national data which<br />
may be outdated and assume a linear relationship between<br />
weight changes and energy consumption without accounting<br />
for substitution behaviour by consumers and often relies on<br />
self-reported data.[41] The substitution effect is an obvious<br />
confounder in studies that do not classify fruit juices as SSBs,<br />
despite juices often containing more sugar than soft drinks.<br />
[14] Another limitation of modelling studies is the lack of<br />
information on long-term SSB price elasticity that is specific<br />
to geographic and economic subgroups.[14]<br />
Six months after implementation of an SSB excise tax<br />
($0.01 per ounce), consumption of SSBs decreased in<br />
Berkeley, California (–21%) and increased in comparable<br />
neighbouring cities that did not levy a sugar tax (+4%). Of the<br />
124 people who reported changing drinking habits as a result<br />
of the tax, 82% reported drinking SSBs less frequently and<br />
40% reported drinking smaller sizes because of the tax.[44]<br />
Similarly, following introduction of an SSB tax (1 peso/litre)<br />
by the Mexican government, the purchase of SSBs declined<br />
by an average of 6% during the first year of the tax and this<br />
decline was greater in low income groups.[45] The average<br />
Mexican purchased 4.2 litres less taxed beverages than<br />
expected during the first year, however, purchase of untaxed<br />
beverages increased by 13 litres on average.[45] Whether the<br />
increased consumption of untaxed beverages compensated<br />
for the reduced caloric intake due to the decline in taxed<br />
beverages was unable to be determined, so the effect of the<br />
sugar tax on net caloric intake remains to be seen. Given<br />
their short time frame, these observational studies provide<br />
no indication of the effect of a sugar tax on actual obesity<br />
rates in a population.<br />
Similarly, surveys investigating consumers’ purchasing<br />
behaviour may not necessarily predict their actual purchasing<br />
habits.[46] This is critical in light of the fact that a 20% tax on<br />
SSBs did not result in an appreciable reduction in consumers’<br />
likelihood to buy SSBs, despite their perception that they were<br />
more expensive.[46] Notwithstanding these pitfalls, a review<br />
of cross-sectional and longitudinal studies investigating the<br />
impact of sugar taxes on weight gain found several studies<br />
that demonstrated an inverse association between price<br />
increase of SSBs and point prevalence of overweight and<br />
obesity.[13] However, the magnitude of change reported in<br />
these studies was small.[13]<br />
Outlook<br />
Reduced consumption of sugar by virtue of an SSB tax<br />
may not necessarily translate to decreased body weight,<br />
particularly if unhealthy alternatives still exist. A tax on<br />
SSBs will only be effective in reducing obesity when there<br />
is no substitution with another untaxed high-calorie food or<br />
beverage.[47] A tax on sugar-rich foods (e.g. confectionary)<br />
in conjunction with a tax on SSBs would reduce the likelihood<br />
of substitution and therefore increase the effectiveness of<br />
the public health intervention. Taxes on high-fat foods will<br />
need to be considered in the future as adjuncts to the sugar<br />
tax. Given the complexity of taxing foods high in sugar and<br />
fat, and limited research on their effectiveness, this requires<br />
further study.<br />
In addition to reducing calorie intake through a sugar<br />
tax, other aspects of the obesogenic environment that<br />
require monitoring and regulation include food labelling,<br />
food portions, food advertisements, and plain packaging. A<br />
sugar tax on its own is unlikely to be the panacea for obesity<br />
prevention. It is widely accepted that taxes have the potential<br />
to reduce sugar consumption, drive production reformulation,<br />
and generate substantial revenue for governments.[16] While<br />
it appears plausible that reduced sugar consumption and<br />
product reformulation would be beneficial to tackle obesity,<br />
whether this is actually the case remains to be seen. To<br />
address the obesity epidemic, a number of other population<br />
level policy measures, including advertising restriction,<br />
31
eformulation targets, health star rating systems, promotion<br />
of healthy transport choices, and sustained high-impact<br />
education campaigns are warranted.[48]<br />
While the effect of sugar taxes on SSB consumption<br />
and obesity have been carried out in some low- and middleincome<br />
groups,[38, 41, 43] there is a paucity of literature<br />
from developing nations on the impact of decreasing SSB<br />
consumption on obesity rates. This is pertinent given that lowand<br />
middle-income nations are disproportionately impacted<br />
by obesity and related non-communicable diseases.<br />
“A sugar tax on its own is unlikely to be<br />
the panacea for obesity prevention.”<br />
Conclusion<br />
Obesity and obesity-related diseases are a significant<br />
burden on healthcare systems around the world. The global<br />
prevalence of obesity has increased and excess consumption<br />
of sugar, in particular SSBs, is one of the strongest drivers<br />
of that increase. To curb the obesity epidemic, a number of<br />
countries have adopted various forms of sugar taxes. While<br />
theoretically and economically sound, a sugar tax on its own<br />
might be insufficient to curb the obesity epidemic. However,<br />
a tax on sugar is likely to be a step in the right direction as it<br />
would raise public awareness of the adverse health effects<br />
of excess sugar and de-normalise excess consumption.<br />
A tax on SSBs can also encourage industry to reformulate<br />
its products with lower sugar levels. Taxes in combination<br />
with other policy and regulatory approaches, for example<br />
subsidies to healthy foods, graphic warning labels, and<br />
awareness campaigns, might be more effective to curb the<br />
obesity epidemic than a tax on its own. A sustained, focussed,<br />
and multi-pronged public health intervention worked in the<br />
past against Big Tobacco. There is no reason to believe that<br />
similar perseverance will not work against Big Sugar.<br />
Conflicts of interest<br />
None declared<br />
Correspondance<br />
saiujbhat59@hotmail.com<br />
References<br />
1. World Health Organisation. Obesity and overweight [Internet].<br />
2016 [cited <strong>2017</strong> March 24]. Available from: http://www.who.int/<br />
mediacentre/factsheets/fs3<strong>11</strong>/en/<br />
2. World Health Organisation. Report of the commission<br />
of ending childhood obesity [Internet]. 2016 [cited<br />
<strong>2017</strong> March 24]. Available from: http://apps.who.int/iris/<br />
bitstream/10665/204176/1/9789241510066_eng.pdf?ua=1<br />
3. Bays H, Scinta W. Adiposopathy and epigenetics: an<br />
introduction to obesity as a transgenerational disease. Curr Med<br />
Res Opin. 2015 Nov;31(<strong>11</strong>):2059-69.<br />
4. James WP. WHO recognition of the global obesity epidemic.<br />
Int J Obes (Lond). 2008 Dec;32 Suppl 7:S120-6.<br />
5. World Health Organisation. Global status on noncommunicable<br />
diseases 2014 [Internet]. Geneva: WHO Press; 2014<br />
[cited <strong>2017</strong> March 24]. Available from: http://www.who.int/nmh/<br />
publications/ncd-status-report-2014/en/<br />
6. Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT,<br />
Moodie ML, et al. The global obesity pandemic: shaped by global<br />
drivers and local environments. Lancet. 20<strong>11</strong> Aug;378(9793):804-<br />
14.<br />
7. Albuquerque D, Stice E, Rodríguez-López R, Manco L,<br />
Nóbrega C. Current review of genetics of human obesity: from<br />
molecular mechanisms to an evolutionary perspective. Mol Genet<br />
Genomics, 2015 Aug;290(4):<strong>11</strong>91-221.<br />
8. Kickbusch I, Allen L, Franz C. The commercial determinants<br />
of health. Lancet Glob Health. 2016 Dec;4(12):e895-e896. DOI:<br />
10.1016/S2214-109X(16)30217-0.<br />
9. Hu FB, Malik VS. Sugar-sweetened beverages and risk of<br />
obesity and type 2 diabetes: epidemiologic evidence. Physiol Behav.<br />
2010 Apr;100(1):47-54.<br />
10. Brownell KD, Farley T, Willett WC, Popkin BM, Chaloupka<br />
FJ, Thompson JW, et al. The public health and economic benefits<br />
of taxing sugar-sweetened beverages. New Eng J Med. 2009<br />
Oct;361(16):1599-1605.<br />
<strong>11</strong>. Han E, Powell LM. Consumption patterns of sugarsweetened<br />
beverages in the United States. J Acad Nutr Diet. 2013<br />
Jan;<strong>11</strong>3(1):43-53.<br />
12. Welsh JA, Sharma AJ, Grellinger L, Vos MB. Consumption<br />
of added sugars is decreasing in the United States. Am J Clin Nutr.<br />
20<strong>11</strong> Sep;94(3):726-734.<br />
13. Escobar MAC, Veerman JL, Tollman SM, Bertram MY, Hofman<br />
KJ. Evidence that a tax on sugar sweetened beverages reduces the<br />
obesity rate: a meta-analysis. BMC Public Health. 2013 Nov;13:1072.<br />
14. Sanchez-Romero LM, Penko J, Coxson PG, Fernandez<br />
A, Mason A, Moran AE, et al. Projected impact of mexico’s sugarsweetened<br />
beverage tax policy on diabetes and cardiovascular<br />
disease: A modeling study. PLoS Med [Internet]. 2016 Nov [cited <strong>2017</strong><br />
July 6];13(<strong>11</strong>):e1002158. DOI: 10.1371/journal.pmed.1002158.<br />
15. Bes-Rastrollo M, Sayon-Orea C, Ruiz-Canela M, Martinez-<br />
Gonzalez MA. Impact of sugars and sugar taxation on body weight<br />
control: A comprehensive literature review. Obesity (Silver Spring).<br />
2016 Jul;24(7):1410-26.<br />
16. Roache SA, Gostin LO. The untapped power of soda taxes:<br />
incentivizing consumers, generating revenue, and altering corporate<br />
behavior. Int J Health Policy Manag. <strong>2017</strong> Sep;6(9):489-493.<br />
17. Singh GM, Micha R, Khatibzadeh S, Lim S, Ezzati M,<br />
Mozaffarian D. Estimated global, regional, and national disease<br />
burdens related to sugar-sweetened beverage consumption in<br />
2010. Circulation. 2015 Aug; 132(8):639-66.<br />
18. World Health Organisation Guideline: Sugars intake for adults<br />
and children [Internet]. 2015 [cited <strong>2017</strong> March 24]. Available from: http://<br />
apps.who.int/iris/bitstream/10665/149782/1/9789241549028_<br />
eng.pdf<br />
19. Dietary Guidelines Advisory Committe. Advisory report<br />
to the secretory of health and human services and the secretary<br />
of agriculture [Internet]. 2015 [cited <strong>2017</strong> March 24]. Available<br />
from: https://health.gov/dietaryguidelines/2015-scientific-report/<br />
pdfs/scientific-report-of-the-2015-dietary-guidelines-advisorycommittee.pdf<br />
20. Ludwig DS, Peterson KE, Gortmaker SL. Relation<br />
between consumption of sugar-sweetened drinks and childhood<br />
obesity: a prospective, observational analysis. Lancet. 2001<br />
Feb;357(9255):505-508.<br />
21. De Castro JM. The effects of the spontaneous ingestion<br />
of particular foods or beverages on the meal pattern and overall<br />
nutrient intake of humans. Physiol Behav. 1993 Jun; 53(6):<strong>11</strong>33-44.<br />
22. Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened<br />
beverages and weight gain in children and adults: a systematic<br />
review and meta-analysis. Am J Clin Nutr. 2013 Oct; 98(4):1084-102.<br />
23. Epstein LH, Jankowiak N, Nederkoorn C, Raynor HA, French<br />
SA, Finkelstein E. Experimental research on the relation between<br />
32
food price changes and food-purchasing patterns: a targeted<br />
review. Am J Clin Nutr. 2012 Apr;95(4):789-809.<br />
24. European Competitiveness and Sustainable Industrial Policy<br />
Consortium. Food taxes and their impact on competitiveness<br />
in the agri-food sector [Internet]. Rotterdam, The Netherlands;<br />
2014. Available from: http://webcache.googleusercontent.com/<br />
search?q=cache:zVN-mS-b6wEJ:ec.europa.eu/DocsRoom/<br />
documents/5827/attachments/1/translations/en/renditions/<br />
pdf+&cd=1&hl=en&ct=clnk&gl=au&client=safari<br />
25. Malik VS, Popkin BM, Bray GA, Després J-P, Hu FB. Sugarsweetened<br />
beverages, obesity, type 2 diabetes mellitus, and<br />
cardiovascular disease risk. Circulation. 2010;121(<strong>11</strong>):1356-1364.<br />
26. Nakhimovsky SS, Feigl AB, Avila C, O’Sullivan G, Macgregor-<br />
Skinner E, Spranca M. Taxes on sugar-sweetened beverages<br />
to reduce overweight and obesity in middle-income countries: a<br />
systematic review. PLoS One [Internet]. 2016 Sep [cited <strong>2017</strong> July<br />
6];<strong>11</strong>(9):e0163358. DOI: 10.1371/journal.pone.0163358.<br />
27. Bonnet C, Requillart V. Does the EU sugar policy reform<br />
increase added sugar consumption? An empirical evidence on the<br />
soft drink market. Health Econ. 20<strong>11</strong> Sep;20(9):1012-24.<br />
28. World Health Organisation. Population-based approaches<br />
to childhood obesity prevention [Internet]. 2012 [cited <strong>2017</strong><br />
October 15]. Available from: http://www.who.int/dietphysicalactivity/<br />
childhood/approaches/en/<br />
29. World Health Organisation. Global action plan for the<br />
prevention and control of non-communicable diseases [Internet].<br />
2013 [cited <strong>2017</strong> October 15]. Available from: http://www.who.int/<br />
nmh/events/ncd_action_plan/en/<br />
30. Drewnowski A, Darmon N. The economics of obesity: dietary<br />
energy density and energy cost. Am J Clin Nutr. 2005 Jul;82(1):265S-<br />
273S.<br />
31. Withrow D, Alter DA. The economic burden of obesity<br />
worldwide: a systematic review of the direct costs of obesity. Obes<br />
Rev. 20<strong>11</strong> Feb;12(2):131-41.<br />
32. Buchmueller TC, Johar M. Obesity and health expenditures:<br />
evidence from Australia. Econ Hum Biol. 2015 Apr;17:42-58.<br />
33. Anis AH, Zhang W, Bansback N, Guh DP, Amarsi Z, Birmingham<br />
CL. Obesity and overweight in Canada: an updated cost-of-illness<br />
study. Obes Rev. 2010 Jan;<strong>11</strong>(1):31-40.<br />
34. Colagiuri S, Lee CM, Colagiuri R, Magliano D, Shaw JE,<br />
Zimmet PZ, et al. The cost of overweight and obesity in Australia.<br />
Med J Aust. 2010 Mar;192(5):260-4.<br />
35. Lehnert T, Sonntag D, Konnopka A, Riedel-Heller S, König<br />
HH. Economic costs of overweight and obesity. Best Pract Res Clin<br />
Endocrinol Metab. 2013 Apr; 27(2):105-15.<br />
36. Veerman JL, Sacks G, Antonopoulos N, Martin J. The impact<br />
of a tax on sugar-sweetened beverages on health and health care<br />
costs: a modelling study. PLoS One [Internet]. 2016 Apr [cited <strong>2017</strong><br />
July 6];<strong>11</strong>(4):e0151460. DOI: 10.1371/journal.pone.0151460.<br />
37. Cobiac LJ, Tam K, Veerman L, Blakely T. Taxes and subsidies<br />
for improving diet and population health in Australia: a costeffectiveness<br />
modelling study. PLoS Med [Internet]. <strong>2017</strong> Feb [cited<br />
<strong>2017</strong> July 6];14(2):e1002232. DOI: 10.1371/journal.pmed.1002232.<br />
38. Finkelstein EA, Zhen C, Nonnemaker J, Todd JE. Impact of<br />
targeted beverage taxes on higher- and lower-income households.<br />
Arch Intern Med. 2010 Dec;170(22):2028-2034.<br />
39. Long MW, Gortmaker SL, Ward ZJ, Resch SC, Moodie ML,<br />
Sacks G, et al. Cost effectiveness of a sugar-sweetened beverage<br />
excise tax in the US. Am J Prev Med. 2015 Jul;49(1):<strong>11</strong>2-123.<br />
40. Brownell KD, Frieden TR. Ounces of prevention - the public<br />
policy case for taxes on sugared beverages. New Eng J Med. 2009<br />
Apr;360(18):1805-1808.<br />
41. Schwendicke F, Stolpe M. Taxing sugar-sweetened<br />
beverages: impact on overweight and obesity in Germany. BMC<br />
Public Health. <strong>2017</strong> Jan;17(1):88.<br />
42. Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria<br />
P, et al. Priority actions for the non-communicable disease crisis.<br />
Lancet. 20<strong>11</strong> Apr; 377(9775):1438-47.<br />
43. Sharma A, Hauck K, Hollingsworth B, Siciliani L. The effects<br />
of taxing sugar-sweetened beverages across different income<br />
groups. Health Econ. 2014 Sep;23(9):<strong>11</strong>59-<strong>11</strong>84.<br />
44. Falbe J, Thompson HR, Becker CM, Rojas N, McCulloch CE,<br />
Madsen KA. Impact of the Berkeley excise tax on sugar-sweetened<br />
beverage consumption. Am J Public Health. 2016 Oct;106(10):1865-<br />
71.<br />
45. Colchero MA, Guerrerro-López CM, Molina M, Rivera JA.<br />
Beverages sales in Mexico before and after implementation<br />
of a sugar sweetened beverage tax. PLoS One [Internet]. 2016<br />
Sep [cited <strong>2017</strong> July 6];<strong>11</strong>(9): e0163463. DOI: 10.1371/journal.<br />
pone.0163463.46.<br />
46. Bollard T, Maubach N, Walker N, Ni Mhurchu C. Effects of plain<br />
packaging, warning labels, and taxes on young people’s predicted<br />
sugar-sweetened beverage preferences: an experimental study. Int<br />
J Behav Nutr Phys Act. 2016 Sep;13(1):95.<br />
47. Bíró A. Did the junk food tax make the Hungarians eat<br />
healthier? Food Policy. 2015 July;54:107-<strong>11</strong>5.<br />
48. Obesity Policy Coalition and Global Obesity Centre. Tipping<br />
the Scales: Australian Obesity Prevention Consensus [Internet].<br />
<strong>2017</strong> [cited <strong>2017</strong> October 15]. Available from: http://www.opc.org.<br />
au/tipping-the-scales.aspx<br />
33
Drug Control in Australia: Where to next?<br />
[Review]<br />
Raquel Maggacis<br />
Raquel Maggacis is a final year medical student at the University of Queensland. She has<br />
a keen passion for public health endeavours and hopes to one day intertwine this with a<br />
career as a medical physician.<br />
Abstract<br />
Substance use and associated disorders are increasingly recognised as a global health issue. As attitudes towards drug<br />
use disorders evolve, varying drug control policies worldwide are called into question. Nations such as the United States<br />
of America utilise the criminal justice system to place sanctions on those contravening drug control policy, which often<br />
results in cycles of incarceration, further drug use, and poverty. In contrast, Portugal has revolutionised its approach to drug<br />
control since the turn of the century by decriminalising all drugs to great effect. In view of this wide spectrum of attitudes<br />
“towards drug control, the future of Australia’s approach to drug control policy is examined.<br />
”<br />
Introduction<br />
without aiming to reduce consumption.[1] Substance use<br />
disorders are perpetuated by social stigma and thus the<br />
political context is a key determinant of long-term health<br />
outcomes.[3]<br />
Benefits and detriments of different policy approaches<br />
The International Classification of Diseases defines<br />
substance use disorders as “continuing drug consumption<br />
despite severe adverse consequences”.[1] A report by<br />
the office of National Drug Control Policy in 2010 outlined<br />
the detriments of substance use disorders using a<br />
biopsychosocial paradigm (Figure 1).[1, 2]<br />
Substance use disorders are managed through three main<br />
drug policy approaches: decriminalisation, criminalisation,<br />
and harm minimisation. Decriminalisation involves prohibiting<br />
and regulating drugs but excluding sanctions from criminal<br />
law jurisdiction, whereas criminalisation is the attribution<br />
of criminal offences to drug-related activities.[3, 4] Harm<br />
minimisation strives to decrease adverse consequences<br />
Criminalisation of drugs, and the subsequent incarceration<br />
of drug users, provides the immediate benefit of removing the<br />
individual from an environment that exacerbates their drug<br />
use, and prevents the community from being threatened<br />
by drug-affected behaviour. Additionally, incarceration<br />
allows the government to demonstrate the work being<br />
done to tackle drugs in a manner that is tangible and easily<br />
understood by the general public. However, punitive drug law<br />
enforcement alone may fail to address or even worsen health<br />
Figure 1: The biopsychosocial adverse outcomes related to substance use disorders [1, 2]<br />
34
complications of drug use. It can marginalise populations at<br />
risk of poorer health and increase barriers to seeking health<br />
services, as illustrated by the growing epidemic of HIV/AIDS<br />
and hepatitis C amongst injecting drug users.[5] Moreover,<br />
drug law enforcement has minimal impact on the drug market<br />
itself, although there is some evidence that it may alleviate a<br />
degree of associated harm.[1, 6]<br />
Advantages of the harm minimisation approach include<br />
curbing the progression of the HIV/AIDs epidemic through<br />
safe needle programs and deterring criminal behaviours.[1,<br />
7] This is achieved through demand and supply reduction,<br />
prevention campaigns, and improved access to treatment<br />
and harm reduction.[8] Critiques of this approach include<br />
maintaining demand for the illicit drug market, and ineffectively<br />
addressing all biopsychosocial facets of substance use<br />
disorders.[8]<br />
“Decriminalisation addresses substance<br />
use disorders in a biopsychosocial context<br />
and identifies it as a key public health issue”<br />
The main benefit of decriminalisation is that it reframes<br />
drug use as a public health problem, which allows for<br />
reallocation of funds from drug-related criminal justice<br />
proceedings and the prison system to rehabilitation services<br />
focusing on long-term health outcomes.[3] This, coupled with<br />
a shift in criminal justice focus to high-level drug offenders,<br />
ultimately results in less drug use and better long-term<br />
health outcomes.[3] Decriminalisation addresses substance<br />
use disorders in a biopsychosocial context and identifies<br />
it as a key public health issue, both key steps in arresting<br />
the perpetuation of stigma which only serves to isolate drug<br />
users from health services.[3] Criticisms of decriminalisation<br />
include potential for increased accessibility to drugs and a<br />
cheaper street value, which could result in increased uptake<br />
of drug use.[9]<br />
In 2009, Antonio Costa, the executive director of the<br />
United Nations Office on Drugs and Crime, affirmed that<br />
“drug use should be treated as an illness in need of medical<br />
help”, and appealed for universal access to drug treatment.[2]<br />
In 20<strong>11</strong>, the Global Commission on Drug Policy emphasised<br />
that it was time to “end the criminalization, marginalization<br />
and stigmatization of people who use drugs but who do<br />
no harm to others”.[1] The World Health Organization and<br />
the United Nations echoed this view in their joint statement<br />
published in June <strong>2017</strong>, stating that to ignore such a call to<br />
“[review] and [repeal] punitive laws...[including] drug use or<br />
possession of drugs for personal use” would be to “[violate]<br />
the most fundamental human rights protected in international<br />
treaties and in national laws and constitutions”.[10] This<br />
strong stance against discrimination in health care settings<br />
reflects the global shift in attitudes towards drug policy, from<br />
incarceration to rehabilitation of drug offenders.<br />
Drug control approaches worldwide<br />
Criminalisation: the United States<br />
The United States (US) has a strong stance of<br />
criminalisation towards illicit drugs and has a low threshold<br />
to prosecute drug offenders.[3] Its prison population<br />
has increased by almost 800% since 1980, in marked<br />
disproportion to its population growth, with 47% of all<br />
inmates imprisoned for drug-related crimes, and many with<br />
drug use disorders.[3] In 2010 alone, US $80 billion was<br />
spent on continuing incarceration of inmates.[3] Drug users,<br />
possessors and traffickers are treated equally in this criminal<br />
system, with mandatory minimum prison sentences.[3]<br />
Without adequate rehabilitation services or emphasis on<br />
drug use and use disorders as a public health issue, the high<br />
rates of recidivism are unsurprising, often resulting in a cycle<br />
of criminality, incarceration and poverty, with subsequent<br />
economic burden on the community.[3] This is an issue fuelled<br />
by media sensationalism, portraying drug law enforcement in<br />
an enamouring light with dramatic drug busts and arrests,<br />
acting only to perpetuate fear within the general population.<br />
Where drug courts - legal committees which redirect nonviolent<br />
drug offenders from incarceration to treatment - have<br />
been trialled in the US, they have proven to decrease crime<br />
rates (7-14%) and recidivism (up to 35%), and improving<br />
rehabilitation uptake, treatment outcomes and stability of the<br />
family unit.[2] Such models are estimated to reduce health<br />
care costs related to substance use disorders by US $4 for<br />
every US $1 spent.[2]<br />
“This is an issue fuelled by media<br />
sensationalism, portraying drug law<br />
enforcement in an enamouring light with<br />
dramatic drug busts and arrests, acting<br />
only to perpetuate fear within the general<br />
population.”<br />
While marijuana is considered illicit under US federal law,<br />
states are able to make independent laws, which are only<br />
disregarded in cases concerning juveniles, cross-border<br />
trafficking, or organised crime.[9, <strong>11</strong>] Presently, over half of<br />
American states have legalised medicinal marijuana, and<br />
eight have further allowed recreational use.[9] Given the<br />
relatively recent legalisation of marijuana, data on its impact<br />
on usage patterns is currently conflicting, and more time is<br />
required for reliable assessment.[9] Studies have indicated<br />
that diversion of black market marijuana from legalised to<br />
criminalised states is likely to decrease marijuana prices,<br />
although the degree and impact of this is uncertain.[12, 13]<br />
Notably, there are significant economic benefits associated<br />
with the legalisation of marijuana.[9] In Colorado, where<br />
recreational marijuana use is legal, marijuana tax and<br />
licensing fees have been implemented, together generating<br />
over US $70 million in the first year alone.[9] This revenue was<br />
subsequently funnelled into school construction and youth<br />
35
and substance use programs).[9]<br />
Criminalisation: Central Asia<br />
Central Asian countries, such as Tajikistan, Kazakhstan,<br />
and Uzbekistan, have adopted an increasingly stringent<br />
approach to drugs.[14] In the year following the September<br />
<strong>11</strong> attacks, these countries received US $187.5 million<br />
from the US government to improve border control, counterterrorism<br />
measures and counter-narcotics initiatives.[14]<br />
Between 2004 and 2007, a strong criminal justice-based<br />
approach was further reinforced in Central Asia with funding<br />
from international agencies, other foreign governments and<br />
national budgets directed to legal action against drug use.<br />
[14]<br />
Further, national campaigns in Central Asia often label<br />
drug users as evil, increasing the stigma and discrimination<br />
which perpetuates cycles of drug use.[15] Little or no<br />
rehabilitation or treatment is available for substance users,<br />
with such countries preferring a model of criminalisation and<br />
incarceration.[14] For example, opioid substitution treatment<br />
is prohibited in Tajikistan and Turkmenistan, minimally<br />
available in Uzbekistan and Kyrgyzstan, and non-existent in<br />
Kazakhstan.[14] The lack of treatment for drug users and<br />
increasing accessibility of opiates has resulted in a growing<br />
HIV epidemic in Central Asian prison systems with poor longterm<br />
health outcomes.[14]<br />
Decriminalisation: Portugal<br />
Prior to 2001, drug use was criminalised in Portugal,<br />
yet rates of heroin use and drug trafficking continued to<br />
increase.[3] Consequently, the Portuguese government<br />
drafted a law decriminalising all drugs purchased, possessed<br />
or consumed for personal use. This law also had a public<br />
health focus towards rehabilitating those with substance<br />
use disorders, and a punitive focus towards high-level drug<br />
trafficking. This involves a committee of two medicallytrained<br />
persons and one legally-trained person, deciding first<br />
whether an offence is protected by this law, and then whether<br />
the offender is suffering from a drug use disorder.[3] This law<br />
only aimed to decriminalise low-level drug offences; strict<br />
laws remain against high-level offenders and drug traffickers<br />
who propagate this vicious cycle and endanger the general<br />
community.[16]<br />
After this law was passed,<br />
Portugal reduced its burden on the<br />
criminal-justice system, allowing<br />
more funding allocation towards<br />
public health endeavours, including<br />
prevention campaigns, treatment,<br />
and facilities.[17] Treatment<br />
uptake consequently increased,<br />
resulting in decreasing rates of drug-associated illnesses.[4,<br />
18] During the four years following decriminalisation in 2000<br />
to 2006, there was a significant decrease in the incidence<br />
of new cases of HIV/AIDS amongst drug users in Portugal,<br />
from almost 1400 to 400 persons.[18] Decreased rates of<br />
new hepatitis B and C infections have also been evident,<br />
attributed to the improved treatment and rehabilitation<br />
programs afforded by decriminalisation.[17, 18] Moreover,<br />
“...a staggering 400 Australians die yearly<br />
from heroin overdose, and most areas have<br />
a demand for substitution products far outweighing<br />
the supply”<br />
absolute numbers of drug-related deaths by each prohibited<br />
substance decreased; the total number of drug-related<br />
deaths decreased from 400 in 1999 to 290 in 2006.[18]<br />
Importantly, while some speculated that decriminalisation<br />
would lead to lower prices of drugs and subsequent<br />
higher rates of usage, the cost of drugs did not decrease.<br />
[19] In fact, the rates of cannabis and cocaine use after<br />
decriminalisation have been three times lower than before.<br />
[18] Further, data extrapolations have predicted lower lifetime<br />
prevalence rates of drug use for almost all drug categories<br />
post-decriminalisation.[18]<br />
Decriminalisation: West Africa<br />
West African countries must contend with both<br />
international drug cartels and the growing transit of illicit<br />
substances to Europe and North America. Consequently, local<br />
consumption of illicit substances has increased, especially<br />
among younger persons, with significant economic, health<br />
and social consequences.[20] While data is scarce, in 2008 it<br />
was estimated there were 1.8 million intravenous drug users<br />
in Sub-Saharan Africa, of whom 12% were thought to be living<br />
with HIV.[20, 21]<br />
In 2014, the West Africa Commission on Drugs published<br />
a declaration specifically stating that “criminalisation of drug<br />
use worsens health and social problems, puts huge pressures<br />
on the criminal justice system and incites corruption”, and<br />
that “drug use must be regarded primarily as a public health<br />
problem”, mirroring the movements of Portugal.[20] Despite<br />
these recommendations, there is currently no evidence<br />
that any West African countries have been successful in<br />
implementing drug decriminalisation policies.<br />
Drug policy in Australia and the way forward<br />
In 1985, the Australian Government adopted an official<br />
national drug policy of harm minimisation.[1] In the 2002-<br />
03 financial year, the Australian Government allocated $3.2<br />
billion to managing illicit drugs, 75% of which was spent on<br />
drug law enforcement, aiming to decrease drug and drugrelated<br />
crime, and improve public health and safety.[1,<br />
16] Despite this investment, a staggering 400 Australians<br />
die yearly from heroin overdose, and most areas have<br />
a demand for substitution products far out-weighing the<br />
supply, notwithstanding the costly<br />
co-payment.[1] The methadone<br />
substitution program and syringe<br />
exchange services available in<br />
Australia have made an impact, yet<br />
with a growing affected population<br />
and the root cause unaddressed,<br />
the need is largely unmet.[1]<br />
Harm minimisation still perpetuates discrimination and<br />
marginalisation of drug users, instead, decriminalisation can<br />
reduce stigma and is essential to better health outcomes.[3]<br />
The Australia21 report, published in 2012, was effective<br />
in initiating a debate on drug reform. The report not only<br />
illustrated the harmful effects of criminalising possession<br />
and personal use on drug-dependent individuals in an<br />
36
Australian context, but also highlighted the potential health<br />
benefits of some currently illicit drugs.[1, 8] This report left<br />
Australians to decide which legal system would allow for<br />
better biopsychosocial health and economic stability for<br />
the community with respect to those consuming drugs –<br />
rehabilitation or incarceration.<br />
Australia should act to follow countries like Portugal<br />
that have prospered from revolutionising drug policy with<br />
respect to low-level offences and reform to decriminalise<br />
all drugs. As supported by the Global Commission on Drug<br />
Policy, a move towards decriminalisation of low-level drug<br />
offenses in Australia would allow for decreased economic<br />
burden on the criminal justice system, reallocation of funds<br />
to drug rehabilitation programs, and a sharpened focus on<br />
the illegality of high-level drug trafficking offenses.[3] Viewing<br />
drug use as a public health problem is the key first step to<br />
reducing stigma and consequently improving access to<br />
treatment and long-term health outcomes.<br />
Conclusion<br />
Criminalisation marginalises those afflicted with drug use<br />
disorders, who are already burdened with significant health,<br />
social and economic disadvantage. Where there is demand,<br />
there is supply, and tackling drug use disorders with criminal<br />
law is simply too late to create a meaningful impact on the<br />
individual or society at large. Poverty breeds poverty; while<br />
incarceration may remove the immediate threat from society,<br />
it does nothing to address the root cause.<br />
Substance use disorders are a medical condition and<br />
public health problem, not a moral choice. Epitomised<br />
by Portugal, decriminalisation of drugs and rehabilitation<br />
fortifies a community, not just immediately, but with long-term<br />
positive effects in the workforce and crime rates, spanning<br />
generations. Substance use disorders, therefore, need to be<br />
reframed from a criminal, punitive problem, to one befitting<br />
the biopsychosocial model of health. Fortunately, throughout<br />
the world this is increasingly becoming the case.<br />
Acknowledgements<br />
Sophie Lim, <strong>Vector</strong> Associate Editor<br />
IDEAS Working Paper Series from RePEc. <strong>2017</strong>.<br />
5. Elliott R, Csete J, Palepu A, Kerr T. Reason and rights in global<br />
drug control policy. CMAJ. 2005;172(5):655-6.<br />
6. Mazerolle L, Soole DW, Rombouts S. Street-level drug law<br />
enforcement: A meta-analytical review. Journal of Experimental<br />
Criminology. 2006;2(4):409-35.<br />
7. Webster IW. Managing legal and medical complexities in<br />
caring for people with drug and alcohol problems: a call for change.<br />
Med J Aust. 2016;204(4):141-2.<br />
8. The prohibition of illicit drugs is killing and criminalising<br />
our children and we are all letting it happen. [press release].<br />
Canberra2012.<br />
9. Homel PB, Rick. Marijuana legalisation in the United States:<br />
An Australian perspective. Canberra: Australian Institute of<br />
Criminology; <strong>2017</strong> June <strong>2017</strong>.<br />
10. Joint United Nations statement on ending discrimination in<br />
health care settings [press release]. World Health Organisation<strong>2017</strong>.<br />
<strong>11</strong>. Adler J. Symposium Marijuana, Federal Power, and the States:<br />
Introduction. Case Western Reserve Law Review. 2015;65(3):505-<br />
12.<br />
12. Caulkins JP, Bond BM. Marijuana Price Gradients. Journal of<br />
Drug <strong>Issue</strong>s. 2012;42(1):28-45.<br />
13. Hall W, Weier M. Assessing the public health impacts of<br />
legalizing recreational cannabis use in the USA. Clin Pharmacol<br />
Ther. 2015;97(6):607-15.<br />
14. Latypov A. Understanding post 9/<strong>11</strong> drug control policy and<br />
politics in Central Asia. Int J Drug Policy. 2009;20(5):387-91.<br />
15. Wolfe D. Paradoxes in antiretroviral treatment for injecting<br />
drug users: access, adherence and structural barriers in Asia and<br />
the former Soviet Union. Int J Drug Policy. 2007;18(4):246-54.<br />
16. Willis K. Measuring the effectiveness of drug law enforcement.<br />
Trends and <strong>Issue</strong>s in Crime and Criminal Justice. 20<strong>11</strong>;406(1):1-7.<br />
17. Hughes CE, Stevens A. What Can We Learn From The<br />
Portuguese Decriminalization of Illicit Drugs? British Journal of<br />
Criminology. 2010;50(6):999-1022.<br />
18. Greenwald G. Drug Decriminalization in Portugal: Lessons for<br />
Creating Fair and Successful Drug Policies. Washington, DC: Cato<br />
Institute; 2009.<br />
19. Felix S, Portugal P. Drug decriminalization and the price of<br />
illicit drugs. Int J Drug Policy. <strong>2017</strong>;39:121-9.<br />
20. Drugs WACo. Not Just in Transit: Drugs, the State and Society<br />
in West Africa. West Africa Commission on Drugs; 2014.<br />
21. Mathers BMD, Louisa; Phillips, Benjamin; Wiessing, Lucas;<br />
Hickman, Matthew; Strathdee, Steffanie A; Wodak, Alex; Panda,<br />
Samiran; Tyndall, Mark; Toufik, Abdalla; Mattick, Richard P. Global<br />
epidemiology of injecting drug use and HIV among people who inject<br />
drugs: a systematic review. The Lancet. 2008;372(9651):1733-45.<br />
Conflict of Interest<br />
None declared<br />
Correspondance<br />
raquel.maggacis@uqconnect.edu.au<br />
References<br />
1. Wodak AD. The need and direction for drug law reform in<br />
Australia. The Medical Journal of Australia. 2012;197(6):312-3.<br />
2. Madras BK. Office of National Drug Control Policy: a scientist<br />
in drug policy in Washington, DC. Ann N Y Acad Sci. 2010;<strong>11</strong>87:370-<br />
402.<br />
3. Sapp CE. Rehabilitate or incarcerate? A comparative analysis<br />
of the United States’ sentencing laws on low-level drug offenders<br />
and Portugal’s decriminalization of low-level drug offenses. Cardozo<br />
Journal of International & Comparative Law. 2014;23(1):63-97.<br />
4. Félix S, Portugal P, Tavares A. Going after the Addiction, Not<br />
the Addicted: The Impact of Drug Decriminalization in Portugal.<br />
37
Dengue in the Pacific Islands<br />
[Review]<br />
Madeleine Marsland and Dunya Tomic<br />
Madeleine is a fourth year medical student who is interested in global health and research.<br />
She combines these interests in her role as Chief of Editorials and Publications<br />
for the Pacific Medical Students’ Association, and is also undertaking research with the<br />
Department of Anatomy and Developmental Biology at Monash University. She hopes<br />
to pursue global health research and policy.<br />
Dunya is a fourth year medical student at Monash University with a particular interest<br />
in clinical research and medical ethics. She hopes to one day combine this with a<br />
career as a physician.<br />
Abstract<br />
Without a fully effective vaccine, prophylactic measures, or sufficient treatment options, dengue has emerged as a significant<br />
global health threat. The Pacific Islands are particularly susceptible to dengue as they provide favourable conditions for<br />
the Aedes mosquito population, the vector responsible for spreading the virus. Strong public health protocols with an<br />
emphasis on vector control are considered to be the best way to combat dengue in this region. However, for a variety of<br />
social, economic, environmental and political factors, vector surveillance and control mechanisms are failing. This review<br />
seeks to provide an overview on the emergence of dengue in the Pacific Islands, why this region is susceptible due to virus<br />
“and vector factors, and what has been done and can be done in the future to contain the dengue threat in this region.<br />
Introduction<br />
Dengue virus is a vector-borne disease primarily<br />
spread by the Aedes mosquito population; it is one of the<br />
most significant infectious diseases that remains without<br />
definitive prevention or treatment options. Due to a variety<br />
of environmental and social factors, the Pacific Islands are<br />
particularly susceptible to dengue and other arbovirus.[1,<br />
2] This has significant associated morbidity, mortality and<br />
economic cost, particularly when patients contract ‘severe<br />
dengue’.[1-3] A diagnosis of dengue can be based on clinical<br />
signs and/or laboratory diagnosis, whilst a diagnosis of ‘severe<br />
dengue’ is based on serious complications including plasma<br />
leakage, severe haemorrhage or severe organ impairment.[3]<br />
These clinical manifestations and complications of dengue<br />
can cause severe illness, particularly in susceptible patient<br />
groups including children.[3]<br />
Treatment options are limited particularly in resource<br />
poor settings, and thus preventing dengue and recognising<br />
outbreaks is critical.[3] Dengvaxia, a world-first dengue<br />
vaccine, has recently been approved for use in endemic<br />
settings, with the World Health Organization recommending<br />
high-risk nations implement it as part of their vaccination<br />
program.[4-6] However, the vaccine has variable levels of<br />
efficacy, and is not yet considered a cost-effective solution.<br />
[5, 6] Whilst dengue remains a growing threat, the Pacific<br />
Island region must urgently develop alternative cost-effective<br />
diagnostic, detection, treatment and prevention strategies.[4,<br />
7, 8]<br />
Methods<br />
The intended focus of this literature review was dengue<br />
in the Pacific Island region. An Ovid MEDLINE search was<br />
conducted combining the search terms “Dengue”, “Aedes”<br />
and “Pacific”. Grey literature and data was also sourced from<br />
the World Health Organization (WHO) and other non-profit<br />
organisations. Additional resources were identified through<br />
analysing the articles retrieved through these searches.<br />
Epidemiology<br />
”<br />
Prevalence<br />
Dengue has been reported in several Pacific Island<br />
nations since the 1950s, but in the past decade the incidence<br />
has grown exponentially.[1, 9] Whilst in 2000 there was only<br />
50 reported cases per 1000 people, by 2012 this had grown<br />
to 350 per 1000.[1] It is difficult to determine reliable data<br />
on the endemic levels of dengue in the Pacific Islands, as<br />
this depends on accurate and timely reporting to the Pacific<br />
Public Health Surveillance Network, still under development.<br />
[2] However, whilst dengue is not endemic in all Pacific Islands,<br />
it is emerging in previously untouched islands including the<br />
Solomon Islands and Papua New Guinea.[9] From 2016 to<br />
<strong>2017</strong> alone, there has been an unusual increase in dengue<br />
38
Table 1: Dengue Serotypes and Epidemiology<br />
DENV Serotype Notable related epidemiology and outbreaks<br />
DENV-1<br />
The most prominent serotype in 2012-2013, causing the largest-ever documented<br />
outbreak affecting New Caledonia.[21]<br />
DENV-2 Caused recent outbreaks in Tuvalu and a current outbreak in Samoa.[10, 22]<br />
DENV-3<br />
After 18 years of absence, has recently become the dominant serotype in the<br />
Pacific islands causing five ongoing outbreaks [23].<br />
DENV-4 Caused one outbreak since 2012, is rare in the Pacific Islands [10].<br />
illness reported in the Solomon Islands, Vanuatu, Fiji and<br />
Palau.[10] With this growth, some reports indicate that the<br />
vast majority of the Pacific Island population will be infected<br />
at some point in their lives.[1] In Samoa, one study showed<br />
96% of the population tested positive for IgG antibodies,<br />
indicating prior infection.[<strong>11</strong>] With 89% of 18-25 year olds<br />
testing positive, this demonstrated that most Samoans first<br />
contracted dengue during childhood, when dengue illness is<br />
more likely to be fatal.[7, <strong>11</strong>]<br />
Outbreaks<br />
Dengue typically follows an epidemic pattern with 1 of<br />
the 4 serotypes causing outbreaks across the Pacific every<br />
three to five years. However, the number of outbreaks of<br />
concurrent serotypes has been growing.[2] After an outbreak<br />
of a single serotype, this strain of the virus tends to circulate<br />
throughout the region until the next outbreak of a different<br />
strain occurs.[12] A single outbreak can affect a large portion<br />
of the population, with the 2009 outbreaks affecting 14<br />
Pacific nations.[13] During such outbreaks, complications<br />
increase, placing a burden on hospital resources, with 4%<br />
of the Federated States of Micronesia’s population requiring<br />
hospitalisation during the Kosrae state outbreak.[14] The<br />
frequency of outbreaks appears to be increasing,[4] though<br />
this may be due to improved surveillance.<br />
The virus<br />
Dengue virus (DENV) is a single-stranded, positivesense<br />
RNA virus of the Flavivirus genus.[15] There are<br />
four serotypes DENV-1 to DENV-4. Though they only share<br />
65% of their genomes, their clinical syndromes are nearly<br />
identical, and they all occupy the same ecological niche.<br />
[16, 17] Dengue epidemics usually result from introduction of<br />
a single serotype from hyper-endemic countries, which will<br />
remain dominant in the region for several years.[12,18,19]<br />
However, in 2012, outbreaks of all four DENV serotypes were<br />
noted in a single year [20]. Each DENV serotype has caused<br />
outbreaks or been prevalent in the Pacific Islands at various<br />
times (Table 1).<br />
Repeated infection of DENV of the same serotype is<br />
associated with increase risk of progressing to severe<br />
dengue, which is associated with higher morbidity and<br />
mortality if left untreated.[24] Those living in endemic areas<br />
such as the Pacific Islands are at an increased risk of being<br />
reinfected and thus complications are more common.<br />
The <strong>Vector</strong><br />
Dengue, zika, chikungunya and other arboviruses are<br />
transmitted to humans through the bites of infected Aedes<br />
mosquitoes.[25] Aedes aegypti is the primary vector in the<br />
Pacific Islands and is widespread across the region except<br />
for Futuna and other isolated islands.[26,27] Aedes aegypti is<br />
associated with human migration and urbanisation, enabling<br />
it to be dominant in the region, however, Aedes albopictus,<br />
Aedes polynesiensis and nine other potential vectors have<br />
also been identified in the Pacific Islands.[27, 28]<br />
Aedes mosquitoes begin their transmission cycle upon<br />
acquiring the dengue virus from the blood of a viraemic<br />
person; the virus then replicates in mosquito midgut<br />
epithelium before shedding its progeny into the haemocoel,<br />
which then disseminates into secondary target tissues such<br />
as salivary glands.[29] During the next feeding event, the<br />
mosquito transmits the virus to the host through saliva.[29,30]<br />
Aedes aegypti is capable of repeatedly transmitting the virus<br />
through this process irrespective of its number of hosts.[30]<br />
The introduction of Aedes aegypti into different islands has<br />
been spurred by human migration; there have been intense<br />
population migrations in the Pacific Islands since European<br />
colonization.[31] Though the first dengue epidemic in the<br />
Pacific Islands was reported in the 1880s, descriptions of<br />
Aedes aegypti didn’t emerge until the 1960s in Fiji and Tonga.<br />
[20, 32, 33] Aedes aegypti then spread during World War II,<br />
when travel between the Pacific Islands and Asia, Europe,<br />
and America became more frequent.[34] Recent studies<br />
have now identified genetic variability in nine locations<br />
across Fiji, New Caledonia, Tonga and French Polynesia,<br />
suggesting a link between human migration and Aedes<br />
aegypti populations, possibly related to island isolation and<br />
environmental conditions.[25]<br />
Several factors influence the transmission of DENV<br />
from mosquitoes to humans, including climate.[30] Higher<br />
temperatures enable the virus to replicate in higher<br />
concentrations, enhancing the vectors’ risk for pathogen<br />
transmission and contributing to the high prevalence of<br />
dengue infection in the tropical Pacific Islands[30] Globally,<br />
climate-induced variations in modelled Aedes aegypti<br />
populations were strongly correlated to historical dengue<br />
cases between 1958 to 1995.[35] Recent research from New<br />
Caledonia, where dengue spread by Aedes aegypti is a major<br />
39
public health problem, showed that the epidemic dynamics of<br />
dengue were predominantly driven by climate in the last forty<br />
years.[36] Another study found a positive correlation between<br />
dengue infection and El Nino southern oscillation in ten<br />
countries, with evidence of infection spreading from larger<br />
islands to smaller surrounding islands.[37] It is predicted that<br />
global warming will increase the latitudinal and altitudinal<br />
distribution of Aedes aegypti and subsequently DENV.[38,39]<br />
Dengue Surveillance Methods<br />
Dengue surveillance and tracking is essential to enable<br />
timely epidemic responses.[8] Though representatives from<br />
the Pacific Islands believe there is adequate surveillance<br />
infrastructure and systems, governments have not<br />
emphasised prevention. These systems must be strengthened<br />
to more accurately track dengue epidemiological data [8, 40].<br />
Given financial difficulties, this may be better accomplished<br />
through alternative mechanisms.<br />
One such alternative is the transport of serum and blood<br />
samples internationally.[41] When a new serotype emerges<br />
in one Pacific country, this is often followed by outbreaks in<br />
neighbouring countries [42]; using blood samples to identify<br />
emerging serotypes enables surveillance of viral spread<br />
across the region. Filter paper (FP)-dried blood spots have<br />
minimal health risk and so are not bound by dangerous<br />
goods regulations present in several Pacific nations [43].<br />
Blood spiked with cultured DENV can be blotted on FP-cards<br />
and the serotype determined using reverse-transcriptase<br />
polymerase chain reaction.[44]. The serotype and genotype<br />
of DENV can be identified using FP-dried serum even after<br />
being transported over thousands of kilometres at tropical<br />
temperatures.[41] This method of surveillance particularly<br />
useful in the Pacific Islands, where samples may need to be<br />
transported over long distances.<br />
Another method to monitor dengue levels is the use of<br />
international travellers as ‘sentinels’, so that the risk of dengue<br />
infection can be estimated through proxies who travelled to<br />
particular areas.[45] Patterns of local dengue incidence in<br />
the Pacific Islands were shown to be closely correlated with<br />
patterns of dengue incidence imported from the Pacific to<br />
New Zealand.[46] However, this method is more commonly<br />
retrospective and cannot provide an indication of outbreaks.<br />
A combination of both methods could be implemented to<br />
cheaply and effectively improve dengue surveillance in the<br />
regions.<br />
Dengue Prevention and Control, Now and in the Future<br />
Strategies and Policies<br />
Many nations have been attempting to meet the<br />
WHO infectious disease strategy objectives (Figure 1) by<br />
implementing policies that address vector surveillance,<br />
health education for vector control and dengue prevention,<br />
and emergency response capacity.[8] However, an urgent<br />
policy review to combat dengue is needed, with a focus on<br />
emphasising dengue in climate change and environmental<br />
medicine policies.[48] It is also essential that dengue is<br />
classed as a notifiable disease across all Pacific Islands<br />
through legislation.[48]<br />
A Dengue Vaccine<br />
Although several live-attenuated dengue vaccines are<br />
undergoing phase III clinical trials, currently Dengvaxia (CYD-<br />
TDV) is the only vaccine that is licensed and registered for use<br />
in individuals aged 9-45 years and living in dengue endemic<br />
areas.[40] Modelling has shown that Dengvaxia would only<br />
have the highest net benefit and be most cost-effective if the<br />
majority of the population is vaccinated in dengue-endemic<br />
nations.[52] The WHO has recommended that nations with<br />
a high burden of disease, defined as seroprevalence >70%<br />
in 9 year-olds, introduce the vaccine.[4, 1] However, many<br />
nations worldwide are still debating this, and Dengvaxia is not<br />
currently licensed for use in Pacific Island nations.[5, 51]<br />
From the two major phase III clinical trials for Dengvaxia,<br />
overall vaccine efficacy against severe dengue was 79%,<br />
however, this varied by serotype, age at vaccination, and<br />
previous dengue infection.[52] For those with a previous<br />
dengue infection, vaccination efficacy was 78%, however, it<br />
was only 38% for those with no prior infection.[52] In fact, a<br />
study has shown that Dengvaxia can also increase the risk of<br />
hospitalisation when seronegative individuals are vaccinated<br />
and later experience natural secondary dengue infection.<br />
[51] The pooled efficacy for those older than 9 years old was<br />
higher than those under 9 years of age, who have a higher<br />
risk of severe dengue (66% vs 44%).[3, 52] Finally, in terms<br />
of serotype, vaccine efficacy was shown to be higher against<br />
Figure 1: Outline of the World Health Organization Infectious Disease Strategy [47]<br />
40
serotypes 3 (72%) and 4 (77%) than for serotypes 1 (55%)<br />
and 2 (43%).[52]<br />
Further study is ongoing to determine whether dengue<br />
illness and hospitalisation has reduced in nations that have<br />
implemented Dengvaxia.[53, 54] However, with varying<br />
efficacy, and questions regarding long-term safety and<br />
cost-effectiveness, it is predicted that vaccination will only<br />
be possible in the Pacific Islands if it is priced competitively.<br />
[53, 54] Thus, for the time being, vector control will remain the<br />
focus of dengue control strategy in the Pacific Islands, with<br />
the aim of integrating vaccination once it is more efficacious<br />
and cost-effective.[55] At present, it is far more affordable<br />
and effective to combat dengue by improving vector control<br />
mechanisms, and vaccination will be most useful as an<br />
adjunct if appropriate for specific nations.<br />
<strong>Vector</strong> Control: Currently Used Methods<br />
<strong>Vector</strong> control currently offers the best option for<br />
preventing dengue, but delivery of prevention programmes<br />
in the Pacific Islands is often inefficient, ineffective or both.<br />
[7] Several mechanisms exist in various Pacific Islands to<br />
control outbreaks once they occur, however some of the<br />
most common efforts, such as pesticide spraying, have<br />
limited effectiveness.[56]<br />
Factors that increase the risk of dengue transmission have<br />
included poor household drainage and hygiene problems,<br />
issues that can be addressed by health education programs<br />
to build a ‘prevention attitude’ among Pacific residents.[57,<br />
58] However, it is believed that improving health education,<br />
awareness campaigns and technical support is necessary<br />
to ensure successful vector control.[8] Environmental factors<br />
such as buckets of stagnant water, allowing mosquitoes to<br />
breed, and host larvae and pupae, are other key risk factor<br />
which could be targeted through education campaigns.<br />
[59] Chemical treatment of breeding sites, insecticide<br />
spraying and biological control by introducing predators are<br />
mechanisms already utilised by some Pacific Islands which<br />
could be further implemented for vector control in the future.<br />
[60]<br />
<strong>Vector</strong> Control: Innovative Approaches<br />
Novel vector-based approaches aimed at controlling<br />
dengue include the use of obligate intracellular bacterium<br />
Wolbachia pipientis,[61] which interferes with reproduction in<br />
over 40% of insect species.[62] Although Wolbachia does not<br />
occur naturally in Aedes aegypti species, transinfection has<br />
been shown to be successful.[63] Recent studies in Cairns,<br />
Australia have shown stable transinfection of natural A.<br />
aegypti populations with the wMel strain of Wolbachia, rising<br />
to near-fixation within a matter of months and remaining<br />
established in those field sites unaided.[64] The antiviral<br />
activity of wMel has shown to be highly effective in laboratory<br />
studies even one year after field release.[65] The evidence<br />
supports the long-term stability of Wolbachia against the<br />
dengue virus, however, the effects on reduction of human<br />
disease in dengue-endemic regions is yet to be established,<br />
this is currently under investigation in Indonesia and Vietnam.<br />
[61]<br />
Another promising vector control method is the sterile<br />
insect technique (SIT), which has historically been successful<br />
against a multitude of agricultural pests.[66] In the 1960s,<br />
large-scale SIT programs enabled the elimination of A.<br />
aegypti from 23 American countries.[67] SIT has recently<br />
re-emerged as a vector control strategy due to innovative<br />
technological advances including genetic modification<br />
of mosquitoes.[68] Using SIT, Cuba has come close to the<br />
eradication of A. aegypti [69] and Singapore has kept levels<br />
of the mosquitoes down for more than 30 years.[70] Though<br />
neither of these methods is currently used widely in Pacific<br />
Islands, these innovative strategies are potential costeffective<br />
vector reduction methods.<br />
Emergency Response Capacity<br />
There is a significant need to grow emergency-response<br />
and outbreak-response to combat dengue.[8] Currently, the<br />
WHO and Red Cross manage the majority of outbreak control,<br />
both logistically and financially[14, 71] The Pacific Public<br />
Health Surveillance Network has provided some support in<br />
capacity building, and multiagency response teams have<br />
successfully been implemented during some outbreaks,<br />
but there remains a need to engage Pacific Directors and<br />
Ministers of Health to help prepare these multidisciplinary<br />
response teams for future outbreaks.[2, 14]<br />
Conclusion<br />
Dengue remains a significant threat in the Pacific Islands,<br />
with prevalence levels and the number of outbreaks continuing<br />
to increase. Until Dengvaxia or another dengue vaccine has<br />
a proven cost-effective public health benefit beyond the<br />
currently calculated values, it is unlikely to be deployed in<br />
Pacific Islands.[5, 51] The best hope for containing dengue<br />
is by improving region-wide surveillance and cost-effective,<br />
sustainable vector control mechanisms [6-8]. This requires<br />
Pacific Island governments to integrate dengue prevention<br />
into their environmental and public health policy, and work to<br />
improve vector surveillance and control methods, which may<br />
involve implementing innovative approaches [8, 48]. Another<br />
area that requires significant improvement is outbreak<br />
response, and upskilling all Pacific doctors to appropriately<br />
respond to dengue outbreaks [8, 60]. Ultimately, until the<br />
objectives outlined by the WHO are addressed, dengue<br />
will remain a growing challenge in the Pacific Islands.<br />
[7, 47] These islands must engage with the growing body<br />
of organisations working in the region to develop new and<br />
innovative surveillance and control approaches and combat<br />
dengue in the future.[7]<br />
Conflicts of interest<br />
None declared<br />
Correspondance<br />
dtom4@student.monash.edu<br />
References<br />
1. Arima Y, Chiew M, Matsui T. Epidemiological update on the<br />
dengue situation in the Western Pacific Region, 2012. Western<br />
Pacific Surveillance and Response Journal. 2015;6(2):82-89.<br />
2. Roth A, Mercier A, Lepers C, Hoy D, Duituturaga S, Benyon E<br />
41
et al. Concurrent outbreaks of dengue, chikungunya and Zika virus<br />
infections – an unprecedented epidemic wave of mosquito-borne<br />
viruses in the Pacific 2012–2014. Eurosurveillance. 2014;19(41):1<br />
- 8.<br />
3. Dengue Guidelines for Diagnosis, Treatment, Prevention and<br />
Control [Internet]. World Health Organization (WHO) and the Special<br />
Programme for Research and Training in Tropical Diseases (TDR);<br />
2009 [cited 27 July <strong>2017</strong>]. Available from: http://www.who.int/tdr/<br />
publications/documents/dengue-diagnosis.pdf<br />
4. Dengue and Severe Dengue [Internet]. World Health<br />
Organization. <strong>2017</strong> [cited <strong>11</strong> August <strong>2017</strong>]. Available from: http://<br />
www.who.int/mediacentre/factsheets/fs<strong>11</strong>7/en/<br />
5. Wilder-Smith A, Vannice KS, Hombach J, Farrar J, Nolan<br />
T. Population Perspectives and World Health Organization<br />
Recommendations for CYD-TDV Dengue Vaccine. J Infect Dis.<br />
2016;214(12):1796-1799.<br />
6. Olivera-Botello G, Coudeville L, Fanouillere K, Guy B,<br />
Chambonneau L, Noriega F et al. Tetravalent Dengue Vaccine<br />
Reduces Symptomatic and Asymptomatic Dengue Virus Infections<br />
in Healthy Children and Adolescents Aged 2-16 Years in Asia and<br />
Latin America. J Infect Dis. 2016;214(7):994-1000.<br />
7. Guzman M, Halstead S, Artsob H, Buchy P, Farrar J, Gubler D et<br />
al. Dengue: a continuing global threat. Nature Reviews Microbiology.<br />
2010;8(12):S7-S16.<br />
8. Tambo E, Chen J, Zhou X, Khater E. Outwitting dengue threat<br />
and epidemics resurgence in Asia-Pacific countries: strengthening<br />
integrated dengue surveillance, monitoring and response systems.<br />
Infectious Diseases of Poverty. 2016;5(1).<br />
9. Kline K, McCarthy J, Pearson M, Loukas A, Hotez P. Neglected<br />
Tropical Diseases of Oceania: Review of Their Prevalence,<br />
Distribution, and Opportunities for Control. PLoS Neglected Tropical<br />
Diseases. 2013;7(1):1 - 6.<br />
10. Pacific: Dengue Outbreak – Oct 2016 [Internet]. Disasters.<br />
ReliefWeb. <strong>2017</strong> [cited <strong>11</strong> August <strong>2017</strong>]. Available from: http://<br />
reliefweb.int/disaster/ep-2016-000<strong>11</strong>2-slb<br />
<strong>11</strong>. Duncombe J, Lau C, Weinstein P, Aaskov J, Rourke M, Grant<br />
R et al. Seroprevalence of Dengue in American Samoa, 2010.<br />
Emerging Infectious Diseases. 2013;19(2):324-326.<br />
12. Dupont-Rouzeyrol M, Aubry M, O’Connor O, Roche C, Gourinat<br />
A, Guigon A et al. Epidemiological and molecular features of dengue<br />
virus type-1 in New Caledonia, South Pacific, 2001–2013. Virology<br />
Journal. 2014;<strong>11</strong>(1):61.<br />
13. Dengue in the Western Pacific Region [Internet]. World Health<br />
Organization Western Pacific Region. <strong>2017</strong> [cited 26 February<br />
<strong>2017</strong>]. Available from: http://www.wpro.who.int/emerging_diseases/<br />
Dengue/en/<br />
14. Taulung L, Masao C, Palik H, Samo M, Barrow L, Pretrick M<br />
et al. Dengue Outbreak — Federated States of Micronesia, 2012–<br />
2013 [Internet]. Morbidity and Mortality Weekly Report. 2013 [cited<br />
26 February <strong>2017</strong>]. Available from: https://www.cdc.gov/mmwr/<br />
preview/mmwrhtml/mm6228a3.htm<br />
15. Dupont-Rouzeyrol M, Aubry M, O’Connor O, Roche C,<br />
Gourinat AC, Guigon A et al. Epidemiological and molecular features<br />
of dengue virus type-1 in New Caledonia, South Pacific, 2001-2013.<br />
Virol J. 2014;<strong>11</strong>:61.<br />
16. Sabin AB. Research on dengue during World War II. Am J Trop<br />
Med Hyg. 1952;1:30–50.<br />
17. Halstead SB. Dengue virus – mosquito interactions. Annu Rev<br />
Entomol. 2008;53:273-91.<br />
18. A-Nuegoonpipat A, Berlioz-Arthaud A, Chow V, Endy T, Lowry<br />
K, le Mai Q et al. Sustained transmission of dengue virus type 1 in<br />
the Pacific due to repeated introductions of different Asian strains.<br />
Virology. 2004;329(2):505-12.<br />
19. Morens DM. Dengue fever: a prevention summary for Pacific<br />
health workers. Pacific Health Dialog. 1996;3(1):240-52.<br />
20. Singh N, Kiedrzynski T, Lepers C, Benyon EK. Dengue in the<br />
Pacific – an update of the current situation. Pacific Health Dialog.<br />
2005;12(2):<strong>11</strong>1-9.<br />
21. Roth A, Mercier A, Lepers C, Hoy D, Duituturaga S, Benyon E<br />
et al. Concurrent outbreaks of dengue, chikungunya and Zika virus<br />
infections - an unprecedented epidemic wave of mosquito-borne<br />
viruses in the Pacific 2012-2014. Euro Surveill. 2014;19(41):20929.<br />
22. Centers for Disease Control and Prevention (CDC). Dengue<br />
outbreak – Federated States of Micronesia, 2012-2013. MMWR.<br />
Morbidity and mortality weekly report. 2013;62(28):570-3.<br />
23. Cao-Lormeau VM, Roche C, Musso D, Mallet HP, Dalipanda<br />
T, Dofai A, et al. Dengue virus type 3, South Pacific Islands, 2013.<br />
Emerg Infect Dis. 2014;20(6):1034-6.<br />
24. World Health Organization. Dengue haemorrhagic fever.<br />
Diagnosis, Treatment, Prevention and Control. Geneva (CH); 1997.<br />
92 p. Report No.: 2.<br />
25. Calvez E, Guillaumot L, Millet L, Marie J, Bossin H, Rama V et<br />
al. and Phylogeny of Aedes aegypti, the Main Arbovirus <strong>Vector</strong> in the<br />
Pacific. PLoS Negl Trop Dis. 2016;10(1):1-2.<br />
26. Guillaumot L. Arboviruses and their vectors in the Pacific –<br />
status report. Pac Health Dialog. 2005;12(2):45-52.<br />
27. Lounibos LP. Invasions by insect vectors of human disease.<br />
Annu Rev Entomol. 2002;47(1):233-66.<br />
28. Paupy C, Vazeille-Falcoz M, Mousson L, Rodhain F, Failloux<br />
AB. Aedes aegypti in Tahiti and Moorea (French Polynesia):<br />
isoenzyme differentiation in the mosquito population according to<br />
human population density. Am J Trop Med Hyg. 2000;62(2):217-24.<br />
29. Carrington LB, Simmons CP. Human to Mosquito Transmission<br />
of Dengue Viruses. Front Immunol. 2014;5:290.<br />
30. Scott T, Takken W. Feeding strategies of anthropophilic<br />
mosquitoes result in increased risk of pathogen transmission.<br />
Trends Parasitol. 2012;28(3):<strong>11</strong>4-121.<br />
31. Rallu JL. Tendance recentes des migrations dans le Pacifique<br />
Sud. Espace, population, sociétés. 1994;12(2):201-212.<br />
32. Perry WJ. The mosquitoes and mosquito-borne diseases on<br />
New Caledonia, an historic account; 1885–1946. Am J Trop Med<br />
Hyg. 1950;30(1):103-14.<br />
33. Chow CY. Aedes aegypti in the Western Pacific Region. Bull<br />
World Health Organ. 1967;36(4):544-6.<br />
34. Kuno G. Research on dengue and dengue-like illness in East<br />
Asia and the Western Pacific during the First Half of the 20th century.<br />
Rev Med Virol. 2007;17(5):327-41.<br />
35. Hopp MJ, Foley JA. Worldwide fluctuations in dengue fever<br />
cases related to climate variability. Clim Res. 2003;25:85-94.<br />
36. Descloux E, Mangeas M, Menkes CE, Lengaigne M,<br />
Leroy A, Tehei T et al. Climate-Based Models for Understanding<br />
and Forecasting Dengue Epidemics. PLoS Negl Trop Dis.<br />
2012;6(2):e1470.<br />
37. Hales S, Weinstein P, Souares Y, Woodward A. El Nino and<br />
the Dynamics of <strong>Vector</strong>borne Disease Transmission. Environ Health<br />
Perspect. 1999;107(2):99-102.<br />
38. Hales S, de Wet N, Maindonald J, Woodward A. Potential<br />
effect of population and climate changes on global distribution of<br />
dengue fever: an empirical model. Lancet. 2002;360:830-834.<br />
39. Jetten TH, Focks DA. Potential changes in the distribution of<br />
dengue transmission under climate warming. Am J Trop Med Hyg.<br />
1997;57:285-297.<br />
40. Masahiro U, Sengebau-Kinzio M, Nakamura K, Ridep E,<br />
Watanabe M, Takano T. Household risk factors associated with<br />
dengue-like illness, Republic of Palau, 2000-2001. BioScience<br />
Trends. 2007;1(1):33 - 37.<br />
41. Aubry M, Roche C, Dupont-Rouzeyrol M, Aaskov J, Viallon<br />
J, Marfel M et al. Use of serum and blood samples on filter paper<br />
to improve the surveillance of dengue in Pacific Island Countries.<br />
Journal of Clinical Virology. 2012;55(1):23-29.<br />
42. Cao-Lormeau VM, Roche C, Descloux E, Viallon J, Lastere<br />
S, Wiegandt A et al. Lost in French Polynesia: which strategies for a<br />
dengue virus to spread? Am J Trop Med Hyg Suppl. 2007;12:<strong>11</strong>1-19.<br />
43. Guidance on regulations for the transport of infectious<br />
substances 20<strong>11</strong>–2012 [Internet]. World Health Organization; 2010<br />
[cited 31 July <strong>2017</strong>]. Available from: http://www.who.int/entity/ihr/<br />
42
publications/who_hse_ihr_20100801/en/index.html<br />
44. Prado I, Rosario D, Bernardo L, Alvarez M, Rodriguez R,<br />
Vasquez S et al. PCR detection of dengue virus using dried whole<br />
blood spotted on filter paper. J Virol Methods. 2005;125:75-81.<br />
45. Fukusumi M, Arashiro T, Arima Y, Matsui T, Shimada T,<br />
Kinoshita H et al. Dengue Sentinel Traveler Surveillance: Monthly<br />
and Yearly Notification Trends among Japanese Travelers, 2006–<br />
2014. PLOS Neglected Tropical Diseases. 2016;10(8):1 - 14.<br />
46. Lau CL, Weinstein P, Slaney D. Dengue surveillance by proxy:<br />
travellers as sentinels for outbreaks in the Pacific Islands. Epidemiol<br />
Infect. 2013 Nov;141(<strong>11</strong>): 2328–34.<br />
47. Strategy [Internet]. Emerging Disease Surveillance and<br />
Response. <strong>2017</strong> [cited 26 February <strong>2017</strong>]. Available from: http://<br />
www.wpro.who.int/emerging_diseases/strategy/Strategy/en/<br />
48. Beatty M, Stone A, Fitzsimons D, Hanna J, Lam S, Vong S et<br />
al. Best Practices in Dengue Surveillance: A Report from the Asia-<br />
Pacific and Americas Dengue Prevention Boards. PLoS Neglected<br />
Tropical Diseases. 2010;4(<strong>11</strong>):e890.<br />
49. Malavige GN, Fernando S, Fernando DJ, Seneviratne SL.<br />
Dengue viral infections. Postgrad Med J. 2004;80(948):588-601.<br />
50. Rodriguez T. Dengvaxia Most Effective in High-Transmission<br />
Areas [Internet]. Infectious Disease Advisor. 2016 [cited 3 April<br />
<strong>2017</strong>]. Available from: http://www.infectiousdiseaseadvisor.com/<br />
vector-borne-illnesses/dengvaxia-effective-in-high-transmissionareas/article/579948/<br />
51. Aguiar M, Stollenwerk N, Halstead S. The Impact of the Newly<br />
Licensed Dengue Vaccine in Endemic Countries. PLOS Neglected<br />
Tropical Diseases. 2016;10(12):e0005179.<br />
52. Questions and Answers on Dengue Vaccines [Internet].<br />
Immunization, Vaccines and Biologicals. World Health Organization.<br />
<strong>2017</strong> [cited <strong>11</strong> August <strong>2017</strong>]. Available from: http://www.who.int/<br />
immunization/research/development/dengue_q_and_a/en<br />
53. Hadinegoro S, Arredondo-García J, Capeding M, Deseda<br />
C, Chotpitayasunondh T, Dietze R et al. Efficacy and Long-Term<br />
Safety of a Dengue Vaccine in Regions of Endemic Disease.<br />
New England Journal of Medicine [Internet]. 2015 [cited 3 April<br />
<strong>2017</strong>];373(13):<strong>11</strong>95-1206. Available from: http://www.nejm.org/doi/<br />
full/10.1056/NEJMoa1506223#t=article<br />
54. Flasche S, Jit M, Rodríguez-Barraquer I, Coudeville L, Recker<br />
M, Koelle K et al. The Long-Term Safety, Public Health Impact, and<br />
Cost-Effectiveness of Routine Vaccination with a Recombinant,<br />
Live-Attenuated Dengue Vaccine (Dengvaxia): A Model Comparison<br />
Study. PLOS Medicine. 2016;13(<strong>11</strong>):e1002181.<br />
55. Background Paper on Dengue Vaccines [Internet]. 1st ed.<br />
SAGE Working Group on Dengue Vaccines and WHO Secretariat;<br />
2016 [cited 3 April <strong>2017</strong>]. Available from: http://www.who.int/<br />
immunization/sage/meetings/2016/april/1_Background_Paper_<br />
Dengue_Vaccines_2016_03_17.pdf<br />
56. Masahiro U, Sengebau-Kinzio M, Nakamura K, Ridep E,<br />
Watanabe M, Takano T. Household risk factors associated with<br />
dengue-like illness, Republic of Palau, 2000-2001. BioScience<br />
Trends. 2007;1(1):33 - 37.<br />
57. Noel M. Dengue fever larval control in New Caledonia:<br />
assessment of a door-to-door health educators program. Pacific<br />
Health Surveillance and Response. 2005;12(2):39 - 44.<br />
58. Morrow GBowen K. Accounting for health in climate change<br />
policies: a case study of Fiji. Global Health Action. 2014;7(1):23550.<br />
59. Burkot T, Handzel T, Schmaedick M, Tufa J, Roberts J,<br />
Graves P. Productivity of natural and artificial containers for Aedes<br />
polynesiensis and Aedes aegypti in four American Samoan villages.<br />
Medical and Veterinary Entomology. 2007;21(1):22-29.<br />
60. Chang M, Christophel E, Gopinath D, Abdur R. Challenges and<br />
future perspective for dengue vector control in the Western Pacific<br />
Region. Western Pacific Surveillance and Response. 20<strong>11</strong>;2(2):1 - 7.<br />
61. McGraw EA, O’Neill SL. Beyond insecticides: new thinking on<br />
an ancient problem. Nat Rev Microbiol. 2013 Mar;<strong>11</strong>(3):181-93.<br />
62. Zug R, Koehncke A, Hammerstein P. Epidemiology in<br />
evolutionary time: the case of Wolbachia horizontal transmission<br />
between arthropod host species. J Evol Biol. 2012 Nov;25(<strong>11</strong>):2149-<br />
60.<br />
63. Xi Z, Khoo CC, Dobson SL. Wolbachia establishment and<br />
invasion in an Aedes aegypti laboratory population. Science. 2005<br />
Oct;310(5746):326-8.<br />
64. Walker T, Johnson PH, Moreira LA, Iturbe-Ormaetxe I, Frentiu<br />
FD, McMeniman CJ, et al. The wMel Wolbachia strain blocks dengue<br />
and invades caged Aedes aegypti populations. Nature. 20<strong>11</strong><br />
Aug;476:450-3.<br />
65. Frentiu FD, Zakir T, Walker T, Popovici J, Pyke AT, van der<br />
Hurk A, et al. Limited Dengue Virus Replication in Field-Collected<br />
Aedes aegypti Mosquitoes Infected with Wolbachia. PLoS Negl Trop<br />
Dis. 2014 Feb;8(2):e2688.<br />
66. Dyck VA, Hendrichs J, Robinson AS, editors. Sterile Insect<br />
Technique: Principles and Practice in Area-Wide Integrated Pest<br />
Management. Dordrecht: Springer; 2005. 787 p.<br />
67. Soper FL. The elimination of urban yellow fever in the<br />
Americas through the eradication of Aedes aegypti. Am J Public<br />
Health Nations Health. 1963 Jan;53(1):7-16.<br />
68. Phuc HK, Andreasen MH, Burton RS, Vass C, Epton MJ, Pape<br />
G, et al. Late-acting dominant lethal genetic systems and mosquito<br />
control. BMC Biol. 2007 Mar;5:<strong>11</strong>.<br />
69. Kourí G, Guzmán MG, Bravo J. Hemorrhagic dengue in Cuba:<br />
history of an epidemic. Bull Pan Am Health Organ. 1986;20(1):24-30.<br />
70. Ooi EE, Goh KT, Gubler DJ. Dengue prevention and 35 years<br />
of vector control in Singapore. Emerg Infect Dis. 2006 Jun;12(6):887-<br />
93.<br />
71. Disaster relief and emergency fund enables dengue outbreak<br />
response [Internet]. Fédération internationale des Sociétés de la<br />
Croix-Rouge. 2014 [cited 26 February <strong>2017</strong>]. Available from: http://<br />
www.ifrc.org/fr/nouvelles/nouvelles/common/disaster-relief-andemergency-fund-enables-dengue-outbreak-response-65371/<br />
43
Family, Unity and Success - Australian<br />
Indigenous Doctors’ Association (AIDA) <strong>2017</strong><br />
[Conference report]<br />
Narawi Foley Boscott<br />
Narawi completed a Bachelor of Science (Biomed) at the University of<br />
Queensland and is currently completing a Doctor of Medicine as well as<br />
a Graduate Certificate in Business Leadership. Narawi is pssionate about<br />
Badtjala culture and aspiring to improve Indigenous and mental health.<br />
Hunter Valley<br />
The Australian Indigenous Doctors’ Association<br />
(AIDA) celebrated 20 years strong by holding their annual<br />
conference for <strong>2017</strong> in the Hunter Valley, traditionally<br />
owned by the Wonnarua people. This four-day long intensive<br />
collaboration of keynote speakers, engaging workshops as<br />
well as invaluable cultural and networking events created<br />
a leading platform to connect and be inspired. The AIDA<br />
<strong>2017</strong> conference focussed on “family, unity and success”<br />
with the overarching theme of supporting and connecting<br />
Aboriginal and Torres Strait Islander medical students and<br />
doctors to ultimately improve the health of Indigenous people<br />
in Australia.[1] This conference has grown to not only bring<br />
Indigenous students and doctors together but also to provide<br />
networking opportunities for associate members, medical<br />
college representatives, other health professionals and key<br />
invited guests, making it an important medical and political<br />
event.<br />
“...in the medical curriculum, where<br />
education about Aboriginal and Torres<br />
Strait Islander culture and cultural safety<br />
is often poor, undervalued or realistically<br />
done too late to change some attitudes<br />
and beliefs.”<br />
Family<br />
This was the second AIDA conference I have attended as a<br />
medical student. I believe many people would underestimate<br />
the value of bringing together fellow Indigenous medical<br />
students and doctors from across Australia. However, this<br />
sense of belonging and knowing you are not alone in medicine,<br />
whether it be through sharing stories in the yarning circle<br />
44
or networking in the lunch break, is why I believe the AIDA<br />
conference and AIDA itself is so successful. Recently, AMSA<br />
Blue Week highlighted conversations regarding the need to<br />
do more about the mental health crisis amongst medical<br />
students and doctors.[2] Research also shows that mental<br />
health disorders are more prevalent amongst Indigenous<br />
Australians than their non-Indigenous counterparts [3] and it<br />
is well documented that good social support is protective for<br />
mental illness.[4] This highlights the importance for Aboriginal<br />
and Torres Strait Islander medical students and doctors, in<br />
particular, to have a strong support network throughout their<br />
medical journey. AIDA provides a support network as a familylike<br />
organisation, its members backing each other as they<br />
embark on their medical careers and embrace the enormous<br />
task of improving Indigenous health.<br />
Unity<br />
So what do we know about Indigenous health? There is<br />
still a lot to do, but as an attendee of the AIDA conference, I<br />
was surrounded by people who are already are, or are soon<br />
to be, making a real impact on many people’s lives. However,<br />
the media continues to portray a narrative that there are<br />
only a few well-educated Aboriginal or Torres Strait Islander<br />
people. Australia’s history of Aboriginal and Torres Strait<br />
Islander people is still poorly taught in schools. Not only this<br />
but key Aboriginal and Torres Strait Islander people in the<br />
past who have formed a better path for our people are either<br />
unheard of or undervalued in our society.[5] This is reflected<br />
in the medical curriculum, where education about Aboriginal<br />
and Torres Strait Islander culture and cultural safety is often<br />
poor, undervalued or realistically done too late to change<br />
some attitudes and beliefs.[6]<br />
broader society, particularly in how we value Aboriginal and<br />
Torres Strait Islander lives, challenge racism and become<br />
more culturally aware. At this year’s AIDA conference,<br />
it was encouraging to see many of the medical college<br />
representatives understand the need for more Indigenous<br />
doctors, and the need for cultural change to challenge racism<br />
and improve cultural awareness within their own colleges.<br />
Medicare exclusions for prisoners is a key issue that<br />
highlights systemic racism and contributes to health<br />
disparities. Currently, prisoners in Australia are excluded<br />
from Medicare and the Pharmaceutical Benefits Scheme<br />
subsidies. This limited access to good healthcare is<br />
shortening life expectancy and decreasing the quality of life<br />
of many people who are incarcerated.[<strong>11</strong>] Aboriginal and<br />
Torres Strait Islander people are over-represented in prisons<br />
and are 13 times more likely to be incarcerated.[12] This is<br />
not closing the gap but in fact, widening the existing chasm in<br />
health disparities.[13]<br />
The beautiful but complex aspect to Aboriginal and Torres<br />
Strait Islander people and culture is that there are many<br />
communities, languages and cultural protocols; in improving<br />
Indigenous health there is no “one size fits all” approach. The<br />
best outcomes at a grass-roots level are when a community<br />
is meaningfully involved, a lengthy but essential strategy to<br />
drive improvements to Indigenous health.[14] Targeting the<br />
social determinants of health are also key, however tackling<br />
systemic racism, the lack in cultural awareness and creating<br />
a cultural change in society to value Aboriginal and Torres<br />
Strait Islander lives should be our focus for enduring change.<br />
All medical students and medical schools in Australia<br />
The question then arises: is the problem really about the<br />
lack of teaching about Aboriginal and Torres Strait Islander<br />
culture, when racism (both institutional and interpersonal) is<br />
known to be associated with poorer health and poorer health<br />
outcomes?[7] Should the curriculum entail teachings on<br />
racism, both identifying it and stopping it? This conference<br />
asked whether it is the job of Indigenous people to educate<br />
non-Indigenous people on racism itself. The term “hidden<br />
curriculum” – the values and attitudes that medical students<br />
see around them – highlights the importance of lecturers,<br />
tutors, administrators and academics in showing strong<br />
leadership and changing the culture of our universities to<br />
stop racism and strongly value Aboriginal and Torres Strait<br />
Islander culture and health.[8]<br />
It is not just universities that need to step up. The United<br />
Nations (UN) recently described Australia’s progress in<br />
Closing the Gap as “woefully inadequate”.[9] Hearing this<br />
in a room full of people who are driving positive change<br />
and having real impacts on lives can be very disheartening,<br />
especially when Aboriginal and Torres Strait Islander people<br />
make up only 2.8% of Australia’s population.[10] However,<br />
this highlights the importance for all Australians to unite to<br />
make Indigenous health an absolute priority amongst many<br />
key stakeholders. There needs to be a cultural change in<br />
Painted stethoscope<br />
45
should start talking about the idea that you are not clinically<br />
competent until you are culturally competent. This is<br />
imperative to reduce existing health disparities and eradicate<br />
diseases still present in remote Indigenous communities.<br />
AIDA and their supporters are ready to save and improve<br />
Aboriginal and Torres Strait Islander peoples lives, but<br />
everyone should also feel a sense of responsibility to unite to<br />
change the narrative from “woeful” to making real and lasting<br />
change.<br />
Success<br />
One of the most anticipated events of the conference<br />
every year is the stethoscope ceremony. This ceremony is<br />
where newly graduated Indigenous medical students and<br />
newly qualified Indigenous fellows are recognised for their<br />
hard work, sleepless nights, sacrifice and often added<br />
weight of responsibility by being presented with a handpainted<br />
stethoscope. This creates mentorship at AIDA and<br />
inspiration that success is possible and very achievable as<br />
an Indigenous medical student and graduate.<br />
The other most anticipated event (for me anyway) is the<br />
cultural excursion on the last day. I had very high expectations<br />
after last year, living dangerously and tasting a particular<br />
species of ant that tasted like citrus. However, I survived<br />
that last year, and can tell you that I thoroughly enjoyed the<br />
trip this year when people of the Wonnarua nation took us<br />
to Biame cave, the site of a significant piece of rock art in<br />
the Hunter Valley. These opportunities to have culture and<br />
knowledge shared are invaluable. What I also learnt was<br />
about how the traditional owners had worked with the non-<br />
Indigenous property owners on which this significant site sits<br />
in order to protect it, and make it accessible for those who<br />
wish to visit and appreciate its significance - thousands of<br />
“All medical students and medical schools<br />
in Australia should start talking about the<br />
idea that you are not clinically competent<br />
until you are culturally competent.<br />
years of culture and knowledge. The Wonnarua people also<br />
believe there are many other significant sites around that<br />
area. They hope that by setting this as precedent, not only<br />
can they work with other property owners in the region, but<br />
this can be applied to other significant sites across Australia.<br />
So, if you, your family or your friends own a property with an<br />
Indigenous site on it, or if you are unsure, please be in contact<br />
with your local Indigenous community because there may<br />
be thousands of important sites nationwide that need to be<br />
protected for generations to come.<br />
When talking about medicine today, we often think of just<br />
the mind and body, but for many Indigenous people, there<br />
is an element of the spirit. It is also important to recognise<br />
that before colonisation, traditional healers or Ngangkari<br />
looked after our people, probably with the same care and<br />
dedication we hope to have as good doctors one day. These<br />
Ngangkari included the spirit in healing; some are still around<br />
today treating Indigenous people. So from an Indigenous<br />
medical student’s perspective, in a society faced with racism<br />
and disparity, perhaps we should put the humanity back into<br />
medical school and not just hope, but work hard to create<br />
a better world and health outcomes for this nation’s first<br />
peoples.<br />
Conflict of Interest<br />
None declared<br />
Correspondance<br />
narawi.kefb@gmail.com<br />
References<br />
1. Australian Indigenous Doctors’ Association. AIDA Conference<br />
<strong>2017</strong> [Internet].[cited <strong>2017</strong> Oct 1]<br />
Available from: https://www.aida.org.au/conference/<br />
2. AMSA mental health. About the Campaign. [Internet]. [cited<br />
<strong>2017</strong> Oct 1].<br />
Available from: http://mentalhealth.amsa.org.au/about-thecampaign/<br />
3. Jorm A, Bourchier S, Cvetkovski S, Stewart G. Mental health<br />
of Indigenous Australians: a review of findings from community<br />
surveys. Med J Aust. 2012 196 (2):<strong>11</strong>8-121.<br />
4. Ozbay F, Johnson D, Dimoulas E, Morgan C, Charney D,<br />
Southwick S. Social Support and Resilience to Stress. Psychiatry<br />
(Edgmont). 2007 May 4(5):35-40.<br />
5. NITV. Do our teachers care enough about Indigenous<br />
Australia to bring it into the classroom? [Internet]. <strong>2017</strong> May 9<br />
[updated <strong>2017</strong> May 9; cited <strong>2017</strong> Oct 1].<br />
Available from: http://www.sbs.com.au/nitv/article/<strong>2017</strong>/05/09/<br />
do-our-teachers-care-enough-about-indigenous-australia-bring-itclassroom<br />
6. Durey A. Reducing racism in Aboriginal health care in<br />
Australia: where does cultural education fit? Australian and New<br />
Zealand Journal of Public Health. 2010 July 34(1):87-92.<br />
7. Larson A, Gillies M, Howard P, Coffin J. It’s enough to make<br />
you sick: the impact of racism on the health of Aboriginal Australians.<br />
Australian and New Zealand Journal of Public Health. 2007 August<br />
31(4):322-229.<br />
8. Mahood S. Medical education-Beware the hidden curriculum.<br />
Can Fam Physician. 20<strong>11</strong> September 57(9):983-985.<br />
9. Brennan, B. Australia’s progress on Closing the Gap ‘woefully<br />
inadequate’, UN says. [Internet]. ABC News. <strong>2017</strong> September <strong>11</strong><br />
[cited <strong>2017</strong> Oct 2].<br />
Available from: http://www.abc.net.au/news/<strong>2017</strong>-09-<strong>11</strong>/closingthe-gap-progress-woeful-un-says/8892980<br />
10. Australian Bureau of Statistics. Census: Aboriginal<br />
and Torres Strait Islander population. [Internet]. <strong>2017</strong><br />
June 27 [updated <strong>2017</strong> June 26; cited <strong>2017</strong> Oct 2]<br />
Available from: http://www.abs.gov.au/ausstats/abs@.nsf/<br />
46
Four perspectives on<br />
the World Congress on public health<br />
[Conference report]<br />
Michael Au, Ka Man Li, Helena<br />
Qian and Michael Wu<br />
“Leadership is the capacity to translate vision into reality”<br />
– Warren Bennis<br />
The World Congress on Public Health (WCPH) is held every<br />
2-4 years and organised by the World Federation of Public<br />
Health Associations (WFPHA). Attracting between 2000-<br />
4000 delegates from over 80 countries, the main objective of<br />
this international forum was to engage diverse voices, ideas,<br />
vision and actions of committed professionals and citizens<br />
to strengthen and transform the global public health effort<br />
and influence decision makers.[1] With a comprehensive<br />
academic program, field trips, World Leadership Dialogues,<br />
satellite events and meetings, and a glitzy social program,<br />
this is truly the ultimate conference for public health inclined<br />
peers.<br />
To apply, there was a simple online questionnaire and<br />
requirement to volunteer at least 20 hours throughout the<br />
conference. As this meant volunteering for four hours per day,<br />
I wasn’t able to attend all the academic workshops/sessions.<br />
I mainly worked with the media department whereby I sent<br />
interesting quotes from plenary sessions to the team for<br />
Twitter content. I also had the opportunity to directly converse<br />
with speakers in a relaxed setting, after their interview with<br />
the media team.<br />
We evaluate the experiences of attending the WCPH,<br />
the benefits of meeting like-minded individuals, the sense<br />
of optimism in the face of challenge and the problems on<br />
financial supports in four different perspectives: a volunteer,<br />
a presenter, a medical student and a young researcher.<br />
A Volunteer’s Perspective - Helena Qian<br />
Helena is a third year medical student at the University<br />
of Newcastle with a keen interest in improving global health<br />
and aiding underserved communities. She hopes to work with<br />
WHO and MSF in the future as a collaborative researcher,<br />
advocate, field doctor and volunteer.<br />
“When ‘I’ is replaced with ‘We’, even ‘Illness’ becomes<br />
‘Wellness’.” - Malcolm X<br />
As someone passionate about improving public health,<br />
I noticed a curriculum gap in which public health was only<br />
briefly touched upon. WCPH was the perfect meeting of<br />
likeminded individuals, leaders and global health enthusiasts<br />
from which I could gain a holistic understanding of public<br />
health from a grassroots standpoint to a global perspective.<br />
With a registration fee of $770 for students (excluding<br />
accommodation and flights) and being on a uni student<br />
budget, I opted to attend the conference for free as a<br />
volunteer.<br />
Despite the vast array of expertise and interests,<br />
discussion points centred around the confluence of global<br />
environmental degradation, differing political agendas,<br />
civil unrest and widening inequities in health outcomes.<br />
Interestingly, despite proven health detriments from excess<br />
alcohol, tobacco and sugar consumption, Prof. Mike Daube<br />
stated, ‘Where engagement has occurred, it has invariably<br />
been counterproductive.’ Hence, a significant barrier<br />
preventing implementation of effective public health policies<br />
are the industry groups who place private profits over the<br />
health of their consumers. As Dr Bronwyn King eloquently<br />
encapsulated, “60% of the tobacco industry involves child<br />
labour - is there no baseline standard below which we will<br />
sink to raise money?” Where negotiations with industry have<br />
failed, focus has shifted to the consumer. Exposing the fund<br />
managers who invest in these corporations and highlighting<br />
that indirect health and environmental costs rest with<br />
taxpayers, whereas revenue stays with manufacturers, have<br />
resulted in approximately $5 billion AUD being withdrawn<br />
from investment in the tobacco industry alone.[2]<br />
47
Ultimately, the conference epitomised the power of public<br />
health to draw connections to unseen patterns of disease,<br />
highlighted hidden societal inequalities and served as a<br />
platform for marginalised or underserved populations to have<br />
a say. Backed by epidemiology and evidence based medicine,<br />
public health brings ugly truths to the forefront of discussion<br />
and ‘has a duty to speak truth to power’.<br />
I’m immensely grateful to have attended as a volunteer and<br />
to have met such an inspiring network of public health leaders<br />
and fellow peers. As a student, I highly recommend attending<br />
as a volunteer, especially as you gain unprecedented access<br />
to event organisers and plenary speakers. Hope to see you at<br />
the 16th WCPH in Rome 2020!<br />
A Delegate’s Perspective - Michael Wu<br />
Michael is a second year medical student and current Chair<br />
of GlobalHOME at the University of Sydney with a burning<br />
passion for health that disregards borders. Like Helena, he<br />
dreams of working all over the world with MSF. His heroes include<br />
inspirational figures such as Dr Catherine Hamlin. He also enjoys<br />
sunsets and hummus.<br />
The most palpable feeling one senses at a gathering of<br />
minds tackling the most complex social health issues in the<br />
world is that of positivity. Despite the clear adversity, there is<br />
a strong belief that we have the tools and allies needed to<br />
succeed in our agendas.<br />
As anyone that is interested in optimising health outcomes<br />
and promoting medical equity, the words “World Congress<br />
of Public Health” instantly caught my attention when I first<br />
heard them. The WCPH was a melting pot of inspiration,<br />
edgy research and health reform superstars from all over the<br />
world. This gathering does not come cheap but it also comes<br />
only once every 2-4 years and can be anywhere in the world.<br />
It was an opportunity I couldn’t miss.<br />
To pay for my privilege to be a fly on the wall I sought<br />
the assistance of the University. Unfortunately, the Sydney<br />
Medical Program only sets aside funds for conferences if you<br />
are a presenter, however, the Sydney University Postgraduate<br />
Association was more than happy to hear me out. All I had<br />
to do was attend a general meeting, provide background<br />
information on the event and my interest and how this can<br />
benefit their interests then prepare an “ask”. They saw fit<br />
to offer me a grant for $480 to subsidise my registration in<br />
exchange for sharing what I learnt with their Women’s Officer<br />
and Environmental Officer.<br />
This year, the University of Sydney’s Global Health<br />
Society - GlobalHOME - committed to numerous key areas<br />
of interest, including climate change and the impact on<br />
Healthcare. The plenaries for the WCPH not only had this,<br />
but also talks about Female Genital Mutilation, First Nations<br />
people, Non-Communicable Disease and Tobacco Control.<br />
These were talks dedicated to some of the most difficult<br />
healthcare issues today, and WCPH would see some of the<br />
greatest minds gather to discuss them. With Plain Packaging<br />
2.0, we may start seeing cigarettes marked along their length<br />
with the cost to your life expectancy. There was research<br />
on the resiliency of health care systems in warzones. One<br />
researcher working on his PhD had just returned from Eritrea<br />
to add to his pool of data from nine other countries into which<br />
he had ventured during active fighting.<br />
As a student, it is a little daunting to attend a professional<br />
conference out of your direct field but all you need is an<br />
interest and passion. I made many connections and took<br />
home plenty of key messages. I would encourage anyone<br />
looking to attend a professional conference to do so<br />
and to not be fazed by a lack of scholarship availability. It<br />
would be worthwhile approaching your student council or<br />
representative organisation and present to them to secure a<br />
bursary of your own making.<br />
A Presenter’s Perspective - Michael Au<br />
Michael is a fourth year medical student at James Cook<br />
University. He is committed towards the promotion of human rights,<br />
social justice, and health equity. His interests lie in refugee and<br />
maternal health, health systems and the social determinants of<br />
health. He is currently completing research investigating refugee<br />
health systems in Far North Queensland.<br />
Although there is much to celebrate in public health, Dr<br />
Margaret Chan at the conference described “new challenges<br />
of unprecedented complexities” facing the world in the areas<br />
of antibiotic resistance, obesity and chronic diseases. These<br />
issues are intertwined with social, political and cultural issues<br />
which make them increasingly difficult to address.<br />
The status quo is not enough and there is still so much to be<br />
achieved in public health. However, many students, including<br />
myself, fall into the trap of complacency towards the state<br />
of affairs in global health. As Australian students, we view<br />
the rest of the world through the lens of a developed country,<br />
distorted by daily privileges which we take for granted. The<br />
solution? A continual pursuit for truth and information with a<br />
high degree of scientific scepticism. This was just one of the<br />
few gems I gathered from this conference.<br />
With the support of the Royal Australasian College of<br />
Physicians (RACP), I was fortunate to be given full registration<br />
and travel assistance to attend the WCPH as a John Snow<br />
Scholar. The scholarship gave me the opportunity to present<br />
research which I had completed as a medical student, entitled<br />
48
“HIV/HCV Prevention in Australian Incarcerated Populations:<br />
A Review into Preventative Practices and Outcomes”. My<br />
review highlighted the growing disparity in health outcomes<br />
between prison populations and the community due to a<br />
lack of preventative programs in Australian prisons against<br />
infectious blood-borne diseases. I encourage all medical<br />
students to consider applying for the John Snow Scholarship.<br />
[3]<br />
Attending this conference gave me the opportunity to<br />
meet with leading academics in my area of research. In<br />
addition to bringing together academics from across the<br />
globe, both government and private sectors were closely<br />
involved. It was my great pleasure to meet with the Australian<br />
Capital Territory (ACT) Chief Health Officer who was leading<br />
the reform in needle-syringe programs as well as other<br />
academics prominent within the field of my research topic. I<br />
found this most peculiar and warming, that an event like this<br />
is able to bring people together from different parts of the<br />
world, addressing a certain issue and to share, foster and<br />
inspire other like-minded individuals.<br />
Many medical students would have had experience<br />
in attending AMSA Global Health and AMSA National<br />
Convention events. The WCPH differs to AMSA events in that<br />
it is a professional research intensive conference. These<br />
events demarcate the knowledge frontier in public health<br />
in a setting that aims to create professional networks and<br />
expanding partnerships.<br />
A Young Researcher’s Perspective - Ka Man Li<br />
Ka Man is a final year Biomedical Science student at<br />
the University of Melbourne with a strong devotion to furnish<br />
approaches for current health concerns: healthy ageing and<br />
preventive cardiology. She aims to serve as a part of WHO<br />
and WFPHA to optimise global health in the nearest future.<br />
“Pioneering spirit should continue, not to conquer the<br />
planet or space... but rather to improve the quality of life.” –<br />
Bertrand Piccard<br />
As a young researcher, I always dreamt about either<br />
standing behind the podium presenting my novel research<br />
findings in front of experts in the field, or seeing my name on<br />
publications. On the 4th of April this year, my dream finally<br />
came true.<br />
It all began an hour before a regular Monday meeting with<br />
my supervisor. With little progression in my thesis, I did not<br />
want to be a disappointment thus I googled an upcoming<br />
conference related to my research field. I submitted an<br />
abstract in the spur of the moment to this conference. Months<br />
later, I got accepted as an orator for my study entitled, “The<br />
Effect of Physical Activity, Body Mass Index on Cardiovascular<br />
Risk in Australian Older Women”. I was overwhelmed by a<br />
cocktail of excitement and anxiety.<br />
Weeks before the conference commenced, I spent<br />
countless days and nights working on my results for the<br />
presentation, enduring many failures along the way. Numerous<br />
times, I had to go back and forth changing the inclusion and<br />
exclusion criteria for my literature review, refining the rationale<br />
and interpreting my statistical regressions. However, with<br />
the support and encouragements from my supervisor and<br />
colleagues, I finally finished my results for the presentation.<br />
As soon as I arrived at the venue of WCPH, my first<br />
international conference, all my doubts, insecurities and<br />
anxieties suddenly vanished. I was impressed by the scale,<br />
the conference production value and the number of people<br />
participating! It was a pleasure to meet with a diverse group<br />
of delegates from different professional fields across<br />
the globe. We were able to share personal experiences,<br />
discuss typical research mistakes and exchange knowledge<br />
about improving global health. One of the most memorable<br />
highlights was meeting with leading academics, including Dr<br />
Michael Moore, President of the World Federation of Public<br />
Health Associations (WFPHA) and the CEO of Public Health<br />
Association of Australia. Not only did he inspire me with his<br />
persistence and belief in research but he also expanded my<br />
vision for certain health issues with different perspectives.<br />
Ultimately, WCPH was a life-changing conference. I was<br />
delighted to achieve my dream at such an early stage of my<br />
research career, presenting formally at one of the biggest<br />
international conferences. WCPH has certainly reignited my<br />
unwavering passion for public health research despite all the<br />
challenges. It has given me an opportunity to engage, learn<br />
and foster ideas with many like-minded individuals.<br />
Although funding is not always available for research<br />
students, conferences like WCPH are worth the cost! As Mr<br />
Greg Hunt, MP, stated at the opening ceremony, we need<br />
more frontier researchers to contribute to and enhance<br />
quality of life. We, as tomorrow’s researchers, ought to raise<br />
our voices to develop a comprehensive vision to take action<br />
and improve global health nationally and globally.<br />
Acknowledgements<br />
Sydney University Postgraduate Representative Association<br />
(Michael Wu)<br />
Royal Australasian College of Physicians (RACP) (Ka Man Li)<br />
Photo Credit<br />
Helena Qian, Michael Wu, Michael Au, Ka Man Li<br />
Conflicts of interest<br />
None declared<br />
Correspondance<br />
helena.qian@uon.edu.au<br />
References<br />
1. WCPH About [Internet] Retrieved on 28th August <strong>2017</strong>; Last<br />
Updated <strong>2017</strong>. Available from: http://www.wcph<strong>2017</strong>.com/about.php<br />
2. WCPH Program Handbook. Proceedings of the World Congress<br />
of Public Health; <strong>2017</strong> Apr 3-7; Melbourne, AU. <strong>2017</strong>.<br />
3. John Snow Scholarship Information website [Internet]<br />
Retrieved on 10th September <strong>2017</strong>; Last Updated <strong>2017</strong>. Available<br />
from: https://www.racp.edu.au/about/racp-foundation-awards/<br />
division-faculty-chapter-regional-awards/australasian-faculty-ofpublic-health-medicine/john-snow-scholarship<br />
49
Welfare cuts to refugees, AMSA Global Health<br />
Crossing Borders National Managers<br />
[Commentary]<br />
Sibella Breidahl<br />
and Jasmin Sekhon<br />
Crossing Borders For Health is AMSA Global Health’s project that aims to advocate for<br />
refugees and people seeking asylum. With arms covering Education, Advocacy and<br />
Projects we aim to give students a functional understand of the refugee crisis, with a<br />
focus on the Australian context, as well as contributing to the advocacy based around<br />
creating a fair and fast processing system for people seeking asylum in Australia. Jasmin<br />
and Sib are Crossing Border’s <strong>2017</strong> National Project Managers<br />
We live in a society founded on the values of fairness,<br />
reciprocity and freedom. Whether you call it a scallop<br />
or a potato cake, you’re a millennial or older than Phillip<br />
Ruddock, across lines of politics and race, these values<br />
hold true.<br />
We would all like to think that in our moment of<br />
need we would be supported by our<br />
community. Daily across Facebook and<br />
the media, there are countless examples<br />
of people proudly going above and<br />
beyond for members of their community,<br />
even for complete strangers. The<br />
#sofaforlondon movement in the wake<br />
of the London Bridge attack earlier this<br />
year is a perfect example of this. People<br />
posted on social media offering beds<br />
(and salt and vinegar chips) to strangers who were left<br />
stranded in the attacks.[1] Examples of this exist at<br />
home as well, like the overwhelming response after the<br />
Victorian bushfires in the last decade. We are great at<br />
jumping into action when people need help. Why then,<br />
are Australians so happy to eschew these values when<br />
We are great at jumping into<br />
action when people need<br />
help. Why then, are Australians<br />
so happy to eschew these<br />
values when considering the<br />
question of refugees?<br />
considering the question of refugees?<br />
Many social and economic factors inform the health<br />
and wellbeing of humans. Housing insecurity, job hunting,<br />
lack of access to proper medical care, limited education<br />
pathways, lack of transport. These things pile up. Not<br />
only do refugees face these stresses with no supportive<br />
community or family, but also after years<br />
of trying to get to Australia, often fleeing<br />
horrific wars, genocides and famines.[2]<br />
At the time of their greatest need, the<br />
government resolves that the best thing<br />
to do it to lock them up and throw away<br />
the key.<br />
The government decided in late<br />
August to cut welfare payments to 100<br />
of the 400 people seeking asylum in Australia that have<br />
come to the mainland from regional processing centres<br />
for medical treatment.[3] They plan to extend the cuts to<br />
the other 300 people in this group in the coming months,<br />
including pregnant women, 37 babies and 90 children<br />
who attend school in Australia. This means they will stop<br />
50
eceiving the paltry $200 a fortnight they have to support<br />
their family, and will also be kicked out of supported<br />
accommodation. With a name that would not be out of<br />
place in an Orwell novel, the “Final Departure bridging E<br />
visa” which stipulates these conditions, was given to 100<br />
people with no notice.<br />
It is deeply concerning that<br />
post-arrival factors have a<br />
worse impact on the outcomes<br />
for children seeking asylum,<br />
than the trauma of the wartorn<br />
countries they come from<br />
As a young, qualified person with an acceptable grasp<br />
of the English Language and a good knowledge of the<br />
workings of Australian society, I know how hard it can be<br />
to find a job. These people who have been transferred to<br />
Australia for serious medical illness must find a way to<br />
support themselves in just three weeks, with the possibility<br />
of being deported at any time, a prospect sure to turn<br />
off any employer. To add insult to injury, the government<br />
has also stuck by its policy that those over 18 years old<br />
cannot access education or training programs, giving<br />
them even less opportunity to find jobs. This has huge<br />
implications for those at school. Why bother applying<br />
yourself and working hard, just to be barred from further<br />
education and face a desperate future?<br />
Being transferred to Australia in the first place is no<br />
mean feat, as we have seen in several cases, such of<br />
that of Hamid Kazhei, who died on Manus Island of sepsis<br />
from a cut in his foot because the government would<br />
not transfer him to the mainland to get the attention<br />
he needed. Or the multiple pregnant mothers with preeclampsia<br />
who have been refused transfer and have no<br />
access to obstetric care. This shows that the group in<br />
question who did make it to Australia are extraordinarily<br />
resilient and are in genuine need of care.<br />
There is strong evidence to show that reduction in<br />
funding for welfare has major effects on the health of<br />
newcomers. Eroding economic and social conditions<br />
negatively impacts on health by reducing access to<br />
healthcare, deterioration in mental health and increases<br />
domestic violence. [4]<br />
The government has already made people seeking<br />
asylum vulnerable, through damaging policies that<br />
incorporate unnecessarily long processing times, keep<br />
people in detention under inhospitable conditions, offer<br />
few options for family reunification, deny full work rights<br />
and withhold social services. This new policy will further<br />
exacerbate the disadvantage that these people currently<br />
endure.<br />
It is deeply concerning that post-arrival factors have<br />
a worse impact on the outcomes for children seeking<br />
asylum, than the trauma of the war-torn countries they<br />
come from.[1] A recent study published in the Journal<br />
of Paediatrics and Child Health showed that childrens’<br />
environment after arriving in Australia had more impact<br />
on their physical health and wellbeing than the process<br />
of getting to Australia and the traumas they experienced<br />
before arriving.[5] Irresponsible policies like the recent<br />
welfare cuts contribute strongly to this observation. The<br />
government even went as far as threatening children in<br />
their letter about the Bridging E visa, writing to parents<br />
“Please remind your children that they will also be<br />
required to abide by Australian values and laws. Breaking<br />
Australian laws may result in their removal from the<br />
community.”[3]<br />
Refugees and people seeking<br />
asylum are starting from a point of<br />
compromise. It is our obligation as a<br />
caring community that values equity<br />
to springboard them into starting their<br />
lives in Australia<br />
The Government is pushing the financial burden to<br />
support asylum seekers on community and not-for-profit<br />
organisations, straining their already limited resources.<br />
Refugees and people seeking asylum are starting from<br />
a point of compromise. It is our obligation as a caring<br />
community that values equity to springboard them<br />
into starting their lives in Australia, rather than holding<br />
them back or providing a flimsy safety net. It’s time to<br />
say enough is enough and stop them bullying the most<br />
vulnerable members of our society.<br />
Conflicts of interes<br />
None declared<br />
Correspondance<br />
jasmin.sekhon@amsa.org.au<br />
sibella.harebreidahl@amsa.org.au<br />
References<br />
1. The Guardian staff and Press Association (<strong>2017</strong>).<br />
#sofaforlondon: residents open their doors in wake of London<br />
Bridge attack. The Guardian.<br />
2. Marmot, M., Wilkinson R. (2003). Social Determinants<br />
of Health, The Solid Facts. [online] The World Health<br />
Organisation. Available at: https://books.google.com.au/<br />
51
Start where you are, use what you<br />
have, do what you can<br />
-<br />
Adelaide Global Health Conference <strong>2017</strong> Closing Address<br />
AMSA Global Health Chair <strong>2017</strong><br />
Liz Bennett<br />
Good afternoon, wonderful GHC delegates. I’m Liz,<br />
the Chair of AMSA Global Health and a final year medical<br />
student at Flinders. As some of you would have heard<br />
yesterday, my experiences in global health have taken me<br />
from Adelaide, to Tennant Creek, to Oxford, to Geneva,<br />
and to Tanzania, but GHC has always held a special<br />
place in my heart and attending my first GHC was one of<br />
the first steps on my global health journey.<br />
I wanted to start by taking some time to reflect<br />
on my time with AMSA Global Health this year. AMSA<br />
Global Health is a team of 22 people from around the<br />
country who work year round to advocate for, represent<br />
and educate medical students like you on global health<br />
issues. We focus on refugee and asylum seeker health,<br />
climate health, sexual and reproductive health and most<br />
recently non-communicable diseases.<br />
There have been so many incredible moments this<br />
year, from watching Sib, one of our Crossing Borders<br />
For Health National Project managers, shine in her first<br />
radio interview on refugee and asylum seeker health; to<br />
watching Georgia, our Vice Chair Operations seamlessly<br />
put the Council agenda together; to reading the amazing<br />
divestment action plan for AMSA put together by the<br />
Code Green National Project Managers, the Belles; to<br />
seeing Carrie publish the first copy of <strong>Vector</strong>, our student<br />
written, peer-reviewed global health journal, in two years<br />
and then watch her guard the hard, print copies with her<br />
life! I’ve participated in AMSA Global Health meetings<br />
from Byron Bay, from Alice Springs, Darwin, Geneva and<br />
most recently using dodgy airport internet in Tanzania,<br />
and every single one has been a joy.<br />
I would like to thank my AMSA Global Health team for<br />
all of the amazing work they have done this year. It has<br />
been a privilege to work with each and everyone one of<br />
you and it has been incredible to watch your passion grow<br />
into tangible products that have benefited so many.<br />
At GHC, we are given the chance to learn how<br />
phenomenal and passionate individuals - who are<br />
often our idols - are making change. We are inspired,<br />
challenged and empowered to then go forth and change<br />
ourselves. I still remember sitting in plenary hall in Hobart<br />
at my first GHC in 2013, listening to Julian Burnside talk<br />
about his work in refugee and asylum seeker advocacy.<br />
It was one of the first times I actually heard about the<br />
impacts of immigration detention and I started crying<br />
because I had never heard someone speak so candidly<br />
52
about its devastating mental health effects. I could not<br />
believe that this was happening in our country and that<br />
our government was knowingly subjecting vulnerable<br />
people to institutionalised torture. After a small period of<br />
feeling hopeless, I began to get angry. It was this seed of<br />
anger that has fuelled my passion for health inequalities<br />
more broadly since then and I think this is a reason why I<br />
am up here today.<br />
But it is not enough to be<br />
inspired. There is too much<br />
to be done. We do not have<br />
the luxury of apathy and you<br />
cannot afford to waste time<br />
thinking that you are too small<br />
to make a difference.<br />
However, if you had told me then that four years from<br />
now, I would have been able to learn about global health<br />
research with the George Institute in Oxford, I would have<br />
been fortunate enough to spend 6 weeks being inspired<br />
by global health babe, Sandro Demaio at the WHO in<br />
Geneva, and that I would eventually publish an article with<br />
Julian Burnside in the Lancet calling for immediate action<br />
on refugee and asylum seeker health, I would not have<br />
believed you. But it all started at GHC.<br />
have the luxury of apathy and you cannot afford to waste<br />
time thinking that you are too small to make a difference.<br />
I encourage all of you to leave here and be productive<br />
with the seed of inspiration that has been planted this<br />
week. Continue to challenge yourself to make change and<br />
always foster inquisitiveness and love of global health.<br />
Ensure that you it, watch it grow and share its fruit with<br />
those around you. This might be something as simple as<br />
starting a conversation with someone using some of the<br />
knowledge you gained, it could be putting pen to paper<br />
and recording your ideas to share with others, it could be<br />
joining a local advocacy group doing great work that you<br />
are passionate about in your community, or it could be<br />
joining an organisation like AMSA Global Health.<br />
Start where you are, use what you have and do what<br />
you can.<br />
Photo credit<br />
Karl Asmussen, Vienna Tran<br />
Correspondance<br />
liz.bennett@amsa.org.au<br />
And so I would to thank Holly and her amazing team<br />
for this fantastic event. Since that first GHC in Hobart,<br />
this conference has gone from strength to strength and it<br />
would not be possible without individuals like you.<br />
This conference has given us the ability to challenge<br />
ourselves in many different areas. We have been<br />
provided with an opportunity to realise our strengths, as<br />
well as our faults and imperfections. But it is not enough<br />
to be inspired. There is too much to be done. We do not<br />
53
Where to now?<br />
-<br />
<strong>Vector</strong> Journal & GHC Writing Competition<br />
Helena Qian<br />
Helena is a 3rd year medical student at the University of Newcastle with a keen<br />
interest in improving global health and aiding underserved communities. She hopes<br />
to work with WHO and MSF in the future as a collaborative researcher, advocate,<br />
field doctor and volunteer.<br />
What: “We are resolved to free the human race within<br />
this generation from the tyranny of poverty and want,<br />
and to heal and secure our planet for the present and for<br />
future generations.” – The 2030 Agenda for Sustainable<br />
Development<br />
Society is at a critical juncture in world history<br />
whereby a fragile balance exists between global health,<br />
effects of modern-life, social constructs, politics and<br />
economy.[1] The 2003 SARS epidemic encapsulates<br />
how unprecedented population growth and adverse<br />
living conditions have facilitated cross-species shift of<br />
organisms.[1] Despite incredible medical advances, our<br />
exponential increase in knowledge has not matched<br />
public health progress as seen with the re-emergence of<br />
polio in conflict-affected areas.[2]<br />
Why: “If we see injustice, why can’t we make a change<br />
right now?” – Mr Kon Karapanagiotidis GHC <strong>2017</strong><br />
From conversing with Dr Stewart Condon, poor<br />
application of knowledge due to differing political/<br />
financial agendas have largely been to blame. These<br />
stem from a failure of stakeholders/society to appreciate<br />
the ‘complex links between social and economic aspects’<br />
[1] of disease and address health at a world-population<br />
level.<br />
Contrary to popular belief, there is no shortage of<br />
resources to improve global health,[3] only a lack of moral<br />
imagination and political will to change long-standing,<br />
inefficient healthcare systems and implement strategies<br />
to broaden attitudes towards health.<br />
Where to now? “The world is coming to recognise<br />
more and more that problems in one country reverberate<br />
in another...this is why it is so important to make the most<br />
of our collective strengths.” - Ban Ki Moon<br />
As privileged medical students with access to<br />
platforms that engage our community, we can challenge<br />
the complacency of those who don’t fully comprehend<br />
the magnitude of impact every individual has on others<br />
less fortunate. As future doctors, we should endeavour<br />
to couple excellent care of individual patients to public<br />
health programs that more efficiently disseminates<br />
information and healthcare.<br />
Although the way forward is challenging, it’s not<br />
impossible with positive steps such as the creation of the<br />
Coalition for Epidemic Preparedness Innovations (CEPI)<br />
aiming to efficiently develop new vaccines to prevent<br />
epidemics.<br />
“It is because it is so dark that we need to burn the<br />
brightest right now.”- Mr Kon Karapanagiotidis GHC <strong>2017</strong><br />
Conflicts of Interest<br />
None declared<br />
Correspondance<br />
helena.qian@uon.edu.au<br />
References<br />
1. Solomon R Benatar Global Health: Where to Now?<br />
Retrieved <strong>2017</strong>, August 19; Last Updated Unknown; Global<br />
Health Governance, 2009;<strong>11</strong>;2 Available from: <br />
2. Akil L, Ahmad HA. The recent outbreaks and<br />
reemergence of poliovirus in war and conflict-affected areas.<br />
Retrieved <strong>2017</strong>, August 19; Last Updated 2016; International<br />
journal of infectious diseases : IJID : official publication of the<br />
International Society for Infectious Diseases. 2016;49:40-46.<br />
doi:10.1016/j.ijid.2016.05.025.<br />
3. Benatar, Daar, and Singer, “Global health ethics: the<br />
rationale for mutual caring”; Benatar, Gill and Bakker, “Making<br />
progress in global health: the need for new paradigms.”<br />
Retrieved <strong>2017</strong>, August 21; Last Updated Unknown<br />
Moving forward, societal introspection are shifting<br />
from a narrow, monetised view of global health to a multifaceted<br />
appreciation for an interdependent world that<br />
can drive forces for change. Greater emphasis should<br />
be placed on collaboration to address health inequalities<br />
and social determinants of health.<br />
54
A Walk to Remember<br />
[Book review]<br />
Anna Marie Plant<br />
Anna Marie Plant is a Medical student at the University of Sydney with a<br />
strong interest in Global Health. She wishes to pursue a career in surgery<br />
with a humanitarian focus and work for an organisation such as Médecins<br />
Sans Frontières (MSF) to address the global shortage of safe surgical care,<br />
especially in orthopaedics and trauma.<br />
Walking Free<br />
by A/Prof Munjed Al Muderis with<br />
Patrick Weaver.<br />
p 336. Allen & Unwin. $22.99<br />
Despite our common motivations and<br />
dedication to learning, the journey of each<br />
medical student is unique. Despite managing<br />
intense study loads, we probably cannot<br />
imagine the added stress of living under a<br />
brutal dictatorship, as was the experience of<br />
Associate Professor Munjed Al Muderis. He<br />
began his Medical studies at Basra University<br />
in southern Iraq, near the Kuwaiti border that<br />
former Iraqi President Saddam Hussein’s<br />
forces had invaded a month prior. It was clear<br />
from the outset that A/Prof Al Muderis’ journey<br />
was never going to be straightforward.<br />
awoken the following morning to the sound<br />
of planes overhead and explosions nearby;<br />
it was the 17th of January 1991 and the<br />
commencement of Operation Desert Storm.<br />
After he tended to civilian casualties at his<br />
teaching hospital, he made the journey along<br />
the war-ravaged Western highway, and passed<br />
the Imam Ali Air Base that was under active<br />
airstrikes by the US-led coalition, to Baghdad.<br />
Al Muderis’ gripping vignette ensures that one<br />
will never again complain about long flights or<br />
drives to visit family.<br />
Fast forward and the young Dr Al Muderis<br />
found himself in one of the worst imaginable<br />
situations: he had to choose between honouring<br />
the Hippocratic Oath by refusing to remove the<br />
ears of army deserters, or facing death at the<br />
hands of Saddam’s military police. For most<br />
of us this is a nightmare situation but sadly it<br />
is the reality for some healthcare workers in<br />
unstable geopolitical environments.<br />
“the young Dr Al Muderis found himself<br />
in one of the worst imaginable situations:<br />
he had to choose between honouring the<br />
Hippocratic Oath by refusing to remove<br />
the ears of army deserters, or facing<br />
death at the hands of Saddam’s military<br />
police”<br />
Midway through his first year of medical<br />
school, his parents called one evening and<br />
implored him to return home to safety. He was<br />
After the journey to Australia, his stay in<br />
Curtin Detention Centre would prove another<br />
55
major hurdle. As detainee 982 (names were<br />
replaced by numbers), his experience was the<br />
rule, not the exception: extended periods of<br />
solitary confinement, a general lack of privacy,<br />
and navigating the complex web of rumours and<br />
tensions that a confined environment instigated<br />
between detainees. Detainees were constantly<br />
reminded that their stay was indefinite and they<br />
may never be resettled in Australia, but could<br />
return to their country of origin at any time.<br />
Al Muderis has presented the events of<br />
his life as actions and reactions, rather than<br />
delving into whether his experiences had any<br />
long term psychological toll, however in writing<br />
your own story you afford to keep some cards<br />
close to your chest. Walking Free is the journey<br />
of someone who achieved their dreams against<br />
the odds of complex, challenging and evolving<br />
geopolitical circumstances. It gives a face and<br />
story to those on the other side of the fence:<br />
“Al Muderis has presented the events<br />
of his life as actions and reactions, rather<br />
than delving into whether his experiences<br />
had any long term psychological toll”<br />
The story only briefly covered Al Muderis’ rise<br />
through the medical ranks in Australia, most<br />
likely because the day-to-day experiences<br />
of surgical training are seemingly mundane<br />
in comparison to the preceding journey.<br />
Nevertheless, a more in-depth discussion of his<br />
pioneering use of osseointegration surgery in<br />
Australia would have been appreciated.<br />
Despite the seemingly unbelievable events<br />
of Walking Free, there are some commonalities<br />
about life that hold true irrespective of personal<br />
context. Marriage and a newborn child midway<br />
through medical school was never an easy<br />
undertaking but religious differences and<br />
constant interference from both families<br />
may ensure any union is doomed. There is<br />
the sobering reminder that a bond and later<br />
marriage forged through a treacherous boat<br />
journey and stay in detention could be broken<br />
by the strain of long working hours and constant<br />
relocations associated with a surgical career.<br />
My favourite anecdotes involve the<br />
savviness of Mrs Al Muderis. She managed the<br />
family finances during wartime and economic<br />
sanctions, she provided USD $22 000 in cash<br />
to her son upon hearing his need to flee during a<br />
time in which owning US dollars in Iraqi banks was<br />
prohibited, and organised legal representation<br />
during his stay in Australian detention centres.<br />
When family is involved, mothers will always find<br />
a way.<br />
locked up, anonymous individuals only seen<br />
in glimpses of news reports as the ‘dangerous<br />
other’; individuals that are every bit as human<br />
as us, but who have been dealt a very different<br />
hand in life.<br />
As medical students, it can be easy to<br />
become entangled in the inevitable drama and<br />
competition that surrounds us, and lose sight<br />
of why we are pursuing this goal. Walking Free<br />
is a humbling reminder that everything can<br />
change in the blink of an eye and that no matter<br />
how tortuous the journey becomes, there is<br />
something to be learnt from every step of the<br />
way.<br />
Conflicts of interest<br />
The author of this book review declares that<br />
they have no conflict of interest.<br />
Correspondance<br />
apla9692@uni.sydney.edu.au<br />
56
57